Abstract
Large traumatic macular holes (TMHs) tend to be irregular and have a variable predictability. The inverted flap technique makes use of remnants of internal limiting membrane (ILM) at the periphery of the MH. The peeled-off ILM contains Müller cell fragments which can induce gliosis and help in closure of MH. We operated on a case of large TMH (~899 μ minimum linear diameter) with choroidal rupture and subretinal hemorrhage in a young female with the inverted flap technique of ILM peeling and observed successful closure of the MH. The excellent anatomical and surgical results achieved in our case seem to suggest this to be a safe and effective surgical manoeuvre for such cases.
Keywords: Choroidal rupture, inverted flap technique, internal limiting membrane peeling, subretinal hemorrhage, traumatic macular hole
Introduction
Common causes of full-thickness macular hole (FTMH) are idiopathic, trauma, and high myopia. Traumatic MHs (TMHs) have long been thought to arise from a contrecoup mechanism. A sudden axial compression of the globe can result in flattening of the posterior sclera. With a fixed volume, the subsequent decrease in the globe's anterior-posterior diameter causes a compensatory equatorial expansion. This dynamic change in the globe structure can lead to horizontal forces and splitting of the retinal layers at the fovea. The extent of the retinal injury is likely related to the force applied to the eye, along with inherent structural features of the patient's eye.[1]
The predictability of traumatic injuries is always difficult, and the progression to TMH is no different. This contrecoup mechanism of TMH formation is likely supplemented by varying degrees of vitreous traction within the globe. The dynamic forces alter the structure of the globe at several key attachments of the vitreous to the retina. Unlike the slowly evolving vitreoretinal traction of an idiopathic MH, the tangential vitreous forces created by blunt ocular trauma are more variable. This variation can often lead to a much more irregular configuration of the hole than the often perfectly circular shape seen in idiopathic MH.[1]
Inverted flap technique for internal limiting membrane (ILM) peeling – this technique in which a remnant of ILM attached to the margins of MH is left in place and inverted into the hole after trimming with cutter is useful in large MHs[2] and MH in myopic eyes.[3] The peeled off ILM contains Muller cell fragments which can induce gliosis both inside retina and on the surface of ILM, thus help in healing MH.
We operated on a case of TMH with choroidal rupture and subretinal hemorrhage with the inverted flap technique of ILM peel and observed successful closure of the large TMH.
Case Report
A 16-year-old female presented with a history of gradual diminution of vision in the right eye (RE) for 2 months following road traffic accident. She gave H/O multiple fractures of midfacial bones for which she was operated elsewhere.
On examination, her best-corrected visual acuity (BCVA) in RE was 5/60 and left eye was 6/5, N5. Intraocular pressure was normal. Pupillary reactions revealed RAPD in RE. Anterior segment examination was unremarkable.
Fundus examination of RE shows temporal pallor of optic nerve head, traumatic FTMH with choroidal rupture and subretinal hemorrhage [Figures 1 and 2].
Figure 1.
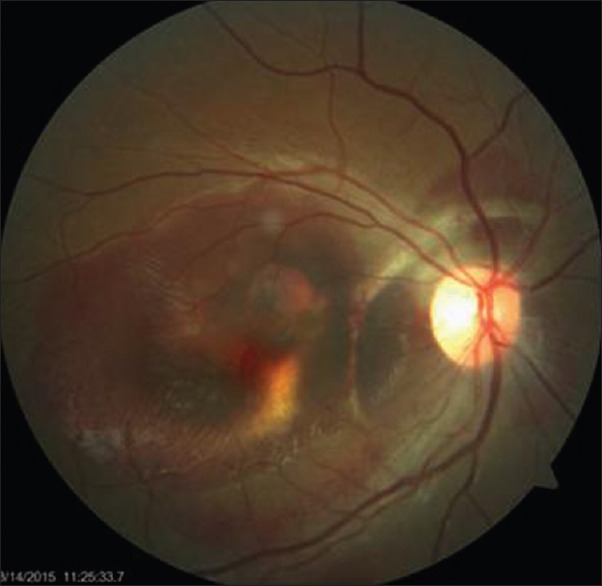
Fundus photo showing full thickness macular hole with subretinal hemorrhage and choroidal rupture
Figure 2.
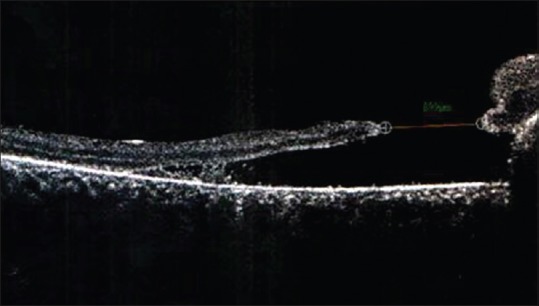
Optical coherence tomography showing full thickness macular hole at the edge of subretinal hemorrhage (arrowhead). The area of scarring is seen at the nasal edge of the hole (arrow). The minimum linear diameter on optical coherence tomography was 899 μm
She was advised and underwent vitrectomy, ILM peel, laser indirect ophtahlmoscopy, and gas injection – ILM peeling was carried out in a 2 disc diameter area around the hole, the edges were trimmed with the cutter and reposited gently into the hole with a soft tipped brush needle. During fluid-air exchange, the brush needle was placed temporal to the optic nerve adjacent to the hole to help the peeled ILM cover the hole. Postoperative period was uneventful.
Two months postoperative, her BCVA improved to 6/36. Optical coherence tomography showed closed MH with persisting neurosensory detachment. Six months postoperative her BCVA improved to 6/18. Colour photo shows closed macular hole with overlying atrophy and choroidal rupture nasal to fixation [Figures 3]. OCT shows closed macular hole [Figure 4]. Autoflourescence shows area of hypoflourecence in areas of choroidal rupture and RPE atrophy [Figure 5].
Figure 3.
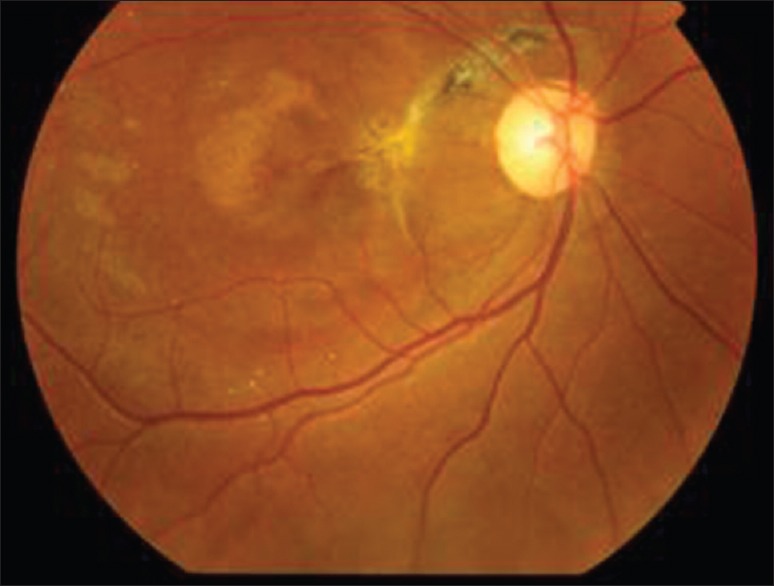
Fundus photo at 6 months
Figure 4.

Optical coherence tomography, closed macular hole at 6 months
Figure 5.
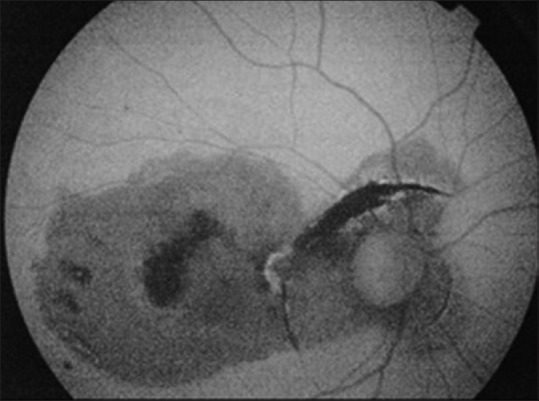
Autofluorescence at 6 months - hypofluorescence at area of choroidal rupture and hypo with rim of hyperfluorescence at posterior pole
Discussion
The improvement in technique and development of finer instrumentation in vitreoretinal surgery has significantly improved the surgical outcome of MHs in terms of anatomical and functional success. The single most reliable factor affecting the surgical outcome following surgery is the size of the hole.[4]
A number of studies have established that the minimum linear diameter of the hole is closely related to the rate of anatomic success. Furthermore, it has been shown that the most favorable outcomes for visual recovery were associated with better initial visual acuity. Among all the different techniques for MH surgery, the one with the most positive effect on final outcome is vitrectomy with ILM peeling, to release tangential forces acting on the MH. In addition to promoting hole closure, peeling of the ILM also reduces the probability of its reopening.[5,6] Dye assisted technique is safe and useful in visualizing the ILM, leading to the performance of successful peeling of ILM with minimal damage to the retina. Brilliant blue selectively stains the ILM and can be safely used for staining the ILM.[7] The peeled-off ILM contains Müller cell fragments which can induce gliosis and help in closure of MH.[8]
Thus, if a segment of peeled-off ILM is left attached, it may provoke gliosis both inside the retina and on the surface of the ILM.[8] The ILM also may be a scaffold for tissue proliferation.
Large MHs (>400 μ) have an increased risk of surgical failure. Up to 44% of large MHs are flat open after surgery and associated with limited improvement in visual acuity. Inverted flap technique prevents the postoperative flat open appearance of an MH and improves functional and anatomic outcomes of vitrectomy for MHs >400 μ.[2] Michalewska et al. observed closure of the MH by a thin membrane with an appearance consistent with the ILM.[2]
Trauma-related pathogenesis occurring at the time of injury including commotion retinae, choroidal rupture or retinal tears can all limit the final visual potential.[9] If significant disruption of RPE is present near or within the centre of macula, this has significant importance for vision recovery after trauma and attempted repair of an MH.[10]
Although the initiating factors of TMH are quite different from idiopathic MHs, the results of vitrectomy surgery indicate good prognosis. Johnson et al. in their series of TMHs reported a closure rate of 96% and improvement in visual acuity by two lines.[10]
We decided to do inverted flap technique in view of a very large MH (899 μ) and obtained a good closure in this young girl. The excellent anatomical and surgical results achieved in our case seem to suggest this to be a safe and effective surgical manoeuvre for such cases. Larger studies will be required to validate our result.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Miller JB, Yonekawa Y, Eliott D, Vavvas DG. A review of traumatic macular hole: Diagnosis and treatment. Int Ophthalmol Clin. 2013;53:59–67. doi: 10.1097/IIO.0b013e3182a26efe. [DOI] [PubMed] [Google Scholar]
- 2.Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25. doi: 10.1016/j.ophtha.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Kuriyama S, Hayashi H, Jingami Y, Kuramoto N, Akita J, Matsumoto M. Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol. 2013;156:125–131.e1. doi: 10.1016/j.ajo.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 4.Freeman WR, Azen SP, Kim JW, el-Haig W, Mishell DR, 3rd, Bailey I. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol. 1997;115:11–21. doi: 10.1001/archopht.1997.01100150013002. [DOI] [PubMed] [Google Scholar]
- 5.Yamanishi S, Emi K, Motokura M, Oshima Y, Nakayama M, Watanabe M. Visual outcome of macular hole surgery with internal limiting membrane peeling. Nippon Ganka Gakkai Zasshi. 2001;105:788–93. [PubMed] [Google Scholar]
- 6.Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J. Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology. 1999;106:1392–7. doi: 10.1016/S0161-6420(99)00730-7. [DOI] [PubMed] [Google Scholar]
- 7.Enaida H, Hisatomi T, Hata Y, Ueno A, Goto Y, Yamada T, et al. Brilliant blue G selectively stains the internal limiting membrane/brilliant blue G-assisted membrane peeling. Retina. 2006;26:631–6. doi: 10.1097/01.iae.0000236469.71443.aa. [DOI] [PubMed] [Google Scholar]
- 8.Mahalingam P, Sambhav K. Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol. 2013;61:601–3. doi: 10.4103/0301-4738.121090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weng CY, Berrocal AM. Traumatic macular holes in the paediatric and adolescent populations. Retinal Physician. 2014;11:16–19. [Google Scholar]
- 10.Johnson RN, McDonald HR, Lewis H, Grand MG, Murray TG, Mieler WF, et al. Traumatic macular hole: Observations, pathogenesis, and results of vitrectomy surgery. Ophthalmology. 2001;108:853–7. doi: 10.1016/s0161-6420(00)00650-3. [DOI] [PubMed] [Google Scholar]


