Abstract
The growing epidemic of noncommunicable diseases (NCDs) has impacted the national health systems, policies, and socioeconomic developments, thereby leading to increasing country level disparities. Despite substantial improvements in health indicators made in the past decade, the Indian health-care system continues to contribute disproportionately to the global disease burden, wherein NCDs holds significant prominence. Against this background, the present review analyzes the current NCD landscape from the perspective of India's health system preparedness toward meeting this growing challenge. Implementation and delivery of strategies and interventions are often impeded by existing grass root level challenges. Recognizing the importance of effective primary care, the review highlights the importance of implementing affordable, accessible, and comprehensive interventions, and delivering them at societal, a community and individual level. This simultaneously calls for strengthening of the primary care system through appropriate strategy and policy frameworks. Toward addressing India-specific needs in NCD prevention and management, concerted efforts on development of robust surveillance mechanisms, intersectoral and interdepartmental collaborations, integration of national programs, enhanced role of education and awareness should be made, to ensure effectivity, scale-up, and outreach of services in primary care.
Keywords: Noncommunicable disease, primary care, public health
Introduction
The Millennium Development Goals (MDG) have made significant progress in the achievement of its ambitious targets aimed at improving the lives of people all over the world.[1] While on one hand, efforts for the expansion of basic health-care coverage to tackle infectious diseases and child mortality were successful, on the other hand, the conspicuous absence of noncommunicable diseases (NCD) from the MDG framework proved to be a stumbling block in the progress made so far.[2]
The growing epidemic of NCDs in the 21st century has severely impacted the national health systems, policies, and socioeconomic developments, thus increasing disparities and inequities between countries.[3] The inadequate interpretation of MDGs in the low- and middle-income countries (LMICs) has resulted in delivery of vertical and disease-specific health programs at the ground.[4] As a consequence, the health system in LMICs has not only remained distorted but also ill-equipped to manage the dual burden of communicable as well as NCDs.[5,6] NCDs have contributed to about 68% of the total deaths in 2012, nearly three quarters of which (28 million) have been reported from the LMICs. As per the World Health Organization (WHO), improved control of infectious diseases, rapid urbanization, and aging population will increase projected NCD deaths to about 52 million by 2030.[7] Epidemiological evidence indicate that four major chronic diseases, namely, cardiovascular diseases (CVDs), cancers, diabetes, and chronic respiratory diseases have contributed to 82% of all the NCD deaths.[8] The growing burden of NCDs has also heavily impacted the social and economic aspects of sustainable human development.[9]
With the more comprehensive and holistic sustainable development goals (SDGs) coming into picture, NCD management has garnered paramount importance in the context of achieving healthy lives and well-being for all.[10,11] SDG3 aims to reduce NCD-induced premature mortality through prevention and treatment and also promote mental health and well-being by 2030. The need for integrated action for NCD prevention through multisectoral action and health system strengthening has thus been recognized universally and is deemed to lay the foundation for improved health, mitigated socioeconomic impacts, and accelerated sustainable development.
India represents the third largest economy and one of the most populous countries in the world. Despite substantial improvements in health indicators made in the past decade, the Indian health-care system continues to contribute disproportionately to the global disease burden.[12] India is presently experiencing a phase of rapid health transition, wherein the mounting magnitude of NCDs is gaining prominence with substantial repercussion on health and economic productivity.[13] With this background, it is important to perceive India's health system preparedness toward meeting the growing NCD challenge. This article presents an overview of the current landscape of NCDs in India, an understanding of India's readiness to tackle NCDs and emphasizes on the relevance of empowering the primary care system for NCD prevention and management.
The Noncommunicable Diseases Landscape in India
The health-care system in India presents a three-tier structure comprising of the primary, secondary and tertiary care services. The services range from population-based health services at the ground (primary level care) to curative services (secondary level care) and highly personalized and specialized medical care (tertiary level care). As per norms of the Indian Public Health standards (IPHS), the delivery of primary health care is designed to provide an integrated curative, preventive, and promotive care to the rural population, through the subcenter, primary health center (PHC), and community health center (CHC); secondary care delivered at district and subdistrict hospitals, and tertiary care at regional/central level institutions or super-specialty hospitals.
NCDs have emerged as the leading causes of death in India, accounting for 15% of the global NCD deaths and 60% of total deaths in the country.[14] This is complemented by significant economic threats on households and health-care delivery system.[15] The leading cause of NCD mortality in India is CVDs (26%), cancer (7%), chronic respiratory disorders (13%), diabetes (2%), and other NCDs (12%).[16] Findings from the Global Burden of Disease indicate that ischemic heart disease was one of the highest-ranking causes that led to premature deaths in India in 2013.[17] Diabetes is predicted to affect about 109 million people between 20 and 79 years of age by 2035.[18]
NCDs share a strong association to the common behavioral risk factors. Table 1 below summarizes the prevalence of the major risk factors in India that have contributed to raising the burden of NCDs in India.
Table 1.
Prevalence of the major risk factors in India that have contributed to increasing the burden of noncommunicable diseases*
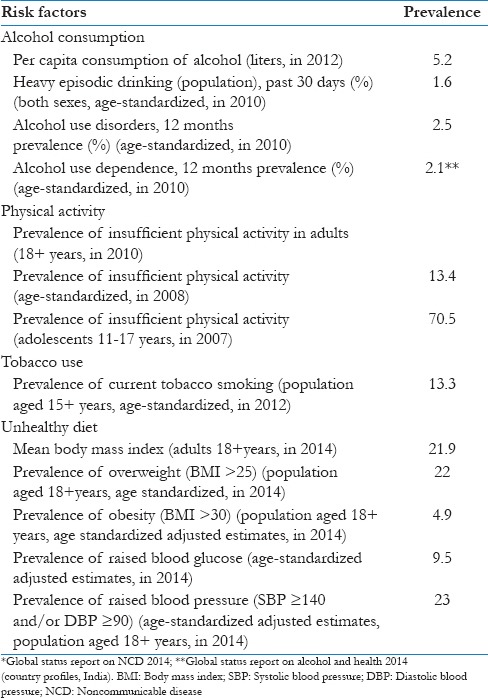
The Global Adult Tobacco Survey (2009–2010), estimated that the number of tobacco users in India was 274.9 million.[19] The total economic costs attributable to tobacco use from all diseases for persons aged 35–69, amounted to US$ 22.4 billion in the year 2011. CVDs shared the highest burden of health-care expenses attributable to tobacco use.[20] Results from the first phase of National Family Health Survey 4 (2015–2016), released in early 2016 expressed concern on overnutrition becoming a major health issue for adults. Studies on the prevalence, awareness, and control of hypertension indicated that the prevalence has increased notably in both urban and rural subjects.[21] On the economic front, the estimated losses in national income from heart disease, stroke, and diabetes for 2015 in India was US$ 54 billion with gross domestic product reduction of around 1%.[22] Health expenditure among people from all socioeconomic groups was higher for chronic diseases than for infectious diseases and more was spent on private sector services than public sector services.[23] Most people suffering from NCDs incurred high out-of-pocket expenses to meet healthcare costs. The economic burden for NCD treatment falls unevenly on the poor lending financial vulnerability.
Chronic Disease Care
Chronic diseases confront patients with a varied and wide spectrum of care needs which is long-term, proactive, planned, coordinated, and continuous. The growing burden of NCDs, however, indicates that the outreach of NCD care has remained suboptimal. Key factors that have impeded the optimal delivery of chronic care include (i) fee for service structure, (ii) dearth of skilled health workers with knowledge about NCD prevention, (iii) lack of coordination within multidisciplinary care teams, (iv) irregular review and follow-ups, (v) limited engagement between patient and health-care provider, (vi) underdeveloped decision support systems, (vii) weak health system infrastructure, and (viii) limited access to essential medicines.[24,25,26,27] In addition, significant administrative burdens such as inadequate funding, ineffective planning and monitoring, inappropriate models of service delivery, and the complexity of innumerable and fragmented health programs pose challenges to the provision of NCD services at the ground.[26] In the light of these limitations, the immediate focus should be on reforming the health system through multisectoral action to deliver quality care to patients afflicted with chronic diseases. Several studies have highlighted that an integrated and comprehensive, patient-centered, and community-based strategy is the best way forward.[28,29,30]
Role of primary care in noncommunicable diseases prevention and control
Evidence-based chronic disease prevention and treatment approaches rooted in the primary care settings present an efficient and effective way to address challenges associated with chronic disease prevention and management. While strategies and interventions are well known, delivering them at the ground level using primary health-care approach, and to make significant impact is crucial. Priority must be given for implementing interventions that are comprehensive, low cost, effective, and appropriate. The 2008 World Health Report, emphasizes on the importance of primary health care, through reforms in universal coverage, service delivery, public policy and leadership. It calls for the establishment of a continuum of care that addresses the increasing concerns of chronic and NCD.[31]
Primary health-care management of chronic diseases entails assessment of risk factors, early detection of disease, pharmacological/physiological interventions, adequate treatment approaches, long-term follow-ups, regular monitoring, and promotion of adherence to treatment. Additional interventions that are to be put in place to reap a better future with improved quality of life include commitment and ownership, cross-sectoral coordination, trained health workforce, effective health information system, effective procurement and supply management system, community participation and engagement, and community-level health education programs. It is essential that such interventions to be delivered at the societal, community, and the individual levels to cope with the chronic disease epidemic worldwide.
Creative solutions are needed to address the escalating health-care demands of chronic conditions, especially in countries with limited primary care infrastructure. The inclusion of evidence-based approaches can bring increased coherence and efficiency to health-care systems and provide a means for improving quality across a range of chronic health problems. The chronic care model, one of the most influential and multifaceted models for chronic care management and the recently introduced WHO Package of Essential NCD Interventions, present flexible and comprehensive templates to guide the redesigning of health systems, especially in low-resource settings.[32,33] Both these frameworks envisage the integration of NCDs into primary health-care settings and delivery of a prioritized set of quality and cost-effective interventions at the primary care level.
Noncommunicable diseases prevention, control, and management in India
Recognizing the growing threat of NCDs, the Ministry of Health and Family Welfare (MoHFW), Government of India has launched National Programme for Prevention and Control of Cancer, Diabetes, CVD and Stroke (NPCDCS), a national program for control of NCDs. The NPCDCS seeks to integrate NCD interventions into the framework of public-health delivery through the promotion of healthy lifestyle habits, early diagnosis of diabetes, hypertension, CVDs and stroke, the establishment of NCD clinics at CHCs, capacity building for health promotion, regular supervision, monitoring, and evaluation of the programme. Additionally, preventive, curative and rehabilitative care for the elderly in various government health facilities is envisaged under the National Programme for Care of the Elderly. The National Tobacco Control Programme has facilitated the implementation of the tobacco control laws in the country. The launch of the National Mental Health Program ensured the availability and accessibility of appropriate mental health care for the vulnerable population. Figure 1 summarizes the various programs embarked on by the government in the country toward addressing NCD-related issues.
Figure 1.
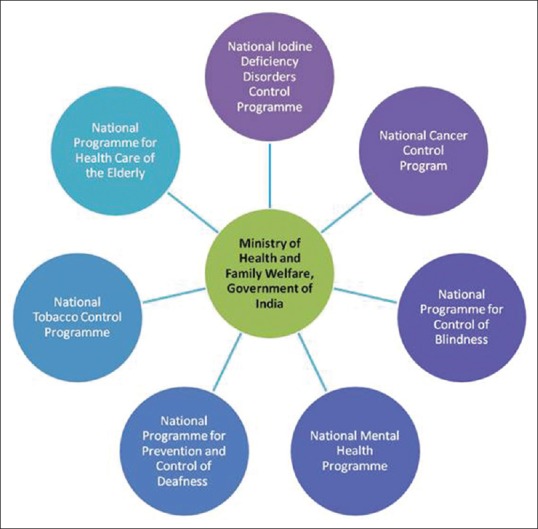
Government-initiated programs targeted at noncommunicable diseases prevention and control
Despite commendable efforts, the focus of primary care in India has been communicable diseases, reproductive, and child health services. The present government initiated health programs for both communicable as well as NCDs appear to be fragmented, vertical and disease-specific, with more emphasis on rendering acute care services. There remains considerable inadequacies in the delivery of NCD care services both at the primary and secondary care level. The NCD Scorecard (http://www.ncdglobalscorecard.org), developed from the United Nations political declaration after the High-level Meeting on the Prevention and Control of NCD in 2011 indicates India's very low progress in terms of health system response for NCD and low performance in its efforts to reduce risk factors and conducting disease surveillance of disease. India's present health system readiness is an issue of concern. Some of the major bottlenecks in the smooth delivery of NCD services are discussed below.
Shortfall of public health facilities
As per the Rural Health Statistics 2014–2015 released by the MoHFW, the subcentres, PHCs, and CHCs have increased in number over the last decade. The current numbers are yet not sufficient to meet their population norms. There is yet a shortfall of 20% in the SCs, 22% in the PHCs, and 32% in the CHCs in India.[34]
Nonavailability of appropriate infrastructure
There is a significant gap in infrastructure such as laboratory, operation theater, beds, at the primary care level, on the basis of number of health facilities functioning in the country. Only 20.72% PHCs are said to be functioning as per IPHS norms.[34]
Poor density of health workforce trained to deliver noncommunicable diseases services
Shortage of skilled health workers, trained in providing chronic at the field level is another critical issue. India paints a disappointing picture in terms of the density of health workforce per 10,000 populations. In comparison to global scenario, only 7 physicians and 17.1 nursing/midwife personnel were available per 10,000 population in India.[35] The Rural Health Statistics (2014-2015) indicate that in case of PHC, there was a shortfall of 49.2% for female health assistant and 61.3% for male health assistants. A significant percentage of sanctioned posts were found to be vacant at all levels. For instance, 10.5% of the sanctioned posts of HW (Female)/auxiliary nurse midwives (ANMs) were vacant at SC and PHCs, 27.0% of the sanctioned posts for doctors at PHC were vacant. The statistics highlight that 8.1% of the PHCs were functioning without a doctor, 38.1% without a laboratory technician and 21.9% without a pharmacist.[34]
Discordance in drug availability at primary care level
The availability of essential technologies and medicines to treat NCDs at the primary care level is an essential prerequisite. While there is an essential drug list for all PHCs, there remains a discordance in the availability of these recommended and essential drugs for NCDs, which are either not available or their supplies are intermittent.
Absence of noncommunicable diseases standards
Although the IPHS outlines separate standards and guidelines for SC, PHC, and CHC, the lack of NCD focus is conspicuous in these standards.
Targets, Strategies, and Interventions for Noncommunicable Diseases Care
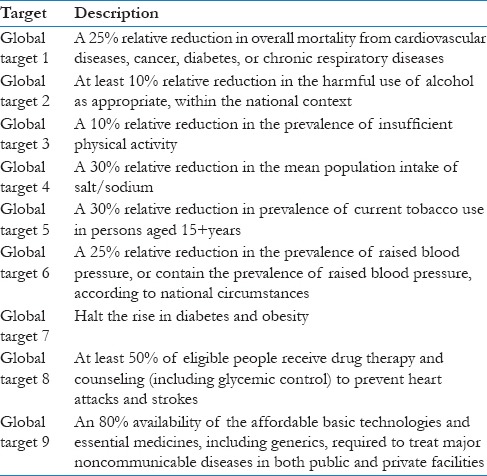
The voluntary global NCD targets, set out by the Global Action Plan for Prevention and Control of NCD 2013-2020, adopted by the World Health Assembly in 2013[36] is shown in Table 2.
Table 2.
Global noncommunicable disease targets for prevention and control of noncommunicable diseases 2013-2020
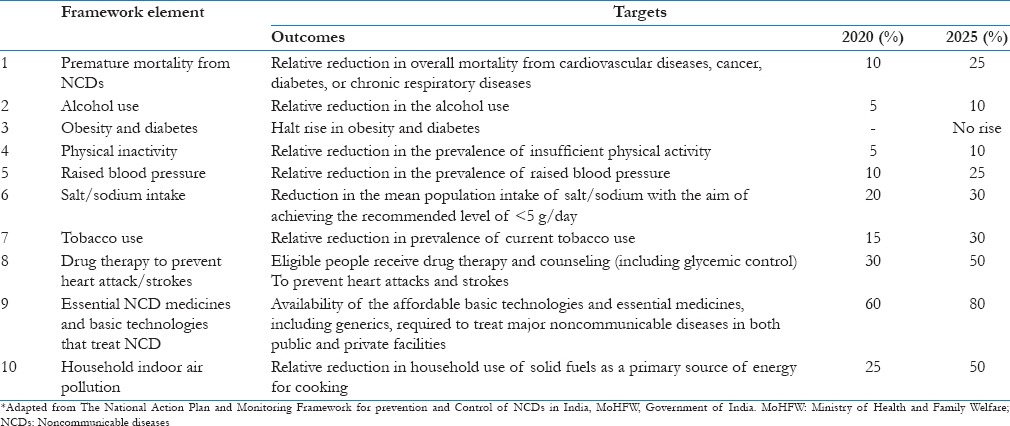
As a WHO member state, India is committed to implement an appropriate action plan to meet the objectives under the Global Action Plan. The National NCD Monitoring framework was established in India in 2013, outlines indicators and targets which will be used to track the progress of actions designed to prevent and control NCDs.[37] Table 3 outlines the key targets and timelines set in this framework.
Table 3.
Indicators and targets for prevention and control of noncommunicable disease in India*
It is important that strategy and policy frameworks for NCD prevention and control comprehensively contribute to overall health system strengthening. The key areas critical for NCD containment efforts have therefore been aligned with the building blocks of the WHO Health System framework [Figure 2].
Figure 2.
Aligning noncommunicable diseases containment approaches with the WHO Health System building blocks
Toward addressing India specific needs in noncommunicable diseases prevention and management
Amidst the diverse nature and complexities involved in delivering a comprehensive NCD care, an impetus to prioritize NCD control efforts in India is much needed. Concerted efforts must be made to build a well-defined and strategic framework for new solutions, ensuring effectivity and scale-up of already existing NCD interventions at the primary care levels. It is essential that there is dedicated political commitment and widespread population coverage of such interventions at the ground level.
Policy-based interventions
An operational multisectoral national policy and guidelines for the management of NCD through sustainable primary care should be developed. The overarching policy, specific to NCDs should advocate the need for strengthening social frameworks at the primary care level.
Robust surveillance mechanisms
Provision of reliable and timely data on NCD complications, quality of healthcare, or health expenditures is critical and calls for the need for a robust surveillance system. Under this system, routine data collection for chronic diseases in primary care; data for registration, and all causes of death including NCD should be collated and analyzed, thus leading to a consolidated database that could be used by communities.
Intersectoral collaborations
Increased interactions among the public and private sector as well as the civil society should be encouraged. A holistic approach that involves such multisectoral experiences including those from the Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homoeopathy and allied health science practitioners will help create an enabling environment to promote healthy lifestyles.
Integration of existing national noncommunicable diseases-related programs
Implementation of NCD-specific programs should not only be strengthened but also consolidated under the broader umbrella of national health missions to enable integration of primary care with public health. Appropriate evaluation and monitoring of existing policies and programs with focus on both economic and health outcomes should be simultaneously performed.
Strengthening health systems
The existing health systems should be empowered by ensuring uninterrupted supply of diagnostics and key NCD drugs, easy access to facilities, and capacity for early disease detection. This also encompasses increased capacity building through training of health-care workforce to deliver primary care services and increased focus on research to identify low-cost solutions deliverable at primary care level.
Education and awareness
Public awareness for successful implementation of existing programs, development and promotion of health education and awareness programs, promoting the importance of self-care and NCD management at household level should also be encouraged. Social scientists, civil societies, and research groups should come together to identify and disseminate information related to existing best and impactful practices pertaining to NCD care. Innovative approaches, customized according to local priorities should be developed and implemented. In addition, promotional efforts encouraging lifestyle modification and behavioral changes at primary care levels, to attenuate the effects of NCD risk factors should also be enhanced.
Newer investment mechanisms
Financing schemes for risk protection among the poor, increased investments in primary health care, social and private insurance funded care for all chronic diseases need to be explored.
Use of information and communication technology
As technology is set to change the health-care landscape, use of information and communication technology to aid understanding of the local needs and design of integrated solutions should be encouraged.
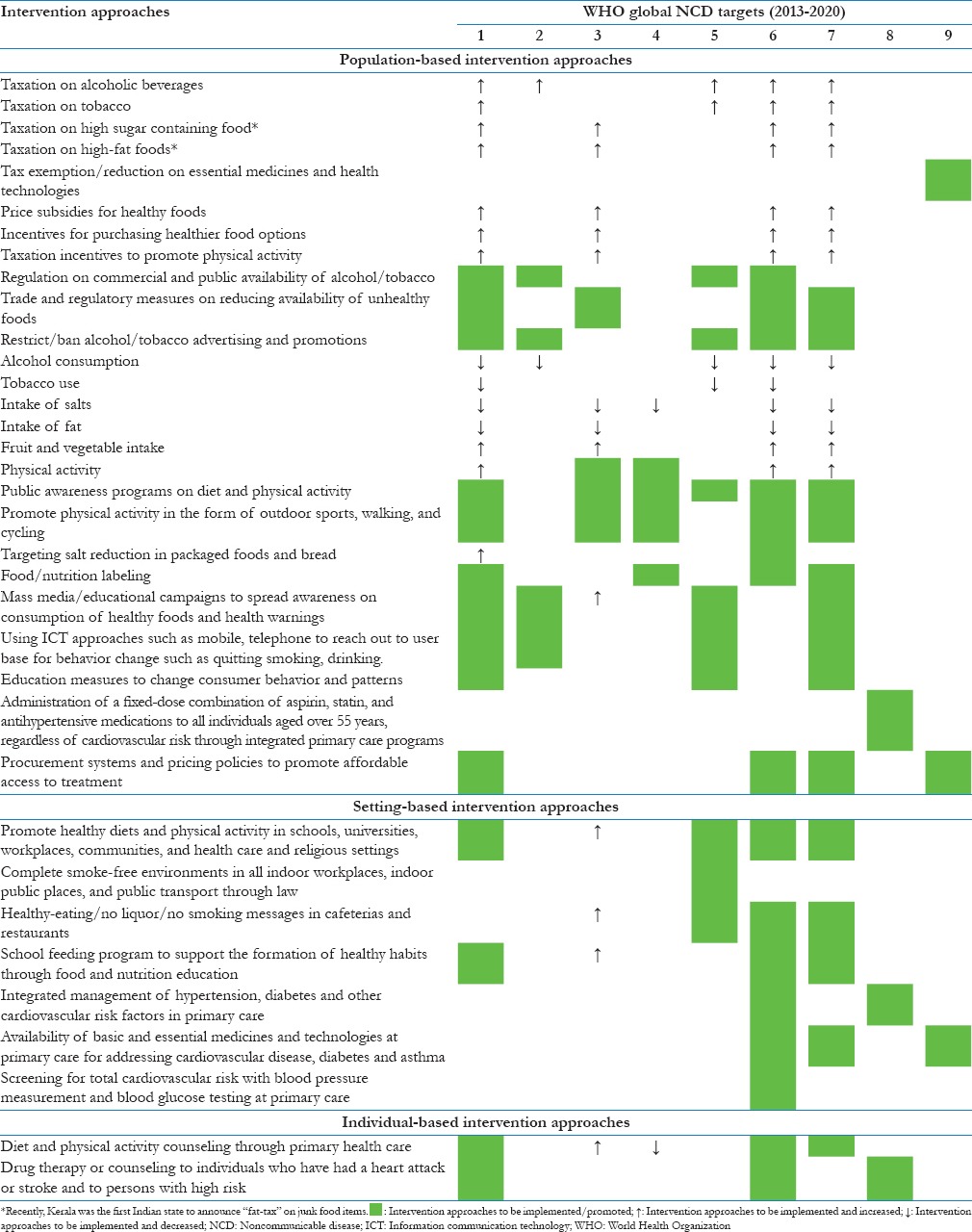
In line with the country-specific requirements and based on wholesome analysis of the globally existing and suggested NCD interventions, some of the possible interventions which could be adopted to support Indian efforts to achieve global NCD targets have been summarized in Table 4.
Table 4.
Key intervention areas to accelerate India's progress toward achieving the global noncommunicable disease targets
Conclusion
While the SDGs aspire to achieve universal health coverage, the current article analyses India's present health system preparedness in tacking the NCD burden. The review concludes that India must strive toward improving efforts to tackle NCD management and emphasizes on the relevance of empowering the primary care system. It is critical that NCD care service delivery models at the primary care level are articulated well keeping in view the Indian scenario and implemented so as to make them available and accessible to the most vulnerable sections of society.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.The Millennium Development Goals Report 2015, United Nations. [Last cited on 2017 Nov 08]. Available from: http://www.undp.org/content/dam/undp/library/MDG/english/UNDP_MDG_Report_2015.pdf .
- 2.Fehling M, Nelson BD, Venkatapuram S. Limitations of the millennium development goals: A literature review. Glob Public Health. 2013;8:1109–22. doi: 10.1080/17441692.2013.845676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Global Status Report on Noncommunicable diseases 2010. [Last cited on 2017 Nov 08]. Available from: http://www.who.int/nmh/publications/ncd_report2010/en/
- 4.NCD Alliance Position Paper: Post-2015 Global Health Thematic Consultation, The NCD Alliance. [Last cited on 2017 Nov 29]. Avaiable from: https://ncdalliance.org/sites/default/files/rfiles/NCDA%20submission%20to%20post-2015%20global%20thematic%20on%20health_Final_30%20Dec%202012.pdf .
- 5.European Commission Public Consultation: Towards a Post-2015 Development Framework, The NCD Alliance. [Last cited on 2017 Nov 10]. Available from: https://ncdalliance.org/sites/default/files/rfiles/NCD%20Alliance%20submission%20to%20EC%20post-2015%20consultation.pdf .
- 6.Lopez AD, Williams TN, Levin A, Tonelli M, Singh JA, Burney PG, et al. Remembering the forgotten non-communicable diseases. BMC Med. 2014;12:200. doi: 10.1186/s12916-014-0200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global Status Report on Noncommunicable diseases 2014, World Health Organization. [Last cited on 2017 Nov 12]. Available from: http://www.who.int/nmh/publications/ncd-status-report-2014/en/
- 8.Noncommunicable Diseases, Factsheet, World Health Organization. [Last cited on 2017 Nov 10]. Available from: http://www.who.int/mediacentre/factsheets/fs355/en/
- 9.Bloom DE, Cafiero ET, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. The Global Economic Burden of Noncommunicable Diseases. Geneva: World Economic Forum; 2011. [Last cited on 2017 Nov 12]. Available from: http://apps.who.int/medicinedocs/documents/s18806en/s18806en.pdf . [Google Scholar]
- 10.Health in 2015: from MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals, World Health Organization. [Last cited on 2017 Nov 12]. Avaiable from: http://www.who.int/gho/publications/mdgs-sdgs/en/
- 11.Minas H, Tsutsumi A, Izutsu T, Goetzke K, Thornicroft G. Comprehensive SDG goal and targets for non-communicable diseases and mental health. Int J Ment Health Syst. 2015;9:12. doi: 10.1186/s13033-015-0003-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel V, Parikh R, Nandraj S, Balasubramaniam P, Narayan K, Paul VK, et al. Assuring health coverage for all in India. Lancet. 2015;386:2422–35. doi: 10.1016/S0140-6736(15)00955-1. [DOI] [PubMed] [Google Scholar]
- 13.Yadav S, Arokiasamy P. Understanding epidemiological transition in India. Glob Health Action. 2014;7:23248. doi: 10.3402/gha.v7.23248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burden of NCDs and their Risk Factors in India, World Health Organization. [Last cited on 2017 Nov 18]. Available from: http://www.searo.who.int/india/topics/noncommunicable_diseases/ncd_situation_global_report_ncds_2014.pdf?ua=1 .
- 15.Thakur J, Prinja S, Garg CC, Mendis S, Menabde N. Social and economic implications of noncommunicable diseases in India. Indian J Community Med. 2011;36:S13–22. doi: 10.4103/0970-0218.94704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noncommunicable Diseases Country Profiles 2014, World Health Organization. [Last cited on 2017 Nov 22]. Available from: http://www.who.int/nmh/publications/ncd-profiles-2014/en/
- 17.Global Burden of Disease Data. [Last cited on 2017 Nov 22]. Available from: http://www.healthdata.org/gbd/data .
- 18.Yesudian CA, Grepstad M, Visintin E, Ferrario A. The economic burden of diabetes in India: A review of the literature. Global Health. 2014;10:80. doi: 10.1186/s12992-014-0080-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Global Adult Tobacco Survey GATS India 2009-10, Ministry of Health and Family Welfare, Government of India, New Delhi. [Last cited on 2017 Nov 22]. Available from: http://www.searo.who.int/tobacco/documents/2010-pub2.pdf .
- 20.Economic Burden of Tobacco Related Diseases in India Executive Summary, Ministry of Health and Family Welfare, Government of India, New Delhi. [Last cited on 2017 Nov 12]. Available from: http://www.searo.who.int/india/topics/tobacco/economic_burden_of_tobacco_related_diseases_in_india_executive_summary.pdf .
- 21.Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Preventing Chronic Diseases-A Vital Investment, World Health Organization. [Last cited on 2017 Nov 08]. Available from: http://www.who.int/chp/chronic_disease_report/full_report.pdf .
- 23.Patel V, Chatterji S, Chisholm D, Ebrahim S, Gopalakrishna G, Mathers C, et al. Chronic diseases and injuries in India. Lancet. 2011;377:413–28. doi: 10.1016/S0140-6736(10)61188-9. [DOI] [PubMed] [Google Scholar]
- 24.Rao M, Mant D. Strengthening primary healthcare in India: White paper on opportunities for partnership. BMJ. 2012;344:e3151. doi: 10.1136/bmj.e3151. [DOI] [PubMed] [Google Scholar]
- 25.Priester R, Kane RL, Totten AM. How the Current System Fails People With Chronic Illnesses. 2005. [Last cited on 2017 Nov 30]. Available from: http://citeseerx.ist.psu.edu/viewdoc/download;jsessionid=480C66AB1B0D478DA5501BBF867C224D?doi=10.1.1.512.452&rep=rep1&type=pdf .
- 26.Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, et al. Prevention and management of chronic disease: A litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. 2010;376:1785–97. doi: 10.1016/S0140-6736(10)61353-0. [DOI] [PubMed] [Google Scholar]
- 27.Harris MF, Zwar NA. Care of patients with chronic disease: The challenge for general practice. Med J Aust. 2007;187:104–7. doi: 10.5694/j.1326-5377.2007.tb01152.x. [DOI] [PubMed] [Google Scholar]
- 28.Nolte E, McKee M. Caring for people with chronic conditions – A health systems perspective. Das Gesundheitswes. 2009;71:A127. [Google Scholar]
- 29.Narain JP. Integrating services for noncommunicable diseases prevention and control: Use of primary health care approach. Indian J Community Med. 2011;36:S67–71. doi: 10.4103/0970-0218.94712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kruis AL, Boland MR, Assendelft WJ, Gussekloo J, Tsiachristas A, Stijnen T, et al. Effectiveness of integrated disease management for primary care chronic obstructive pulmonary disease patients: Results of cluster randomised trial. BMJ. 2014;349:g5392. doi: 10.1136/bmj.g5392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Primary Health Care (Now More Than Ever), The World Health Report 2008, World Health Organization. [Last cited on 2017 Sept 30]. Available from: http://www.who.int/whr/2008/en/
- 32.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: The chronic care model, part 2. JAMA. 2002;288:1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 33.Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings, World Health Organization. [Last cited on 2017 Nov 15]. Available from: http://www.who.int/nmh/publications/essential_ncd_interventions_lr_settings.pdf .
- 34.Rural Health Statistics, Ministry of Health and Family Welfare Statistics Division, Government of India. [Last cited on 2017 Sep 28]. Available from: http://wcd.nic.in/sites/default/files/RHS_1.pdf .
- 35.World Health Statistics 2015, World Health Organization. [Last cited on 2017 Nov 11]. Available from: http://www.who.int/gho/publications/world_health_statistics/2015/en/
- 36.Global Action Plan for the Prevention and Control of NCDs 2013-2020, World Health Organization. [Last cited on 2017 Nov 28]. Available from: http://www.who.int/nmh/events/ncd_action_plan/en/
- 37.National Action Plan and Monitoring Framework for Prevention and Control of Noncommunicable Diseases (NCDs) in India, Ministry of Health and Family Welfare, Government of India, New Delhi. [Last cited on 2017 Nov 28]. Available from: http://www.searo.who.int/india/topics/cardiovascular_diseases/National_Action_Plan_and_Monitoring_Framework_Prevention_NCDs.pdf .



