Abstract
Background:
Anemia is one of the most common nutritional deficiency disorders affecting the pregnant women in the developing countries. Anemia during pregnancy is commonly associated with poor pregnancy outcome and can result in complications that threaten the life of both mother and fetus.
Objective:
The objective of the study was to estimate the prevalence of anemia among pregnant women and to determine its association with maternal and fetal outcomes.
Settings and Design:
This study design was a prospective, observational, community-based study.
Subjects and Methods:
Four hundred and forty-six pregnant women were included in the study from three primary health centers in Kolar district by multistage sampling technique and were followed up till 1 week after delivery.
Statistical Analysis:
The data were analyzed using SPSS version 22; correlation coefficient, Chi-square test, and logistic regression were used.
Results:
There was a significant overall improvement in the hemoglobin levels of pregnant during the follow-up (10.3–10.72 gm%). About 35.6% of the women had maternal or fetal morbidity. Anemia was one of the main pregnancy-related complications (62.3%), other complications include difficult labor (3%), postpartum hemorrhage, and preeclampsia 1.6% each abortions/stillbirths (3.5%). The fetal complications include low birth weight (25.5%) followed by premature delivery (0.2%) and birth asphyxia (0.5%).
Conclusions:
A high prevalence of anemia in pregnant women apparently increases the maternal and fetal risks. To improve maternal and fetal outcome, it is recommended that the primary health care has to be strengthened, prevention, early diagnosis, and treatment of anemia in pregnancy to be given priority.
Keywords: Fetal morbidity, maternal morbidity, prevalence
Introduction
Anemia is one of the most common nutritional deficiency disorders affecting the pregnant women; the prevalence in developed countries is 14%, in developing countries 51%, and in India, it varies from 65% to 75%.[1,2]
Anemia is the second most common cause of maternal death in India and contributing to about 80% of the maternal deaths caused by anemia in South East Asia.[2,3,4,5] Anemia is also an established risk factor for intrauterine growth retardation, leading on to poor neonatal health and perinatal death.[6,7,8,9,10]
The prospective observational study is undertaken to estimate the prevalence and to study maternal and early neonatal morbidity and mortality associated with anemia in a pregnant woman.
Subjects and Methods
A prospective observational study was conducted in three primary health centers (PHCs) of Kolar Taluk during March 2013-January 2015. A sample size of 446 pregnant women was estimated based on the prevalence of anemia of 59% among pregnant women (National Family Health Survey [NFHS]-3 survey) with 95% confidence level and with an absolute precision of 5%, including a dropout rate of 20%.
Multistage sampling technique was adopted to select the pregnant woman. Randomly selected three PHCs and the Accredited Social Health Activists (ASHA) workers of these PHC were trained and motivated to bring all the sampled antenatal care cases to the antenatal clinic at the PHC on fixed days. The pregnant woman was examined by the OBG consultant, and postgraduates and the data were collected. Pretested and a semi-structured questionnaire was used to collect the data; the woman were followed up every month with the help of ASHA worker until 1 week after delivery. The hemoglobin (HB) of the pregnant women was measured at the first visit and repeated at every 3rd month.
The HB measurements of the pregnant woman were measured using HemoCue analyzer (HemoCue Hb 301). Anemia was classified based on the WHO criteria; HB concentration of <11 g/dl was considered as anemia. HB concentration of 10–10.9 g/dl, 7–9.9 g/dl, and <7 g/dl was considered as mild, moderate, and severe anemia, respectively.
The pregnant women were counseled about their HB level and importance of consumption of the iron and folic acid tablets, locally available iron-rich foods and regular antenatal checkups, etc.
The data were analyzed using IBM SPSS Statistics V22.0 (IBM United States). The quantitative measures are presented by mean and standard deviation and qualitative variables by proportions. Chi-square test, correlation coefficient, and logistic regression were used for testing significance. P ≤ 0.05 was considered statistically significant.
Results
A total of 446 pregnant women were enrolled for the study and were followed up until 1st week after delivery. Out of 446 women enrolled, 427 women completed the follow-up with an attrition rate of 9.5%. Mean age of pregnant women was 22.4 years. Most of the women were Hindus, belonging to schedule cast (SC)/schedule tribes (ST) (57.4%) and below poverty line (89%).
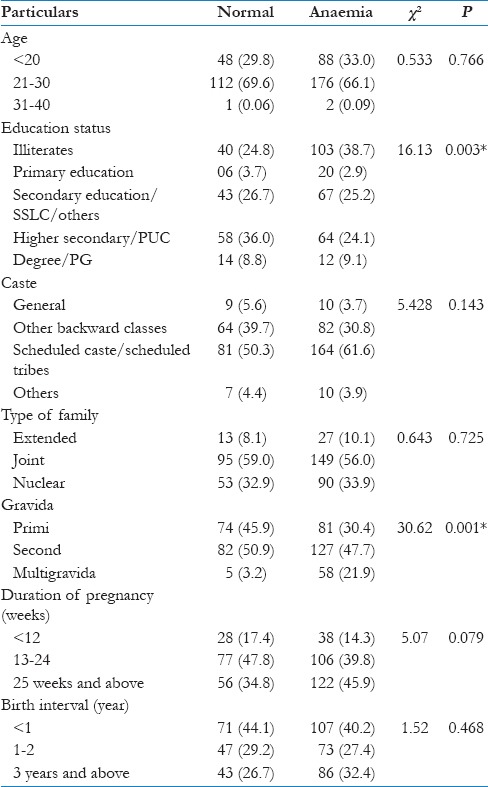
The prevalence of anemia was 62.3% in pregnant women, and it was observed that anemia was common in the age group of 21–30 years (66.1%), SC/ST (61.6%), and OBC (30.8%). There was a significant association of anemia status with educational status and gravida. The prevalence of anemia increased with the duration of pregnancy, but it was not statistically significant. Anemia is more common in the women with birth interval <1 year (40.2%) [Table 1].
Table 1.
Prevalence of anemia according to the sociodemographic status of the study participants
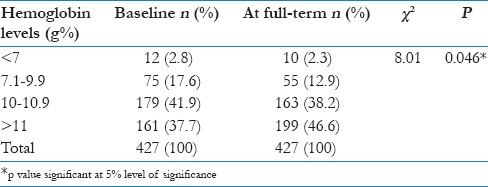
During the follow–up, there was a significant improvement in the HB levels from a mean of 10.3-10.72 g%. The number of women having various grades of anemia reduced and the number of women with normal HB increased during the follow-up this was statistically significant [Table 2].
Table 2.
Comparison of anemia status between baseline and at the end of the study
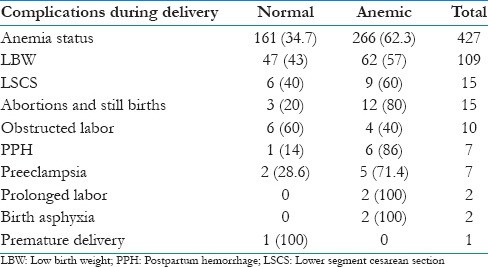
Nearly 35.6% of the pregnant women encountered maternal and fetal morbidity. Majority of the fetal and maternal complications were observed in anemic women. Out of 15 participants who underwent lower segment cesarean section (LSCS) and 60% were anemic. Similarly, 80% of participants who had abortions, 40% of obstructed labor, 86% of postpartum hemorrhage (PPH), 71.4% of preeclampsia, and all the women with prolonged labor were anemic. Around 25% of women delivered low birth babies, 57% of low birth weight (LBW) babies, 69% of abortions/stillbirths, and all the newborn with birth asphyxia occurred in mothers who were anemic [Table 3].
Table 3.
Distribution of pregnant women according to complications and anemia status
No significant positive correlation between birth weight and follow-up Hb of pregnant women was observed in this study (r = 0.041, P = 0.406).
No significant positive correlation was observed between birth weight and follow-up Hb of pregnant women (r = 0.041, P = 0.406).
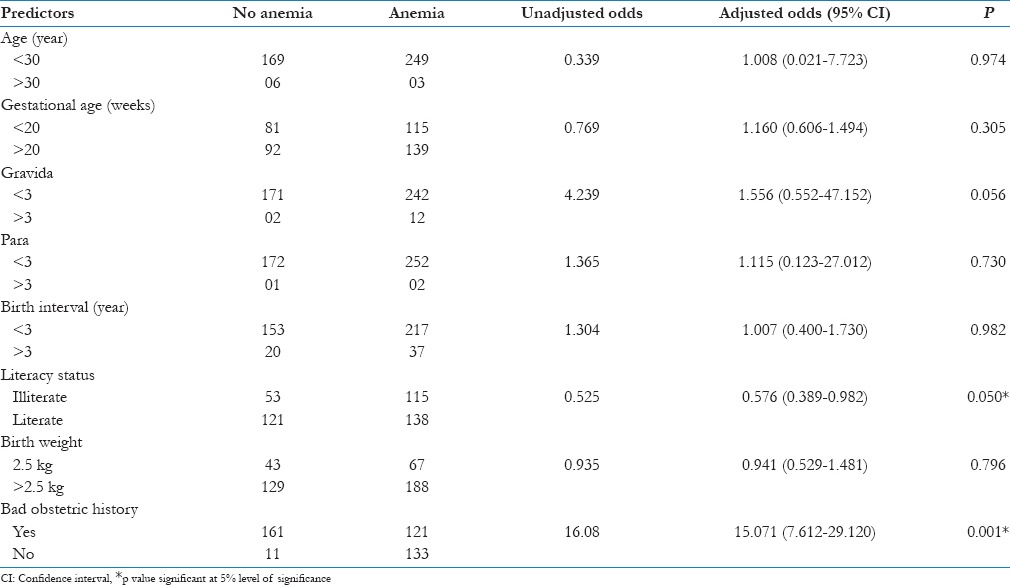
Independent factors contributing to the risk of anemia was evaluated by logistic regression model. It was observed that literacy status (OR = 0.576) and bad obstetric history (OR = 15.07) were the important and independent risk factors for anemia among pregnant women [Table 4].
Table 4.
Logistic regression analysis of risk factors in anemia and outcome
Discussion
Indian Council of Medical Research surveys showed that over 70% of pregnant women in the country were anemic.[2] Similar prevalence rate of anemia (63%) in pregnant women was observed in the present study. In contrast, very high prevalence was observed by Viveki et al., Totega, Agarwal et al., and Gautam et al. (82.9%, 84.9%, 84%, and 96.5%, respectively).[4,7,11,12] However, lower prevalence was reported from Nepal (42.5%) and Haryana (51%) and NFHS-2 and 3 (49.7%).[1,2,4]
Severe anemia among the participants in the present study was low (2.3%) which was similar to study by Kapil and Sareen (1.6%) and NHFS-2 (2.5%).[13] Whereas other studies reported higher prevalence; Totega (13.1%), Agarwal et al. (9.2%), Vivek et al. (7%), and Gautam et al. (22.8%).[4,7,11,12] In a study by Bhargavi Vemulapalli et al., 40.97% had a moderate degree of anemia and 6.28% of the population had a severe degree of anemia.[14] The high prevalence of anemia can be attributed to low dietary intake of iron and folic acid, deprived bioavailability of iron or chronic blood loss due to infections.[2]
Maternal anemia is considered as risk factor for poor pregnancy outcomes, and it threatens the life of fetus. Available data from India indicate that maternal morbidity rates are higher in anemic women.[2,9,15] In the present study, about 35.6% of the women had maternal and fetal morbidity, LSCS, abortions, obstructed labor, PPH, preeclampsia, prolonged labor, LBW, and birth asphyxia were commonly seen among anemic pregnant women.
There is a substantial amount of evidence showing that maternal iron deficiency anemia early in pregnancy can result in LBW subsequent to preterm delivery.[10] In the present study, around 25% of women delivered low birth babies; the majority of them (57%) were among women with anemia.
A study by Sangeetha in Bangalore reported highest (63%) prevalence of LBW among pregnant women, whereas Marahatta observed least (16.6%).[1,6] The other fetal complications among pregnant women in the present study include premature delivery (0.2%) and birth asphyxia (0.5%).
Studies in India demonstrated that the high proportion of maternal deaths are due to anemia in pregnant women,[8] whereas in the present study, there were no maternal deaths and no preterm delivery, whereas Marahatta in Nepal reported 3% preterm deliveries in anemic women.[1]
In the present study, gravida, education of pregnant women, and bad obstetric history were significantly associated with anemia. A study by Chowdhury et al. in Bangladesh also found that education of women was significantly associated with anemia in pregnancy,[16] whereas in a study by Singh et al. observed an insignificant association between anemia and gravida.[17]
Anemia seems to be higher among women with parity more than three in the present study, but it was not statistically significant. In a similar study conducted by Obse et al. in Ethiopia parity > 5 has a significant association with anemia.[18]
It was observed in the present study that, among pregnant women with birth interval more than 3 years, anemia was high with an odds ratio 2, in a similar study conducted by Alemayehu Bekele in Ethiopia birth interval was significantly associated with anemia with an odds ratio of 3.[19]
There was a significant statistical association between anemia and complications during pregnancy in the present study, which is similar to the study conducted by Nair et al.[20]
Conclusions
High prevalence of anemia in pregnant women (63%) indicates that anemia continues to be a major public health problem in rural areas of India. Anemia in pregnancy increases the maternal and fetal risks. Gravida status, female literacy, and bad obstetric history were important risk factors contributing for anemia in pregnant women.
To improve maternal and fetal outcome, it is recommended that the primary health care has to be strengthened and high priority has to be given to aspects such as prevention, early diagnosis, and treatment of anemia in pregnancy.
Health education on reproductive health, monitoring the consumption of iron folic acid tablets, early diagnosis of high-risk pregnancy, and appropriate management and strengthening of their healthcare-seeking behavior are important health-care measures to be undertaken at the community level. Furthermore, it is time for the realization that health system should focus on various factors that contribute to the occurrence of anemia and include them as important indicators in the National Health Policy.
Financial support and sponsorship
This study was financially supported by SDUAHER.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr. Mahesh V, Assistant Professor, Department of Community Medicine, Interns and Accredited Social Health Activists workers for their support in collection of data.
References
- 1.Marahatta R. Study of anaemia in pregnancy and its outcome in Nepal medical college teaching hospital, Kathmandu, Nepal. Nepal Med Coll J. 2007;9:270–4. [PubMed] [Google Scholar]
- 2.Kalaivani K. Prevalence and consequences of anaemia in pregnancy. Indian J Med Res. 2009;130:627–33. [PubMed] [Google Scholar]
- 3.Mbule MA, Byaruhanga YB, Kabahenda M, Lubowa A. Determinants of anaemia among pregnant women in rural Uganda. Rural Remote Health. 2013;13:2259. [PubMed] [Google Scholar]
- 4.Viveki RG, Halappanavar AB, Viveki PR, Halki SB, Maled VS. Prevalence of anaemia and its epidemiological determinants in pregnant women. Al Ameen J Med Sci. 2012;5:216–23. [Google Scholar]
- 5.Ahmad N. The prevalence of anaemia and associated factors in rural Indian community. Australas Med J. 2010;1:276–80. [Google Scholar]
- 6.Sangeetha VB, Pushpalatha S. Severe maternal anemia and neonatal outcome. Sch J Appl Med Sci. 2014;2:303–9. [Google Scholar]
- 7.Gautam VP, Bansal Y, Taneja DK, Saha R, Shah B, Marg Z, et al. Prevalence of anaemia amongst pregnant women and its socio-demographic associates in a rural area of Delhi. IJCM. 2002;27:157–60. [Google Scholar]
- 8.Iyengar K. Early postpartum maternal morbidity among rural women of Rajasthan, India: A community-based study. J Health Popul Nutr. 2012;30:213–25. doi: 10.3329/jhpn.v30i2.11316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ivan EA, Mangaiarkkarasi A. Evaluation of anaemia in booked antenatal mothers during the last trimester. J Clin Diagn Res. 2013;7:2487–90. doi: 10.7860/JCDR/2013/6370.3586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allen LH. Anaemia and iron deficiency: Effects on pregnancy outcome. Am J Clin Nutr. 2000;7:1280–4. doi: 10.1093/ajcn/71.5.1280s. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal KN, Agarwal DK, Sharma A, Sharma K, Prasad K, Kalita MC, et al. Prevalence of anaemia in pregnant & lactating women in India. Indian J Med Res. 2006;124:173–84. [PubMed] [Google Scholar]
- 12.Totega GS. Prevalence of anaemia among pregnant women and adolescent girls in 16 districts of India. Food Nut Bull. 2006;27:311–5. doi: 10.1177/156482650602700405. [DOI] [PubMed] [Google Scholar]
- 13.Kapil U, Sareen N. Prevalence of anemia amongst overweight and obese children in NCT of Delhi. IJCH. 2014;26:295–7. [Google Scholar]
- 14.Vemulapalli B, Rao KK. Prevalence of anaemia among pregnant women of rural community in Vizianagaram, North Coastal Andhra Pradesh, India. Asian J Med Sci. 2013;5:21–5. [Google Scholar]
- 15.Singh R, Chauhan R, Nandan D, Singh H, Gupata SC, Bhatnagar M. Morbidity profile of women during pregnancy: A hospital record based study in Western UP. IJCH. 2012;24:342–6. [Google Scholar]
- 16.Chowdhury HA, Ahmed KR, Jebunessa F, Akter J, Hossain S, Shahjahan M. Factors associated with maternal anaemia among pregnant women in Dhaka city. BMC Women Health. 2015;15:77. doi: 10.1186/s12905-015-0234-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh R, Singh AK, Gupta SC, Singh HK. Correlates of anaemia in pregnant women. Indian J Community Health. 2015;27:351–5. [Google Scholar]
- 18.Obse N, Mossie A, Gobena T. Magnitude of anaemia and associated risk factors among pregnant women attending antenatal care in Shalla Woreda, West Arsi Zone, Oromia Region, Ethiopia. Ethiop J Health Sci. 2013;23:165–73. [PMC free article] [PubMed] [Google Scholar]
- 19.Bekele A, Tilahun M, Mekuria A. Prevalence of anemia and its associated factors among pregnant women attending antenatal care in health institutions of Arba Minch town, Gamo Gofa Zone, Ethiopia: A Cross-sectional study. Anemia. 2016;2016:1073192. doi: 10.1155/2016/1073192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nair M, Choudhury MK, Choudhury SS, Kakoty SD, Sarma UC, Webster P, et al. Association between maternal anaemia and pregnancy outcomes: A cohort study in Assam, India. BMJ Glob Health. 2016;1:e000026. doi: 10.1136/bmjgh-2015-000026. [DOI] [PMC free article] [PubMed] [Google Scholar]


