Abstract
Although many new anti-infectives have been discovered and developed solely using phenotypic cellular screening and assay optimization, most researchers recognize that structure-guided drug design is more practical and less costly. In addition, a greater chemical space can be interrogated with structure-guided drug design. The practicality of structure-guided drug design has launched a search for the targets of compounds discovered in phenotypic screens. One method that has been used extensively in malaria parasites for target discovery and chemical validation is in vitro evolution and whole genome analysis (IVIEWGA). Here, small molecules from phenotypic screens with demonstrated antiparasitic activity are used in genome-based target discovery methods. In this Review, we discuss the newest, most promising druggable targets discovered or further validated by evolution-based methods, as well as some exceptions.
Keywords: malaria, phenotypic screening, selections, resistance
Target Discovery: On the Road to Malaria Eradication
Malaria is the most prevalent parasitic disease in man. The World Health Organization (WHO) estimated 216 million cases and 445 000 deaths in 2016 globally, out of which 91% were in Africa alone and 99% were due to Plasmodium falciparum infections (WHO, World Malaria Report 2017). Most deaths occur in children under the age of five.
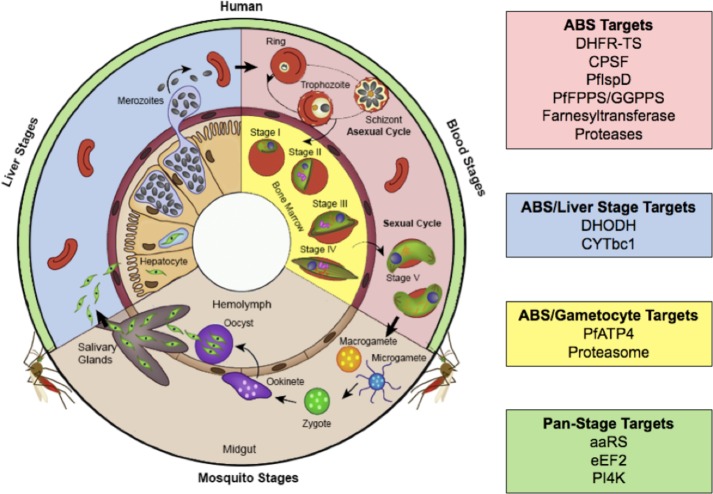
Malaria in humans is caused by 6 different species of Plasmodium, where P. falciparum causes the deadliest form of infection and P. vivax is the most widespread (WHO, World Malaria Report 2017). Plasmodium infection of the human host begins with the transmission of the parasite through the bite of an infected mosquito (Figure 1). Parasites immediately travel through the bloodstream, invade hepatocytes, and replicate asexually, resulting in thousands of merozoites. In P. vivax and P. ovale, sporozoites might form “hypnozoites”, a dormant form, which can be activated weeks to months later and cause relapse of infection. The exoerythrocytic cycle in liver transcends into the intraerythrocytic stage with asexual replication in red blood cells. The lysis of red blood cells to release more parasites causes the symptomatic disease and can be fatal.1 Some intraerythrocytic stage parasites can develop into “gametocytes”, the sexual stage, that can subsequently be transmitted into the mosquito to perpetuate the infection cycle.
Figure 1.
Plasmodium life cycle with chemically validated targets for chemotherapeutic intervention divided by the stages in which they have demonstrated antimalarial activity. Adapted with permission from Nilsson, S. K., Childs, L. M., Buckee, C., and Marti, M. (2015) Targeting Human Transmission Biology for Malaria Elimination. PLoS Pathog.11 (6), e1004871. DOI: 10.1371/journal.ppat.1004871 (ref (200)). Copyright 2015 Nilsson et al.
Artemisinin combination therapy (ACT) is the first line of treatment for uncomplicated falciparum malaria. To mitigate issues with their short half-lives and help avoid development of drug resistance, artemisinin (ART) derivatives are administered with partner drugs such as amodiaquine, piperaquine, lumefantrine, mefloquine, sulphadoxine–pyrimethamine, and pyronaridine, which have separate mechanisms of action and potentially different half-lives. The emergence of parasites showing resistance to ACTs in the Greater Mekong region could bring about a reversal in malaria control and undermine the feasibility of elimination, as has been reviewed previously.2,3 For this reason, the consensus in the medical and scientific community is that there is a great need for the development of new classes of antimalarial medicines if malaria elimination is to be achieved.4 The ideal drug would target multiple stages of the parasite’s life cycle, block or prevent transmission, or act against Plasmodium vivax liver hypnozoites. Because there are very few known drug targets, a major focus of the past decade has been the search for novel, chemically validated targets that can be starting points for development of next-generation antimalarials.
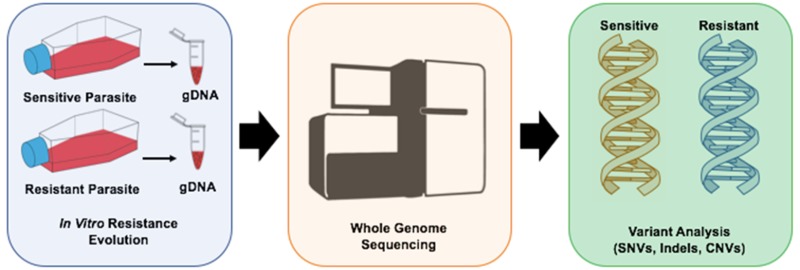
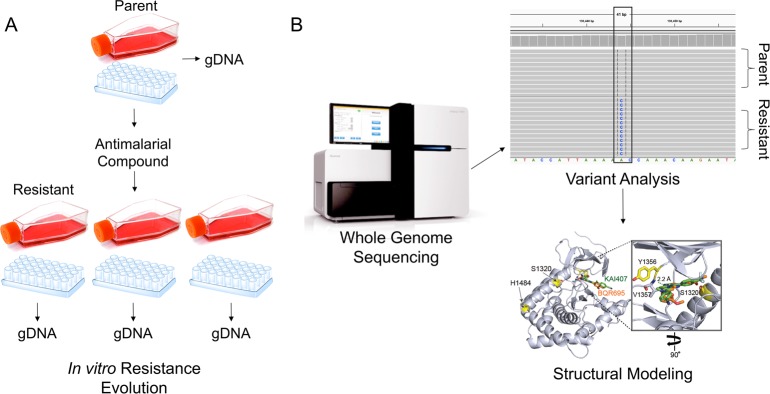
A method that has been used with great success to find new drug targets is in vitro evolution and whole genome analysis (IVIEWGA). In this method (Figure 2), parasites are exposed to sublethal concentrations of compounds that have shown antiparasitic activity. These compounds typically are identified in phenotypic screens, and some are active throughout the parasite lifecycle. To identify the genetic basis of their resistance, the genomes of the resistant clones are analyzed using tiling microarrays or more typically using whole genome sequencing (WGS) and are compared to the sensitive parent clone. In many cases, newly emerged genomic lesions are found in genes that are predicted to encode the targets. Modeling, crystallography, and further functional studies can confirm that the gene product is the actual target and resistance is not conferred nonspecifically by a multidrug resistance gene (e.g., a transporter that is frequently observed). The advantage of targets discovered through this method is that they are, by default, chemically validated and druggable, though complementary studies may be needed to further validate the targets and their clinical relevance. This Review discusses some of the many new drug targets (Table 1) that have been discovered or reconfirmed using this method.
Figure 2.
Overview of IVIEWGA process. (A) A clonal aliquot (obtained by limiting dilution in a microtiter plate) of a sensitive parent P. falciparum strain is cultured in triplicate and subjected to the selective pressure of an antimalarial compound using a slow ramping or pulse method. Upon successful generation of resistant parasite bulk cultures, clones are isolated using limiting dilution and retested for resistance. (B) Whole genome sequencing is performed using gDNA extracted from the parent and resistant clones. Bioinformatic analysis calls variants between the parent and resistant lines to determine which mutations confer resistance. Generally, mutations that arise in multiple, independently derived clones are prioritized for further validation, which may include structural modeling, molecular docking simulations, and/or reverse genetics techniques.
Table 1. Chemically Validated Targets for Plasmodium falciparum.
| drug target | inhibitor | references |
|---|---|---|
| PfATP4 | KAE609 (Cipargamin), GNF-Pf-4492, PA21A092, SJ733 | (6, 8, 11, 12) |
| aminoacyl-tRNA sythetases | (18−20, 22, 27, 29) | |
| prolyl-tRNA synthetase | febrifugine, halofuginone | |
| lysyl-tRNA sythetase | cladosporin | |
| isoleucyl-tRNA synthetase | mupirocin, thiaisoleucine | |
| phenylalynyl-tRNA sythetase | BRD1095 | |
| threonyl-tRNA sythetase | borrelidin | |
| tryptophanyl-tRNA synthetase | indolmycin | |
| translation elongation factor 2 | DDD107498 | (38) |
| dihydroorotate dehydrogenase | DSM265, DSM421, DSM1, DSM74, Genz-669178, Genz-666136, BRD7539, BRD9185 | (20, 42, 43, 45, 50) |
| cytochrome bc1 | atovaquone, decoquinate, tetracyclic benzothiazepine, GW844520, GSK932121 | (51, 53) |
| dihydrofolate reductase-thymidylate synthase | pyrimethamine, cycloguanil, MMV027634 | (58) |
| phosphatidylinositol 4-kinase | KDU691, MMV390048, KAI407, BQR695, BRD73842 | (8, 56, 62, 99) |
| cleavage and polyadenylation specificity factor | AN3661 | (63) |
| isoprenoid biosynthesis | fosmidomycin, MMV008138, MMV019313 | (67, 69, 70) |
| farnesyltransferase | BMS-388891, MMV019066 | (58) |
| proteasome inhibition | bortezomib, carfilzomib, carmaphycin B, WLL-vs | (84, 86) |
| proteases | (101, 102, 104) | |
| aspartic proteases | ||
| plasmepsin I, II, IV | 2-aminoquinazolin-4(3H)-ones | |
| plasmepsin V | aminohydantoins | |
| cysteine protease | WEHI-842, WEHI-916 | |
| metalloprotease | actinonin |
P. falciparum P-Type Cation ATPase
One of the first novel targets that was discovered with IVIEWGA was PfATP4, a P. falciparum p-type cation ATPase. It was first identified as the target of the spiroindolone compound, KAE609 (also called NITD609), which is now commercially called Cipargamin.5 KAE609 is highly active against both blood-stage P. falciparum and P. vivax field isolates and culture-adapted isolates with single-digit nanomolar IC50s.6 It is also active against gametocyte and oocyst development in mosquitoes which would enable this compound to block transmission. Parasites generated from in vitro resistance evolution using KAE609 and analyzed with microarrays display both copy number variants (CNVs) and single nucleotide variants (SNVs) in various positions of PfATP4 (Table 2). These mutations were later proven to confer resistance in P. falciparum and result in at least a 10-fold increase in IC50 values.6,7 KAE609 has progressed through Phase I and IIa clinical trials,5 and it remains to be seen how far it will advance in drug development.
Table 2. Drug Target Mutations Observed in P. falciparum IVIEWGA Studiesa.
| drug target | inhibitor | gene ID | mutations |
|---|---|---|---|
| PfATP4 | KAE609 | PF3D7_1211900 | Asp1247Tyr; Pro990Arg; Thr418Asn; Ile398Phe |
| GNF-Pf-4492 | Ala211Thr; Ile203Leu; Pro990Arg; Ala187Val | ||
| PA21A092 | Val178Ile | ||
| SJ733 | Val415Asp; Leu350His; Pro412Thr; Pro966Ser; Pro966Thr | ||
| aaRs | thiaisoleucine | PF3D7_1332900 | Leu810Phe |
| mupirocin | PF3D7_1225100 | Pro1233Ser | |
| cladosporin | PF3D7_1350100 | amplification | |
| halofuginone | PF3D7_1213800 | Leu482His; Leu482Phe | |
| BRD1095 | PF3D7_0109800 | Leu550Val; Met316Ile; Gly512Glu; Val545Ile | |
| eEF2 | DDD107498 | PF3D7_1451100 | Glu134Gly; Glu134Asp; Tyr186Asn; Ala482Thr; Ile183Thr; Thr185Ile; Pro754Ala; Pro754Ser; Leu755Phe; Ser474Arg |
| DHODH | DSM1 | PF3D7_0603300 | amplification |
| DSM74 | Glu182Asp; Leu531Phe | ||
| DSM265 | Gly181Cys | ||
| Genz-669178 | Phe188Ile; Phe188Leu | ||
| Genz-666136 | Glu182Asp; Phe227Ile | ||
| Cytbc1 | atovaquone | mal_mito_3 | Met133Val; Met133Ile; Leu144Ser; Phe267Val |
| decoquinate | Ala122Thr; Tyr126Cys | ||
| tetracyclic benzothiazepine | Gly131Ser; Phe264Leu | ||
| DHFR-TS | MMV027634 | PF3D7_0417200 | Gly378Glu; Ile403Leu; His551Asn |
| PI4K | KAI407 | PF3D7_0509800 | His1484Tyr |
| BQR695 | Ser1320Leu; Tyr1356Phe | ||
| CPSF | AN3661 | PF3D7_1438500 | Thr406Ile; Tyr408Ser; Thr409Ala; Asp470Asn; His36Tyr |
| PfDXR | fosmidomycin | PF3D7_1467300 | amplification |
| PfIspD | MMV008138 | PF3D7_0106900 | Glu688Gln; Leu244Ile |
| PfFPPS/GGPPS | MMV019313 | PF3D7_1128400 | Ser228Thr |
| farnesyltransferase | BMS-388891 | PF3D7_1147500 | Asn315Y; Gly612Ala |
| MMV019066 | Ala515Val; Ala515Thr |
Although there are concerns that PfATP4 could be involved in multidrug resistance,8 it is generally accepted to be a good drug target. All cells must maintain low cytosolic Na+ concentration to survive, and PfATP4 mediates active extrusion of Na+ from the parasite to maintain low-[Na+]/high-[K+] in the host cell cytosol upon infection.9 PfATP4 is found in the Plasmodium plasma membrane, and the gene is expressed in all asexual blood stages of Plasmodium.7 PfATP4 has been suggested to be the mechanism of action for multiple potential antimalarial candidates which have been shown to disturb Na+ regulation and homeostasis in the parasite.7,10
Shortly after the discovery that PfATP4 was the target of the spiroindolones, evolution studies showed that it was involved in resistance to several other compound classes, including the aminopyrazoles, pyrazoleamides, and dihydroisoquinolones, all compounds identified by phenotypic screening.8,11,12 Like spiroindolones, aminopyrazoles target both the asexual blood stages of the parasite and oocyst formation in mosquitoes, thus preventing transmission of the parasite. Mutations in PfATP4 acquired after treatment with the aminopyrazole GNF-Pf-4492 also confer resistance to spiroindolones. PfATP4 mutations found in resistant parasite lines treated with either small molecule are present in the region of the predicted transmembrane (TM) domain, suggesting they might exhibit a shared structure–function relationship. One of the selections also yielded a point mutation in the putative ADP/ATP transporter protein (PF3D7_1037300) localized to the inner mitochondrial membrane, which may be a compensatory mutation.5
Like all other PfATP4 inhibitors, pyrazoleamides kill both P. falciparum asexual laboratory isolates and P. falciparum and P. vivax field isolates, at very low nanomolar IC50 values. In addition, the lead compound PA21A092 inhibits gametocyte development similar to KAE609.12 PA21A092 enables rapid increase in cytosolic Na+, and since it does not affect resting cytosolic Ca2+ levels, the parasites swell due to the osmotic uptake of water.12
The dihydroisoquinolone SJ733 also originated with a cellular screen. Selections with SJ733 resulted in resistant parasite lines that displayed an IC50 increase of 2- to 750-fold, and WGS detected mutations in PfATP4 not seen previously in KAE609-resistant lines. Despite the different location of the mutations, SJ733-resistant lines are cross-resistant to spiroindolones.11 SJ733 causes an increase in the parasite’s cytosolic Na+ level and concurrent alkalinization of the cytosol which seems in line with the loss of PfATP4 activity.11 The overrepresentation of PfATP4 inhibitors in many phenotypic screens may be because PfATP4 is a high-value target whose inhibition results in rapid death, even at low inhibitor concentrations.11 Additionally, its localization to the parasite plasma membrane may make it a more accessible target since membrane permeability of inhibitors would not be necessary for drug efficacy. Despite its significance, no crystal structure of PfATP4 or biochemical assay is available, and thus, there are still many open questions about how these compounds act and whether pfatp4 may also function as a resistance gene.
Aminoacyl-tRNA Synthetases
A well-known class of targets in other species, which has become increasingly relevant due to multiple discoveries using IVIEWGA in Plasmodium, is the tRNA synthetase family. During protein synthesis, aminoacyl-tRNA synthetases (aaRS) accurately pair the cognate tRNAs with their corresponding amino acids hence defining the genetic code.13 Translation fidelity is attained by two events: correct pairing of an amino acid with the matching tRNA and the accurate selection of the charged aminoacyl-tRNAs on the ribosome. Functional aspects of aaRSs and their role in keeping translational errors in check have been reviewed previously.14,15
Apicomplexan parasites have nuclear, apicoplast, and mitochondrial genomes which each require charged tRNAs for translation. To synthesize its proteome, the malaria parasite utilizes a combined array of 36 aaRSs (instead of the theoretical 60 aaRSs for the three compartments).16 Of these, 16 aaRSs are present exclusively for cytoplasm and 15 nuclear-encoded aaRSs are present exclusively for the apicoplast. The mitochondria is speculated to import charged tRNAs from the cytoplasmic tRNA pool and only harbors an enzymatically active mitochondrial phenylalanyl-tRNA synthetase, a feature unique to Plasmodium.17 There are multiple sites that can provide binding sites for small molecule inhibitors, including the editing site, aminoacylation pocket, and the tRNA binding region.13,18−20
Isoleucyl-tRNA Synthetase
The first hints that aaRSs might be important drug targets for antimalarials came from IVIEWGA studies with two known inhibitors of isoleucyl-tRNA synthetase, thiaisoleucine and mupirocin.18P. falciparum contains two isoleucyl-tRNA synthetases, one in the cytoplasm and the other in the apicoplast.21 Mupirocin, a natural product that is clinically used as an antibiotic, was found to inhibit the P. falciparum apicoplastic isoleucyl-tRNA synthetase, and the isoleucine analog, thiaisoleucine, was shown to target cytoplasmic isoleucyl-tRNA synthetase. Both compounds kill asexual blood stage parasites at mid-nanomolar and low-micromolar concentrations, respectively.18
Lysyl-tRNA Synthetase
Lysyl-tRNA synthetase was discovered as another potential important target using array-based IVIEWGA. The P. falciparum cytosolic lysyl-tRNA synthetase is selectively and specifically inhibited by a fungal secondary metabolite, cladosporin, which has potent, nanomolar activity against both blood and liver stages of the parasite.22 Cladosporin has >100-fold more potency against the parasite’s lysyl-tRNA synthetase as compared to the human ortholog. This was corroborated by other studies that observed the dissociation constant for P. falciparum lysyl-tRNA synthetase with cladosporin to be ∼14 nM, while the human lysyl-tRNA synthetase was ∼4 μM.23,24 Another study designed and tested inhibitors against apicoplast lysyl-tRNA synthetase and confirmed that the Plasmodium apicoplastic lysyl-tRNA synthetase can be specifically inhibited with compounds that show antimalarial activity in the micromolar range.25
Prolyl-tRNA Synthetase
Cytoplasmic glutamyl-prolyl tRNA synthetase activity in mammalian cells is inhibited by febrifugine, a compound derived from a Chinese herb, and its synthetic derivative halofuginone.26 However, these inhibitors could not be developed clinically because of their high toxicity. Herman and co-workers developed an analog called halofuginol that is active against both liver and asexual blood stages of the rodent malaria parasite P. berghei and is much better tolerated.19 IVIEWGA was used with halofuginone to identify prolyl-tRNA synthetase as the target.19 The group also showed that febrifugine analogs induce eukaryotic initiation factor 2α phosphorylation in both Plasmodium and transgenic yeast that express cytoplasmic prolyl-tRNA synthetase, making them important chemical tools to study the amino acid starvation pathway in both species. The importance of prolyl-tRNA synthetases as targets in multiple human eukaryotic pathogens (Plasmodium, Leishmania, Toxoplasma, Cryptosporidium, and Eimeria) is supported by the development of quinazolinone inhibitors using structure-guided drug design.27
Phenylalanyl-tRNA Synthetase
Three structurally and functionally different phenylalanyl-tRNA synthetases are present in the malaria parasite, each essential to the parasite’s translational machinery in each of its compartments.16,17 The cytoplasmic enzyme is an (αβ)2 hetrotetramer while its apicoplast and mitochondrial counterparts are monomeric.17 Kato et al. screened ∼100 000 compounds from the diversity-oriented synthesis (DOS) library against P. falciparum and identified a series of bicyclic azetidines, which were then shown to inhibit the phenylalanyl-tRNA synthetase following in vitro evolution. These compounds showed activity at a single low-concentration dose in mice against all life cycle stages of the parasite.20 This seems to be a very promising new drug target due to its presence in all three translational compartments in the parasite.
Dual tRNA Synthetase Targets
Although in vitro evolution has been often used to assign specific inhibitors to tRNA synthetase targets in an unbiased manner, data from other species can create testable hypotheses about which tRNA synthetase might be inhibited. Biochemical evidence from E. coli has indicated that indolmycin inhibits tryptophanyl-tRNA synthetase,28 leading to the testable hypothesis that it behaves similarly in P. falciparum.29 Likewise, borrelidin is a bacterial secondary metabolite with known antimalarial properties.30 Characterization of borrelidin-resistant mutants in Escherichia coli showed that tolerance resulted from ThrRS (encoding threonyl-tRNA synthetase) overexpression.31 Threonyl-tRNA (as with alanyl-, glycyl-, and cysteinyl-tRNA) synthetase is a very interesting potential target due to its dual localization in both cytosol and apicoplast. Targeting this enzyme would theoretically stall translation in all three compartments.21,32,33 On the other hand, borrelidin also inhibits human threonyl-tRNA synthetase, making it highly toxic. To overcome this, a library of borrelidin analogs was synthesized and tested for toxicity and antimalarial activity. Some analogs lost their toxicity to human cells and still maintained antiparasitic activity both in vitro and in vivo when tested in mice against P. yoelii.34 Although several of these analogs inhibited P. falciparum threonyl-tRNA synthetase in aminoacylation assays, it is theoretically feasible that these compounds exert their antiparasitic activity through interaction with a different target. The use of in vitro evolution studies can provide unbiased confirmation of on-target activity for threonyl and tryptophanyl tRNA synthetase.
Translation Elongation Factor 2
Previous studies have implicated translation elongation factor 2 (eEF2) as an important drug target in Saccharomyces cerevisiae for the antifungal compound sordarin.35,36 Eukaryotic protein synthesis requires several elongation factors, and eEF2 is responsible for the translocation of the ribosome along the mRNA. Yeast studies have demonstrated that selective inhibitors for eEF2 can be synthesized that would not inhibit protein synthesis in human cells.36,37
IVIEWGA was used to show that P. falciparum eEF2 is inhibited by compound DDD107498. This compound has high potency and, like the tRNA synthetase inhibitors, antimalarial activity against multiple stages of the parasite’s life cycle.38 In a recent study, DDD107498 was confirmed to have transmission-blocking activity in experimental mosquito models using parasite densities observed in natural infections, supporting the decision to move this compound into early stage clinical trials.39 The identification of inhibitors for tRNA synthetases and translation elongation factors clearly demonstrate that targeting protein synthesis in Plasmodium is a very effective way for attaining multistage antiparasitic activity.
Dihydroorotate Dehydrogenase
Dihydroorotate dehydrogenase (DHODH) was already known to be a promising target for the development of antimalarial chemotherapy but has been rediscovered using evolution-based methods. DHODH is an enzyme localized to the mitochondrial electron transport chain (mETC), which provides oxidized ubiquinone as an electron acceptor for DHODH to synthesize pyrimidines de novo.40,41 The parasite cannot salvage pyrimidines from its host, so the activity of the mETC is essential.42 DHODH can be considered a good potential drug target with low toxicity due to the differences in the active site across species. Selective inhibitor binding with triazolopyrimidines in Plasmodium was first shown by Phillips and Rathod.42
A later triazolopyrimidine derivative, DSM265, has now advanced to Phase II clinical trials and is active against both liver and asexual blood stages of the parasite.43 It has promising efficacy with single-dose regimens in human trials.44 A secondary derivative, DSM421, has a similar selectivity and potent antimalarial activity.45 In addition, 5-benzimidazolyl-theophene-2-carboxamides46 and 7-arylaminopyrazolo[1,5-α]pyrimidines47 have also been shown to inhibit DHODH. In vitro evolution with DSM1, a scaffold related to DSM265, has shown that P. falciparum acquires copy number variants that encompass the DHODH loci, providing further in vivo validation of the target.48
Growth inhibition phenotypic screening identified many compounds with multistage activity against Plasmodium using diversity oriented synthesis.20 BRD7539, an azetidine-2-carbonitrile, has been shown to inhibit DHODH in P. falciparum selectively over human DHODH and is potent against the parasite’s asexual blood and liver stages. An optimized compound, BRD9185, has in vitro activity against blood and liver stage parasites and can clear infection in mouse models in just three doses.49 This class of compounds is another promising group of potential new antimalarials that target DHODH.
Ross and co-workers showed that resistance to PfDHODH inhibitors is primarily due to mutations and amplifications of the target gene DHODH. Several point mutations were found along with gene amplification that contributed to resistance. They also showed that the mutant parasites were sensitive to other PfDHODH inhibitors (Genz-669178, Genz-666136, and DSM74) which suggests a novel combination therapy approach to prevent resistance.50
Cytochrome bc1 Complex
The cytochrome bc1 complex (ubiquinol/cytochrome c oxidoreductase; complex III) is another target localized in the mETC and was previously known to be inhibited by drugs used in the treatment of malaria and toxoplasmosis. The dimeric cytochrome bc1 protein is comprised of three catalytic subunits: cytochrome b, cytochrome c1, and the Rieske iron–sulfur protein. The cytochrome bc1 complex catalyzes the transfer of electrons from ubiquinol to cytochrome c and, in P. falciparum, plays a very important role in pyrimidine biosynthesis by providing oxidized ubiquinone to DHODH.40 Cytochrome bc1 is the target of atovaquone (which is combined with proguanil in the antimalarial drug, Malarone), a hydroxynapthoquinone which is a competitive inhibitor of the Qo site.
The importance of cytochrome bc1 as an antimalarial target was first reconfirmed using IVIEWGA and decoquinate, a compound with low nanomolar activity against P. yoelii liver stage and P. falciparum blood stages.51 Analysis of decoquinate-resistant lines revealed two new cytochrome bc1 mutations, A122T and Y126C, were present in the evolved lines and that these mutations mapped to the Qo binding pocket of cytochrome bc1.51 Although both atovaquone and decoquinate interact in the ubiquinol binding site of the cytochrome bc1 complex, each compound adopts a different mode of binding as has been shown by molecular docking studies and identification of different mutations in the respective resistant lines.52 There is very limited cross-resistance with decoquinate in atovaquone-resistant lines.51 At about the same time, a G131S mutation in the Qo quinol binding site in resistant evolved lines was detected after selection with tetracyclic benzothiazepines, a compound class discovered in a phenotypic screen. In this case, however, only the cytochrome bc1-encoding gene was amplified and sequenced.53
Not much is known about the Qi binding site of cytochrome bc1 with respect to the interaction of its inhibitors. Recent studies have suggested that antimalarial compounds like 1-hydroxy-2-dodecyl-4(1H)quinolone bind to this site and are even effective against atovaquone-resistant strains with known Qo mutations.54 X-ray crystallography studies later provided evidence that 4(1H)-pyridone compounds GW844520 and GSK932121 bind to the Qi site of cytochrome bc1 complex and overcome atovaquone resistance.55 IVIEWGA also established that the quinolone reduction site (Qi site) of cytochrome bc1 is a druggable target using an antimalarial probe from the DOS library that lacks cross-resistance with Qo site inhibitors like atovaquone.56 The presence of two different active sites in the same enzyme indicates that cytochrome bc1 is a very promising drug target. Furthermore, the absence of cross-resistance between inhibitors targeting these two sites can be harnessed for development of effective combination therapies.
Thymidylate Synthase Portion of Bifunctional Dihydrofolate Reductase-Thymidylate Synthase
Dihydrofolate reductase-thymidylate synthase (DHFR-TS) is a very well-established drug target in P. falciparum for antifolates such as pyrimethamine and cycloguanil. This bifunctional enzyme is essential in the production of folates and thymidylate, which are crucial for DNA synthesis.57 Although many antimalarials inhibit the DHFR portion of this bifunctional enzyme, a recent study evolved resistant parasites against the benzoquinazolinone MMV027634 and identified 3 nonsynonymous mutations in the TS portion. A previously published crystal structure allowed the mapping of these novel mutations to the active TS binding site of the protein, revealing that each mutation occurs on the fringe of the 2′-deoxyuridylic acid (dUMP) binding site.58
Understanding the role of the junctional region of DHFR-TS could prove useful in antimalarial drug development, since it has been shown that a critical length of this junctional region (at least 44 amino acids) is essential for the P. falciparum TS domain to be catalytically active.59 Exploiting the junctional region of this multifaced enzyme would simultaneously inhibit other portions of DHFR-TS enzyme to overcome drug resistance.
Phosphatidylinositol 4-Kinase
Another target discovered using IVIEWGA is phosphatidylinositol 4-kinase (PI4K). This important new antimalarial drug target operates in all stages of the Plasmodium life cycle. PI4K is an essential cellular regulatory molecule, conserved in all eukaryotes that phosphorylate lipids (phosphatidylinositol to PI4-phosphate) to regulate intracellular signaling and trafficking.60 In Plasmodium, PI4-P recruits lipid-binding effector proteins that are driven by Rab11A for the late-stage membrane ingression during merozoite biogenesis.61
PI4K was first discovered as the target of imidazopyrazines, a new class of antimalarial molecule that shows potency against blood-stage field isolates of P. falciparum and P. vivax. Imidazopyrazines such as KDU691 demonstrate therapeutic, preventive, and transmission-blocking activity in the malaria parasite by altering PI4-phosphate levels and membrane trafficking.61 Selections with analogs of KDU691 (KAI407, KAI715, and BQR695) yielded both CNVs and SNVs in PI4K, confirming it as the target of this compound class.58
Subsequent phenotypic screens have identified other PI4K inhibitors. MMV390048, a 2-aminopyridine, also inhibits the PI4K enzyme, although this was discovered using affinity chromatography. Strains resistant to other antimalarials are sensitive to MMV390048, and it has activity against all stages of the parasite life cycle except hypnozoites.62 Another compound, BRD73842, has activity in all stages of the parasite life cycle and was discovered in the DOS library discussed above.20 It is notable that all three are structurally quite different from one another (Figure 3).
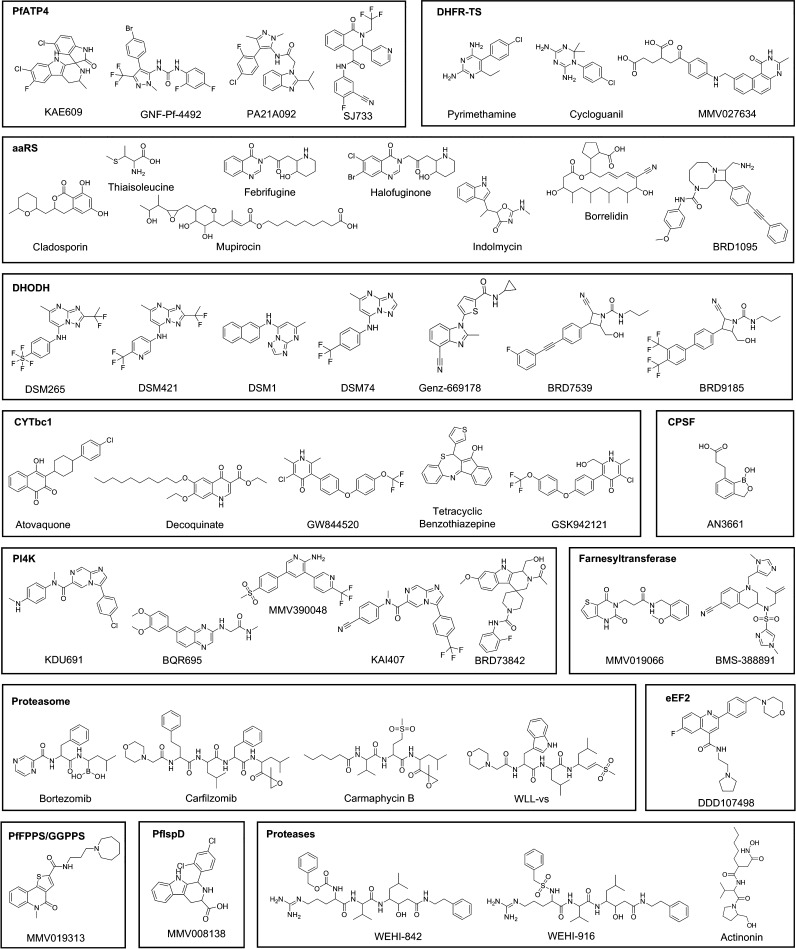
Figure 3.
Antimalarial compounds grouped by targets as determined or supported by IVIEWGA studies. References are given in Table 1. SMILES for each compound are given in Table S1.
Cleavage and Polyadenylation Specificity Factor Subunit 3
Cleavage and polyadenylation specificity factor (CPSF) is a multiprotein complex present in all eukaryotic cells that plays an important role in processing pre-mRNA to mRNA by cleavage and polyadenylation at the 3′ end of pre-mRNA.63 CPSF was discovered to be a promising antimalarial drug target when point mutations were found in P. falciparum lines resistant to the small molecule AN3661, a benzoxaborole. Homology modeling studies showed the mutations were located in the active site where AN3661 binds to the protein. This compound was found to be highly potent against multiple stages of the parasite’s life cycle in vitro, indicating further efforts should be made to design inhibitors that target CPSF.63
Isoprenoid Pathway
The isoprenoid biosynthesis pathway is essential in Plasmodium and occurs via the methyl-d-erythritol-4-phosphate (MEP) pathway. Isoprenoids are essential for protein prenylation and the synthesis of ubiquinone, dolichols, carotenoid, and vitamin E; tRNA prenylation has also been shown to be dependent on the isoprenoid pathway, making this pathway an attractive target for the development of new antimalarial therapies.64−66 The first successful application of the IVIEWGA method to identify an antimalarial target attributed acquired fosmidomycin resistance to copy number variation in the pfdxr gene, which is involved in the isoprenoid biosynthesis pathway.67 More recently, IVIEWGA using small molecules from the MMV Malaria Box, a library of 400 diverse drug- and probe-like molecules,68 has identified multiple targets of this pathway, which will be discussed below.
P. falciparum 2-C Methyl-d-erythritol 4-Phosphate Cytidylyltransferase
P. falciparum 2-C methyl-d-erythritol 4-phosphate cytidylyltransferase (PfIspD) is a key enzyme in the MEP isoprenoid biosynthesis pathway and was identified as the target of MMV008138 from the MMV Malaria Box. In vitro selections with MMV008138 followed by whole genome sequencing of drug-resistant parasites identified E688Q and L244I mutations to confer resistance.69 The MEP pathway is not functionally conserved in humans, but an orthologous enzyme is expressed. The human ISPD shows only very weak sequence similarity to PfIspD, so antimalarials developed for this target should display low toxicity.
Bifunctional Farnesyl/Geranylgeranyl Diphosphate Synthase
IVIEWGA using MMV019313 from the MMV Malaria Box68 identified a SNV, S228T, in the P. falciparum bifunctional farnesyl and geranylgeranyl diphosphate synthase (PfFPPS/GGPPS) that conferred resistance.70 PfFPPS/GGPPS synthesizes C15 and C20 prenyl chains for multiple downstream enzymes in the isoprenoid biosynthesis pathway. Bisphosphonates used for the treatment of osteoporosis also target PfFPPS/GGPPS and were shown previously to clear Plasmodium parasites in a mouse model, validating this enzyme as an antimalarial drug target. MMV019313 represents the first nonbisphosphonate inhibitor of PfFPPS/GGPPS and demonstrates superior physicochemical properties. It is highly selective for the Plasmodium FPPS/GGPPS and showed no activity against human FPPS or GGPPS.
Notably, Gisselberg et al. had to employ chemical mutagenesis with the alkylating agent ethylmethanesulfonate (EMS) in their selections to facilitate resistance evolution after multiple unsuccessful attempts to identify resistant strains using a standard protocol.70 This represents a useful alternative strategy for resistance evolution when traditional IVIEWGA methods fail.
Farnesyltransferase
An important post-translational event in eukaryotic organisms is the prenylation of proteins, which allows for protein–protein interactions and binding of intracellular proteins to membranes. One key process is the farnesylation of proteins, driven by farnesyltransferase. This enzyme catalyzes the transfer of the farnesyl group, a 15-carbon isoprenoid lipid unit, from farnesyl pyrophosphate to the C-terminus of proteins containing the CaaX motif.71 Farnesyltransferase is an interesting known potential drug target in P. falciparum since the inhibition of this enzyme is fatal to the parasite.72,73 Inhibitors of the protein have also been developed into anticancer therapeutics.74,75
Previously, resistance evolution of the parasite with the farnesyltransferase inhibitor BMS-388891, a tetrahydroquinoline, showed mutations in the protein at the peptide substrate binding domain. In selections with BMS-339941, another tetrahydroquinoline, a mutation was identified in the farnesyl pyrophosphate binding pocket.76
In a very recent IVIEWGA study, two different mutations in amino acid 515 (A515 V and A515T) were found in the beta subunit of the farnesyltransferase in P. falciparum strains resistant to MMV019066, a pyrimidinedione from the MMV Malaria Box. Modeling studies revealed that the mutations distort the critical interaction site of the small molecule with the farnesylation active site, thereby conferring resistance.58
Using IVIEWGA in Other Species To Inform Antimalarial Drug Development and Target Identification
IVIEWGA data from other species can also be used to confirm likely on-target activity or to suggest new targets. In vitro evolution with Saccharomyces cerevisiae has shown that cladosporin, mentioned above, also inhibits yeast lysyl-tRNA synthase, just as it inhibits P. falciparum lysyl-tRNA synthetase.22 IVIEWGA using KAE609 showed that mutations in the orthologous yeast protein PMA1 confer resistance.77 In addition, yeast selections have been used to confirm on-target activity of proteasome inhibitors.
The proteasome is a well-known drug target important in the treatment of both infectious diseases78 and cancer.79 For example, the boronic acid inhibitor bortezomib has cytotoxic activity and is very effective in treating hematopoietic malignancies by targeting the β5 subunit.80,81 On the basis of its success in cancer drug development, researchers suspected that proteasome inhibitors could also be antimalarials if problems with specificity could be overcome. A study using affinity probes showed that, when the β2 and β5 activities are inhibited in the P. falciparum proteasome, parasite growth is inhibited in all asexual blood stages even after short treatment.82 Carfilzomib is an α′,β′-epoxyketone inhibitor used to treat refractory or relapsed multiple myeloma that also kills P. falciparum, including artemisinin-resistant strains.82,83 Later work identified WLL-vs (Trp-Leu-Leu-vinylsulfone) as a molecule that inhibits multiple subunits of the Plasmodium proteasome simultaneously while having lower activity against the human proteasome.84 When tested in a P. chabaudi infection model, WLL-vs caused a drastic reduction in the parasite burden and was well-tolerated by host cells.84 Carmaphycin B is a natural product derived from cyanobacterium Symploca sp. that targets the β5 subunit of the proteasome but exerts a cytotoxic effect on human lung adenocarcinoma and a colon cancer cell line.85 Analogs have been designed that display high antimalarial activity against both asexual blood stages and gametocytes but also low human cytotoxicity.86
Although proteasome inhibitors bind to the proteasome in in vitro assays, questions remain as to whether the proteasome is their primary target. Employing IVIEWGA in S. cerevisiae has shown that carmaphycin B targets the β5 subunit as predicted, confirming affinity profiling data and the usefulness of IVIEWGA studies across species to identify the mechanism of action of small molecule compounds.
Protease Inhibition
Although many important targets have been discovered or confirmed with IVIEWGA, several new targets have been identified using conventional reverse genetic approaches. The best examples are the proteases. Malaria parasites utilize highly evolved and specific proteolytic pathways to invade and replicate in host cells while simultaneously avoiding the host immune response. Proteases play both regulatory and effector roles in parasite egress and invasion of red blood cells (RBCs). Proteases have well-characterized active site structures and are considered good drug targets. Protease inhibitors are already used to treat various human diseases like cancer, cardiovascular disorders such as hypertension and congestive heart failure, HIV, diabetes, and osteoporosis.87,88
In malaria parasites, serine proteases are implicated in RBC deformability and cytoadhesion89 as well as in egress and RBC/hepatocyte invasion.90,91 Aspartyl proteases (plasmepsins I–V),92 cysteine proteases (falcipains 2, 2′, and 3; DPAP1),93−97 and the metalloprotease falcilysin98,99 all play an important role in hemoglobin degradation. Plasmepsin V is an essential aspartyl protease with a major role in the export of effector proteins to parasite-infected erythrocytes by cleaving proteins within the Plasmodium export element (PEXEL) in the parasite’s endoplasmic reticulum.100,101 Recent studies have shown that plasmepsin V might be an important drug target for both P. falciparum and P. vivax. Plasmepsin V is inhibited by WEHI-842, a compound designed to mimic the parasite PEXEL motif,101 and by WEHI-916, which blocks PEXEL cleavage and kills the parasite at the ring-trophozoite transition.102
Plasmepsins IX and X are another class of aspartyl proteases that have remained unexplored until recently. Plasmepsin IX is functionally involved in erythrocyte invasion, targeting the biogenesis of the rhoptry secretory organelle. Plasmepsin X is paramount in both invasion and egress and for the final processing step carried out by subtilisin-like serine protease (SUB1) in the exoneme secretory vesicles.103 Treatment with inhibitors in the aminohydantoin class resulted in an accumulation of schizonts and loss of SUB1 and SERA5 (a cysteine protease) maturation. Because inhibitors of plasmepsin X impair egress events downstream, aspartyl protease is a very promising antimalarial target.
The membrane metalloprotease FtsH1 was recently discovered as the target of the antibiotic actinonin using resistance evolution in Toxoplasma gondii after attempts to generate resistance in P. falciparum failed.104 Treatment of P. falciparum with actinonin resulted in apicoplast biogenesis defects, establishing it as a promising target for a couple of reasons. Because apicoplast biogenesis is essential in proliferative stages of the Plasmodium life cycle, inhibitors of FtsH1 may have multistage efficacy. Additionally, there may be a decreased risk of host–cell toxicity since the organelle is unique to apicomplexan parasites.105,106
The attention that proteases have received leads to questions about why they have not been identified frequently using IVIEWGA. One possibility is that protease inhibitors lack specificity and/or there is genetic redundancy in the protease family. If a compound inhibits multiple proteases simultaneously, it is possible that specific mutations would not be identified. Alternatively, mutations in protease catalytic sites could lead to nonviable parasites given the many important biological functions they carry out in the parasite life cycle.
Conclusions
The recent dramatic increase in novel druggable pathways in Plasmodium parasites has been facilitated largely by the utilization of in vitro resistance evolution combined with mutation identification through a variety of genomic techniques. The increased efficiency and declining cost of WGS has only accelerated the rate of target discovery by this approach. Nonetheless, certain challenges remain in WGS analysis. The extreme A–T richness of the P. falciparum genome presents a unique problem for standard bioinformatic analysis protocols, for example, especially within intergenic regions where polymerase chain reaction (PCR) amplification bias can severely distort depth of coverage. Additionally, alignment confidences decrease across the highly variable Plasmodium genes involved in antigenic variation. Lack of complete functional annotation across the genome is another challenge for IVIEWGA studies because potentially interesting mutations may occur in uncharacterized genes. One example of this was the identification of mutations in the uncharacterized P. falciparum cyclic amine resistance locus (PfCARL) in selections with the clinical candidate KAF156.107 As next-generation sequencing technology advances and methods of SNV and CNV detection become more sensitive, however, target discovery will become a more streamlined process. To date, the IVIEWGA method has been successfully applied to identify a number of novel antimalarial targets to expedite drug discovery. This Review highlights core druggable targets identified or further confirmed via IVIEWGA that should be integrated into the antimalarial drug development pipeline.
Genes that are identified using IVIEWGA are already chemically validated but must be further validated through structural docking studies and reverse genetics to prove their direct role in resistance. When a compound lacks strong on-target activity, mutation calls may be inconclusive or resistance may be conferred by generalized resistance mechanisms rather than a mutation in the target itself. Additionally, background and compensatory mutations that play an indirect role in resistance acquisition must be filtered out from genes that are truly relevant and druggable. While sequencing of resistant clones leads to more robust results, deep-coverage sequencing of bulk populations instead could make IVIEWGA more efficient. In a sample sequenced to 500× coverage, alleles with 1% frequency might be robustly detected and the additional time required to generate clones would be unnecessary. Nevertheless, if there is ambiguity, whole genome sequencing of singular parasite clones may be needed. The most promising mutations are ones that occur in multiple, independently derived resistant lines using the same compound. Even in cases where IVIEWGA identifies resistance genes rather than druggable targets, those genes are valuable for epidemiological tracking of antimalarial resistance when compounds enter clinical use. For example, presence of the Kelch13 C580Y mutation is used to track resistance to artemisinin and its derivatives in field isolates.
At present, no intergenic alleles have led to the identification of a target, although in theory mutations in promoter sequences could yield transcriptional upregulation of a target. Better annotations of promoter regions in Plasmodium, which has been accomplished for the human ENCODE projects, could be useful for defining regulatory regions.
Occasionally, IVIEWGA methods fail during the in vitro resistance evolution process. Chemical mutagenesis has been shown to assist in resistance generation,70 but alternative methods may still need to be developed. Despite several challenges, IVIEWGA has proven to be a very successful and robust method for target identification studies. The discovery of these druggable pathways will facilitate the creation of an ideal antimalarial that will be orally bioavailable, be cheap to synthesize, be easily stored at room temperature, and demonstrate low host cytotoxicity. It remains to be seen whether this same method will be adopted successfully for target identification in other pathogens.
Acknowledgments
The authors are supported by grants from the NIH (5R01AI090141 and R01AI103058) and by grants from the Bill and Melinda Gates Foundations (OPP1086217, OPP1141300).
Glossary
Abbreviations
- IVIEWGA
in vitro evolution and whole genome analysis
- WHO
World Health Organization
- ACT
artemisinin combination therapy
- ART
artemisinin
- WGS
whole genome sequencing
- PfATP4
P. falciparum p-type cation ATPase
- CNV
copy number variant
- SNV
single nucleotide variant
- aaRS
aminoacyl-tRNA synthetases
- eEF2
translation elongation factor 2
- TM
transmembrane
- DHODH
dihydoorotate dehydrogenase
- mETC
mitochondrial electron transport chain
- DHFR-TS
dihydrofolate reductase-thymidylate synthase
- dUMP
2′-deoxyuridylic acid
- PI4K
phosphatidylinositol 4-kinase
- CPSF
cleavage and polyadenylation specificity factor
- MEP
methyl-d-erythritol-4-phosphate
- PfIspD
P. falciparum 2-C methyl-d-erythritol 4-phosphate cytidylyltransferase
- PfFPPS/GGPPS
P. falciparum bifunctional farnesyl and geranylgeranyl diphosphate synthase
- EMS
ethylmethanesulfonate
- RBC
red blood cell
- PEXEL
Plasmodium export element
- SUB1
subtilisin-like serine protease
- PCR
polymerase chain reaction
- PfCARL
P. falciparum cyclic amine resistance locus
- SMILES
simplified molecular-input line-entry system
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acsinfecdis.7b00276.
Table S1: Simplified molecular-input line-entry system (SMILES) and structures of antimalarial compounds (XLSX)
Author Contributions
† M.R.L. and P.G. contributed equally. M.R.L., P.G., S.O., and E.A.W. reviewed studies and wrote the manuscript.
The authors declare no competing financial interest.
Supplementary Material
References
- White N. J.; Pukrittayakamee S.; Hien T. T.; Faiz M. A.; Mokuolu O. A.; Dondorp A. M. (2014) Malaria. Lancet 383 (9918), 723–35. 10.1016/S0140-6736(13)60024-0. [DOI] [PubMed] [Google Scholar]
- Nilsson S. K.; Childs L. M.; Buckee C.; Marti M. (2015) Targeting Human Transmission Biology for Malaria Elimination. PLoS Pathog. 11 (6), e1004871. 10.1371/journal.ppat.1004871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilley L.; Straimer J.; Gnadig N. F.; Ralph S. A.; Fidock D. A. (2016) Artemisinin Action and Resistance in Plasmodium falciparum. Trends Parasitol. 32 (9), 682–96. 10.1016/j.pt.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasco B.; Leroy D.; Fidock D. A. (2017) Antimalarial drug resistance: linking Plasmodium falciparum parasite biology to the clinic. Nat. Med. 23 (8), 917–928. 10.1038/nm.4381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M. A.; Burrows J. N.; Manyando C.; van Huijsduijnen R. H.; Van Voorhis W. C.; Wells T. N. C. (2017) Malaria. Nature reviews. Disease primers 3, 17050. 10.1038/nrdp.2017.50. [DOI] [PubMed] [Google Scholar]
- White N. J.; Pukrittayakamee S.; Phyo A. P.; Rueangweerayut R.; Nosten F.; Jittamala P.; Jeeyapant A.; Jain J. P.; Lefevre G.; Li R.; Magnusson B.; Diagana T. T.; Leong F. J. (2014) Spiroindolone KAE609 for falciparum and vivax malaria. N. Engl. J. Med. 371 (5), 403–10. 10.1056/NEJMoa1315860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rottmann M.; McNamara C.; Yeung B. K.; Lee M. C.; Zou B.; Russell B.; Seitz P.; Plouffe D. M.; Dharia N. V.; Tan J.; Cohen S. B.; Spencer K. R.; Gonzalez-Paez G. E.; Lakshminarayana S. B.; Goh A.; Suwanarusk R.; Jegla T.; Schmitt E. K.; Beck H. P.; Brun R.; Nosten F.; Renia L.; Dartois V.; Keller T. H.; Fidock D. A.; Winzeler E. A.; Diagana T. T. (2010) Spiroindolones, a potent compound class for the treatment of malaria. Science (Washington, DC, U. S.) 329 (5996), 1175–80. 10.1126/science.1193225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman N. J.; Allen R. J.; McNamara C. W.; Yeung B. K.; Winzeler E. A.; Diagana T. T.; Kirk K. (2013) Na(+) regulation in the malaria parasite Plasmodium falciparum involves the cation ATPase PfATP4 and is a target of the spiroindolone antimalarials. Cell Host Microbe 13 (2), 227–37. 10.1016/j.chom.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery E. L.; McNamara C. W.; Kim S. W.; Kato T. S.; Li F.; Teng C. H.; Gagaring K.; Manary M. J.; Barboa R.; Meister S.; Kuhen K.; Vinetz J. M.; Chatterjee A. K.; Winzeler E. A. (2015) Mutations in the P-type cation-transporter ATPase 4, PfATP4, mediate resistance to both aminopyrazole and spiroindolone antimalarials. ACS Chem. Biol. 10 (2), 413–20. 10.1021/cb500616x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg H.; Handeli S.; Friedman S.; Gorodetsky R.; Krugliak M. (1986) Effects of red blood cell potassium and hypertonicity on the growth of Plasmodium falciparum in culture. Z. Parasitenkd. 72 (2), 185–99. 10.1007/BF00931146. [DOI] [PubMed] [Google Scholar]
- Allman E. L.; Painter H. J.; Samra J.; Carrasquilla M.; Llinas M. (2016) Metabolomic Profiling of the Malaria Box Reveals Antimalarial Target Pathways. Antimicrob. Agents Chemother. 60 (11), 6635–6649. 10.1128/AAC.01224-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez-Diaz M. B.; Ebert D.; Salinas Y.; Pradhan A.; Lehane A. M.; Myrand-Lapierre M. E.; O’Loughlin K. G.; Shackleford D. M.; Justino de Almeida M.; Carrillo A. K.; Clark J. A.; Dennis A. S.; Diep J.; Deng X.; Duffy S.; Endsley A. N.; Fedewa G.; Guiguemde W. A.; Gomez M. G.; Holbrook G.; Horst J.; Kim C. C.; Liu J.; Lee M. C.; Matheny A.; Martinez M. S.; Miller G.; Rodriguez-Alejandre A.; Sanz L.; Sigal M.; Spillman N. J.; Stein P. D.; Wang Z.; Zhu F.; Waterson D.; Knapp S.; Shelat A.; Avery V. M.; Fidock D. A.; Gamo F. J.; Charman S. A.; Mirsalis J. C.; Ma H.; Ferrer S.; Kirk K.; Angulo-Barturen I.; Kyle D. E.; DeRisi J. L.; Floyd D. M.; Guy R. K. (2014) (+)-SJ733, a clinical candidate for malaria that acts through ATP4 to induce rapid host-mediated clearance of Plasmodium. Proc. Natl. Acad. Sci. U. S. A. 111 (50), E5455–62. 10.1073/pnas.1414221111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidya A. B.; Morrisey J. M.; Zhang Z.; Das S.; Daly T. M.; Otto T. D.; Spillman N. J.; Wyvratt M.; Siegl P.; Marfurt J.; Wirjanata G.; Sebayang B. F.; Price R. N.; Chatterjee A.; Nagle A.; Stasiak M.; Charman S. A.; Angulo-Barturen I.; Ferrer S.; Belen Jimenez-Diaz M.; Martinez M. S.; Gamo F. J.; Avery V. M.; Ruecker A.; Delves M.; Kirk K.; Berriman M.; Kortagere S.; Burrows J.; Fan E.; Bergman L. W. (2014) Pyrazoleamide compounds are potent antimalarials that target Na+ homeostasis in intraerythrocytic Plasmodium falciparum. Nat. Commun. 5, 5521. 10.1038/ncomms6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham J. S.; Dawson K. L.; Jackson K. E.; Lim E. E.; Pasaje C. F.; Turner K. E.; Ralph S. A. (2014) Aminoacyl-tRNA synthetases as drug targets in eukaryotic parasites. Int. J. Parasitol.: Drugs Drug Resist. 4 (1), 1–13. 10.1016/j.ijpddr.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling J.; Reynolds N.; Ibba M. (2009) Aminoacyl-tRNA synthesis and translational quality control. Annu. Rev. Microbiol. 63, 61–78. 10.1146/annurev.micro.091208.073210. [DOI] [PubMed] [Google Scholar]
- Yadavalli S. S.; Ibba M. (2012) Quality control in aminoacyl-tRNA synthesis its role in translational fidelity. Adv. Protein Chem. Struct. Biol. 86, 1–43. 10.1016/B978-0-12-386497-0.00001-3. [DOI] [PubMed] [Google Scholar]
- Bhatt T. K.; Kapil C.; Khan S.; Jairajpuri M. A.; Sharma V.; Santoni D.; Silvestrini F.; Pizzi E.; Sharma A. (2009) A genomic glimpse of aminoacyl-tRNA synthetases in malaria parasite Plasmodium falciparum. BMC Genomics 10, 644. 10.1186/1471-2164-10-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A.; Sharma A. (2015) Plasmodium falciparum mitochondria import tRNAs along with an active phenylalanyl-tRNA synthetase. Biochem. J. 465 (3), 459–69. 10.1042/BJ20140998. [DOI] [PubMed] [Google Scholar]
- Istvan E. S.; Dharia N. V.; Bopp S. E.; Gluzman I.; Winzeler E. A.; Goldberg D. E. (2011) Validation of isoleucine utilization targets in Plasmodium falciparum. Proc. Natl. Acad. Sci. U. S. A. 108 (4), 1627–32. 10.1073/pnas.1011560108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman J. D.; Pepper L. R.; Cortese J. F.; Estiu G.; Galinsky K.; Zuzarte-Luis V.; Derbyshire E. R.; Ribacke U.; Lukens A. K.; Santos S. A.; Patel V.; Clish C. B.; Sullivan W. J. Jr.; Zhou H.; Bopp S. E.; Schimmel P.; Lindquist S.; Clardy J.; Mota M. M.; Keller T. L.; Whitman M.; Wiest O.; Wirth D. F.; Mazitschek R. (2015) The cytoplasmic prolyl-tRNA synthetase of the malaria parasite is a dual-stage target of febrifugine and its analogs. Sci. Transl. Med. 7 (288), 288ra77. 10.1126/scitranslmed.aaa3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato N.; Comer E.; Sakata-Kato T.; Sharma A.; Sharma M.; Maetani M.; Bastien J.; Brancucci N. M.; Bittker J. A.; Corey V.; Clarke D.; Derbyshire E. R.; Dornan G. L.; Duffy S.; Eckley S.; Itoe M. A.; Koolen K. M.; Lewis T. A.; Lui P. S.; Lukens A. K.; Lund E.; March S.; Meibalan E.; Meier B. C.; McPhail J. A.; Mitasev B.; Moss E. L.; Sayes M.; Van Gessel Y.; Wawer M. J.; Yoshinaga T.; Zeeman A. M.; Avery V. M.; Bhatia S. N.; Burke J. E.; Catteruccia F.; Clardy J. C.; Clemons P. A.; Dechering K. J.; Duvall J. R.; Foley M. A.; Gusovsky F.; Kocken C. H.; Marti M.; Morningstar M. L.; Munoz B.; Neafsey D. E.; Sharma A.; Winzeler E. A.; Wirth D. F.; Scherer C. A.; Schreiber S. L. (2016) Diversity-oriented synthesis yields novel multistage antimalarial inhibitors. Nature 538 (7625), 344–349. 10.1038/nature19804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S.; Sharma A.; Jamwal A.; Sharma V.; Pole A. K.; Thakur K. K.; Sharma A. (2011) Uneven spread of cis- and trans-editing aminoacyl-tRNA synthetase domains within translational compartments of P. falciparum. Sci. Rep. 1, 188. 10.1038/srep00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoepfner D.; McNamara C. W.; Lim C. S.; Studer C.; Riedl R.; Aust T.; McCormack S. L.; Plouffe D. M.; Meister S.; Schuierer S.; Plikat U.; Hartmann N.; Staedtler F.; Cotesta S.; Schmitt E. K.; Petersen F.; Supek F.; Glynne R. J.; Tallarico J. A.; Porter J. A.; Fishman M. C.; Bodenreider C.; Diagana T. T.; Movva N. R.; Winzeler E. A. (2012) Selective and specific inhibition of the plasmodium falciparum lysyl-tRNA synthetase by the fungal secondary metabolite cladosporin. Cell Host Microbe 11 (6), 654–63. 10.1016/j.chom.2012.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S.; Sharma A.; Belrhali H.; Yogavel M.; Sharma A. (2014) Structural basis of malaria parasite lysyl-tRNA synthetase inhibition by cladosporin. J. Struct. Funct. Genomics 15 (2), 63–71. 10.1007/s10969-014-9182-1. [DOI] [PubMed] [Google Scholar]
- Fang P.; Han H.; Wang J.; Chen K.; Chen X.; Guo M. (2015) Structural Basis for Specific Inhibition of tRNA Synthetase by an ATP Competitive Inhibitor. Chem. Biol. 22 (6), 734–44. 10.1016/j.chembiol.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoen R.; Novoa E. M.; Lopez A.; Camacho N.; Cubells L.; Vieira P.; Santos M.; Marin-Garcia P.; Bautista J. M.; Cortes A.; Ribas de Pouplana L.; Royo M. (2013) Selective inhibition of an apicoplastic aminoacyl-tRNA synthetase from Plasmodium falciparum. ChemBioChem 14 (4), 499–509. 10.1002/cbic.201200620. [DOI] [PubMed] [Google Scholar]
- Keller T. L.; Zocco D.; Sundrud M. S.; Hendrick M.; Edenius M.; Yum J.; Kim Y. J.; Lee H. K.; Cortese J. F.; Wirth D. F.; Dignam J. D.; Rao A.; Yeo C. Y.; Mazitschek R.; Whitman M. (2012) Halofuginone and other febrifugine derivatives inhibit prolyl-tRNA synthetase. Nat. Chem. Biol. 8 (3), 311–7. 10.1038/nchembio.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain V.; Yogavel M.; Kikuchi H.; Oshima Y.; Hariguchi N.; Matsumoto M.; Goel P.; Touquet B.; Jumani R. S.; Tacchini-Cottier F.; Harlos K.; Huston C. D.; Hakimi M. A.; Sharma A. (2017) Targeting Prolyl-tRNA Synthetase to Accelerate Drug Discovery against Malaria, Leishmaniasis, Toxoplasmosis, Cryptosporidiosis, and Coccidiosis. Structure (Oxford, U. K.) 25 (10), 1495–1505.e6. 10.1016/j.str.2017.07.015. [DOI] [PubMed] [Google Scholar]
- Werner R. G.; Thorpe L. F.; Reuter W.; Nierhaus K. H. (1976) Indolmycin inhibits prokaryotic tryptophanyl-tRNA ligase. Eur. J. Biochem. 68 (1), 1–3. 10.1111/j.1432-1033.1976.tb10758.x. [DOI] [PubMed] [Google Scholar]
- Pasaje C. F.; Cheung V.; Kennedy K.; Lim E. E.; Baell J. B.; Griffin M. D.; Ralph S. A. (2016) Selective inhibition of apicoplast tryptophanyl-tRNA synthetase causes delayed death in Plasmodium falciparum. Sci. Rep. 6, 27531. 10.1038/srep27531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otoguro K.; Ui H.; Ishiyama A.; Kobayashi M.; Togashi H.; Takahashi Y.; Masuma R.; Tanaka H.; Tomoda H.; Yamada H.; Omura S. (2003) In vitro and in vivo antimalarial activities of a non-glycosidic 18-membered macrolide antibiotic, borrelidin, against drug-resistant strains of Plasmodia. J. Antibiot. 56 (8), 727–9. 10.7164/antibiotics.56.727. [DOI] [PubMed] [Google Scholar]
- Frohler J.; Rechenmacher A.; Thomale J.; Nass G.; Bock A. (1980) Genetic analysis of mutations causing borrelidin resistance by overproduction of threonyl-transfer ribonucleic acid synthetase. J. Bacteriol. 143 (3), 1135–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham J. S.; Sakaguchi R.; Yeoh L. M.; De Silva N. S.; McFadden G. I.; Hou Y. M.; Ralph S. A. (2014) A dual-targeted aminoacyl-tRNA synthetase in Plasmodium falciparum charges cytosolic and apicoplast tRNACys. Biochem. J. 458 (3), 513–23. 10.1042/BJ20131451. [DOI] [PubMed] [Google Scholar]
- Jackson K. E.; Pham J. S.; Kwek M.; De Silva N. S.; Allen S. M.; Goodman C. D.; McFadden G. I.; Ribas de Pouplana L.; Ralph S. A. (2012) Dual targeting of aminoacyl-tRNA synthetases to the apicoplast and cytosol in Plasmodium falciparum. Int. J. Parasitol. 42 (2), 177–86. 10.1016/j.ijpara.2011.11.008. [DOI] [PubMed] [Google Scholar]
- Novoa E. M.; Camacho N.; Tor A.; Wilkinson B.; Moss S.; Marin-Garcia P.; Azcarate I. G.; Bautista J. M.; Mirando A. C.; Francklyn C. S.; Varon S.; Royo M.; Cortes A.; Ribas de Pouplana L. (2014) Analogs of natural aminoacyl-tRNA synthetase inhibitors clear malaria in vivo. Proc. Natl. Acad. Sci. U. S. A. 111 (51), E5508–17. 10.1073/pnas.1405994111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty B.; Mukherjee R.; Sengupta J. (2013) Structural insights into the mechanism of translational inhibition by the fungicide sordarin. J. Comput.-Aided Mol. Des. 27 (2), 173–84. 10.1007/s10822-013-9636-8. [DOI] [PubMed] [Google Scholar]
- Justice M. C.; Hsu M. J.; Tse B.; Ku T.; Balkovec J.; Schmatz D.; Nielsen J. (1998) Elongation factor 2 as a novel target for selective inhibition of fungal protein synthesis. J. Biol. Chem. 273 (6), 3148–51. 10.1074/jbc.273.6.3148. [DOI] [PubMed] [Google Scholar]
- Shastry M.; Nielsen J.; Ku T.; Hsu M. J.; Liberator P.; Anderson J.; Schmatz D.; Justice M. C. (2001) Species-specific inhibition of fungal protein synthesis by sordarin: identification of a sordarin-specificity region in eukaryotic elongation factor 2. Microbiology (London, U. K.) 147 (2), 383–390. 10.1099/00221287-147-2-383. [DOI] [PubMed] [Google Scholar]
- Baragana B.; Hallyburton I.; Lee M. C.; Norcross N. R.; Grimaldi R.; Otto T. D.; Proto W. R.; Blagborough A. M.; Meister S.; Wirjanata G.; Ruecker A.; Upton L. M.; Abraham T. S.; Almeida M. J.; Pradhan A.; Porzelle A.; Luksch T.; Martinez M. S.; Luksch T.; Bolscher J. M.; Woodland A.; Norval S.; Zuccotto F.; Thomas J.; Simeons F.; Stojanovski L.; Osuna-Cabello M.; Brock P. M.; Churcher T. S.; Sala K. A.; Zakutansky S. E.; Jimenez-Diaz M. B.; Sanz L. M.; Riley J.; Basak R.; Campbell M.; Avery V. M.; Sauerwein R. W.; Dechering K. J.; Noviyanti R.; Campo B.; Frearson J. A.; Angulo-Barturen I.; Ferrer-Bazaga S.; Gamo F. J.; Wyatt P. G.; Leroy D.; Siegl P.; Delves M. J.; Kyle D. E.; Wittlin S.; Marfurt J.; Price R. N.; Sinden R. E.; Winzeler E. A.; Charman S. A.; Bebrevska L.; Gray D. W.; Campbell S.; Fairlamb A. H.; Willis P. A.; Rayner J. C.; Fidock D. A.; Read K. D.; Gilbert I. H. (2015) A novel multiple-stage antimalarial agent that inhibits protein synthesis. Nature 522 (7556), 315–320. 10.1038/nature14451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dechering K. J.; Duerr H. P.; Koolen K. M. J.; Gemert G. V.; Bousema T.; Burrows J.; Leroy D.; Sauerwein R. W. (2017) Modelling mosquito infection at natural parasite densities identifies drugs targeting EF2, PI4K or ATP4 as key candidates for interrupting malaria transmission. Sci. Rep. 7 (1), 17680. 10.1038/s41598-017-16671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painter H. J.; Morrisey J. M.; Mather M. W.; Vaidya A. B. (2007) Specific role of mitochondrial electron transport in blood-stage Plasmodium falciparum. Nature 446 (7131), 88–91. 10.1038/nature05572. [DOI] [PubMed] [Google Scholar]
- Vaidya A. B.; Mather M. W. (2009) Mitochondrial evolution and functions in malaria parasites. Annu. Rev. Microbiol. 63, 249–67. 10.1146/annurev.micro.091208.073424. [DOI] [PubMed] [Google Scholar]
- Phillips M. A.; Rathod P. K. (2010) Plasmodium dihydroorotate dehydrogenase: a promising target for novel anti-malarial chemotherapy. Infect. Disord.: Drug Targets 10 (3), 226–239. 10.2174/187152610791163336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M. A.; Lotharius J.; Marsh K.; White J.; Dayan A.; White K. L.; Njoroge J. W.; El Mazouni F.; Lao Y.; Kokkonda S.; Tomchick D. R.; Deng X.; Laird T.; Bhatia S. N.; March S.; Ng C. L.; Fidock D. A.; Wittlin S.; Lafuente-Monasterio M.; Benito F. J.; Alonso L. M.; Martinez M. S.; Jimenez-Diaz M. B.; Bazaga S. F.; Angulo-Barturen I.; Haselden J. N.; Louttit J.; Cui Y.; Sridhar A.; Zeeman A. M.; Kocken C.; Sauerwein R.; Dechering K.; Avery V. M.; Duffy S.; Delves M.; Sinden R.; Ruecker A.; Wickham K. S.; Rochford R.; Gahagen J.; Iyer L.; Riccio E.; Mirsalis J.; Bathhurst I.; Rueckle T.; Ding X.; Campo B.; Leroy D.; Rogers M. J.; Rathod P. K.; Burrows J. N.; Charman S. A. (2015) A long-duration dihydroorotate dehydrogenase inhibitor (DSM265) for prevention and treatment of malaria. Sci. Transl. Med. 7 (296), 296ra111. 10.1126/scitranslmed.aaa6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy J. S.; Lotharius J.; Ruckle T.; Chalon S.; Phillips M. A.; Elliott S.; Sekuloski S.; Griffin P.; Ng C. L.; Fidock D. A.; Marquart L.; Williams N. S.; Gobeau N.; Bebrevska L.; Rosario M.; Marsh K.; Mohrle J. J. (2017) Safety, tolerability, pharmacokinetics, and activity of the novel long-acting antimalarial DSM265: a two-part first-in-human phase 1a/1b randomised study. Lancet Infect. Dis. 17 (6), 626–635. 10.1016/S1473-3099(17)30171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips M. A.; White K. L.; Kokkonda S.; Deng X.; White J.; El Mazouni F.; Marsh K.; Tomchick D. R.; Manjalanagara K.; Rudra K. R.; Wirjanata G.; Noviyanti R.; Price R. N.; Marfurt J.; Shackleford D. M.; Chiu F. C.; Campbell M.; Jimenez-Diaz M. B.; Bazaga S. F.; Angulo-Barturen I.; Martinez M. S.; Lafuente-Monasterio M.; Kaminsky W.; Silue K.; Zeeman A. M.; Kocken C.; Leroy D.; Blasco B.; Rossignol E.; Rueckle T.; Matthews D.; Burrows J. N.; Waterson D.; Palmer M. J.; Rathod P. K.; Charman S. A. (2016) A Triazolopyrimidine-Based Dihydroorotate Dehydrogenase Inhibitor with Improved Drug-like Properties for Treatment and Prevention of Malaria. ACS Infect. Dis. 2 (12), 945–957. 10.1021/acsinfecdis.6b00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booker M. L.; Bastos C. M.; Kramer M. L.; Barker R. H. Jr.; Skerlj R.; Sidhu A. B.; Deng X.; Celatka C.; Cortese J. F.; Guerrero Bravo J. E.; Crespo Llado K. N.; Serrano A. E.; Angulo-Barturen I.; Jimenez-Diaz M. B.; Viera S.; Garuti H.; Wittlin S.; Papastogiannidis P.; Lin J. W.; Janse C. J.; Khan S. M.; Duraisingh M.; Coleman B.; Goldsmith E. J.; Phillips M. A.; Munoz B.; Wirth D. F.; Klinger J. D.; Wiegand R.; Sybertz E. (2010) Novel inhibitors of Plasmodium falciparum dihydroorotate dehydrogenase with anti-malarial activity in the mouse model. J. Biol. Chem. 285 (43), 33054–64. 10.1074/jbc.M110.162081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azeredo L. F.; Coutinho J. P.; Jabor V. A.; Feliciano P. R.; Nonato M. C.; Kaiser C. R.; Menezes C. M.; Hammes A. S.; Caffarena E. R.; Hoelz L. V.; de Souza N. B.; Pereira G. A.; Ceravolo I. P.; Krettli A. U.; Boechat N. (2017) Evaluation of 7-arylaminopyrazolo[1,5-a]pyrimidines as anti-Plasmodium falciparum, antimalarial, and Pf-dihydroorotate dehydrogenase inhibitors. Eur. J. Med. Chem. 126, 72–83. 10.1016/j.ejmech.2016.09.073. [DOI] [PubMed] [Google Scholar]
- Guler J. L.; Freeman D. L.; Ahyong V.; Patrapuvich R.; White J.; Gujjar R.; Phillips M. A.; DeRisi J.; Rathod P. K. (2013) Asexual populations of the human malaria parasite, Plasmodium falciparum, use a two-step genomic strategy to acquire accurate, beneficial DNA amplifications. PLoS Pathog. 9 (5), e1003375. 10.1371/journal.ppat.1003375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maetani M.; Kato N.; Jabor V. A. P.; Calil F. A.; Nonato M. C.; Scherer C. A.; Schreiber S. L. (2017) Discovery of Antimalarial Azetidine-2-carbonitriles That Inhibit P. falciparum Dihydroorotate Dehydrogenase. ACS Med. Chem. Lett. 8 (4), 438–442. 10.1021/acsmedchemlett.7b00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L. S.; Gamo F. J.; Lafuente-Monasterio M. J.; Singh O. M.; Rowland P.; Wiegand R. C.; Wirth D. F. (2014) In vitro resistance selections for Plasmodium falciparum dihydroorotate dehydrogenase inhibitors give mutants with multiple point mutations in the drug-binding site and altered growth. J. Biol. Chem. 289 (26), 17980–95. 10.1074/jbc.M114.558353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam T. G.; McNamara C. W.; Bopp S.; Dharia N. V.; Meister S.; Bonamy G. M.; Plouffe D. M.; Kato N.; McCormack S.; Bursulaya B.; Ke H.; Vaidya A. B.; Schultz P. G.; Winzeler E. A. (2011) A chemical genomic analysis of decoquinate, a Plasmodium falciparum cytochrome b inhibitor. ACS Chem. Biol. 6 (11), 1214–22. 10.1021/cb200105d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corey V. C.; Lukens A. K.; Istvan E. S.; Lee M. C.; Franco V.; Magistrado P.; Coburn-Flynn O.; Sakata-Kato T.; Fuchs O.; Gnadig N. F.; Goldgof G.; Linares M.; Gomez-Lorenzo M. G.; De Cozar C.; Lafuente-Monasterio M. J.; Prats S.; Meister S.; Tanaseichuk O.; Wree M.; Zhou Y.; Willis P. A.; Gamo F. J.; Goldberg D. E.; Fidock D. A.; Wirth D. F.; Winzeler E. A. (2016) A broad analysis of resistance development in the malaria parasite. Nat. Commun. 7, 11901. 10.1038/ncomms11901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong C. K.; Urgaonkar S.; Cortese J. F.; Gamo F. J.; Garcia-Bustos J. F.; Lafuente M. J.; Patel V.; Ross L.; Coleman B. I.; Derbyshire E. R.; Clish C. B.; Serrano A. E.; Cromwell M.; Barker R. H. Jr.; Dvorin J. D.; Duraisingh M. T.; Wirth D. F.; Clardy J.; Mazitschek R. (2011) Identification and validation of tetracyclic benzothiazepines as Plasmodium falciparum cytochrome bc1 inhibitors. Chem. Biol. 18 (12), 1602–10. 10.1016/j.chembiol.2011.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallieres C.; Fisher N.; Antoine T.; Al-Helal M.; Stocks P.; Berry N. G.; Lawrenson A. S.; Ward S. A.; O’Neill P. M.; Biagini G. A.; Meunier B. (2012) HDQ, a potent inhibitor of Plasmodium falciparum proliferation, binds to the quinone reduction site of the cytochrome bc1 complex. Antimicrob. Agents Chemother. 56 (7), 3739–47. 10.1128/AAC.00486-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capper M. J.; O’Neill P. M.; Fisher N.; Strange R. W.; Moss D.; Ward S. A.; Berry N. G.; Lawrenson A. S.; Hasnain S. S.; Biagini G. A.; Antonyuk S. V. (2015) Antimalarial 4(1H)-pyridones bind to the Qi site of cytochrome bc1. Proc. Natl. Acad. Sci. U. S. A. 112 (3), 755–60. 10.1073/pnas.1416611112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukens A. K.; Heidebrecht R. W. Jr.; Mulrooney C.; Beaudoin J. A.; Comer E.; Duvall J. R.; Fitzgerald M. E.; Masi D.; Galinsky K.; Scherer C. A.; Palmer M.; Munoz B.; Foley M.; Schreiber S. L.; Wiegand R. C.; Wirth D. F. (2015) Diversity-oriented synthesis probe targets Plasmodium falciparum cytochrome b ubiquinone reduction site and synergizes with oxidation site inhibitors. J. Infect. Dis. 211 (7), 1097–103. 10.1093/infdis/jiu565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanetich K. M.; Santi D. V. (1990) Bifunctional thymidylate synthase-dihydrofolate reductase in protozoa. FASEB J. 4 (6), 1591–7. 10.1096/fasebj.4.6.2180768. [DOI] [PubMed] [Google Scholar]
- Cowell A. N.; Istvan E. S.; Lukens A. K.; Gomez-Lorenzo M. G.; Vanaerschot M.; Sakata-Kato T.; Flannery E. L.; Magistrado P.; Owen E.; Abraham M.; LaMonte G.; Painter H. J.; Williams R. M.; Franco V.; Linares M.; Arriaga I.; Bopp S.; Corey V. C.; Gnadig N. F.; Coburn-Flynn O.; Reimer C.; Gupta P.; Murithi J. M.; Moura P. A.; Fuchs O.; Sasaki E.; Kim S. W.; Teng C. H.; Wang L. T.; Akidil A.; Adjalley S.; Willis P. A.; Siegel D.; Tanaseichuk O.; Zhong Y.; Zhou Y.; Llinas M.; Ottilie S.; Gamo F. J.; Lee M. C. S.; Goldberg D. E.; Fidock D. A.; Wirth D. F.; Winzeler E. A. (2018) Mapping the malaria parasite druggable genome by using in vitro evolution and chemogenomics. Science (Washington, DC, U. S.) 359 (6372), 191–199. 10.1126/science.aan4472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaianantakul N.; Sirawaraporn R.; Sirawaraporn W. (2013) Insights into the role of the junctional region of Plasmodium falciparum dihydrofolate reductase-thymidylate synthase. Malar. J. 12, 91. 10.1186/1475-2875-12-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayinger P. (2012) Phosphoinositides and vesicular membrane traffic. Biochim. Biophys. Acta, Mol. Cell Biol. Lipids 1821 (8), 1104–13. 10.1016/j.bbalip.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara C. W.; Lee M. C.; Lim C. S.; Lim S. H.; Roland J.; Simon O.; Yeung B. K.; Chatterjee A. K.; McCormack S. L.; Manary M. J.; Zeeman A. M.; Dechering K. J.; Kumar T. S.; Henrich P. P.; Gagaring K.; Ibanez M.; Kato N.; Kuhen K. L.; Fischli C.; Nagle A.; Rottmann M.; Plouffe D. M.; Bursulaya B.; Meister S.; Rameh L.; Trappe J.; Haasen D.; Timmerman M.; Sauerwein R. W.; Suwanarusk R.; Russell B.; Renia L.; Nosten F.; Tully D. C.; Kocken C. H.; Glynne R. J.; Bodenreider C.; Fidock D. A.; Diagana T. T.; Winzeler E. A. (2013) Targeting Plasmodium PI(4)K to eliminate malaria. Nature 504 (7479), 248–253. 10.1038/nature12782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquet T.; Le Manach C.; Cabrera D. G.; Younis Y.; Henrich P. P.; Abraham T. S.; Lee M. C. S.; Basak R.; Ghidelli-Disse S.; Lafuente-Monasterio M. J.; Bantscheff M.; Ruecker A.; Blagborough A. M.; Zakutansky S. E.; Zeeman A. M.; White K. L.; Shackleford D. M.; Mannila J.; Morizzi J.; Scheurer C.; Angulo-Barturen I.; Martinez M. S.; Ferrer S.; Sanz L. M.; Gamo F. J.; Reader J.; Botha M.; Dechering K. J.; Sauerwein R. W.; Tungtaeng A.; Vanachayangkul P.; Lim C. S.; Burrows J.; Witty M. J.; Marsh K. C.; Bodenreider C.; Rochford R.; Solapure S. M.; Jimenez-Diaz M. B.; Wittlin S.; Charman S. A.; Donini C.; Campo B.; Birkholtz L. M.; Hanson K. K.; Drewes G.; Kocken C. H. M.; Delves M. J.; Leroy D.; Fidock D. A.; Waterson D.; Street L. J.; Chibale K. (2017) Antimalarial efficacy of MMV390048, an inhibitor of Plasmodium phosphatidylinositol 4-kinase. Sci. Transl. Med. 9 (387), eaad9735. 10.1126/scitranslmed.aad9735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonoiki E.; Ng C. L.; Lee M. C.; Guo D.; Zhang Y. K.; Zhou Y.; Alley M. R.; Ahyong V.; Sanz L. M.; Lafuente-Monasterio M. J.; Dong C.; Schupp P. G.; Gut J.; Legac J.; Cooper R. A.; Gamo F. J.; DeRisi J.; Freund Y. R.; Fidock D. A.; Rosenthal P. J. (2017) A potent antimalarial benzoxaborole targets a Plasmodium falciparum cleavage and polyadenylation specificity factor homologue. Nat. Commun. 8, 14574. 10.1038/ncomms14574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh A. P.; Zhang Y.; No J. H.; Docampo R.; Nussenzweig V.; Oldfield E. (2010) Lipophilic bisphosphonates are potent inhibitors of Plasmodium liver-stage growth. Antimicrob. Agents Chemother. 54 (7), 2987–93. 10.1128/AAC.00198-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- No J. H.; de Macedo Dossin F.; Zhang Y.; Liu Y. L.; Zhu W.; Feng X.; Yoo J. A.; Lee E.; Wang K.; Hui R.; Freitas-Junior L. H.; Oldfield E. (2012) Lipophilic analogs of zoledronate and risedronate inhibit Plasmodium geranylgeranyl diphosphate synthase (GGPPS) and exhibit potent antimalarial activity. Proc. Natl. Acad. Sci. U. S. A. 109 (11), 4058–63. 10.1073/pnas.1118215109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin M. B.; Grimley J. S.; Lewis J. C.; Heath H. T. 3rd; Bailey B. N.; Kendrick H.; Yardley V.; Caldera A.; Lira R.; Urbina J. A.; Moreno S. N.; Docampo R.; Croft S. L.; Oldfield E. (2001) Bisphosphonates inhibit the growth of Trypanosoma brucei, Trypanosoma cruzi, Leishmania donovani, Toxoplasma gondii, and Plasmodium falciparum: a potential route to chemotherapy. J. Med. Chem. 44 (6), 909–16. 10.1021/jm0002578. [DOI] [PubMed] [Google Scholar]
- Dharia N. V.; Sidhu A. B.; Cassera M. B.; Westenberger S. J.; Bopp S. E.; Eastman R. T.; Plouffe D.; Batalov S.; Park D. J.; Volkman S. K.; Wirth D. F.; Zhou Y.; Fidock D. A.; Winzeler E. A. (2009) Use of high-density tiling microarrays to identify mutations globally and elucidate mechanisms of drug resistance in Plasmodium falciparum. Genome biology 10 (2), R21. 10.1186/gb-2009-10-2-r21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangenberg T.; Burrows J. N.; Kowalczyk P.; McDonald S.; Wells T. N.; Willis P. (2013) The open access malaria box: a drug discovery catalyst for neglected diseases. PLoS One 8 (6), e62906. 10.1371/journal.pone.0062906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W.; Herrera Z.; Ebert D.; Baska K.; Cho S. H.; DeRisi J. L.; Yeh E. (2015) A chemical rescue screen identifies a Plasmodium falciparum apicoplast inhibitor targeting MEP isoprenoid precursor biosynthesis. Antimicrob. Agents Chemother. 59 (1), 356–64. 10.1128/AAC.03342-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gisselberg J.; Herrera Z.; Orchard L. M.; Llinas M.; Yeh E. (2018) Specific inhibition of the bifunctional farnesyl/geranylgeranyl diphosphate synthase in malaria parasites via a new small molecule binding site. Cell Chemical Biology 25, 185. 10.1016/j.chembiol.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eastman R. T.; Buckner F. S.; Yokoyama K.; Gelb M. H.; Van Voorhis W. C. (2006) Thematic review series: lipid posttranslational modifications. Fighting parasitic disease by blocking protein farnesylation. J. Lipid Res. 47 (2), 233–40. 10.1194/jlr.R500016-JLR200. [DOI] [PubMed] [Google Scholar]
- Nallan L.; Bauer K. D.; Bendale P.; Rivas K.; Yokoyama K.; Horney C. P.; Pendyala P. R.; Floyd D.; Lombardo L. J.; Williams D. K.; Hamilton A.; Sebti S.; Windsor W. T.; Weber P. C.; Buckner F. S.; Chakrabarti D.; Gelb M. H.; Van Voorhis W. C. (2005) Protein farnesyltransferase inhibitors exhibit potent antimalarial activity. J. Med. Chem. 48 (11), 3704–13. 10.1021/jm0491039. [DOI] [PubMed] [Google Scholar]
- Wiesner J.; Kettler K.; Sakowski J.; Ortmann R.; Katzin A. M.; Kimura E. A.; Silber K.; Klebe G.; Jomaa H.; Schlitzer M. (2004) Farnesyltransferase inhibitors inhibit the growth of malaria parasites in vitro and in vivo. Angew. Chem., Int. Ed. 43 (2), 251–4. 10.1002/anie.200351169. [DOI] [PubMed] [Google Scholar]
- Rao S.; Cunningham D.; de Gramont A.; Scheithauer W.; Smakal M.; Humblet Y.; Kourteva G.; Iveson T.; Andre T.; Dostalova J.; Illes A.; Belly R.; Perez-Ruixo J. J.; Park Y. C.; Palmer P. A. (2004) Phase III double-blind placebo-controlled study of farnesyl transferase inhibitor R115777 in patients with refractory advanced colorectal cancer. J. Clin. Oncol. 22 (19), 3950–7. 10.1200/JCO.2004.10.037. [DOI] [PubMed] [Google Scholar]
- Doll R. J.; Kirschmeier P.; Bishop W. R. (2004) Farnesyltransferase inhibitors as anticancer agents: critical crossroads. Curr. Opin. Drug Discovery Dev. 7 (4), 478–486. [PubMed] [Google Scholar]
- Eastman R. T.; White J.; Hucke O.; Yokoyama K.; Verlinde C. L.; Hast M. A.; Beese L. S.; Gelb M. H.; Rathod P. K.; Van Voorhis W. C. (2007) Resistance mutations at the lipid substrate binding site of Plasmodium falciparum protein farnesyltransferase. Mol. Biochem. Parasitol. 152 (1), 66–71. 10.1016/j.molbiopara.2006.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldgof G. M.; Durrant J. D.; Ottilie S.; Vigil E.; Allen K. E.; Gunawan F.; Kostylev M.; Henderson K. A.; Yang J.; Schenken J.; LaMonte G. M.; Manary M. J.; Murao A.; Nachon M.; Stanhope R.; Prescott M.; McNamara C. W.; Slayman C. W.; Amaro R. E.; Suzuki Y.; Winzeler E. A. (2016) Comparative chemical genomics reveal that the spiroindolone antimalarial KAE609 (Cipargamin) is a P-type ATPase inhibitor. Sci. Rep. 6, 27806. 10.1038/srep27806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bibo-Verdugo B.; Jiang Z.; Caffrey C. R.; O’Donoghue A. J. (2017) Targeting proteasomes in infectious organisms to combat disease. FEBS J. 284 (10), 1503–1517. 10.1111/febs.14029. [DOI] [PubMed] [Google Scholar]
- Gandolfi S.; Laubach J. P.; Hideshima T.; Chauhan D.; Anderson K. C.; Richardson P. G. (2017) The proteasome and proteasome inhibitors in multiple myeloma. Cancer Metastasis Rev. 36 (4), 561–584. 10.1007/s10555-017-9707-8. [DOI] [PubMed] [Google Scholar]
- Huber E. M.; Groll M. (2012) Inhibitors for the immuno- and constitutive proteasome: current and future trends in drug development. Angew. Chem., Int. Ed. 51 (35), 8708–20. 10.1002/anie.201201616. [DOI] [PubMed] [Google Scholar]
- Kisselev A. F.; van der Linden W. A.; Overkleeft H. S. (2012) Proteasome inhibitors: an expanding army attacking a unique target. Chem. Biol. 19 (1), 99–115. 10.1016/j.chembiol.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H.; van der Linden W. A.; Verdoes M.; Florea B. I.; McAllister F. E.; Govindaswamy K.; Elias J. E.; Bhanot P.; Overkleeft H. S.; Bogyo M. (2014) Assessing subunit dependency of the Plasmodium proteasome using small molecule inhibitors and active site probes. ACS Chem. Biol. 9 (8), 1869–76. 10.1021/cb5001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogovski C.; Xie S. C.; Burgio G.; Bridgford J.; Mok S.; McCaw J. M.; Chotivanich K.; Kenny S.; Gnadig N.; Straimer J.; Bozdech Z.; Fidock D. A.; Simpson J. A.; Dondorp A. M.; Foote S.; Klonis N.; Tilley L. (2015) Targeting the cell stress response of Plasmodium falciparum to overcome artemisinin resistance. PLoS Biol. 13 (4), e1002132. 10.1371/journal.pbio.1002132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H.; O’Donoghue A. J.; van der Linden W. A.; Xie S. C.; Yoo E.; Foe I. T.; Tilley L.; Craik C. S.; da Fonseca P. C.; Bogyo M. (2016) Structure- and function-based design of Plasmodium-selective proteasome inhibitors. Nature 530 (7589), 233–6. 10.1038/nature16936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira A. R.; Kale A. J.; Fenley A. T.; Byrum T.; Debonsi H. M.; Gilson M. K.; Valeriote F. A.; Moore B. S.; Gerwick W. H. (2012) The carmaphycins: new proteasome inhibitors exhibiting an alpha,beta-epoxyketone warhead from a marine cyanobacterium. ChemBioChem 13 (6), 810–7. 10.1002/cbic.201200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaMonte G. M.; Almaliti J.; Bibo-Verdugo B.; Keller L.; Zou B. Y.; Yang J.; Antonova-Koch Y.; Orjuela-Sanchez P.; Boyle C. A.; Vigil E.; Wang L.; Goldgof G. M.; Gerwick L.; O’Donoghue A. J.; Winzeler E. A.; Gerwick W. H.; Ottilie S. (2017) Development of a Potent Inhibitor of the Plasmodium Proteasome with Reduced Mammalian Toxicity. J. Med. Chem. 60 (15), 6721–6732. 10.1021/acs.jmedchem.7b00671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk B. (2006) Targeting proteases: successes, failures and future prospects. Nat. Rev. Drug Discovery 5 (9), 785–99. 10.1038/nrd2092. [DOI] [PubMed] [Google Scholar]
- Drag M.; Salvesen G. S. (2010) Emerging principles in protease-based drug discovery. Nat. Rev. Drug Discovery 9 (9), 690–701. 10.1038/nrd3053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- da Silva F. L.; Dixon M. W.; Stack C. M.; Teuscher F.; Taran E.; Jones M. K.; Lovas E.; Tilley L.; Brown C. L.; Trenholme K. R.; Dalton J. P.; Gardiner D. L.; Skinner-Adams T. S. (2016) A Plasmodium falciparum S33 proline aminopeptidase is associated with changes in erythrocyte deformability. Exp. Parasitol. 169, 13–21. 10.1016/j.exppara.2016.06.013. [DOI] [PubMed] [Google Scholar]
- Yeoh S.; O’Donnell R. A.; Koussis K.; Dluzewski A. R.; Ansell K. H.; Osborne S. A.; Hackett F.; Withers-Martinez C.; Mitchell G. H.; Bannister L. H.; Bryans J. S.; Kettleborough C. A.; Blackman M. J. (2007) Subcellular discharge of a serine protease mediates release of invasive malaria parasites from host erythrocytes. Cell 131 (6), 1072–83. 10.1016/j.cell.2007.10.049. [DOI] [PubMed] [Google Scholar]
- Harris P. K.; Yeoh S.; Dluzewski A. R.; O’Donnell R. A.; Withers-Martinez C.; Hackett F.; Bannister L. H.; Mitchell G. H.; Blackman M. J. (2005) Molecular identification of a malaria merozoite surface sheddase. PLoS Pathog. 1 (3), e29. 10.1371/journal.ppat.0010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee R.; Liu J.; Beatty W.; Pelosof L.; Klemba M.; Goldberg D. E. (2002) Four plasmepsins are active in the Plasmodium falciparum food vacuole, including a protease with an active-site histidine. Proc. Natl. Acad. Sci. U. S. A. 99 (2), 990–5. 10.1073/pnas.022630099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenai B. R.; Sijwali P. S.; Singh A.; Rosenthal P. J. (2000) Characterization of native and recombinant falcipain-2, a principal trophozoite cysteine protease and essential hemoglobinase of Plasmodium falciparum. J. Biol. Chem. 275 (37), 29000–10. 10.1074/jbc.M004459200. [DOI] [PubMed] [Google Scholar]
- Singh N.; Sijwali P. S.; Pandey K. C.; Rosenthal P. J. (2006) Plasmodium falciparum: biochemical characterization of the cysteine protease falcipain-2′. Exp. Parasitol. 112 (3), 187–92. 10.1016/j.exppara.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Sijwali P. S.; Shenai B. R.; Gut J.; Singh A.; Rosenthal P. J. (2001) Expression and characterization of the Plasmodium falciparum haemoglobinase falcipain-3. Biochem. J. 360 (2), 481–489. 10.1042/bj3600481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka T. Q.; Deu E.; Molina-Cruz A.; Ashburne M. J.; Ali O.; Suri A.; Kortagere S.; Bogyo M.; Williamson K. C. (2013) Plasmodium dipeptidyl aminopeptidases as malaria transmission-blocking drug targets. Antimicrob. Agents Chemother. 57 (10), 4645–52. 10.1128/AAC.02495-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F.; Krai P.; Deu E.; Bibb B.; Lauritzen C.; Pedersen J.; Bogyo M.; Klemba M. (2011) Biochemical characterization of Plasmodium falciparum dipeptidyl aminopeptidase 1. Mol. Biochem. Parasitol. 175 (1), 10–20. 10.1016/j.molbiopara.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggleson K. K.; Duffin K. L.; Goldberg D. E. (1999) Identification and characterization of falcilysin, a metallopeptidase involved in hemoglobin catabolism within the malaria parasite Plasmodium falciparum. J. Biol. Chem. 274 (45), 32411–7. 10.1074/jbc.274.45.32411. [DOI] [PubMed] [Google Scholar]
- Murata C. E.; Goldberg D. E. (2003) Plasmodium falciparum falcilysin: a metalloprotease with dual specificity. J. Biol. Chem. 278 (39), 38022–8. 10.1074/jbc.M306842200. [DOI] [PubMed] [Google Scholar]
- Sleebs B. E.; Gazdik M.; O’Neill M. T.; Rajasekaran P.; Lopaticki S.; Lackovic K.; Lowes K.; Smith B. J.; Cowman A. F.; Boddey J. A. (2014) Transition state mimetics of the Plasmodium export element are potent inhibitors of Plasmepsin V from P. falciparum and P. vivax. J. Med. Chem. 57 (18), 7644–62. 10.1021/jm500797g. [DOI] [PubMed] [Google Scholar]
- Hodder A. N.; Sleebs B. E.; Czabotar P. E.; Gazdik M.; Xu Y.; O’Neill M. T.; Lopaticki S.; Nebl T.; Triglia T.; Smith B. J.; Lowes K.; Boddey J. A.; Cowman A. F. (2015) Structural basis for plasmepsin V inhibition that blocks export of malaria proteins to human erythrocytes. Nat. Struct. Mol. Biol. 22 (8), 590–6. 10.1038/nsmb.3061. [DOI] [PubMed] [Google Scholar]
- Sleebs B. E.; Lopaticki S.; Marapana D. S.; O’Neill M. T.; Rajasekaran P.; Gazdik M.; Gunther S.; Whitehead L. W.; Lowes K. N.; Barfod L.; Hviid L.; Shaw P. J.; Hodder A. N.; Smith B. J.; Cowman A. F.; Boddey J. A. (2014) Inhibition of Plasmepsin V activity demonstrates its essential role in protein export, PfEMP1 display, and survival of malaria parasites. PLoS Biol. 12 (7), e1001897. 10.1371/journal.pbio.1001897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasamu A. S.; Glushakova S.; Russo I.; Vaupel B.; Oksman A.; Kim A. S.; Fremont D. H.; Tolia N.; Beck J. R.; Meyers M. J.; Niles J. C.; Zimmerberg J.; Goldberg D. E. (2017) Plasmepsins IX and X are essential and druggable mediators of malaria parasite egress and invasion. Science (Washington, DC, U. S.) 358 (6362), 518–522. 10.1126/science.aan1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amberg-Johnson K.; Hari S. B.; Ganesan S. M.; Lorenzi H. A.; Sauer R. T.; Niles J. C.; Yeh E. (2017) Small molecule inhibition of apicomplexan FtsH1 disrupts plastid biogenesis in human pathogens. eLife 6, e29865. 10.7554/eLife.29865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesner J.; Sanderbrand S.; Altincicek B.; Beck E.; Jomaa H. (2001) Seeking new targets for antiparasitic agents. Trends Parasitol. 17 (1), 7–8. 10.1016/S1471-4922(00)01735-9. [DOI] [PubMed] [Google Scholar]
- Goodman C. D.; McFadden G. I. (2014) Ycf93 (Orf105), a small apicoplast-encoded membrane protein in the relict plastid of the malaria parasite Plasmodium falciparum that is conserved in Apicomplexa. PLoS One 9 (4), e91178. 10.1371/journal.pone.0091178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhen K. L.; Chatterjee A. K.; Rottmann M.; Gagaring K.; Borboa R.; Buenviaje J.; Chen Z.; Francek C.; Wu T.; Nagle A.; Barnes S. W.; Plouffe D.; Lee M. C.; Fidock D. A.; Graumans W.; van de Vegte-Bolmer M.; van Gemert G. J.; Wirjanata G.; Sebayang B.; Marfurt J.; Russell B.; Suwanarusk R.; Price R. N.; Nosten F.; Tungtaeng A.; Gettayacamin M.; Sattabongkot J.; Taylor J.; Walker J. R.; Tully D.; Patra K. P.; Flannery E. L.; Vinetz J. M.; Renia L.; Sauerwein R. W.; Winzeler E. A.; Glynne R. J.; Diagana T. T. (2014) KAF156 is an antimalarial clinical candidate with potential for use in prophylaxis, treatment, and prevention of disease transmission. Antimicrob. Agents Chemother. 58 (9), 5060–7. 10.1128/AAC.02727-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.