Summary
Individuals receiving more Ryan White service classes are more likely to be retained in care and achieve viral suppression. For some populations with insurance, Ryan White services may still be required for optimal health outcomes.
Keywords: HIV/AIDS, Ryan White, care delivery, team care
Abstract
Background
Knowledge gaps remain about how the Ryan White human immunodeficiency virus (HIV)/AIDS Program (RW) contributes to health outcomes. We examined the association between different RW service classes and retention in care (RiC) or viral suppression (VS).
Methods
We identified Virginians engaged in any HIV care between 1 January and 31 December 2014. RW beneficiaries were classified by receipt of ≥1 service from 3 classes: Core medical, Support, and insurance and/or direct medication assistance through the AIDS Drug Assistance Program (ADAP). Receipt of all RW classes was defined as comprehensive assistance. We used multivariable logistic regression to compare the odds of RiC and of VS by comprehensive assistance and by RW classes alone and in combination.
Results
Among 13104 individuals, 58% received any RW service and 17% comprehensive assistance. Comprehensive assistance is significantly associated with RiC (adjusted odds ratio [aOR], 8.8 [95% confidence interval {CI}, 7.2–10.8]) and viral suppression (aOR, 3.3 [95% CI, 2.9–3.8]). Receiving any 2 RW classes or Core alone is significantly associated with RiC and VS, with the strength of association decreasing as the number of classes decreases. Recipients of Support alone are significantly less likely to have VS (aOR, 0.75 [95% CI, .59–.96]). For ADAP recipients also receiving Core and/or Support, insurance assistance is significantly associated with VS compared to receiving direct medication only (aOR, 1.6 [95% CI, 1.3–1.9]); this relationship is not significant for those who receive ADAP alone.
Conclusions
Receiving more classes of RW-funded services is associated with improved HIV outcomes. For some populations with insurance, RW-funded services may still be required for optimal health outcomes.
The federal Ryan White human immunodeficiency virus (HIV)/AIDS Program (RW) supports care services for uninsured and underinsured persons living with human immunodeficiency virus (PLWH). A national model for comprehensive, coordinated care [1–3], RW funds a broad spectrum of services that can be categorized into 3 major classes: core medical services, supportive services, and direct or indirect provision of medications (eg, health insurance premium or cost-sharing assistance) through RW’s AIDS Drug Assistance Program (ADAP) [4, 5]. While cost-sharing assistance has existed since the program’s inception, this provision has played a more prominent role since the passing of the 2010 Patient Protection and Affordable Care Act (ACA), which expanded health insurance access through public health insurance marketplaces and amended Medicaid eligibility requirements [6, 7].
RW remains a critical mechanism through which to provide care for PLWH [7–13], especially in Medicaid nonexpansion states [14]. A strong evidence base suggests an important and ongoing role for the program. RW assistance has been associated with increased retention in care [15], greater receipt of antiretroviral therapy [16, 17], and improved viral suppression [15, 17, 18].
Although evidence is strong about the health benefits associated with receipt of any RW service, little is known about how receipt of different classes of RW assistance influences outcomes along the HIV care continuum, a framework for assessing population health outcomes among PLWH [19]. Leveraging HIV surveillance data from Virginia, a Medicaid nonexpansion state, we examined the relationship between comprehensive care assistance (ie, receipt of all classes of RW assistance), as well as individual classes of RW services alone and in combination, and 2 outcomes: retention in HIV care and viral suppression among PLWH.
METHODS
Data
We used individual-level demographic and health outcome data from the Care Markers Database (“Database”), which is maintained by the Virginia Department of Health. The Database compiles routine HIV surveillance data for PLWH and HIV care and service encounter data for individuals receiving RW assistance, along with calendar dates of care marker data (CD4 cell count, viral load test, HIV-related medical visit, and receipt of antiretroviral prescription) and viral load test results from the Medical Monitoring Project [20]. Through data-sharing agreements, the Database is also populated with CD4 cell count and viral load test results from jurisdictions outside Virginia and calendar dates of CD4 cell count and viral load tests, and antiretroviral prescriptions from the state Medicaid office [21]. Vital status data come from the Department of Health’s Division of Vital Statistics, the National Death Index, the Social Security Death Master File, routine updates from other jurisdictions, and matching with LexisNexis Accurint [22].
Study Population
The study population comprised PLWH in Virginia who met the following criteria: ≥13 years of age and diagnosed with HIV by 31 December 2013; and ≥1 care marker reported between 1 January and 31 December 2014. We defined a care marker as a CD4 cell count and/or viral load test result, antiretroviral prescription, or HIV-related medical visit. We limited the analytic sample to individuals with ≥1 care marker during 2014 to ensure an appropriate comparator of HIV-infected individuals not receiving RW-funded services but engaged in care.
Ryan White Eligibility and Classes of Ryan White Services
In Virginia, one of the eligibility criteria for PLWH to receive RW services is income <400% of the federal poverty level. To further qualify for ADAP assistance, individuals must not be eligible for, or receive, Medicaid assistance [23].
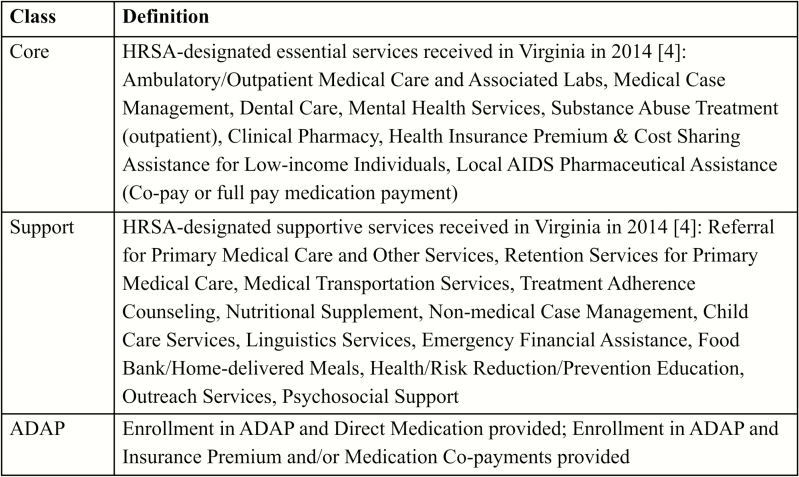
We categorized RW services received during 2014 into 1 of 3 classes [4, 5]: Core, Support, and ADAP (Figure 1). We then classified individuals by the types of services received. Individuals were classified as Core or Support if they received ≥1 Core service or ≥1 Support service, respectively; individuals classified as ADAP received ≥1 month of ADAP services. This classification method focuses on the type of service(s) received vs the number of service encounters. Our primary variable of interest, comprehensive care assistance, was defined as receipt of all 3 classes of RW services—Core, Support, and ADAP.
Figure 1.
Definitions of 3 classes of Ryan White–funded services in Virginia. The definitions reflect services received by Ryan White beneficiaries between 1 January and 31 December 2014, in Virginia. AIDS Drug Assistance Program includes direct medication, premium payments for approved 2010 Patient Protection and Affordable Care Act (ACA) plans, premium payments for Medicare Part D plans, and medication co-payments for ACA, Medicare Part D, and private insurance plans. Abbreviations: ADAP, AIDS Drug Assistance Program; HRSA, Health Resources and Services Administration.
Outcome Measures
We constructed 2 dichotomous outcome measures—retention in HIV care and viral suppression—which reflect key steps along the HIV care continuum in Virginia and nationally [12]. We defined retention in HIV care as ≥2 care markers at least 90 days apart during 2014 [24]. Our second outcome measure, viral suppression, was defined as the last viral load in 2014 ≤200 copies/mL [24]. We assumed that PLWH without a reported viral load test result during 2014 were not virally suppressed, but examined this assumption in secondary analysis.
Statistical Analysis
We reported frequencies and percentages for each sociodemographic and clinical variable by receipt of comprehensive care assistance. Bivariable and multivariable logistic regression compared the odds of retention in care and the odds of viral suppression by receipt of comprehensive care assistance. Multivariable models controlled for sex at birth, categorical age as of 31 December 2014, race and ethnicity, health region of residence in Virginia, HIV transmission risk factor, AIDS diagnosis, and time since HIV diagnosis. To minimize collinearity, we verified that age in its continuous form and time since HIV diagnosis were not highly correlated (r < 0.70) using the Spearman correlation coefficient. Statistical significance was assessed using 95% confidence intervals (CIs). All analyses were performed using SAS software version 9.3 (SAS Institute, Cary, North Carolina).
We used multivariable logistic regression to conduct secondary analysis. First, we restricted our sample to only those PLWH with reported viral load test results during calendar year 2014, to assess our assumption that those missing a viral load test result were not virally suppressed. Second, we included a binary variable for receipt of any HIV care during 2013 to control for previous HIV care status. Third, we restricted the study population to those who received any RW services to examine the impact of receiving comprehensive care assistance vs receipt of some, but not all, classes of RW services. Fourth, we assessed the relationship between different RW service classes or combinations of classes and our outcomes by creating 8 mutually exclusive RW service categories (Table 1). Finally, we examined the relationship between type of ADAP assistance (any insurance assistance vs direct medication only) and viral suppression. Any insurance assistance included premium payments for ACA plans, premium payments for Medicare Part D plans, and medication co-payments for ACA, Medicare Part D, and private insurance plans. Here, we separately assessed those receiving only ADAP services and those receiving ADAP services in addition to other RW services.
Table 1.
Combinations of Classes of Ryan White–Funded Services Examined in Secondary Analysis
| Combination | Class of Ryan White–Funded Service | Sample Size | (%) | ||
|---|---|---|---|---|---|
| ≥1 Core | ≥1 Support | ≥1 month ADAP | |||
| 1 | X | 855 | (6.5) | ||
| 2 | X | 298 | (2.3) | ||
| 3 | X | 1098 | (8.4) | ||
| 4 | X | X | 1536 | (11.7) | |
| 5 | X | X | 1353 | (10.3) | |
| 6 | X | X | 178 | (1.4) | |
| 7a | X | X | X | 2228 | (17.0) |
| 8 | 5558 | (42.4) | |||
Abbreviation: ADAP, AIDS Drug Assistance Program.
aIndividuals receiving all classes of services were defined as receiving Comprehensive Care Assistance.
RESULTS
Sample Characteristics
We identified 24052 PLWH in Virginia as of 31 December 2014. Of these, we excluded 928 due to an HIV diagnosis during 2014, 40 because they were aged <13 years, and 9980 due to lack of a care marker. Of the 13104 PLWH eligible for inclusion in our analytic sample, 7546 (57.6%) received any RW service and 2228 (17.0%) received comprehensive care assistance. The majority of the analytic sample was male (71.3%) and black (61.0%), with a history of an AIDS diagnosis (54.8%). Male-to-male sexual contact was the most highly represented transmission risk factor (48.2%), followed by high-risk heterosexual contact (22.7%).
Supplementary Table 1 shows the frequencies and percentages of the study population by comprehensive care assistance. Compared to PLWH who did not receive comprehensive care assistance in 2014, recipients of comprehensive care assistance were more often aged <40 years (30.5% vs 25.1%; P < .0001), retained in care (95.4% vs 70.6%; P < .0001), and virally suppressed (88.2% vs 62.8%; P < .0001). Recipients of comprehensive care assistance were also more likely to be Hispanic/Latino (15.6% vs 5.6%; P < .0001), less likely to be black (53.3% vs 62.5%; P < .0001), and less likely to be living in Virginia’s Eastern region (8.2% vs 34.4%; P < .0001).
Comprehensive Care Assistance
Comprehensive care assistance was significantly associated with retention in HIV care and viral suppression in both unadjusted and adjusted analyses (Table 2). In adjusted analysis, PLWH receiving comprehensive care assistance had nearly 9 times the odds of being retained in care compared to those not receiving comprehensive care assistance (adjusted odds ratio [aOR], 8.8 [95% CI, 7.2–10.8]). Likewise, individuals receiving comprehensive care assistance had >3 times the odds of viral suppression (aOR, 3.3 [95% CI, 2.9–3.8]).
Table 2.
Association of Comprehensive Care Assistance and Either Retention in Human Immunodeficiency Virus (HIV) Care or Viral Suppression Among HIV-Infected Individuals Living in Virginia
| Characteristic | No. | Retention in Care | Viral Suppression | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | aOR, P Value | OR (95% CI) | aOR (95% CI) | aOR, P Value | ||
| All | 13104 | ||||||
| Comprehensive care assistance | |||||||
| No | 10876 | Reference | Reference | Reference | Reference | ||
| Yes | 2228 | 8.61 (7.03–10.53) | 8.81 (7.16–10.84) | <.0001 | 4.45 (3.89–5.09) | 3.28 (2.85–3.78) | <.0001 |
| Sex at birtha | |||||||
| Male | 9338 | Reference | Reference | Reference | Reference | ||
| Female | 3766 | 1.17 (1.07–1.28) | 1.25 (1.11–1.42) | .0004 | 0.90 (.83–.97) | 0.87 (.77–.97) | .016 |
| Age as of 31 December 2014, ya | |||||||
| 13–29 | 1295 | 1.05 (.90–1.23) | 0.90 (.75–1.08) | .257 | 0.69 (.60–.80) | 0.61 (.51–.72) | <.0001 |
| 30–39 | 2119 | 1.07 (.93–1.23) | 0.97 (.83–1.14) | .723 | 0.90 (.79–1.02) | 0.84 (.72–.97) | .016 |
| 40–49 | 3400 | 1.07 (.95–1.21) | 0.98 (.86–1.12) | .764 | 0.97 (.87–1.10) | 0.90 (.79–1.02) | .109 |
| 50–59 | 4237 | 1.19 (1.06–1.35) | 1.13 (1.00–1.28) | .055 | 1.02 (.91–1.14) | 1.01 (.90–1.14) | .877 |
| ≥60 | 2053 | Reference | Reference | Reference | Reference | ||
| Race/ethnicitya | |||||||
| White | 3717 | Reference | Reference | Reference | Reference | ||
| Black | 7988 | 1.16 (1.06–1.27) | 1.23 (1.11–1.36) | <.0001 | 0.76 (.70–.83) | 0.93 (.84–1.02) | .108 |
| Hispanic | 955 | 1.13 (.96–1.33) | 1.06 (.89–1.28) | .506 | 1.26 (1.07–1.48) | 1.06 (.89–1.27) | .533 |
| Other | 444 | 0.99 (.80–1.24) | 1.11 (.88–1.41) | .369 | 0.88 (.71–1.09) | 0.92 (.73–1.16) | .479 |
| Transmission risk factora,b | |||||||
| HET | 2969 | Reference | Reference | Reference | Reference | ||
| MSM | 6322 | 0.82 (.74–.91) | 1.04 (.90–1.19) | .634 | 1.00 (.91–1.10) | 0.91 (.80–1.04) | .162 |
| IDU | 1064 | 0.99 (.83–1.17) | 1.05 (.87–1.25) | .627 | 1.12 (.96–1.30) | 1.14 (.97–1.35) | .118 |
| MSM and IDU | 521 | 0.89 (.71–1.10) | 0.99 (.78–1.27) | .945 | 1.03 (.84–1.25) | 0.87 (.69–1.09) | .231 |
| Other/unknown | 2228 | 0.62 (.55–.70) | 0.70 (.61–.80) | <.0001 | 0.84 (.75–.94) | 0.95 (.83–1.07) | .382 |
| Region of diagnosisa,c | |||||||
| Eastern | 3921 | Reference | Reference | Reference | Reference | ||
| Central | 3497 | 2.08 (1.87–2.32) | 1.78 (1.59–1.99) | <.0001 | 3.74 (3.39–4.13) | 3.38 (3.05–3.74) | <.0001 |
| Northern | 2981 | 0.90 (.81–.99) | 0.67 (.60–.75) | <.0001 | 3.56 (3.21–3.95) | 2.89 (2.59–3.22) | <.0001 |
| Northwest | 1207 | 2.65 (2.23–3.15) | 2.00 (1.67–2.39) | <.0001 | 5.46 (4.66–6.40) | 4.30 (3.65–5.07) | <.0001 |
| Southwest | 1300 | 2.73 (2.31–3.23) | 2.21 (1.86–2.64) | <.0001 | 4.55 (3.93–5.28) | 3.75 (3.22–4.37) | <.0001 |
| Unknown | 198 | 0.88 (.65–1.19) | 0.85 (.62–1.15) | .287 | 2.78 (2.04–3.79) | 2.60 (1.90–3.56) | <.0001 |
| Disease stagea | |||||||
| AIDS diagnosisd | 7177 | Reference | Reference | Reference | Reference | ||
| No history of AIDS diagnosis | 5927 | 0.83 (.77–.90) | 0.83 (.76–.91) | <.0001 | 0.94 (.87–1.01) | 1.02 (.94–1.11) | .591 |
| Years since HIV diagnosisa | 13104 | 1.00 (.99–1.00) | 0.99 (.99–1.00) | .046 | 1.00 (.99–1.00) | 0.99 (.98–.99) | .0002 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; HET, high-risk heterosexual contact; HIV, human immunodeficiency virus; IDU, injection drug use; MSM, men who have sex with men; OR, odds ratio.
aClient characteristic based on data from Virginia’s Care Markers Database.
bClient’s most likely route of HIV infection; assessed through patient interviews and medical record abstraction shortly after the time HIV diagnosis is reported to the state surveillance system.
cVirginia is divided into 5 geographic regions for health planning purposes: Central, Eastern, Northern, Northwest, Southwest.
dAny CD4 count ≤200 cells/µL or AIDS-defining opportunistic infection since HIV diagnosis.
When we restricted our sample to PLWH with ≥1 viral load laboratory result (n = 10389), the direction, magnitude, and significance of the relationship between comprehensive care assistance and both outcomes of interest remained similar. This suggests that our results were not sensitive to the assumption that, in our sample, PLWH with missing viral load test results were not suppressed. Likewise, our findings were not sensitive to receipt of any HIV care during 2013. In analyses restricted to PLWH who received any RW assistance (n = 7546), comprehensive care assistance remained significantly associated with both retention in care and viral suppression compared to those who received some, but not all, classes of RW services. However, the effect size was smaller (retention in care: aOR, 2.8 [95% CI, 2.3–3.6]; viral suppression: aOR, 2.5 [95% CI, 2.1–2.9]).
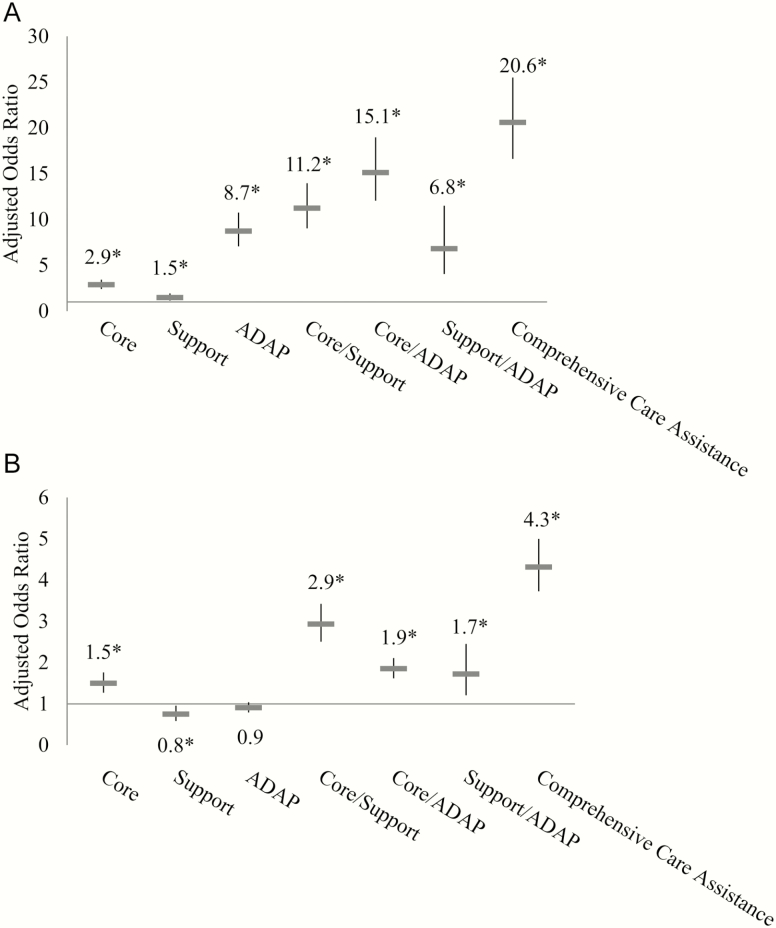
Individual and Combinations of Ryan White Service Classes
The proportion retained in HIV care varied significantly across different combinations of classes of RW services, from 70.1% (Support only) to 95.4% (comprehensive care assistance). In multivariable logistic regression, all combinations of classes of RW services were positively, and significantly, associated with retention in care compared to those not receiving RW services (Figure 2A). Those receiving comprehensive care assistance had >20 times the odds of being retained in HIV care (aOR, 20.6 [95% CI, 16.6–25.5]), and individuals who received 2 classes of RW services also had greater odds of being retained in HIV care (Core/Support: aOR, 11.2 [95% CI, 9.0–14.0]; Core/ADAP: aOR, 15.1 [95% CI, 12.1–19.0]; Support/ADAP: aOR, 6.8 [95% CI, 4.0–11.5]), compared to those who did not receive RW services. Similarly, PLWH receiving only one class of RW services had greater odds of being retained in care, although the strength of the association was generally smaller than for other combinations of classes (Core only: aOR, 2.9 [95% CI, 2.4–3.5]; Support only: aOR, 1.5 [95% CI, 1.1–1.9]; ADAP only: aOR, 8.7 [95% CI, 7.1–10.8]).
Figure 2.
Influence of different classes of Ryan White services on 2 human immunodeficiency virus (HIV) clinical care outcomes. This figure shows the impact of 7 different combinations of classes of Ryan White services on retention in HIV care (A) and viral suppression (B) compared to no Ryan White services. On the x-axis are different mutually exclusive combinations of Ryan White service classes; the y-axis shows adjusted odds ratios and confidence intervals from multivariable logistic regression controlling for sex at birth, age, race/ethnicity, HIV transmission risk factor, region, AIDS diagnosis, and years since HIV diagnosis. An asterisk (*) indicates statistical significance at the P < .05 level. All combinations of classes of Ryan White services were positively and significantly associated with retention in care, with comprehensive care assistance having the strongest association. There was no significant relationship between ADAP-only services and viral suppression, and support services only were negatively, and significantly, associated with viral suppression. All other combinations of classes of Ryan White services were positively and significantly associated with viral suppression, with comprehensive care assistance having the strongest association. Abbreviations: ADAP, AIDS Drug Assistance Program; HIV, human immunodeficiency virus.
The proportion virally suppressed also varied significantly across different combinations of classes of RW services, ranging from 49.9% (ADAP only) to 88.2% (comprehensive care assistance). In multivariable logistic regression (Figure 2B), PLWH receiving comprehensive care assistance had >4 times the odds of viral suppression compared to those not receiving RW services (aOR, 4.3 [95% CI, 3.7–5.0]). A positive and significant association was also observed for recipients of 2 service classes: Core/Support (aOR, 2.9 [95% CI, 2.5–3.4]), Core/ADAP (aOR, 1.9 [95% CI, 1.6–2.1]), and Support/ADAP (aOR, 1.7 [95% CI, 1.2–2.5]). This relationship held for PLWH receiving Core services alone (aOR, 1.5 [95% CI, 1.3–1.8]). However, those receiving Support services only had lower odds of viral suppression compared to those who did not receive any RW services (aOR, 0.75 [95% CI, .59–.96]). There was not a statistically significant relationship between those who received ADAP services only and viral suppression (aOR, 0.91 [95% CI, .79–1.0]).
Insurance Assistance and Viral Suppression Among AIDS Drug Assistance Program Recipients
Of 4857 persons receiving any ADAP services in 2014, more than one-fifth (1098) received ADAP services only, with no additional receipt of RW services. Among these individuals, more than half (610 [55.6%]) received any insurance assistance, with the remainder receiving direct medication only. Among the population receiving only ADAP services, there was no relationship between receipt of any insurance assistance and viral suppression compared with those receiving direct medication only (aOR, 0.98 [95% CI, .75–1.3]). However, when we considered those who received ADAP services in addition to other RW services (n = 3759), individuals receiving any insurance assistance (2277 [60.6%]) had greater odds of viral suppression than those receiving direct medication only (aOR, 1.6 [95% CI, 1.3–1.9]).
DISCUSSION
While existing evidence suggests that RW services are associated with health benefits, little is known about how different classes of RW assistance influence key health indicators. We examined the relationship between receiving comprehensive care assistance and 2 outcomes: retention in HIV care and viral suppression. Relative to receiving no RW services, receiving comprehensive care assistance was associated with the largest odds of retention in care and viral suppression. Smaller, but significant, relationships were found among those who received any 2 classes of services compared to those receiving no RW services. Receiving just one class of RW services was consistently, and positively, associated with retention in care, but not viral suppression. Thus, as the variety of RW service classes received increases, the health benefits appear to increase accordingly.
This work contributes to an increasing evidence base indicating a strong, positive relationship between RW assistance and health outcomes along the HIV care continuum. For example, the literature suggests that among the uninsured, those who receive RW assistance are twice as likely to be virally suppressed [17]. Rates of care retention are higher for those receiving RW-funded services compared to national estimates [15]. RW-funded facilities are more likely to offer a variety of support services, and patients attending those facilities are more likely to report using the support services [18, 25, 26]. Collectively, these studies suggest an integral role for RW assistance in the achievement of HIV care continuum outcomes. Our work builds on this evidence by detailing and examining the full scope of RW assistance, and it improves knowledge on the relationship between different classes of RW assistance and health indicators.
This study provides insight into the potential consequences of fragmented HIV care. We found that receiving Support services alone was negatively, and significantly, associated with viral suppression compared to receiving no RW services. Recent literature supports a strong relationship between coordinated care and receipt of antiretroviral prescriptions, retention in care, and viral suppression [17, 27]. RW services are often highly coordinated by provider teams that include HIV specialists, and the RW program supports services that many public or private insurance plans do not cover [8, 18, 28]. Therefore, individuals who exclusively receive RW assistance for their HIV care may have better service coordination, and more exposure to RW HIV specialty care, than those who only receive RW Support services [17]. Additionally, our data reflect the first year in which low-income PLWH were able to acquire RW-supported insurance coverage through marketplace subsidies. As RW cost-sharing assistance evolves, the role of multiple payers in the receipt of fragmented HIV care should be considered.
Results suggest that among PLWH, insurance alone may not be sufficient to improve health outcomes. A previous study found that ADAP enrollees transitioning from direct medication assistance to a qualified health insurance plan were more likely to achieve viral suppression compared to ADAP enrollees not enrolled in a qualified health plan [6]. This study built on these results by stratifying the sample of ADAP enrollees into those who received ADAP only and those who received ADAP in addition to other RW services. We found that insurance assistance was indeed associated with higher odds of viral suppression compared to direct medication assistance, but only for those who received ADAP support plus other RW services, and not for those receiving ADAP only. While insurance coverage is associated with health benefits for people living with chronic diseases, including HIV [29], our findings indicate that these benefits may occur in conjunction with receipt of other RW-funded services.
This study has limitations. First, as an observational, cross-sectional study, our results lack the temporality to establish causation and the design does not account for all concurrent and historical exposures that may have contributed to our findings. Specifically, the longitudinal relationship between RW assistance and retention in care or viral suppression deserves attention. Second, we lack socioeconomic data, such as income and education, for the non-RW reference population. However, if we could select a non-RW reference sample with the same socioeconomic composition as the RW population, we believe it would reflect a population of low-income individuals who qualify for RW services but have no evidence of their receipt, and who likely have worse outcomes. Consequently, substituting the non-RW, low-income sample for the original non-RW reference population may strengthen the existing positive relationships between receipt of RW services and the outcomes. Therefore, our results may be conservative estimates. Our data also did not capture insurance enrollment for non-RW recipients or fully capture insurance enrollment for RW clients, which will be important for understanding the relationship between our outcomes and different insurers and insurance coverage options. Third, because Virginia is a Medicaid nonexpansion state, our findings may not reflect the experience of states with expanded public insurance. Fourth, there are limitations related to the RW service class definitions. For example, the ADAP service class categorizes recipients of 1 month and 12 months of ADAP services identically, which may underestimate the influence of more continuous ADAP coverage. While we did not find a significant relationship between receipt of ADAP services only and viral suppression, a positive relationship may emerge if continuous or long-term ADAP receipt is specifically investigated. Also, some service overlap exists between the 3 classes we created. For example, provision of antiretroviral medication is predominantly covered by ADAP, but may also be provided through limited cost-sharing in certain Core and Support services. Finally, this study did not assess the influence of specific combinations of individual services on retention in care and viral suppression. Future work can examine how combinations of individual services, both within and across classes, impact HIV health outcomes.
RW serves an essential role in the care of low-income PLWH. Our study suggests that the more classes of RW services an individual receives, the more likely that individual will remain in care and achieve viral suppression. In particular, RW-funded services may still be needed for optimal outcomes, even when insurance is available. As different insurance coverage options evolve or become available to PLWH, future research should examine the impact of fragmented care, especially during periods of insurance transition, on health outcomes. Given a national goal to increase access to HIV care and reduce new HIV infections, comprehensive care assistance through the RW program promises critical and ongoing contributions to improved population health for PLWH.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Notes
Acknowledgments. The authors thank Kimberly Scott at the Virginia Department of Health for her thoughtful and critical review of the manuscript.
Disclaimer. The funding sources played no role in the study, including study design; collection, analysis, and/or interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Financial support. This work was supported by the Health Resources and Services Administration (award number H97HA27534); the National Institutes of Health (National Institute on Minority Health and Health Disparities, award number R01 MD011277); and an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists and funded by the Centers for Disease Control and Prevention (cooperative agreement U38 OT000143).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Beane SN, Culyba RJ, DeMayo M, Armstrong W. Exploring the medical home in Ryan White HIV care settings: a pilot study. J Assoc Nurses AIDS Care 2014; 25:191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gallant JE, Adimora AA, Carmichael JK, et al. ; Infectious Diseases Society of America; Ryan White Medical Providers Coalition Essential components of effective HIV care: a policy paper of the HIV Medicine Association of the Infectious Diseases Society of America and the Ryan White Medical Providers Coalition. Clin Infect Dis 2011; 53:1043–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Saag MS. Ryan White: an unintentional home builder. AIDS Read 2009; 19:166–8. [PubMed] [Google Scholar]
- 4. Health Resources and Services Administration. Ryan White HIV/AIDS Program part B manual Available at: http://hab.hrsa.gov/manageyourgrant/files/habpartbmanual2013.pdf Accessed 11 October 2016.
- 5. Health Resources and Services Administration. AIDS Drug Assistance Program (ADAP) manual Available at: http://hab.hrsa.gov/manageyourgrant/adapmanual.pdf Accessed 11 October 2016.
- 6. McManus KA, Rhodes A, Bailey S, et al. Affordable Care Act qualified health plan coverage: association with improved HIV viral suppression for AIDS drug assistance program clients in a Medicaid nonexpansion state. Clin Infect Dis 2016; 63:396–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Crowley J, Kates J. Updating the Ryan White HIV/AIDS Program for a new era: key issues and questions for the future. Menlo Park, CA: Kaiser Family Foundation, 2013. [Google Scholar]
- 8. Cahill SR, Mayer KH, Boswell SL. The Ryan White HIV/AIDS Program in the age of health care reform. Am J Public Health 2015; 105:1078–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eaton EF, Mugavero MJ. Affordable Care Act, Medicaid expansion … or not: Ryan White Care Act remains essential towards access and equity. Clin Infect Dis 2016; 63:404–6. [DOI] [PubMed] [Google Scholar]
- 10. Leibowitz AA, Lester R, Curtis PG, et al. Early evidence from California on transitions to a reformed health insurance system for persons living with HIV/AIDS. J Acquir Immune Defic Syndr 2013; 64suppl 1:S62–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Morin SF. The future of the Ryan White HIV/AIDS program. JAMA Intern Med 2015; 175:1660–1. [DOI] [PubMed] [Google Scholar]
- 12. Office of National AIDS Policy. National HIV/AIDS strategy for the United States: updated to 2020 Available at: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/overview/index.html Accessed 11 October 2016.
- 13. Sood N, Juday T, Vanderpuye-Orgle J, et al. HIV care providers emphasize the importance of the Ryan White Program for access to and quality of care. Health Aff 2014; 33:394–400. [DOI] [PubMed] [Google Scholar]
- 14. Berry SA, Fleishman JA, Yehia BR, et al. ; HIV Research Network Healthcare coverage for HIV provider visits before and after implementation of the Affordable Care Act. Clin Infect Dis 2016; 63:387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Doshi RK, Milberg J, Isenberg D, et al. High rates of retention and viral suppression in the US HIV safety net system: HIV care continuum in the ryan white HIV/AIDS program, 2011. Clin Infect Dis 2015; 60:117–25. [DOI] [PubMed] [Google Scholar]
- 16. Moore RD, Keruly JC, Bartlett JG. Improvement in the health of HIV-infected persons in care: reducing disparities. Clin Infect Dis 2012; 55:1242–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bradley H, Viall AH, Wortley PM, Dempsey A, Hauck H, Skarbinski J. Ryan White HIV/AIDS Program assistance and HIV treatment outcomes. Clin Infect Dis 2016; 62:90–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weiser J, Beer L, Frazier EL, et al. Service delivery and patient outcomes in Ryan White HIV/AIDS Program-funded and -nonfunded health care facilities in the United States. JAMA Intern Med 2015; 175:1650–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011; 52:793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Blair JM, McNaghten AD, Frazier EL, Skarbinski J, Huang P, Heffelfinger JD. Clinical and behavioral characteristics of adults receiving medical care for HIV infection—Medical Monitoring Project, United States, 2007. MMWR Surveill Summ 2011; 60:1–20. [PubMed] [Google Scholar]
- 21. Ocampo JM, Smart JC, Allston A, et al. Improving HIV surveillance data for public health action in Washington, DC: a novel multiorganizational data-sharing method. JMIR Public Health Surveill 2016; 2:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. LexisNexis Accurint. Available at: http://www.accurint.com/ Accessed 6 December 2016.
- 23. Virginia Department of Health. ADAP eligibility Available at: http://www.vdh.virginia.gov/disease-prevention/eligibility/ Accessed 11 October 2016.
- 24. Health Resources and Services Administration. HIV/AIDS Bureau HIV performance measures Available at: http://hab.hrsa.gov/deliverhivaidscare/habperformmeasures.html Accessed 11 October 2016.
- 25. Sullivan PS, Denniston M, Mokotoff E, Buskin S, Broyles S, McNaghten AD. Quality of care for HIV infection provided by Ryan White Program-supported versus non-Ryan White Program-supported facilities. PLoS One 2008; 3:e3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Valverde E, Del Rio C, Metsch L, et al. Characteristics of Ryan White and non-Ryan White funded HIV medical care facilities across four metropolitan areas: results from the antiretroviral treatment and access studies site survey. AIDS Care 2004; 16:841–50. [DOI] [PubMed] [Google Scholar]
- 27. Irvine MK, Chamberlin SA, Robbins RS, et al. Improvements in HIV care engagement and viral load suppression following enrollment in a comprehensive HIV care coordination program. Clin Infect Dis 2015; 60:298–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kates J. Implications of the Affordable Care Act for people with HIV infection and the Ryan White HIV/AIDS Program: what does the future hold? Top Antivir Med 2013; 21:138–42. [PMC free article] [PubMed] [Google Scholar]
- 29. McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q 2009; 87:443–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.