Abstract
A 27-year-old male patient who presented to the emergency room with complaints of sweating, palpitations, heat intolerance, insomnia and weight loss for the last 3 months. His medical history was significant for hypertension. On examination, he was tachycardic, hypertensive, had tremors of the upper extremities and a smooth goitre with a thyroid bruit. Laboratory assessment revealed a suppressed thyroid-stimulating hormone, high free thyroxine and positive thyroid receptor antibodies. Complete blood count showed pancytopenia. As part of the work-up for pancytopenia, haptoglobin, ferritin, Coombs test, reticulocyte count hepatitis B and C antibodies were done, all of which were normal. Patient was started on methimazole, propranolol and hydrocortisone. His symptoms improved through the hospital course and he was subsequently discharged. Thyroidectomy was done once the patient’s hyperthyroidism was controlled. Levothyroxine was started for the control of postsurgical hypothyroidism. Six months after thyroidectomy, the patient was euthyroid and the pancytopenia resolved.
Keywords: thyroid disease, malignant and benign haematology
Background
Graves’ disease is an autoimmune condition in which antibodies are produced against the thyrotropin (TSH) receptors on the thyroid gland. Activation of these receptors by thyrotropin receptor antibodies (TRabs) leads to hyperthyroidism which is clinically characterised by increased appetite, weight loss, palpitations, tremors, hyperdefecation and insomnia.1
Graves’ disease could be associated with a variety of single cell lineage haematological abnormalities including anaemia, thrombocytopenia and leucopenia. However, pancytopenia is a very rare complication of Graves’ disease.2
Case presentation
A 27-year-old male patient who presented to the emergency department with a 3-month history of sweating, palpitations, heat intolerance, insomnia and weight loss. Medical history was significant for hypertension. Vitals on admission revealed a tachycardia of 113/min, blood pressure of 161/101 mm Hg and a temperature of 97.8°F. Examination revealed an anxious disposition, large smooth goitre with a thyroid bruit and fine tremors of the upper extremities. No exophthalmos or pretibial myxedema was noted.
Investigations
Laboratory assessment revealed a suppressed thyroid-stimulating hormone (TSH) and high free thyroxine. Complete blood count (CBC) done before the initiation of methimazole showed anaemia, leucopenia and thrombocytopenia (table 1). As part of the work-up for pancytopenia, haptoglobin, ferritin, Coombs test, reticulocyte count hepatitis B and C antibodies were done, all of which were normal (table 1). Thyroid peroxidase, TRab and thyroid-stimulating immunoglobulin were positive confirming Graves’ disease as the aetiology of hyperthyroidism (table 1). ECG showed sinus tachycardia. Echocardiogram showed an ejection fraction of 55% and normal left ventricular function.
Table 1.
Laboratory assessment on admission
| Sl no. | Test | Result |
| 1. | TSH (0.27–4.2 mcIU/mL) | 0.01 |
| 2. | FT4 (0.9–1.7 ng/dL) | >7.7 |
| 3. | TRab (0–1.75 IU/L) | 33 |
| 4. | TSI (<1.3 TSI Index) | 3 |
| 5. | TPO (<5.6 IU/mL) | 123.38 |
| 6. | Haemoglobin (13–17 g/dL) | 9.5 |
| 7. | White cell count (4–10 x109/L) | 2.7 |
| 8. | Platelets (150–400 x109/L) | 124 |
| 9. | Ferritin (30–400 ng/mL) | 116 |
| 10. | Coombs test | Negative |
| 11. | Haptoglobin (30–200 mg/dL) | 113 |
| 12. | Reticulocyte count (0.5%–2.3%) | 2 |
| 13. | Hepatitis B surface antigen | Negative |
| 14. | Antihepatitis C virus RNA | Undetected |
| 15. | Antiplatelet antibodies | Undetected |
| 16. | HIV antibody | Undetected |
FT4, free thyroxine; TPO, thyroid peroxidase antibody; TRab, antithyrotropin receptor antibodies; TSH, thyroid-stimulating hormone; TSI, thyroid-stimulating immunoglobulin.
Treatment
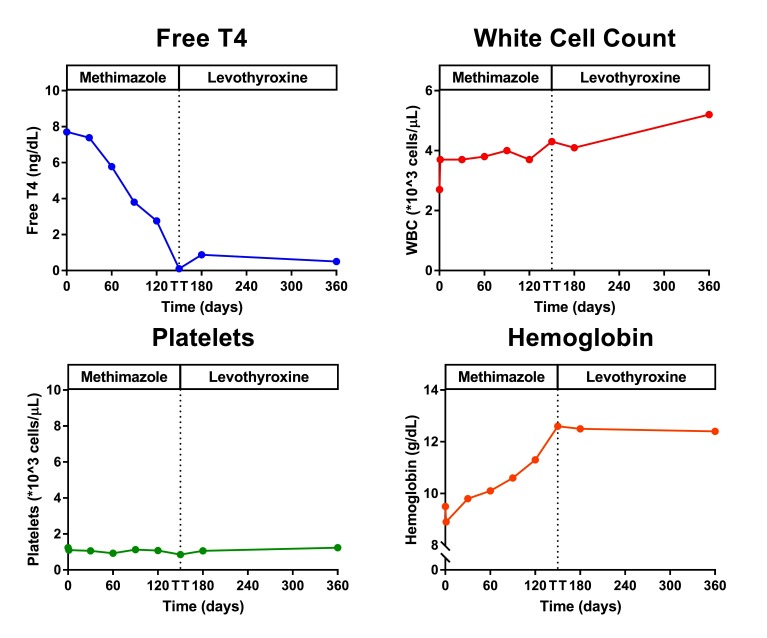
Patient was started on methimazole, propranolol and hydrocortisone for the treatment of his hyperthyroidism. His symptoms improved through the hospital course and he was subsequently discharged. On follow-up in the clinic, patient continued to experience improvement in his symptoms as well as the blood counts (figure 1). Thyroidectomy was done 2 months after the discharge. Pathology revealed diffuse thyroid hyperplasia compatible with Graves’ disease.
Figure 1.
Trends in free T4, white cell count (WCC), platelets and haemoglobin before and after total thyroidectomy.
Outcome and follow-up
Levothyroxine was started for control of postsurgical hypothyroidism. Six months after thyroidectomy, the patient was euthyroid and CBC showed further improvement in the cell count in all cell lines with resolution of pancytopenia (figure 1).
Discussion
Thyroid hormone can affect the haemopoietic system in a number of different ways. While haematological abnormalities are commonly seen in hyperthyroidism clinically significant abnormalities occur infrequently.2 We believe that the prevalence of various haematological disorders in hyperthyroidism is underestimated as haematological parameters are not routinely obtained before initiating therapy. Graves’ disease could be associated with a variety of single cell lineage haematological abnormalities including anaemia, thrombocytopenia and leucopenia. However, pancytopenia is a very rare complication of Graves’ disease.2
Hyperthyroidism causes an increase in the basal metabolic rate as well as oxygen consumption; this causes a relative hypoxia which stimulates the kidneys to secrete erythropoietin.3 Erythropoietin increases the production of red blood cells; however, since there is an increase in the plasma volume as well the haematocrit remains constant.
Hyperthyroidism also causes an increase in 2,3-diphosphoglycerate which decreases the affinity of haemoglobin to oxygen.4
Anaemia is noted in 12%–34% of patients with hyperthyroidism.5 6 Microcytic, normocytic and macrocytic anaemias are observed with hyperthyroidism. Microcytic anaemia could be secondary to accelerated erythropoiesis or iron deficiency.3 Normocytic anaemia is sometimes seen in patients with Graves’ disease with bone marrow erythroid hyperplasia indicating ineffective erythropoiesis.7 Macrocytic anaemia could be secondary to vitamin B12 deficiency or folic acid deficiency.8 Pernicious anaemia which is due to the deficiency of intrinsic factor secretion by the parietal cells in the stomach is seen in about 1%–3% of patients with Graves’ disease.9 Aplastic anaemia can also be secondary to high dose methimazole.10 Our patient had a normal reticulocyte count, iron studies, vitamin B12, folate, haptoglobin and a negative Coombs test. We believe that the anaemia in our patient could have been secondary to ineffective erythropoiesis.
Leucopenia and neutropenia are seen in about 15%–30% of untreated patients who are hyperthyroid.11 Various mechanisms have been implicated which include a decreased granulocyte reserve, decreased leucocyte circulation time and immunological destruction in cases where the antineutrophil cytoplasmic antibody is present.12 13 Agranulocytosis is a well-known side effect of thionamides (methimazole and propylthiouracil).14 It is important to distinguish these two entities as the latter precludes the use of thionamides which are the mainstay of treatment in hyperthyroidism. We therefore recommend a complete blood count in all patients with hyperthyroidism before starting thionamides.
Thrombocytopenia was first noticed in association with hyperthyroidism about 50 years ago. It was believed to be due to increased destruction of platelets secondary to splenic sequestration or antiplatelet antibodies. Antiplatelet antibodies are seen in about 50% of patients with Graves’ disease.15
We searched PubMed using the following keywords: hyperthyroidism or Graves’ disease and pancytopenia. We restricted our search to publications in ‘English’ and involving ‘Human subjects’. Abstract of meetings and unpublished results were not included in our study. The last search was done on 25 November 2017.
The initial search resulted in 27 articles, of which 13 articles were excluded based on the title and abstract. Inclusion criteria was that the pancytopenia be noted prior to the initiation of antithyroid medications. Fourteen articles met the inclusion criteria and were included in table 2.
Table 2.
Literature review 11 16–27
| Sl no. | Authors | Age | Sex | Aetiology | Treatment | Time to recovery of blood counts |
| 1 | Garcia et al 16 | 54 | F | Graves’ disease | RAI | 3 months |
| 2 | Jha et al 17 | 62 | F | Unknown | Unknown | 10 days |
| 3 | Imai et al 18 | 33 | F | Graves’ disease | PTU | 1 month |
| 4 | Loh and Tan19 | 48 | M | Graves’ disease | RAI | Unknown |
| 5 | Chen et al 20 | 36 | F | Unknown | Unknown | 4 days |
| 6 | Hegazi et al 21 | 43 | F | Graves’ disease | Unknown | Unknown |
| 7 | Akoum et al 22 | 65 | F | Toxic multinodular goitre | Carbimazole | 2 months |
| 8 | Lima et al 11 | 71 35 39 18 |
M F M F |
Graves’ disease Graves’ disease Graves’ disease Graves’ disease |
RAI Methimazole Methimazole Methimazole |
1 month 6 months 3 months >1 year |
| 9 | Kebapcilar et al 23 | 53 | F | Graves’ disease | PTU | |
| 10 | Shaw and Mehta24 | 46 | M | Graves’ disease | Carbimazole | Few weeks |
| 11 | Soeki et al 25 | 49 | M | Graves’ disease | Methimazole | 3 months |
| 12 | Burns and Burns8 | Graves’ disease | ||||
| 13 | Ladwig et al 26 | 25 | F | Graves’ disease | PTU | Lost to follow-up |
| 14 | Talansky et al 27 | 48 | F | Graves’ disease | RAI | 10 months |
RAI, radioiodine ablation; PTU, propylthiouracil.
Pancytopenia is a rare but reported complication of hyperthyroidism. It is due to either decreased production of haemopoietic cells or increased destruction by immunological mechanisms or hypersplenism. As shown in the literature, Graves’ disease is the most cause of hyperthyroidism associated with pancytopenia. Achieving euthyroidism regardless of the modality resolves the pancytopenia in most of the cases. It should also be noted that in a majority of the cases the pancytopenia was noted before the diagnosis of hyperthyroidism was made emphasising the importance of performing thyroid function tests in evaluation of pancytopenia.
Learning points.
Hyperthyroidism can be associated with haematological abnormalities (leucopenia, anaemia, thrombocytopenia and pancytopenia) and therefore a complete blood count (CBC) evaluation should be obtained at diagnosis before giving antithyroid medications.
Thionamides can be safely given in hyperthyroidism-induced pancytopenia; however, close monitoring with CBC is warranted.
Most of the haematological abnormalities normalise with the treatment of hyperthyroidism.
In evaluation of unexplained pancytopenia, thyroid evaluation needs to be considered.
Footnotes
Contributors: VVG and SS were involved in writing the manuscript. LY-C was involved in writing the discussion section and editing the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Melmed S, Polonsky K, Larsen P, et al. Williams textbook of endocrinology. 12th ed Philadephia: Elsevier, 2011:362–368. [Google Scholar]
- 2.Braverman LE, Utiger RD. Werner and ingbar’s The thyroid; a fundamental and clinical text. 7th ed Philadelphia: PA: Lippincott-Raven:637–42. [Google Scholar]
- 3.Das KC, Mukherjee M, Sarkar TK, et al. Erythropoiesis and erythropoietin in hypo- and hyperthyroidism. J Clin Endocrinol Metab 1975;40:211–20. 10.1210/jcem-40-2-211 [DOI] [PubMed] [Google Scholar]
- 4.Miller LD, Sugarman HJ, Miller WW, et al. Increased peripheral oxygen delivery in thyrotoxicosis: role of red cell 2, 3-diphosphoglycerate. Ann Surg 1970;172:1051–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boitard C, Anciaux-Lespine ML, Eugène C, et al. Anémie et microcytosis au cours de la maladie de Basedow. Discussion physio-pathologique. Nouv Presse Med 1979;8:499–502. [PubMed] [Google Scholar]
- 6.Klein M, Weryha G, Kaminsky P, et al. Les manifestations hèmatologiques des hyperthyroidies. Ann Med Interne 1993;144:127–35. [PubMed] [Google Scholar]
- 7.Lahtinen R. Sideroblasts and haemosiderin in thyrotoxicosis. Scand J Haematol 1980;25:237–43. 10.1111/j.1600-0609.1981.tb01395.x [DOI] [PubMed] [Google Scholar]
- 8.Burns RW, Burns TW. Pancytopenia due to vitamin B12 deficiency associated with Graves' disease. Mo Med 1996;93:368–72. [PubMed] [Google Scholar]
- 9.Hegazi MO, Ahmed S. Atypical clinical manifestations of graves' disease: an analysis in depth. J Thyroid Res 2012;2012:1–8. 10.1155/2012/768019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas D, Moisidis A, Tsiakalos A, et al. Antithyroid drug-induced aplastic anemia. Thyroid 2008;18:1043–8. 10.1089/thy.2008.0097 [DOI] [PubMed] [Google Scholar]
- 11.Lima CS, Zantut Wittmann DE, Castro V, et al. Pancytopenia in untreated patients with Graves' disease. Thyroid 2006;16:403–9. 10.1089/thy.2006.16.403 [DOI] [PubMed] [Google Scholar]
- 12.Eakin DL, Peake RL, Weiss GB. Effect of therapy on the neutropenia of hyperthyroidism. South Med J 1983;76:335–7. 10.1097/00007611-198303000-00017 [DOI] [PubMed] [Google Scholar]
- 13.Weitzman SA, Stossel TP, Harmon DC, et al. Antineutrophil autoantibodies in Graves' disease. Implications of thyrotropin binding to neutrophils. J Clin Invest 1985;75:119–23. 10.1172/JCI111663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakamura H, Miyauchi A, Miyawaki N, et al. Analysis of 754 cases of antithyroid drug-induced agranulocytosis over 30 years in Japan. J Clin Endocrinol Metab 2013;98:4776–83. 10.1210/jc.2013-2569 [DOI] [PubMed] [Google Scholar]
- 15.Hymes K, Blum M, Lackner H, et al. Easy bruising, thrombocytopenia, and elevated platelet immunoglobulin G in Graves' disease and Hashimoto’s thyroiditis. Ann Intern Med 1981;94:27–30. 10.7326/0003-4819-94-1-27 [DOI] [PubMed] [Google Scholar]
- 16.Garcia J, França L, Ellinger V, et al. Marrow hypoplasia: a rare complication of untreated Grave’s disease. Arq Bras Endocrinol Metabol 2014;58:953–7. 10.1590/0004-2730000003216 [DOI] [PubMed] [Google Scholar]
- 17.Jha P, Singh YP, Ghimire B, et al. Pancytopenia in a surgical patient, a rare presentation of hyperthyroidism. BMC Surg 2014;15:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Imai K, Ohkuchi A, Nagayama S, et al. Pancytopenia in the first trimester: An indicator of hidden hyperthyroidism. J Obstet Gynaecol Res 2015;41:1991–4. 10.1111/jog.12804 [DOI] [PubMed] [Google Scholar]
- 19.Loh HH, Tan F. Pancytopenia in a Patient with Grave’s Disease. Med J Malaysia 2013;68:372–3. [PubMed] [Google Scholar]
- 20.Chen YH, Lin HJ, Chen KT. Rare presentations of hyperthyroidism--Basedow’s paraplegia and pancytopenia. Am J Emerg Med 2009;27 258.e1–258.e2. 10.1016/j.ajem.2008.06.038 [DOI] [PubMed] [Google Scholar]
- 21.Hegazi M, Kumar R, Bitar Z, et al. Pancytopenia related to Graves' disease. Ann Saudi Med 2008;28:48–9. 10.4103/0256-4947.51769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akoum R, Michel S, Wafic T, et al. Myelodysplastic syndrome and pancytopenia responding to treatment of hyperthyroidism: peripheral blood and bone marrow analysis before and after antihormonal treatment. J Cancer Res Ther 2007;3:43–6. 10.4103/0973-1482.31972 [DOI] [PubMed] [Google Scholar]
- 23.Kebapcilar L, Yeşil S, Bayraktar F, et al. Recovery from pancytopaenia and liver dysfunction after administration of propylthiouracil for Graves' disease. N Z Med J 2005;118:U1615. [PubMed] [Google Scholar]
- 24.Shaw B, Mehta AB. Pancytopenia responding to treatment of hyperthyroidism: a clinical case and review of the literature. Clin Lab Haematol 2002;24:385–7. 10.1046/j.1365-2257.2002.00460.x [DOI] [PubMed] [Google Scholar]
- 25.Soeki T, Tamura Y, Kondo N, et al. A case of thyrotoxicosis with pancytopenia. Endocr J 2001;48:385–9. 10.1507/endocrj.48.385 [DOI] [PubMed] [Google Scholar]
- 26.Ladwig P, Coles R, Fischer E, et al. Thyrotoxicosis in pregnancy presenting as pancytopenia. Aust N Z J Obstet Gynaecol 1995;35:457–60. 10.1111/j.1479-828X.1995.tb02168.x [DOI] [PubMed] [Google Scholar]
- 27.Talansky AL, Schulman P, Vinciguerra VP, et al. Pancytopenia complicating Graves' disease and drug-induced hypothyroidism. Arch Intern Med 1981;141:544–5. 10.1001/archinte.1981.00340040140037 [DOI] [PubMed] [Google Scholar]