Abstract
Purpose
To evaluate the relationship between central corneal thickness (CCT) and horizontal corneal diameter (HCD) in eyes with uveal coloboma and microcornea.
Patients and methods
All adult patients with uveal coloboma having microcornea in at least one eye and seen between May 2014 and July 2016 at the cataract clinic of our tertiary eye care center were evaluated. The study group comprised 26 colobomatous eyes of 15 patients who had associated microcornea. The control group comprised eyes with uveal coloboma and normal-sized cornea (n=12 eyes of 9 patients). The main outcome measure included the relationship between CCT and HCD in eyes with uveal coloboma and microcornea.
Results
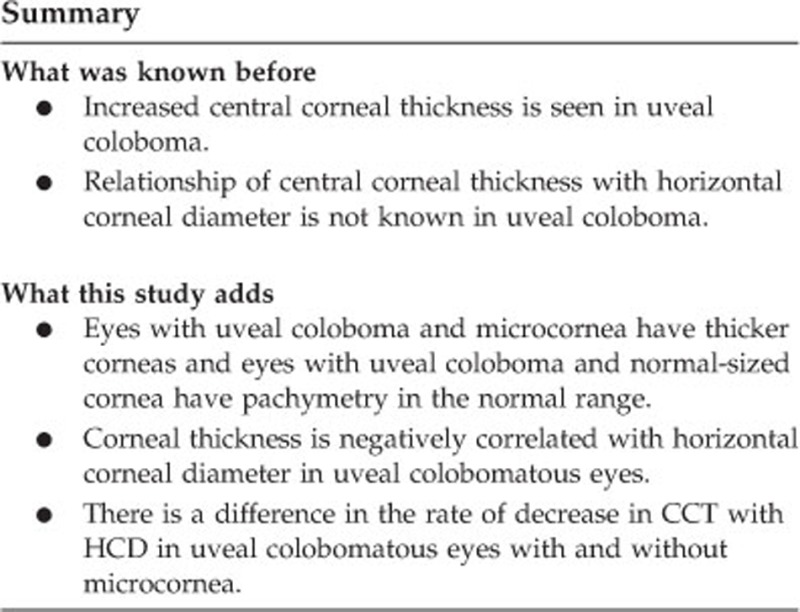
The mean HCD of the study and control groups was 6.97±1.28 and 11.39±0.67 mm, respectively. The mean central pachymetry of the study group was 668.4±40.2 μm compared with 555.3±41.8 μm in the control group. In both the groups, CCT was negatively correlated with HCD (R=−0.62 in the study group and R=−0.72 in the control group).
Conclusions
Uveal colobomatous eyes with microcornea have thicker corneas compared with uveal colobomatous eyes with normal diameter corneas that have normal central corneal thickness. In all the eyes with uveal coloboma, there is a negative correlation between horizontal corneal diameter and central corneal thickness.
Introduction
Uveal coloboma is a congenital condition characterized by a defective closure of the embryonic fissure of the optic cup during development.1 It can be associated with a normal-sized cornea (diameter >10 mm) or a microcornea (diameter <10 mm). The colobomatous eyes have a predisposition to early cataract formation and may require cataract surgery in early age.2 Increased central corneal thickness (CCT) has been earlier reported in four patients with uveal coloboma.3 The relationship of CCT with horizontal corneal diameter (HCD) has not been ascertained in these eyes. An observation that we made in our clinical practice was that the cornea was found to be thicker in the colobomatous eyes that were associated with microcornea. However, these colobomatous eyes with normal-sized cornea appeared to have lower values of corneal pachymetry than those associated with microcornea. In view of this clinical observation, we decided to test the differences in corneal thickness and also the relationship between CCT and HCD in coloboma eyes associated with and without microcornea.
The purpose of this study was to evaluate the relationship between CCT and HCD in the eyes with coloboma that had microcornea or had a normal corneal diameter.
Materials and methods
The Institutional Ethics Committee of LV Prasad Eye Institute, Hyderabad, India, approved the study protocol. The study was performed in accordance with the ethical standards laid down in the Declaration of Helsinki and informed consent was obtained from all subjects. All adult patients with uveal coloboma having microcornea in at least one eye and seen between May 2014 and July 2016 at the cataract clinic of our tertiary eye care center were evaluated. The study group comprised 26 colobomatous eyes of 15 patients who had associated microcornea. The control group comprised eyes with uveal coloboma and normal-sized cornea (n=12 eyes of 9 patients).
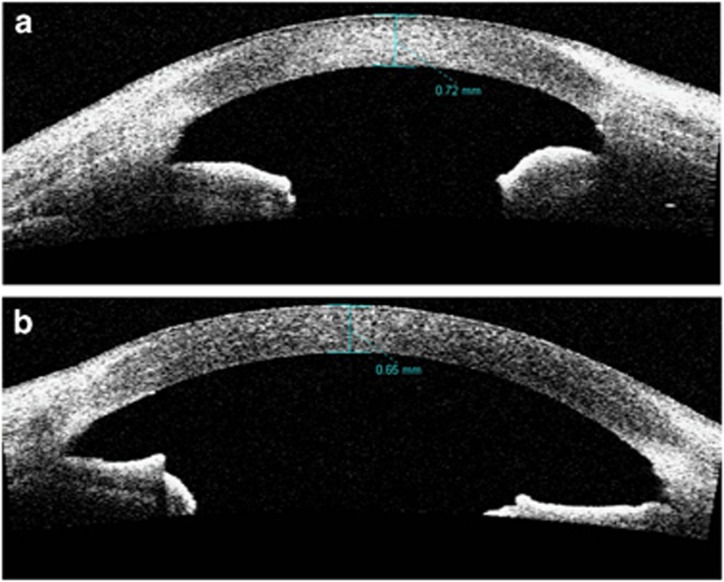
Microcornea was defined as HCD <10 mm and was measured using an IOL master (Carl Zeiss Meditec, Jena, Germany) preoperatively and Castroviejo calipers (E2404; Storz Ophthalmics, Tuttlingen, Germany) intraoperatively at the time of cataract surgery. The pachymetry was assessed using the caliper tool of an anterior segment optical coherence tomography (AS-OCT; Zeiss Visante OCT, Carl Zeiss Meditec, Jena, Germany). Figure 1a and b shows two representative AS-OCT images of eyes with uveal coloboma and bilateral microcornea.
Figure 1.
Anterior segment optical coherence tomography images of two representative eyes with uveal coloboma and bilateral microcornea. (a) Right eye of a subject where horizontal corneal diameter was 6 mm. (b) Left eye of a subject where horizontal corneal diameter was 7.5 mm.
Statistical analysis
The data analysis was performed using the statistical software Origin v7.0 (OriginLab Corporation, Northampton, MA, USA). Continuous data were checked for normality using Shapiro–Wilk test and were described using mean and SD (parametric data) or median and interquartile range (nonparametric data). The variances between two data sets were checked for equality using the Levene test. Independent t-test was used to compare parametric data with equal variance. Mann–Whitney test was used to compare parametric data with unequal variance and nonparametric data. Fisher’s exact test was used to compare the categorical data. Linear regression analysis was performed to evaluate the relationship between HCD and CCT. All the statistical tests were two sided and a P-value of <0.05 was considered statistically significant.
Results
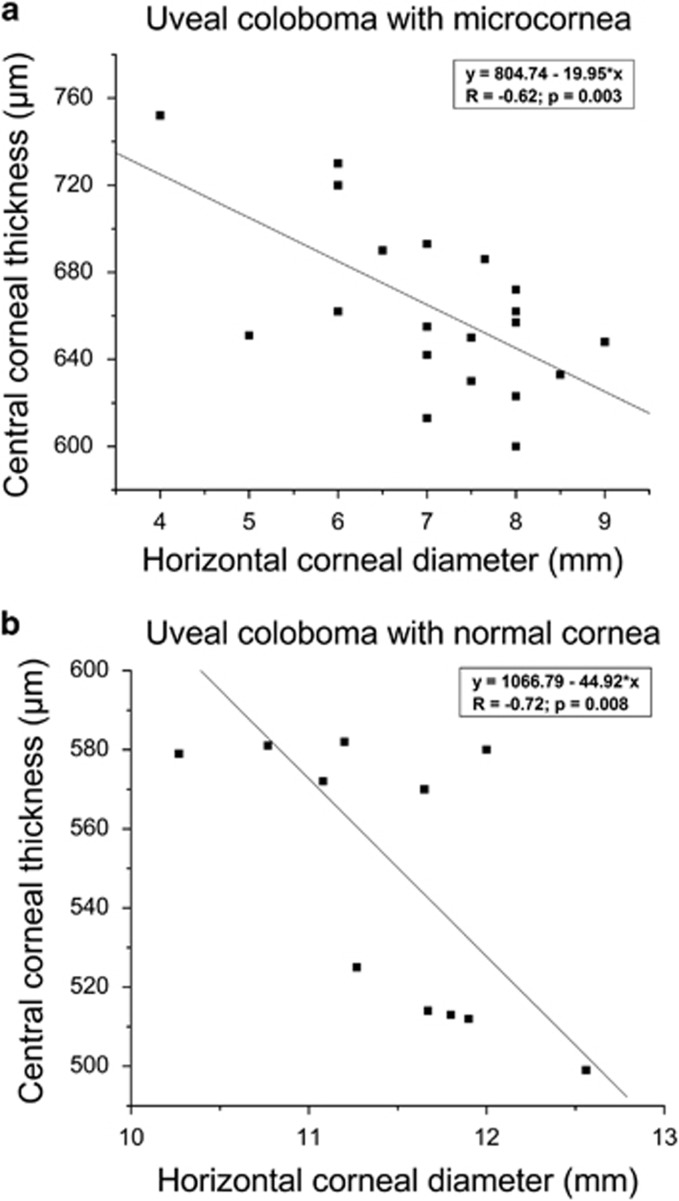
Table 1 compares the observations between study and control groups. As seen in the table, both groups were comparable in terms of age and gender of the patient. The mean HCD of the study and control groups was 6.97±1.28 and 11.39±0.67 mm, respectively. The mean central pachymetry of the study group was 668.4±40.2 μm compared with 555.3±41.8 μm in the control group. In both the groups, CCT was negatively correlated with HCD (Figure 2a and b; R=−0.62 in the study group and R=−0.72 in the control group) similar to our unpublished data in normal subjects. The decrease in CCT per unit increase in HCD in normal-sized corneas (45 μm/mm) was almost twice that in microcorneas (20 μm/mm).
Table 1. Microcornea vs normal cornea in uveal coloboma.
| Parameters | Study group, n=26 eyes | Control group, n=12 eyes | P-value |
|---|---|---|---|
| Age (years), mean±SD | 38.2±13.5 | 43.2±16.1 | 0.42 |
| Males/females | 8:7 | 6:3 | 0.68 |
| Horizontal corneal diameter (mm), mean±SD | 6.97±1.28 | 11.39±0.67 | <0.0001 |
| Central corneal thickness (μm), mean±SD | 668.4±40.2 | 555.3±41.8 | <0.0001 |
This table compares the study group (uveal coloboma with microcornea) and control group (uveal coloboma with normal cornea).
Figure 2.
Significant negative correlation between horizontal corneal diameter and central corneal thickness in both the study and control groups. (a) Microcornea and (b) normal cornea.
Discussion
This study examined the central corneal thickness in uveal colobomatous eyes with both microcornea and normal-sized cornea. The analysis shows that the uveal coloboma eyes with microcornea tend to have an increased corneal pachymetry compared with eyes with normal-sized corneas. This could be attributed to the failure of expansion of the limbal girdle with a relative normal corneal stromal volume at the time of development in utero.
Tang et al3 observed an increased corneal thickness in four eyes with ocular coloboma. Filous et al4 found the mean CCT to be 642.3±93.1 μm in a group of eyes with microphthalmia that included uveal colobomas (5 eyes). We found a slightly higher mean CCT value (668.4±40.2 μm) in our study population. The slight difference may be attributed to a larger sample size (26 eyes) in our study. Bayoumi and El Shakankiri5 also found a mean CCT of 667±72.9 μm in 62 aphakic eyes with microcornea. However, the status of coloboma is not known in these eyes. Filous et al4 also found the mean CCT to be 553.6±33.1 μm in a control group of healthy eyes with normal ocular findings. Bayoumi and El Shakankiri5 found a mean CCT of 545.2±28.1 μm in control eyes with normal corneal diameter. This concurs well with the mean CCT of 555.3±41.8 μm observed in our colobomatous eyes with normal diameter corneas. Similar to our study, the studies by Filous et al4 and Bayoumi and El Shakankiri5 observed a significant difference in CCT between the study and control groups and a significant negative correlation between HCD and CCT in microcornea. Whereas Filous et al4 and Bayoumi and El Shakankiri5 compared coloboma eyes with microcornea and aphakic eyes with microcornea respectively to healthy eyes with normal corneas, our study is unique in making comparisons between microcornea and normal-sized corneas in eyes only with uveal coloboma. It appears that the colobomatous eyes with normal-sized corneas have a corneal pachymetry profile similar to healthy eyes.
Some authors have hypothesized that these thicker-than-normal corneas could arise because of disruption of normal ocular development in uveal coloboma that could cause secondary abnormalities in neural crest migration or be secondary to increased activity of the stromal keratocytes and extracellular matrix over a smaller area in microcornea.3 As per the observations in this study, it is probably because of a compaction of stroma and the extracellular matrix in a smaller area in microcornea. However, we are not certain whether there is an increase in the activity of stromal keratocytes or just the normal activity of the existing number of stromal keratocytes in a smaller area in microcornea. Ocular coloboma is commonly inherited with variable expressivity.2 In colobomatous eyes with normal-sized cornea, it could be that the development of cornea did not get affected and that these corneas had normal diameter and thickness. The rate of change in thickness per mm change in diameter is lesser in microcorneas than the normal-sized corneas, suggesting that there could be an anatomical resistance and tighter packing of collagenous stroma in patients with uveal coloboma and microcornea. It is not known whether there are altered biomechanical properties in microcorneas. A confocal microscopy study to assess the arrangement of stromal lamellae and keratocyte density can help to improve the understanding of this clinical observation.
A sound understanding of biometry in eyes with coloboma is important. Evaluating an optic nerve head in an eye with coloboma is challenging. Central corneal thickness has an influence on intraocular pressure (IOP) assessment. With the findings of this study, it may be presumed that the IOP values may be less affected in the coloboma eyes with normal-sized cornea than those associated with microcornea. The coloboma eyes can have microcornea in one eye and normal-sized cornea in the other eye of the same patient. As the corneal pachymetry and diameter differ between these, the two eyes can have different refractive properties. Identification of possible anisometropia in uveal colobomatous eyes would become valuable and help in preventing the development of anisometric amblyopia.
In conclusion, uveal colobomatous eyes with microcornea have thicker corneas compared with uveal colobomatous eyes with normal diameter corneas that have normal central corneal thickness. In all the eyes with uveal coloboma, there is a negative correlation between horizontal corneal diameter and central corneal thickness.
Footnotes
The authors declare no conflict of interest.
References
- Warburg M. Classification of microphthalmos and coloboma. J Med Genet 1993; 30: 664–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed A, Chaurasia S, Ramappa M, Sangwan VS, Jalali S. Lenticular changes in congenital iridolenticular choroidal coloboma. Am J Ophthalmol 2014; 158: 827–830 e2. [DOI] [PubMed] [Google Scholar]
- Tang J, Gokhale PA, Brooks SE, Blain D, Brooks BP. Increased corneal thickness in patients with ocular coloboma. J AAPOS 2006; 10: 175–177. [DOI] [PubMed] [Google Scholar]
- Filous A, Osmera J, Hlozanek M, Mahelkova G. Central corneal thickness in microphthalmic eyes with or without history of congenital cataract surgery. Eur J Ophthalmol 2011; 21: 374–378. [DOI] [PubMed] [Google Scholar]
- Bayoumi NH, El Shakankiri NM. Central corneal thickness in aphakic children with microcornea-microphthalmia. J Glaucoma 2016; 25: 497–500. [DOI] [PubMed] [Google Scholar]