Abstract
Pseudo-phakic pupillary block glaucoma in postoperative period may mimic acute endophthalmitis. This article illustrates how clinical differentiation of pseudo-phakic pupillary block glaucoma from postoperative acute endophthalmitis was done as ultrasonography produced confusing results.
Keywords: Postoperative endophthalmitis, pseudophakia, pupillary block glaucoma
Introduction
In a postoperative patient of cataract surgery, the occurrence of pain, redness, dimness of vision is always fraught with the fear of endophthalmitis. However, all such cases which appear to be endophthalmitis at first sight may not be endophthalmitis. Differentiation based on clinical features are important as ultrasonographic feature may be equivocal. The purpose of this article is to make the ophthalmologists aware of the clinical features to differentiate pseudophakic pupillary block glaucoma from postoperative endophthalmitis.
Case Report
A 58-year-old nondiabetic and nonhypertensive male attended the emergency with complaint of pain, redness, and dimness of vision in his right eye for 6 days. He had undergone small incision cataract surgery + posterior chamber intraocular lens (PCIOL) implantation in some other hospital 10 days back. As per history, he was following the postoperative medication (which included tablet prednisolone 30 mg O.D.) and doing well for initial 4 days and then suddenly developed these symptoms. He was initially treated by some local ophthalmologist. However, the symptoms in next few days worsened. He then consulted another ophthalmologist who diagnosed him as a case of postoperative endophthalmitis and referred him to our hospital on the 10th postoperative day. In the emergency room, the examination revealed [Figure 1] right eye, Vision- PL+, PR accurate in all quadrants, eyelids-swollen, conjunctiva-chemosed and congested, cornea-corneal edema, circumcorneal congestion, pupil-small (about 2.5 mm), not reacting to light, white reflex in the whole pupillary area seen, anterior chamber-flare and cells-mild, a white transverse band in the mid-lower periphery seen. Iris: periphery of the iris appeared bulged (iris bombe). Digital intraocular pressure (IOP) appeared to be high. On the basis of these clinical findings, the case was provisionally diagnosed as postoperative endophthalmitis with a differential diagnosis of secondary glaucoma. The patient was admitted and put on fortified cefazolin and fortified tobramycin, prednisolone acetate, timolol maleate and cyclopentolate eye drops. He was given tablet ciprofloxacin (750 mg) twice a day and tablet acetazolamide (250 mg) 4 times/day.
Figure 1.
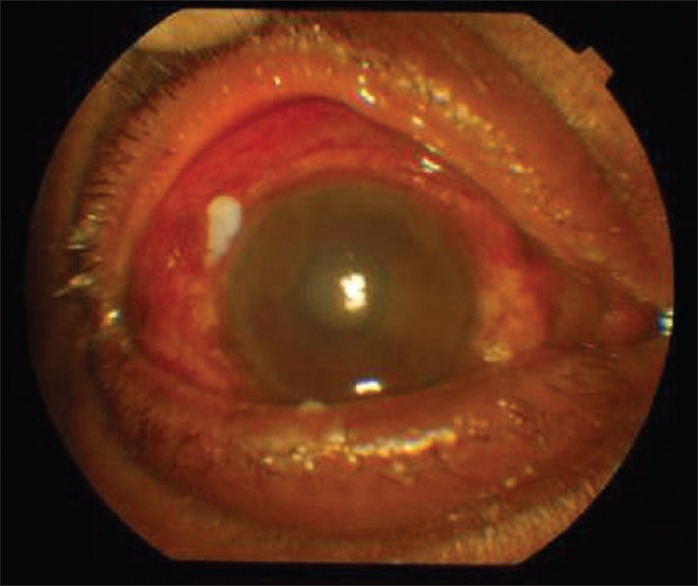
Pseudophakic pupillary block glaucoma, initial presentation (see text)
On the next day, ultrasonogram [Figure 2] was done which showed a chain of low amplitude spikes in A-scan. At high gain a bright anterior echo, followed by multiple reverberations were seen in B-scan.
Figure 2.
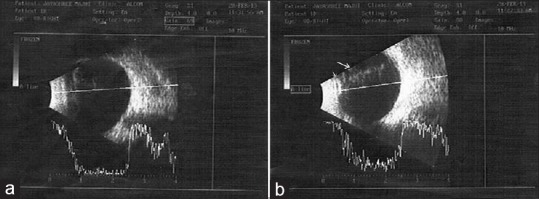
Pseudophakic pupillary block glaucoma, ultrasonogram. (a) Shows chain of low amplitude spikes in A-scan due to sterile vitritis (see text). (b) Shows a bright anterior echo from intraocular lens (short arrow) followed by multiple reverberations (long arrow) in B-scan
IOP was measured and found to be 40 mm. of Hg. A volume of 300 ml of intravenous (IV) Mannitol was given. Intravitreal ceftazidime (2.25 mg/0.1 ml), and vancomycin (1 mg/0.1 ml) was given. Vitreous sample was collected and sent for culture and sensitivity test. Even on 3rd day after admission, no improvement was noticed, pupil was not dilating, vision not improving. On the 4th postadmission day, the anterior chamber was formed with air under proper asepsis and under IV 300 ml mannitol cover. Sub-conjunctival injection containing 0.25 ml each of gentamicin (40 mg/ml), dexamethasone (4 mg/ml) and atropine (0.6 mg/ml) was also given. On the 5th postadmission day, marked symptomatic improvement was noticed, vision improved to finger counting two feet, anterior chamber was well formed. Pupil started dilating and a part of PCIOL could now be seen. IOP reduced to 22 mm of Hg. A repeat sub-conjunctival injection of gentamicin, dexamethasone, and atropine was given.
On the 6th postadmission day, vision improved to finger counting four feet, PR accurate in all quadrants, pupil was mid-dilated, a pupillary membrane was now exposed on the anterior surface of the IOL [Figures 3 and 4]. Ophthalmoscopic examination was done at this stage, glow was present but fundus details was not visible. A repeat sub-conjunctival injection of gentamicin, dexamethasone, and atropine was given.
Figure 3.
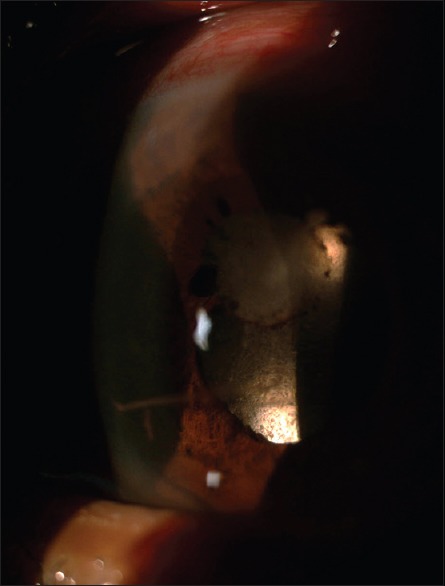
Pseudophakic pupillary block glaucoma: White pupillary membrane unearthed on mydriasis, still attached to iris superiorly but relieved inferiorly
Figure 4.
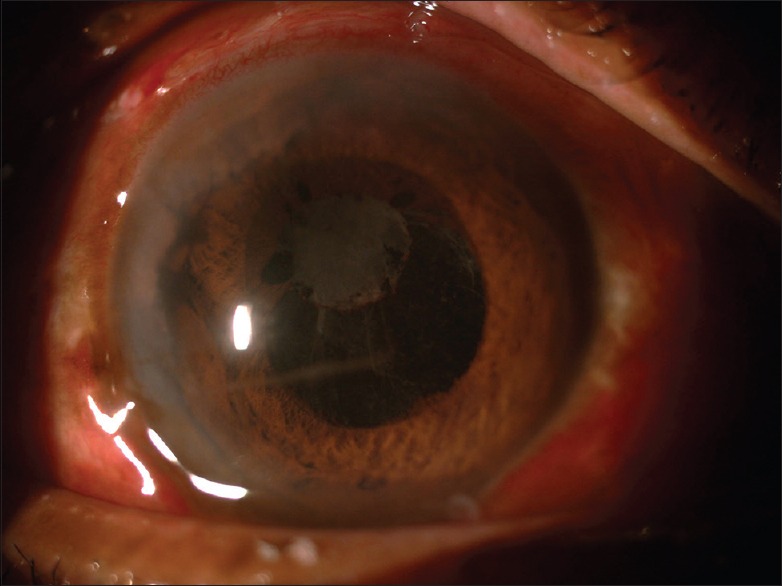
Pseudophakic pupillary block glaucoma: Slit lamp section shows pupillary membrane and superior iris bombe
The patient was discharged with 6/60 vision on the 8th postadmission day.
The vitreous culture showed no growth after 48 h and after 7 days.
Final diagnosis at discharge was pseudophakic pupillary block glaucoma. The patient did not come for follow-up.
Discussion
The symptomatology of psedophakic pupillary block glaucoma and acute postoperative endophthalmitis is almost similar. Pain, redness, dimness of vision, lacrimation, corneal edema, and white papillary reflex occur in both the conditions. In endophthalmitis, the IOP is usually on the lower side of normal but may be elevated in the early stage. In the present case, this sign of differentiation (endophthalmitis-low IOP and pupillary block glaucoma-high IOP), was not elicitable at presentation in emergency room setting because of extreme pain, tenderness, and lid edema associated with the condition. However, the anterior chamber reaction was disproportionately low arousing suspicion of secondary glaucoma. Furthermore, the ultrasonogram findings were equivocal, because of the fact, beside endophthalmitis, the echoes in the vitreous cavity could be caused by sterile vitritis[1] [Figure 2a] and intraocular lens[2] [Figure 2b]. The transverse band in the mid-lower periphery of the anterior chamber [Figures 3 and 4] carried the reminiscence of sterile hypopyon in the early postoperative period. Sterile vitritis might be caused by the spillover of inflammatory cells from hypopyon to the vitreous cavity.[1] Although the white pupillary reflex was suggesting an endophthalmitis, the increased intraocular tension and iris bombe pointed toward pupillary block glaucoma. To be on the safer side for the wellbeing of the patient, one intravitreal injection of ceftazidime and vancomycin was given but no improvement resulted. Nd-Yag laser iridotomy was avoided because effect of laser is temporary and needs to be repeated several times.[3] Then the age old method of treating psedophakic pupillary block glaucoma was resorted to, that is, mydriasis by subconjunctival injection of atropine and formation of anterior chamber by air under cover of IV Mannitol (to simultaneously reduce vitreous pressure). This method readily worked and with three spaced subconjunctival injection of atropine, pupil was sufficiently dilated to unearth the mystery of pupillary white reflex. It was then evident that the white reflex was caused by a whitish pupillary membrane on the anterior surface of the IOL to which the iris was adherent causing pupillary block [Figures 3 and 4]. The pupillary membrane was formed due to organization of proteinous exudates which might have formed excessively due to plastic iridocyclitis following traumatic surgery. (Traumatic surgery was suggested by prescription of tablet prednisolone in postoperative medication). Subsequently with the organization of exudates, the proteinous exudates and inflammatory cells were used up. Therefore, anterior chamber reaction diminished, and hence, anterior chamber reaction was mild at presentation. Mydriasis resulted in the loss of adhesion between the iris and the lens thus relieved glaucoma and patient's condition improved. At the same time, the culture report of vitreous tap showed no growth of microorganism. Therefore, the diagnosis of acute psedophakic pupillary block glaucoma was established beyond doubt.
Had there been a misdiagnosis of endophthalmitis, without keeping in mind the possibility of psedophakic pupillary block glaucoma, there could have effects of uncontrolled secondary glaucoma which in extreme case might even lead to atrophic bulbi.
Therefore, nonimmediate presentation (10th postoperative day in the present case, that is, the time taken for the formation of occlusio pupillae by the organized exudate), disproportionately mild anterior chamber reaction (because cells and exudates were used up in the formation of the pupillary membrane), small and undilating pupil (due to iris adherent to intraocular lens), iris bombe, and high IOP clinically distinguishes pseudophakic pupillary block glaucoma from postoperative endophthalmitis. Ultrasonography was equivocal and not relied on.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Byrne SF, Green RL, editors. Ultrasound of the Eye and Orbit. 2nd ed. St. Louis: Mosby; 2002. Inflammatory diseases of the eye; p. 194. [Google Scholar]
- 2.Green RL, Byrne SF. Diagnostic ophthalmic ultrasound. In: Ryan SJ, editor. Retina. 3rd ed. St. Louis: Mosby; 2001. p. 300. [Google Scholar]
- 3.Naveh N, Wysenbeek Y, Solomon A, Melamed S, Blumenthal M. Anterior capsule adherence to iris leading to pseudophakic pupillary block. Ophthalmic Surg. 1991;22:350–2. [PubMed] [Google Scholar]


