Abstract
Background
Mental disorders often have onset early in life, contribute substantially to the global disease burden, and may interfere with young people’s ability to complete age-relevant tasks in important developmental periods. However, knowledge about prevalence and course of mental disorders in young adulthood is sparse. The aim of the current study was to estimate prevalence and stability of mental disorders from the twenties to the thirties/forties.
Methods
DSM-IV mental disorders were assessed with the Composite International Diagnostic Interview in two waves (1999–2004 and 2010–2011) in 1623 young adult Norwegian twins (63.2% women, aged 19–29 years in wave 1).
Results
In wave 1, the 12-month prevalence of any mental disorder among people in the twenties was 19.8% (men) and 32.4% (women), anxiety disorders: 9.6% (men) and 26.7% (women), anxiety disorders excluding specific phobias: 2.5% (men) and 6.9% (women), major depressive disorder (MDD): 4.4% (men) and 7.2% (women), and alcohol use disorder (AUD): 8.7% (men) and 4.4% (women). The prevalence of any mental disorder decreased from the twenties to the thirties/forties. This was due to a decrease in AUD and specific phobias. Anxiety disorders in the twenties predicted anxiety disorders and MDD ten years later, even when controlling for the association between these disorders in the twenties. MDD in the twenties predicted MDD ten years later. At both ages, two-week and 12-month prevalence estimates differed markedly for MDD - indicating an episodic course.
Conclusions
Common mental disorders are highly prevalent among young adults in the twenties, and somewhat less prevalent in the thirties/forties. Those who suffer from one mental disorder in the twenties are at considerably increased risk for suffering from a disorder ten years later as well. This may have significant implications for young people’s ability to attain education, establish a family, and participate in occupational life.
Electronic supplementary material
The online version of this article (10.1186/s12888-018-1647-5) contains supplementary material, which is available to authorized users.
Keywords: Mental disorders, Young adulthood, Health surveys, Prevalence, Stability
Background
Mental disorders are among the most prevalent health problems affecting the adult population [1]. The Global Burden of Disease Study 2015 (GBD 2015) estimated that seven of the top 25 causes of years lived with disability (YLD) globally were mental disorders, with major depressive disorder (MDD) ranked second and anxiety disorders ranked ninth [2]. The high rankings were a result of both high prevalence and the disability associated with these disorders. Estimates of 12-month prevalence of mental disorders vary between 9.6 and 27.8% in the general adult population [3–8]. Mood disorders, anxiety disorders (including specific phobias), and alcohol use disorders (AUD) are the most prevalent disorders and are included in all the above-mentioned studies.
Young adulthood
The shift in recent decades toward longer educations and higher age when committing to stable relationships and having children, has led researchers to aknowledge the age between 18 and 29 as an important developmental period [9]. It is characterized by changes in love and work life, and frequent residental change [9, 10]. Completing education and building a stable life structure are important developmental tasks in this period, while raising children is an important task for later periods [9, 10].
Mental health problems are associated with poor educational attainment as well as work and interpersonal problems [11–18]. Research results indicate that half of US adolescents’ failure to complete secondary school is attributable to mental disorders [19]. Mental disorders are also associated with maladaptive parenting behaviors, such as low affection toward the child and inconsistent enforcement of rules [20]. Because mental disorders may interfere with developmental tasks in different periods, we need to increase our knowledge about the prevalence and stability of such disorders at different ages to be able to correctly assess the magnitude of this problem.
Prevalence of mental disorders in young adulthood
Findings from the New Zealand Mental Health Survey (NZMHS), the Dutch Tracking Adolescents’ Individual Lives Survey (TRAILS), the US National Comorbidity Survey (NCS) and its replication (NCS-R), and the Children in the Community Study (CICS) from the US, show 12-month prevalence estiatmes of MDD between 8.3 and 12.4% among people between 18 and 33 years [16, 21–23]. The 12-month prevalence was between 19.4 and 22.3% for anxiety disorders (including specific phobias), between 2.5 and 10.3% for acohol dependence, and between 7.1 and 18.4% for alcohol abuse [21–23].
Stability of mental disorders in young adulthood
Previous studies indicate that the prevalence of depression is stable over the earliest part of adulthood, whereas AUD decreases, and findings regarding anxiety disorders are mixed [21, 24]. In the Dunedin study from New Zealand, the 12-month prevalence of MDD was 16.8% at age 21 years and 16.3% at 32 years [21]. The 12-month prevalence of any anxiety disorder (including specific phobias) was 20.3% at 21 years and 22.2% at 32 years. In the Simmons Longitudinal Study from the US, prevalence estiamtes of MDD showed a weak and not statistically significant increase from age 21 to 30 (from 5.4 to 8.0%), while there was a decline in the 12-month prevalence for phobia (including specific phobias) (from 16.8 to 2.3%) [24]. The prevalence of alcohol dependence declined (from 18.4 to 8.1%) from age 21 to 32 in the Dunedin study, and the prevalence of AUD declined from 26.7 to 6.0% in the Simmons Longituidnal Study [21, 24].
Some people have long-lasting and/or recurrent episodes of mental disorders [25, 26]. In the general adult population, about 40% of those who have depression or anxiety at one time point, have been found to have at least one of these disorders 7 years later [27]. Having a disorder or mental health problems in adolescence increases the risk of such disorders/problems in early adulthood [18, 28–30]. Findings from the NCS follow-up (NCS-2) showed that having MDD or generalized anxiety disorder (GAD) in the twenties and thirties predicted having any of these disorders eleven years later [31]. Depression seems to be more episodic than anxiety disorders among adolescents, as shown by higher 12-month to 30-day prevalence ratios of mood than anxiety disorders [22].
Comorbidity
Comorbidity between mental disorders is extensive with up to 50% of those who have one mental disorder also having at least one additional comorbid mental disorder [4, 7, 32]. This is also reported among young people [33]. Comorbidity seems to a large degree to be due to common liablity factors for several disorders [34, 35] and is related to severity and chronicity [27, 33, 36, 37]. Hence, estimates of comorbidity in different developmental periods may increase our understanding of the potential effects of common mental disorders on young adults.
Need for further knowledge
Current knowledge on prevalence and stability of mental disorders among young adults relies heavily on results from the US and New Zealand. Longitudinal studies from several different countries are needed to inform policy makers in different parts of the world and to estimate global disease burden in this age period.
Previous prevalence estiamtes of any mental disorder or any anxiety disorder typically include specific phobias, which by definiton involves imapirment in circumscribed situations and can sometimes be treated in a single therapy session [38]. Prevalence estiamtes both including and excluding such phobias are therefore needed to plan mental health services for young adults.
Findings are divergent with regards to whether or not anxiety disorders become less prevalent during young adulthood. Previous studies have included different anxiety disorders when examining this. There is a lack of studies tracking the episodic versus chronic nature of MDD and anxiety disorders across young adulthood. If depression tends to get more or less episodic over time, the burden of recurrent depression will decrease or increase as people get older. More knowledge about the stability of anxiety disorders and MDD from the twenties to the thirties/forties may increase our understanding of the potential impact of such disorders on young adult development. This is important for planning mental health services for young adults.
A limitation in several previous studies of AUD is different diagnostic criteria across waves and use of alcohol abuse as a screen for alcohol dependence [39]. This may affect estimates of prevalence and stability of this disorder [24, 39].
To the best of our knowledge, no previous studies have examined prevalence and stablity in common mental disorders by both: Following the same individuals from the twenties to the thirties/forties, estimating prevalence of anxiety disorders at the different ages including as well as excluding specific phobias, comparing the episodic versus chronic nature of disorders at both ages, and examining comorbidity between disorders at both ages.
Aims of the study
The overall aim of the current study was to address limitations in previous literature on prevalence and stability of common mental disorders from the twenties to the thirties/forties. More specifically, the aims were to: 1) Estimate the 12-month prevalence of anxiety disorders (with and without specific phobias), mood disorders, and AUD among people aged 19 to 29, 2) Compare these estimates to prevalence estimates ten years later, 3) Compare 12-month to two-week prevalence estimates to examine the episodic nature of disorders across these two developmental periods, 4) Examine the degree to which those who have an anxiety disorder or MDD in the twenties, are at increased risk of having these disorders ten years later, 5) Examine comorbidity of common mental disorders among people in the twenties and ten years later.
Methods
Sample
Data came from the Norwegian Institute of Public Health Twin Panel (NIPHTP), which includes health questionnaires at two time points (Q1 and Q2), and diagnostic interviews at two later time points (wave 1 and wave 2). The current study used data from the two interviews. The NIPHTP is described thoroughly elsewhere [40–44], and recruitment is illustrated in Fig. 1.
Fig. 1.
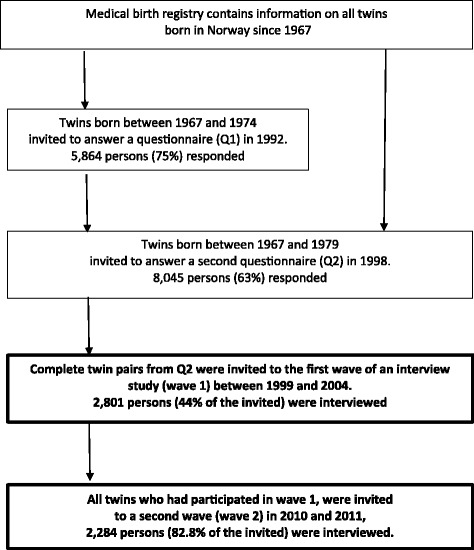
Flow-chart of recruitment to the study. The current study used data from the two interview studies, indicated with bold font
The first wave of the interview study (wave 1) took place between 1999 and 2004, and 2801 individuals (44% of the invited) were interviewed. All twins who had participated in wave 1 were invited for a re-interview between 2010 and 2011 (wave 2). The follow-up participation rate from wave 1 to wave 2 was 82.8% (n = 2284) [41]. Mean age was 28.3 years (range 19–36 years) in wave 1 and 37.9 years (range 30–44 years) in wave 2. Mean time between interviews was 9.6 years (range 7–13 years). Participation in wave 1 was predicted by increasing age and monozygosity, but not by any indicator of mental health [42]. Participation in wave 2 was predicted by high education, female sex, and monozygosity. Neither the total number of mental disorders nor any specific disorder in wave 1 predicted participation in wave 2 [41].
The current study aimed to examine mental disorders in a specific developmental period (19–29 years of age) and follow these individuals over time. Hence, only participants below age 30 in wave 1 were included in the main analyses. This resulted in a sample of 597 men and 1026 women in wave 1, and 457 men and 850 women in wave 2. Mean age in wave 1 was 25.4 years (range 19 to 29), and mean age in wave 2 was 35.3 years (range 30 to 42). Mean time between the two interviews was 9.6 years. Prevalence estimates for the wider age range of the entire sample were also calculated and are presented in Additional file 1: Tables S1 and S2, for readers who are interested in prevalence of mental disorders in a wider age group.
Measures
A Norwegian version of the computerized Munich Composite International Diagnostic Interview (M-CIDI), originally developed by the World Health Organization, was employed in both interview waves [45]. Diagnoses were coded according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). The interview was mainly administered face-to-face in wave 1. For practical reasons, 231 interviews (8.3%) were conducted by telephone. To maximize response rate, all the interviews were conducted by telephone in wave 2. Interviewers were mostly psychology graduate students or experienced psychiatric nurses who had received standardized training by certified instructors. Each twin in a pair was interviewed by a different interviewer.
Respondents answered one question about when they last experienced symptoms of each of the disorders. The response categories were “Within the last two weeks”, “Two weeks to less than a month”, “One to five months”, “6 to 12 months”, “Last 12 months, but cannot remember exactly when”, and “More than one year”. Endorsement of the first option was used to estimate 2-week prevalence, endorsement of any of the first two options to estimate 4-week prevalence, endorsement of any of the first three options to estimate 5(6) month-prevalence, and endorsement of any of the first five options to estimate 12-month-prevalence. Hence, individuals contributing to two-week prevalence estimates were a sub-group of those contributing to all other prevalence estimates of each disorder.
Table 1 shows an overview of combined categories of diagnoses. AUD consisted of alcohol abuse and alcohol dependence. Any mood disorder consisted of MDD and dysthymia. Any anxiety disorder W1 consisted of panic disorder, agoraphobia without a history of panic disorder, specific phobias, social phobia, GAD, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD). In wave 2, OCD and PTSD were not assessed. These two disorders are no longer classified as anxiety disorders in DSM-5 [46]. Any anxiety disorder W1–2 did not include these two disorders, and was constructed for both waves to allow comparison of anxiety disorders across age. Any anxiety disorder W1–2 excluding specific phobias consisted of all anxiety disorders measured in both waves except specific phobias. Any mental disorder W1 consisted of Any mood disorder, Any anxiety disorder W1, and AUD. Any mental disorder W1–2 consisted of Any mood disorder, Any anxiety disorder W1–2, and AUD. Any mental disorder W1–2 excluding specific phobias consisted of Any mood disorder, Any anxiety disorder W1–2 excluding specific phobias, and AUD.
Table 1.
Overview of disorders included in the combined categories
| Combined category | Includes | Constructed for wave |
|---|---|---|
| Any mood disorder | MDD, Dysthymia | 1 and 2 |
| Any anxiety disorder W1 | Panic disorder, Agoraphobia without a history of panic disorder, Specific phobias, Social phobia, GAD, OCD, PTSD. | 1 |
| Any Anxiety disorder W1–2 | Panic disorder, Agoraphobia without a history of panic disorder, Specific phobias, Social phobia, GAD. | 1 and 2 |
| Any anxiety disorder W1–2 excluding specific phobias | Panic disorder, Agoraphobia without a history of panic disorder, Social phobia, GAD. | 1 and 2 |
| AUD | Alcohol abuse, Alcohol dependence. | 1 and 2 |
| Any mental disorder W1 | Any mood disorder, Any anxiety disorder W1, AUD. | 1 |
| Any mental disorder W1–2 | Any mood disorder, Any anxiety disorder W1–2, AUD. | 1 and 2 |
| Any mental disorder W1–2 excluding specific phobias | Any mood disorder, Any anxiety disorder W1–2 excluding specific phobias, AUD. | 1 and 2 |
| Categories only presented in Supplementary table | ||
| Drug use disorder | Drug abuse, drug dependence. | 1 |
| Any substance use disorder | Drug use disorder, AUD. | 1 |
| Any disorder W1- supplement | Any mood disorder, Any anxiety disorder W1, Any substance use disorder | 1 |
Legends: MDD Major depressive disorder, GAD Generalized anxiety disorder, OCD Obsessive-compulsive disorder, PTSD Post-traumatic stress disorder, AUD Alcohol use disorder
W1 Wave 1, W2 wave 2
Total as well as sex-stratified prevalence estimates are presented for MDD, Any mood disorder, Any anxiety disorder (W1, W1–2, as well as W1–2 excluding specific phobias), AUD, and Any mental disorder (W1, W1–2, and W1–2 excluding specific phobias). Prevalence estimates for low frequent specific disorders (e.g. panic disorders and dysthymia) are only presented for both genders together. Drug use disorders (drug addiction and drug abuse) were only assess in wave 1, and are presented in Additional file 1: Table S1.
We report 12-month and 2-week prevalence estimates. The other two measured prevalences (5(6)-month and four-week) are presented in Additional file 1: Tables S1 and S2. Interested readers may use those estimates to compare findings with other studies that have used estimates between 12-month and two-week (as for example [22, 47]).
Statistical analyses
Analyses were performed in Stata version 15. Testing all the prevalence estimates for statistically significant gender differences would imply a large number of tests, thus increasing the risk of random findings. Such testing was therefore only performed for the following estimates: 12-month Any mental disorder W1–2, 12-month Any mood disorder, 12-month Any anxiety disorder W1–2, and 12-month AUD.
The 12-month and 2-week prevalence estimates were compared for MDD and Any anxiety disorder W1–2. Episodic disorders are expected to show higher 12-month than 2-week prevalences whereas the prevalences are expected to be more similar for more chronic disorders.
Absolute stability was examined by comparing prevalence estimates at the two waves. Only those who participated in wave 2, were included in significance testing of change in prevalence estimates, thus reducing the risk of bias du to potential selective attrition. Relative stability refers to the degree to which it is the same or different people who have a diagnosis across ages [48]. This was examined with logistic regression for MDD, Any anxiety disorder W1–2, and AUD, adjusted for age in wave 1. We also examined the degree to which MDD in wave 1 predicted having Any anxiety disorder W1–2 in wave 2, and vice versa, controlled for age. Because of low number of cases and thus low statistical power, AUD was not included. Men and women were collapsed in these analyses to increase statistical power.
Comorbidity within each wave was examined with tetrachoric correlations between MDD, Any anxiety disorders W1–2, and AUD. Comorbidity was also examined by showing the proportion of people with one disorder, who also had another disorder, and by illustrating how many of a hypothetical sample of 100 individuals who would have either one disorder, or a combination of two or three disorders. Men and women were collapsed.
The concordance between twins may affect results. First, standard errors may be too small due to clustering effects [49–51]. This was adjusted for by drawing clusters (twin-pairs) rather than individuals in the bootstrapping/jackknife process and by using the robust estimator for standard errors in logistic regression [49–51]. Second, sensitivity analyses were performed including only one twin from each pair, to see if this affected results.
Results
Prevalence estimates
We report results for 597 men and 1026 women (63.2%) who participated in wave 1 (Table 2) and 457 men and 850 women (65.0%) who also participated in wave 2 (Table 3).
Table 2.
Prevalence of mental disorders in wave 1 (age 19–29 years, n = 597 men and 1026 women)
| Men and women | Men | Women | Ratio (women/men) of 12-month prevalence estimates (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| 12 month prevalence (95% CI) |
Two-week prevalence (95% CI) |
12 month prevalence (95% CI) |
Two-week prevalence (95% CI) |
12 month prevalence (95% CI) |
Two-week prevalence (95% CI) |
||
| MDD | 6.2 5.0–7.4 |
1.3 0.7–1.8 |
4.4 2.8–6.3 |
0.8 0.2–1.6 |
7.2 5.5–8.8 |
1.6 0.9–2.4 |
|
| Dysthymia | 1.7 1.1–2.4 |
1.4 0.8–2.0 |
|||||
| Any mood disorder a | 7.3 5.9–8.6 |
2.3 1.5–3.0 |
4.9 3.2–6.8 |
1.2 0.4–2.2 |
8.7 6.7–10.6 |
2.9 1.9–4.0 |
1.79*** 1.19–2.68 |
| Any anxiety disorder W1 b | 20.4 18.3–22.7 |
15.2 13.5–17.3 |
9.6 7.0–12.4 |
5.9 4.2–8.2 |
26.7 23.7–29.7 |
20.7 18.1–23.5 |
|
| Any anxiety disorder W1–2 c | 19.8 17.7–22.0 |
14.8 13.0–16.7 |
9.3 7.0–12.3 |
5.7 4.0–7.9 |
26.0 23.1–29.0 |
20.1 17.4–22.7 |
2.80*** 2.13–3.68 |
| Any anxiety disorder W1–2 excluding specific phobias d | 5.3 4.2–6.6 |
3.2 2.3–4.1 |
2.5 1.3–4.2 |
1.3 0.5–2.6 |
6.9 5.3–8.7 |
4.2 3.0–5.7 |
|
| Specific phobias | 16.9 14.9–19.0 |
12.4 10.8–14.1 |
7.6 5.5–10.2 |
4.9 3.3–6.9 |
22.3 19.5–25.0 |
16.8 14.5–19.2 |
|
| Panic disorder | 1.5 1.0–2.2 |
0.4 0.1–0.7 |
|||||
| Agoraphobia without panic | 1.4 0.9–2.0 |
1.1 0.6–1.7 |
|||||
| Social phobia | 2.3 1.7–3.3 |
1.8 1.2–2.7 |
|||||
| GAD | 1.2 0.7–1.9 |
0.4 0.1–0.7 |
|||||
| OCD | 0.3 0.1–0.6 |
0.2 0.1–0.4 |
|||||
| PTSD | 1.2 0.7–1.8 |
0.7 0.4–1.2 |
|||||
| Alcohol abuse | 2.8 2.0–3.7 |
0.9 0.5–1.5 |
|||||
| Alcohol Dependence | 4.7 3.6–5.8 |
2.1 1.4–2.8 |
|||||
| AUD | 6.0 4.8–7.3 |
2.7 1.9–3.6 |
8.7 6.5–11.3 |
3.7 2.3–5.4 |
4.4 3.2–5.7 |
2.0 1.2–3.0 |
0.50*** 0.34–0.74 |
| Any mental disorder W1 e | 27.8 25.4–30.3 |
18.6 16.7–20.6 |
19.8 16.4–23.4 |
9.7 7.3–12.4 |
32.4 29.4–35.7 |
23.8 21.1–26.6 |
|
| Any mental disorder W1–2 f | 27.6 25.3–30.2 |
18.2 16.2–20.1 |
19.8 16.4–23.4 |
9.5 7.1–12.2 |
32.2 29.2–35.4 |
23.3 20.7–26.0 |
1.63*** 1.35–1.96 |
| Any mental disorder W1–2 excluding specific phobias g | 15.3 13.5–17.5 |
7.3 6.0–8.8 |
14.3 11.2–17.3 |
5.6 3.7–7.7 |
15.9 13.6–18.5 |
8.3 6.5–10.3 |
|
Legends: *** p < 0.001, MDD Major depressive disorder, GAD Generalized anxiety disorder, OCD Obsessive-compulsive disorder, PTSD Post-traumatic stress disorder, AUD Alcohol use disorders, i.e. alcohol dependence or alcohol abuse
CI Confidence interval. 95% CIs are based on standard errors obtained from bootstrapping (1000 replications), bias corrected for skewness in the bootstrap distribution, and adjusted for cluster-effects among twins
aMDD and/or dysthymia
bPanic disorder, agoraphobia without panic, specific phobias, social phobia, GAD, OCD, and/or PTSD
cPanic disorder, agoraphobia without panic, specific phobias, social phobia and/or GAD
dPanic disorder, agoraphobia without panic, social phobia and/or GAD
eAny mood disorder, Any anxiety disorder W1, AUD
fAny mood disorder, Any anxiety disorder W1–2, AUD
gAny mood disorder, Any anxiety disorder W1–2 excluding specific phobias, AUD
Table 3.
Prevalence of mental disorders in wave 2 (age 30–42 years, n = 457 men and 850 women)
| Men and women | Men | Women | Ratio (women/men) of 12-month prevalence estimates (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| 12 month prevalence (95% CI) |
Two-week prevalence (95% CI) |
12 month prevalence (95% CI) |
Two-week prevalence (95% CI) |
12 month prevalence (95% CI) |
Two-week prevalence (95% CI) |
||
| MDD | 5.0 3.8–6.3 |
1.1 0.6–1.7 |
3.3 1.9–5.2 |
0.9 0.2–1.9 |
5.9 4.3–7.5 |
1.2 0.6–2.0 |
|
| Dysthymia | 1.9 1.2–3.0 |
0.9 0.5–1.5 |
|||||
| Any mood disordera | 5.8 4.6–7.3 |
1.6 1.0–2.4 |
3.7 2.3–5.9 |
1.1 0.2–2.3 |
7.0 5.3–8.7 |
1.9 1.1–3.0 |
1.87** 1.10–3.17 |
| Any anxiety disorder W1–2b | 16.1 13.9–18.4 |
8.3 6.8–9.7 |
5.9 4.0–8.2 |
2.9 1.5–4.7 |
21.6 18.6–24.6 |
11.2 9.0–13.2 |
3.63*** 2.46–5.35 |
| Any anxiety disorder W1–2 excluding specific phobiasc | 6.5 5.2–8.0 |
2.6 1.8–3.7 |
2.6 1.3–4.3 |
0.9 0.2–1.9 |
8.5 6.7–10.7 |
3.5 2.4–5.0 |
|
| Specific phobias | 12.3 10.3–14.3 |
6.5 5.2–7.9 |
4.1 2.4–6.1 |
2.2 1.0–3.9 |
16.8 14.1–19.5 |
8.8 6.9–10.8 |
|
| Panic disorder | 2.1 1.4–3.0 |
0.5 0.2–1.1 |
|||||
| Agoraphobia without panic | 1.2 0.6–1.9 |
0.6 0.2–1.2 |
|||||
| Social phobia | 3.9 2.9–5.2 |
1.4 0.7–2.1 |
|||||
| GAD | 1.5 0.9–2.2 |
0.5 0.2–0.9 |
|||||
| AUD | 2.7 1.8–3.7 |
1.2 0.7–1.8 |
5.3 3.2–7.2 |
2.4 1.2–4.0 |
1.3 0.7–2.2 |
0.5 0.1–1.0 |
0.25** 0.12–0.50 |
| Any mental disorder W1–2d | 20.9 18.6–23.3 |
10.0 8.3–11.7 |
12.9 9.8–16.3 |
5.8 3.8–8.1 |
25.3 22.1–28.6 |
12.3 10.3–14.5 |
1.96*** 1.50–2.55 |
| Any mental disorder W1–2 excluding specific phobiase | 12.4 10.5–14.4 |
4.9 3.6–6.2 |
10.0 7.3–12.6 |
4.2 2.5–6.2 |
13.7 11.4–16.3 |
5.2 3.7–6.9 |
|
Legends: ** p < 0.01, *** p < 0.001, MDD Major depressive disorder, GAD Generalized anxiety disorder, AUD Alcohol use disorders, i.e. alcohol dependence or alcohol abuse
CI Confidence interval. 95% CIs are based on standard errors obtained from bootstrapping (1000 replications), bias corrected for skewness in the bootstrap distribution and adjusted for cluster-effects among twins
aMDD and/or dysthymia
bPanic disorder, agoraphobia without panic, specific phobias, social phobia and/or GAD
cPanic disorder, agoraphobia without panic, social phobia and/or GAD
dAny mood disorder, Any anxiety disorder W1–2, AUD
eAny mood disorder, Any anxiety disorder W1–2 excluding specific phobias, AUD
In wave 1, when the participants were in the twenties, Any anxiety disorder W1 was the most prevalent combined category of disorders for both men and women (see Table 2). The 12-month prevalence for Any anxiety disorder W1 was 9.6% (95% confidence interval (CI) = 7.0–12.4) for men and 26.7% (95% CI = 23.7–29.7) for women. For Any anxiety disorder W1–2, the 12-month prevalence was 9.3 (95% CI = 7.0–12.3) for men and 26.0% (95% CI = 23.1–29.0) for women. AUD ranked second among men (8.7% 12-month prevalence, 95% CI = 6.5–11.3), and Any mood disorder ranked second among women (8.7% 12-month prevalence, 95% CI = 6.7–10.6). Specific phobias were highly prevalent among men and women (12-month prevalence = 7.6% with 95% CI = 5.5–10.2 for men and 22.3% with 95% CI = 19.5–25.0 for women). AUD and Any mood disorder were the most common groups of disorders for men, and Any mood disorder was the most common group of disorders for women when specific phobias were excluded. Results from significance testing of gender difference showed that Any mental disorder W1–2, Any anxiety disorder W1–2, and Any mood disorder were more prevalent among women than men, while AUD was more prevalent among men than women (see Table 2).
In wave 2, the 12-month prevalence of Any anxiety disorder W1–2 was 5.9% (95% CI = 4.0–8.2) for men and 21.6% (95% CI = 18.6–24.6) for women (see Table 3). Again, this was mainly due to the high prevalence of specific phobias (12-month prevalence was 4.1% with 95% CI = 2.4–6.1 for men and 16.8% with 95% CI = 14.1–19.5 for women). Any mood disorder was the second most prevalent group of disorders among women (12-month prevalence 7.0% with 95% CI = 5.3–8.7), and AUD was the second most common disorder among men (12-month prevalence = 5.3% with 95% CI = 3.2–7.2). Any mental disorder W1–2, Any mood disorder, and Any anxiety disorder W1–2, were more prevalent among women than men, and the reverse was true for AUD (see Table 3).
Stability
There was a reduction in Any mental disorder W1–2, Specific phobias, and AUD from wave 1 to wave 2 (95% CI for differences did not include zero). Estimates were stable for MDD and Any anxiety disorder W1–2 excluding specific phobias (95% CI for difference included zero).
Relative stability was measured with logistic regression, presented in Table 4. Having MDD, Any anxiety disorder W1–2, or AUD in the twenties, increased the risk of having these disorders ten years later. The results showed that Any anxiety disorder W1–2 in wave 1 predicted MDD in wave 2, even controlled for MDD in wave 1.
Table 4.
Relative stability in mental disorders from age 19–29 to age 30–42 estimated with logistic regression
| Disorder in W1 not adjusted for each other OR (95% CI) |
MDD and Anxiety in W1 mutually adjusted for each other OR (95% CI) |
|
|---|---|---|
| MDD in wave 2 | ||
| MDD in wave 1 | 3.56*** (1.81–6.98) |
2.60** (1.31–5.17) |
| Anxiety in wave 1 | 2.61*** (1.54–4.42) |
2.18** (1.26–3.75) |
| Anxiety in wave 2 | ||
| MDD in wave 1 | 3.94*** (2.36–6.60) |
1.77 (0.96–3.26) |
| Anxiety in wave 1 | 9.01*** (6.45–12.59) |
8.33*** (5.90–11.78) |
| AUD in wave 2 | 8.10*** | |
| AUD in wave 1 | (3.69–17.76) | |
Legends: OR Odds ratio, CI Confidence interval, MDD Major depressive disorder, Anxiety = Any anxiety disorder W1–2 (Panic disorder, agoraphobia without panic, specific phobias, social phobia and/or generalized anxiety disorder (GAD)). Standard errors were obtained from the robust estimator in Stata, accounting for cluster-effects among twins
Men and women were collapsed in the analyses to increase statistical power. All analyses were adjusted for age in wave 1
Despite relative stability from wave 1 to wave 2, 82.4% of those who had MDD, 54.9% of those who had Any anxiety disorder W1–2, and 85.4% of those who had AUD in Wave 1 (12-mont prevalence), did not have the same disorder in wave 2.
12-month versus 2-week prevalence estimates
The 12-month prevalence of MDD was significantly higher than the 2-week prevalence in both waves. The 12-month to two-week ratios for MDD was 4.8 (95% CI = 3.9–7.5) in wave 1 and 4.6 (95% CI = 3.1–8.6) in wave 2. For Any anxiety disorder W1–2 the ratios were 1.3 (95% CI = 1.3–1.4) in wave 1 and 1.9 (95% CI = 1.7–2.2) in wave 2, indicating a more episodic nature of MDD than anxiety disorders.
Comorbidity
Tetrachoric correlations between 12-month MDD, Any anxiety disorder W1–2, and AUD within each wave are presented in Table 5. There was a strong association between MDD and Any anxiety disorder W1–2 in both waves.
Table 5.
Tetrachoric correlations between different disorders at wave 1 (age 19–29) and wave 2 (age 30–42)
| Wave 1 | Wave 2 | ||||||
|---|---|---|---|---|---|---|---|
| MDD | Anxiety W1–2a |
AUD | MDD | Anxiety W1–2a |
AUD | ||
| Wave 1 | MDD | 0.45*** | 0.00 | 0.31** | 0.38*** | 0.16 | |
| Anxiety W1–2a | 0.10 | 0.26** | 0.65*** | 0.02 | |||
| AUD | 0.07 | 0.07 | 0.49*** | ||||
| Wave 2 | MDD | 0.54*** | 0.12 | ||||
| Anxiety W1–2a | 0.03 | ||||||
| AUD | |||||||
Legends: aPanic disorder, agoraphobia without panic, specific phobias, social phobia and/or generalized anxiety disorder (GAD)
MDD Major depressive disorder. AUD Alcohol use disorders, i.e. alcohol dependence or alcohol abuse. Standard errors were obtained from the jackknife estimator, accounting for cluster-effects among twins. **p < 0.01, ***p < 0.001. Men and women were collapsed to increase statistical power
Comorbidity was also examined by calculating how many of those who had one disorder, also had another disorder. The results are presented in Table 6. The comorbidity numbers for AUD should be interpreted with caution in wave 2, as few people had this diagnosis. Figure 2 shows the number of people with pure versus comorbid MDD, Any anxiety disorder W1–2, and AUD in hypothetical samples of 100 men and 100 women in the twenties and in the thirties/forties.
Table 6.
Comorbidity wave 1 (age 19–29) and wave 2 (age 30–42)
| Men | Women | |||||
|---|---|---|---|---|---|---|
| % with comorbid MDD | % with comorbid Anxiety W1–2 a | % with comorbid AUD | % with comorbid MDD | % with comorbid Anxiety W1–2a |
% with comorbid AUD | |
| Wave 1 | ||||||
| MDD | 34.6 17.6–55.6 |
3.8 0–14.3 |
66.2 54.8–76.8 |
6.8 1.5–13.7 |
||
| Anxiety W1–2a | 15.8 7.3–26.8 |
17.5 8.5–27.3 |
17.4 13.1–21.9 |
5.9 3.6–9.0 |
||
| AUD | 1.9 0–7.1 |
17.5 8.5–27.3 |
11.1 3.4–21.1 |
35.6 22.2–50.0 |
||
| Wave 2 | ||||||
| MDD | 33.3 13.0–53.6 |
16.7 3.7–31.8 |
57.0 46.5–67.0 |
2.0 0.0–5.4 |
||
| Anxiety W1–2a | 17.4 8.3–31.1 |
8.7 2.0–18.0 |
19.5 14.8–24.3 |
1.7 0.3–3.4 |
||
| AUD | 11.4 2.9–23.3 |
11.8 3.0–23.5 |
14.3 0.0–37.5 |
7.1 0.0–25.0 |
||
Legends: MDD Major depressive disorder, AUD Alcohol use disorders, i.e. alcohol dependence or alcohol abuse
aPanic disorder, agoraphobia without panic, specific phobias, social phobia and/or generalized anxiety disorder (GAD)
Fig. 2.
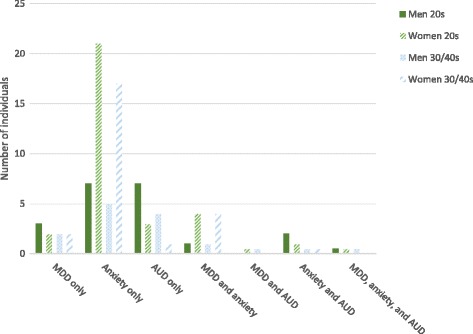
Combinations of disorders in hypothetical groups of 100 men and 100 women at different ages. Legend: MDD = major depressive disorder, Anxiety = Any anxiety disorder W1–2 (Panic disorder, agoraphobia without panic, specific phobias, social phobia and/or generalized anxiety disorder (GAD)), AUD = alcohol use disorder (i.e. alcohol dependence and alcohol abuse)
Sensitivity analyses of concordance between twins
As mentioned in the methods section, the use of twins may have affected results, and sensitivity analyses were therefore performed. If one twin did not have any mental disorder during the last 12 months in wave 1, the co-twin’s risk of having a mental disorder was 21.7% (compared to 27.8% in the full sample). When one twin had a mental disorder, the co-twin’s risk was 43.7%. This concordance between twins was expressed in an intraclass correlation of 0.21. Prevalence of MDD, Any anxiety disorders W1, AUD, and Any mental disorder W1 were estimated for a sub-sample where one twin was randomly chosen from each pair (see Table 7). The estimates were quite similar to estimates from both twins. The ratio of the results (estimates from the entire sample/estimates from only one twin) varied between 1.00 and 1.04.
Table 7.
Prevalence estimates in wave 1 when using both twins versus one twin in each pair
| 12-month prevalence estimate using both twins 95% CIc | 12-month prevalence estimate only including one twin from each pair 95% C.I. | Ratio Entire sample estimate/Estimate using one twin from each pair |
|
|---|---|---|---|
| MDD | 6.2 5.0–7.4 |
6.2 4.5–8.0 |
1.00 |
| Any anxiety disorder W1a | 20.4 18.3–22.7 |
19.6 17.2–22.5 |
1.04 |
| AUD | 6.0 4.8–7.3 |
5.8 4.4–7.5 |
1.03 |
| Any mental disorder W1b | 27.8 25.4–30.3 |
27.8 24.7–31.0 |
1.00 |
Legends: CI Confidence interval, MDD Major depressive disorder
aPanic disorder, agoraphobia without panic, specific phobias, social phobia, generalized anxiety disorder (GAD), obsessive-compulsive disorder (OCD), and/or post-traumatic stress disorder (PTSD)
AUD Alcohol use disorders, i.e. alcohol dependence or alcohol abuse
bAny mental disorder W1 = Any mood disorder, Any anxiety disorder W1, AUD
c95% CIs are based on standard errors obtained from bootstrapping (1000 replications), bias corrected for skewness in the bootstrap distribution, and adjusted for cluster-effects among twins
Discussion
MDD, anxiety disorders, and AUD were highly prevalent at age 19–29. The prevalence of mental disorders was lower at age 30–42, and this was mainly due to decrease in AUD and specific phobias. Prevalence estimates of MDD and anxiety disorders excluding specific phobias were stable in this period. Individuals who had MDD, an anxiety disorder, or AUD in the twenties were of increased risk of having these disorders in the thirties/forties compared to those who did not have these diagnoses in the twenties.
Prevalence estimates
The 12-month prevalence of depressive disorders in people in the twenties was lower in the current study compared to young adults in the CICS [16], the Dunedin study, NZMHS, NCS, and NCS-R [21, 23], but similar to the prevalence among 26-year-olds in the Simmons longitudinal study [24]. The current findings were very similar to results from these other studies with regard to prevalence of anxiety disorders in the twenties. In the Dunedin study, alcohol dependence among people aged 18 to 32 years was more prevalent than the broader category of AUD in both waves in the current study [21]. Likewise, the narrower category alcohol abuse was more prevalent in TRAILS and NCS-R than AUD in the current sample [22, 23]. In the Simmons longitudinal study, the prevalence of AUD was similar to the current results [24].
Our findings are in line with previous studies showing that anxiety disorders tend to be the most prevalent group of disorders, both in the general adult population and among young adults [21, 52]. The current results are in line with previous Norwegian findings of higher prevalence of specific phobias compared to international studies [6, 53].
The most prevalent groups of disorders were mood disorders and AUD among men and mood disorders among women when specific phobias were excluded. Such phobias are very common, but by definiton highly situation-specific. The current results allowed differentiating between this very circumscrbied disorder and mental disorders that affect people in more complex ways across different situations (e.g. MDD, GAD, and AUD).
Stability
Mental disorders became less prevalent as participants went from the twenties to the thirties/forties. Our results converge with findings from the Simmons Longitudinal study regarding a decrease in specific phobias and AUD [24]. Other anxiety disorders did not become less prevalent in the current study. Findings from the Dunedin study showed a marked decrease in acohol dependence, and quite stable prevalence of MDD and anxiety disorders (including specific phobias, GAD, panic disorder, agoraphobia, OCD, and PTSD) from age 21 to age 32 [21]. Decrease in AUD across young adulthood may reflect the circumstances of people in the twenties, who often do not have responsibility for children, and many are students.
Results from a previous study indicate that a third of those who met diagnostic criteria for AUD in late adolescence, also met criteria for AUD at age 26 [54]. In the current study, only about 15% of those who met diagnostic criteria for AUD in the twenties also had AUD in the thirties/forties. Hence, the course of AUD seems to be less chronic from the twenties to the thirties/forties than from late adolescence to age 26. Nevertheless, the current results showed that those who had AUD in the twenties, had increased risk of having AUD in the thirties/forties compared to those who did not have AUD in the twenties.
Previous studies have found that the majority of individuals with anxiety and depressive disorders at one time point are free from these disorders after three to 11 years [25–27, 55]. This was also the case in the current study. However, those who had MDD or anxiety disorders in the twenties, had increased risk of having these disorders in the thirties/forties compared to those who did not have the disorders in the twenties. This is in line with previous findings from a wider age group of adults (age 18 to 65 at baseline) [56].
Anxiety disorders in the twenties strongly predicted MDD ten years later, even controlling for MDD in the twenties, in line with findings of stable and unspecific genetic risk of mental disorders [34, 35, 57]. The association between MDD in the twenties and anxiety disorders in the thirties/forties, controlled for anxiety disorders in the twenties, was not statistically significant, which may be due to low statistical power. However, others have reported similar results by showing that baseline GAD predicted persistence of MDD, but not the other way around among adolescents and young adults in the NCS-2 [31]. This is also in line with other longitudinal findings from the general adult population, showing that anxiety at one time point predicted depression at a later time to a stronger degree than the reverse [58]. In the Netherlands Mental Health Survey and Incidence Study (NEMESIS), mood disorder at follow-up was predicted by anxiety disorders three years earlier, and incident anxiety disorder was predicted by previous mood disorders [59]. In the US National Epidemiological Survey on Alcohol and Related Conditions (NESARC), there was reciprocal longitudinal associations between incidence of MDD and GAD [60]. The Finnish Health 2011 study reported that baseline anxiety disorder predicted new-onset MDD at 11-year follow-up [61]. Hence, anxiety disorders and MDD seem to have common risk factors, but it is unclear whether anxiety is a more robust predictor of later MDD than the reverse.
MDD seemed to be more episodic in its nature than anxiety disorders, in line with previous studies [22, 55]. There was no change toward a more or less chronic course of any of these disorders when the participants got older.
Comorbidity
There was substantial comorbidity between disorders within each wave, in line with previous research [4, 7, 32, 37], and no evidence of increased or decreased comorbidity between MDD and anxiety disorders from the twenties to the thirties/forties. In both waves, more than half of women and about one third of men with MDD, also had an anxiety disorder. Among those who had an anxiety disorder, one in five or fewer, also had MDD. Young people with vulnerability of both MDD and anxiety, may at any time point have higher risk of experiencing a current anxiety disorder than current MDD because the latter disorder tends to be more episodic.
Implications for policy makers
Previous research has shown that most people with mental disorders go untreated [62, 63]. The current results highlight the need to make adequate treatment easily available for young adults, to help them cope with their developmental tasks (e.g. attain education and work experience). Easily available treatment is important because of the high prevalence of mental disorders in the twenties and the thirties/forties, and because these disorders were long lasting and/or recurrent across ten years for a substantial number of young adults.
The high prevalence of AUD between age 19 and 29 suggests that it is important to implement alcohol interventions particularly tailored to fit this age group and their often-changing life circumstances. Specific phobias may impose functional impairment only in particular situations, but may be serious if those situations are difficult to avoid. There seems to be a particularly high need for efficient treatment of specific phobias for people in the twenties.
Other anxiety disorders and MDD did not become less prevalent with age. Anxiety disorders and MDD did not become more episodic from the twenties to the thirties/forties, and comorbidity between them did not change during this period. Hence, mental health needs for other disorders than AUD and specific phobias are stable from the twenties to the thirties/forties, and many young adults will need treatment for more than one mental disorder.
As noted by Schaefer and colleagues, public knowledge about the very common nature of mental disorders may contribute to reduced stigma [64]. In line with this, public information about the current findings of high prevalence of mental disorders among young adults may contribute to reduced stigma in this age group.
Strengths and limitations
The major strength of the present study is the large population-based sample, which has been assessed twice across 10 years for DSM-IV disorders by structured interviews. However, some limitations warrant consideration. First, the results may not be generalizable to other age groups. Second, there may be bias in the results due to selection in recruitment and attrition at follow-up. People with mental health problems tend to be under-represented in survey studies [65]. However, as discussed above, mental health variables did not predict participation in either of the interview waves [41, 42], and bias due to selective response may thus not be substantial.
Third, the results are based on a sample of twins, which may reduce generalizability to the general population. A study from the US compared self-reported symptoms of depression, panic-phobia, somatization, and insomnia between twins and their non-twin relatives, and found that twins had significantly, but modestly, higher scores on the panic-phobia factor, but reported similar levels of psychiatric symptoms as their non-twin relatives on the other factors [66]. The authors concluded that “twins are typical for the general non-twin population in their risk for psychiatric symptoms and syndromes.” (p. 590). Nevertheless, the current findings may be affected by the fact that two individuals from each family were recruited to the study. There was substantial concordance between two twins in a pair regarding mental disorders. Sensitivity analyses were performed with only one twin from each pair included, and results were very similar to the results from both twins.
Conclusion
Mental disorders are common among young people in the twenties and the thirties/forties, but AUD and specific phobias seem to become less prevalent over this age period. Nevertheless, some people are at enduring increased risk of impaired functioning due to mental disorders in consecutive developmental periods. Policy makers should ensure that mental health interventions are available and tailored for young people to help them master their developmental tasks.
Additional file
Tables S1 and S2. Prevalence estimates not shown in the main files. (DOCX 30 kb)
Acknowledgements
Not applicable.
Funding
Supported by Research Council of Norway grant 196148/V50. Previous collection and analysis of twin data from this project was in part supported by grant MH-068643 from the National Institutes of Health and grants from the Norwegian Research Council, the Norwegian Foundation for Health and Rehabilitation, the Norwegian Council for Mental Health, the Borderline Foundation, and the European Commission. The funding bodies did not have any role in the design of the study, the collection, analysis, or interpretation of data, or in writing the manuscript.
Availability of data and materials
The raw data is confidential and cannot readily be shared. Data may be shared with researchers obtaining permissions from The Norwegian Twin Registry and the Regional Committees for Medical and Health Research Ethics. After permissions have been obtained, data can be made available from The Norwegian Twin Registry, contact: Thomas S. Nilsen: ThomasSevenius.Nilsen@fhi.no.
Abbreviations
- AUD
Alcohol use disorders
- CI
Confidence interval
- CICS
Children in Community Study
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- GAD
Generalized anxiety disorder
- GBD
Global Burden of Disease
- M-CIDI
Munich Composite International Diagnostic Interview
- MDD
Major depressive disorder
- NCS
US National Comorbidity Survey
- NCS-2
US National Comorbidity Survey follow-up
- NCS-R
US National Comorbidity Survey Replication
- NEMESIS
Netherlands Mental Helath Survey and Incidence Study
- NESARC
National Epidemiological Survey on Alcohol and Related Conditions
- NIPHTP
Norwegian Institute of Public Health Twin Panel
- NZMHS
New Zealand Mental Health Survey
- OCD
Obsessive-compulsive disorder
- PTSD
Post-traumatic stress disorder
- Q1
Questionnaire 1 in 1992
- Q2
Questionnaire 2 in 1998
- TRAILS
Tracking Adolescents’ Individual Lives Survey
- YLD
Years lived with disability
Authors’ contributions
KG: Contributed to the design of the study, conducted the analyses and interpreted the results, authored the manuscript and approved of the final manuscript as submitted. AKK: Contributed to the design of the study, interpretation of results, authored the manuscript and approved of the final manuscript as submitted. RN: Contributed to the design of the study, interpretation of results, authored the manuscript and approved of the final manuscript as submitted. GPK: Contributed to the design of the study, the data collection, interpretation of results, reviewed and revised the manuscript, and approved of the final manuscript as submitted. SEV: Contributed to the design of the study, interpretation of results, reviewed and revised the manuscript, and approved of the final manuscript as submitted. TR-K: Contributed to the design of the study, the data collection, the interpretation of results, reviewed and revised the manuscript and approved of the final manuscript as submitted.
Ethics approval and consent to participate
Participants provided written informed consent. The name of the ethics review board that approved of our study is “The regional committee for medical and health research ethics, South East D”. (Reference number: 2010/767).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12888-018-1647-5) contains supplementary material, which is available to authorized users.
Contributor Information
Kristin Gustavson, Email: krbr@fhi.no.
Ann Kristin Knudsen, Email: Ann.Kristin.Knudsen@fhi.no.
Ragnar Nesvåg, Email: ragnar.nesvag@legeforeningen.no.
Gun Peggy Knudsen, Email: GunPeggy.Knudsen@fhi.no.
Stein Emil Vollset, Email: SteinEmil.Vollset@fhi.no.
Ted Reichborn-Kjennerud, Email: Ted.Reichborn-Kjennerud@fhi.no.
References
- 1.Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, Bruffaerts R, de Girolamo G, de Graaf R, Gureje O, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, et al. Prevalence of mental disorders in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kringlen E, Torgersen S, Cramer V. Mental illness in a rural area: a Norwegian psychiatric epidemiological study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):713–719. doi: 10.1007/s00127-006-0080-0. [DOI] [PubMed] [Google Scholar]
- 6.Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatr. 2001;158(7):1091–1098. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]
- 7.Jacobi F, Hofler M, Strehle J, Mack S, Gerschler A, Scholl L, Busch MA, Hapke U, Maske U, Seiffert I, et al. Twelve-months prevalence of mental disorders in the German health interview and examination survey for adults - mental health module (DEGS1-MH): a methodological addendum and correction. Int J Methods Psychiatr Res. 2015;24(4):305–313. doi: 10.1002/mpr.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands mental health survey and incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–213. doi: 10.1007/s00127-010-0334-8. [DOI] [PubMed] [Google Scholar]
- 9.Arnett JJ, Zukauskiene R, Sugimura K. The new life stage of emerging adulthood at ages 18-29 years: implications for mental health. Lancet Psychiatry. 2014;1(7):569–576. doi: 10.1016/S2215-0366(14)00080-7. [DOI] [PubMed] [Google Scholar]
- 10.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. doi: 10.1037/0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- 11.Vander Stoep A, Beresford SAA, Weiss NS, McKnight B, Cauce AM, Cohen P. Community-based study of the transition to adulthood for adolescents with psychiatric disorder. Am J Epidemiol. 2000;152(4):352–362. doi: 10.1093/aje/152.4.352. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Merikangas KR, Berglund P, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-V. Arch Gen Psychiatry. 2003;60(11):1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- 13.Mojtabai R, Stuart EA, Hwang I, Eaton WW, Sampson N, Kessler RC. Long-term effects of mental disorders on marital outcomes in the National Comorbidity Survey ten-year follow-up. Soc Psychiatry Psychiatr Epidemiol. 2017;52(10):1217–1226. doi: 10.1007/s00127-017-1373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mojtabai R, Stuart EA, Hwang I, Susukida R, Eaton WW, Sampson N, Kessler RC. Long-term effects of mental disorders on employment in the National Comorbidity Survey ten-year follow-up. Soc Psychiatry Psychiatr Epidemiol. 2015;50(11):1657–1668. doi: 10.1007/s00127-015-1097-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mojtabai R, Stuart EA, Hwang I, Eaton WW, Sampson N, Kessler RC. Long-term effects of mental disorders on educational attainment in the National Comorbidity Survey ten-year follow-up. Soc Psychiatry Psychiatr Epidemiol. 2015;50(10):1577–1591. doi: 10.1007/s00127-015-1083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crawford TN, Cohen P, First MB, Skodol AE, Johnson JG, Kasen S. Comorbid Axis I and Axis II disorders in early adolescence: outcomes 20 years later. Arch Gen Psychiatry. 2008;65(6):641–648. doi: 10.1001/archpsyc.65.6.641. [DOI] [PubMed] [Google Scholar]
- 17.Ormel J, Oerlemans AM, Raven D, Laceulle OM, Hartman CA, Veenstra R, Verhulst FC, Vollebergh W, Rosmalen JG, Reijneveld SA, et al. Functional outcomes of child and adolescent mental disorders. Current disorder most important but psychiatric history matters as well. Psychol Med. 2017;47(7):1271–1282. doi: 10.1017/S0033291716003445. [DOI] [PubMed] [Google Scholar]
- 18.Veldman K, Reijneveld SA, Ortiz JA, Verhulst FC, Bultmann U. Mental health trajectories from childhood to young adulthood affect the educational and employment status of young adults: results from the TRAILS study. J Epidemiol Community Health. 2015;69(6):588–593. doi: 10.1136/jech-2014-204421. [DOI] [PubMed] [Google Scholar]
- 19.Vander Stoep A, Weiss NS, Kuo ES, Cheney D, Cohen P. What proportion of failure to complete secondary school in the US population is attributable to adolescent psychiatric disorder? J Behav Health Serv Res. 2003;30(1):119–124. doi: 10.1007/BF02287817. [DOI] [PubMed] [Google Scholar]
- 20.Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Arch Gen Psychiatry. 2001;58(5):453–460. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- 21.Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ormel J, Raven D, van Oort F, Hartman CA, Reijneveld SA, Veenstra R, Vollebergh WA, Buitelaar J, Verhulst FC, Oldehinkel AJ. Mental health in Dutch adolescents: a TRAILS report on prevalence, severity, age of onset, continuity and co-morbidity of DSM disorders. Psychol Med. 2015;45(2):345–360. doi: 10.1017/S0033291714001469. [DOI] [PubMed] [Google Scholar]
- 23.National Comorbidity Survey (NCS) [https://www.hcp.med.harvard.edu/ncs/ftpdir/NCS-R_12-month_Prevalence_Estimates.pdf].
- 24.Tanner JL, Reinherz HZ, Beardslee WR, Fitzmaurice GM, Leis JA, Berger SR. Change in prevalence of psychiatric disorders from ages 21 to 30 in a community sample. J Nerv Ment Dis. 2007;195(4):298–306. doi: 10.1097/01.nmd.0000261952.13887.6e. [DOI] [PubMed] [Google Scholar]
- 25.Lamers F, Beekman AT, van Hemert AM, Schoevers RA, Penninx BW. Six-year longitudinal course and outcomes of subtypes of depression. Br J Psychiatry. 2016;208(1):62–68. doi: 10.1192/bjp.bp.114.153098. [DOI] [PubMed] [Google Scholar]
- 26.Markkula N, Harkanen T, Nieminen T, Pena S, Mattila AK, Koskinen S, Saarni SI, Suvisaari J. Prognosis of depressive disorders in the general population- results from the longitudinal Finnish health 2011 study. J Affect Disord. 2016;190:687–696. doi: 10.1016/j.jad.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 27.Rhebergen D, Batelaan NM, de Graaf R, Nolen WA, Spijker J, Beekman AT, Penninx BW. The 7-year course of depression and anxiety in the general population. Acta Psychiatr Scand. 2011;123(4):297–306. doi: 10.1111/j.1600-0447.2011.01677.x. [DOI] [PubMed] [Google Scholar]
- 28.Copeland WE, Adair CE, Smetanin P, Stiff D, Briante C, Colman I, Fergusson D, Horwood J, Poulton R, Costello EJ, et al. Diagnostic transitions from childhood to adolescence to early adulthood. J child Psychol Psychiatry. 2013;54(7):791–799. doi: 10.1111/jcpp.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costello EJ, Copeland W, Angold A. The great Smoky Mountains study: developmental epidemiology in the southeastern United States. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):639–646. doi: 10.1007/s00127-015-1168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson JG, Cohen P, Kasen S. Minor depression during adolescence and mental health outcomes during adulthood. Br J Psychiatry. 2009;195(3):264–265. doi: 10.1192/bjp.bp.108.054239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychol Med. 2008;38(3):365–374. doi: 10.1017/S0033291707002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, de Girolamo G, Graaf R, Demyttenaere K, Gasquet I, et al. 12-month comorbidity patterns and associated factors in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:28–37. doi: 10.1111/j.1600-0047.2004.00328.x. [DOI] [PubMed] [Google Scholar]
- 33.Newman DL, Moffitt TE, Caspi A, Magdol L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. J Consult Clin Psychol. 1996;64(3):552–562. doi: 10.1037/0022-006X.64.3.552. [DOI] [PubMed] [Google Scholar]
- 34.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kendler KS, Aggen SH, Knudsen GP, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for Syndromal and Subsyndromal common DSM-IV Axis I and all Axis II disorders. Am J Psychiatr. 2011;168(1):29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lamers F, van Oppen P, Comijs HC, Smit JH, Spinhoven P, van Balkom AJ, Nolen WA, Zitman FG, Beekman AT, Penninx BW. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: the Netherlands study of depression and anxiety (NESDA) J Clin Psychiatry. 2011;72(3):341–348. doi: 10.4088/JCP.10m06176blu. [DOI] [PubMed] [Google Scholar]
- 37.Merikangas KR, Zhang HP, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study - the Zurich cohort study. Arch Gen Psychiatry. 2003;60(10):993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 38.Zlomke K, Davis TE., 3rd One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther. 2008;39(3):207–223. doi: 10.1016/j.beth.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 39.Grant BF, Compton WM, Crowley TJ, Hasin DS, Helzer JE, Li TK, Rounsaville BJ, Volkow ND, Woody GE. Errors in assessing DSM-IV substance use disorders. Arch Gen Psychiatry. 2007;64(3):379–380. doi: 10.1001/archpsyc.64.3.379. [DOI] [PubMed] [Google Scholar]
- 40.Nilsen TS, Knudsen GP, Gervin K, Brandt I, Roysamb E, Tambs K, Orstavik R, Lyle R, Reichborn-Kjennerud T, Magnus P, et al. The Norwegian twin registry from a public health perspective: a research update. Twin Res Hum Genet. 2013;16(1):285–295. doi: 10.1017/thg.2012.117. [DOI] [PubMed] [Google Scholar]
- 41.Reichborn-Kjennerud T, Czajkowski N, Ystrom E, Orstavik R, Aggen SH, Tambs K, Torgersen S, Neale MC, Roysamb E, Krueger RF, et al. A longitudinal twin study of borderline and antisocial personality disorder traits in early to middle adulthood. Psychol Med. 2015;45:1–11. [DOI] [PMC free article] [PubMed]
- 42.Tambs K, Ronning T, Prescott CA, Kendler KS, Reichborn-Kjennerud T, Torgersen S, Harris JR. The Norwegian Institute of Public Health Twin Study of mental health: examining recruitment and attrition Bias. Twin Res Hum Genet. 2009;12(2):158–168. doi: 10.1375/twin.12.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nilsen TS, Brandt I, Magnus P, Harris JR. The Norwegian twin registry. Twin Res Hum Genet. 2012;15(6):775–780. doi: 10.1017/thg.2012.57. [DOI] [PubMed] [Google Scholar]
- 44.Harris JR, Magnus P, Tambs K. The Norwegian Institute of Public Health twin program of research: an update. Twin Res Hum Genet. 2006;9(6):858–864. doi: 10.1375/twin.9.6.858. [DOI] [PubMed] [Google Scholar]
- 45.Wittchen HU, Pfister H. DIA-X interviews (M-CIDI): manual fur screening-Verfahren und interview. Frankfurt: Swets & Zeitlinger; 1997. [Google Scholar]
- 46.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: American Psychiatric Association; 2013.
- 47.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the great Smoky Mountains study. J Am Acad Child Adolesc Psychiatry. 2011;50(3):252–261. doi: 10.1016/j.jaac.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roberts BW, Wood D, Caspi A: The development of personality traits in adulthood. In: Handbook of personality theory and research. Third edn. Edited by John OP, Robins RW, Pervin LA. New York: Guilford; 2008: 375–398.
- 49.Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals, and other measures of statistical accuracy. Stat Sci. 1986;1(1):54–75. doi: 10.1214/ss/1177013815. [DOI] [Google Scholar]
- 50.Singh K, Xie M. Bootstrap: a statistical method. In: Peterson P, Baker E, McGaw B, editors. International encyclopedia of education. Edn: Amsterdam: Rutgers University NJ: Elsevier Science; 2010.
- 51.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New Jersey: Wiley-interscience; 2004. [Google Scholar]
- 52.Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, Ustun TB, Wang PS. The global burden of mental disorders: an update from the WHO world mental health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(1):23–33. doi: 10.1017/S1121189X00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sandanger I, Nygard JF, Ingebrigtsen G, Sorensen T, Dalgard OS. Prevalence, incidence and age at onset of psychiatric disorders in Norway. Soc Psychiatry Psychiatr Epidemiol. 1999;34(11):570–579. doi: 10.1007/s001270050177. [DOI] [PubMed] [Google Scholar]
- 54.Copeland WE, Angold A, Shanahan L, Dreyfuss J, Dlamini I, Costello EJ. Predicting persistent alcohol problems: a prospective analysis from the great Smoky Mountain study. Psychol Med. 2012;42(9):1925–1935. doi: 10.1017/S0033291711002790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Penninx BW, Nolen WA, Lamers F, Zitman FG, Smit JH, Spinhoven P, Cuijpers P, de Jong PJ, van Marwijk HW, van der Meer K, et al. Two-year course of depressive and anxiety disorders: results from the Netherlands study of depression and anxiety (NESDA) J Affect Disord. 2011;133(1–2):76–85. doi: 10.1016/j.jad.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 56.Lahey BB, Zald DH, Hakes JK, Krueger RF, Rathouz PJ. Patterns of heterotypic continuity associated with the cross-sectional correlational structure of prevalent mental disorders in adults. JAMA psychiatry. 2014;71(9):989–996. doi: 10.1001/jamapsychiatry.2014.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gillespie NA, Kirk KM, Evans DM, Heath AC, Hickie IB, Martin NG. Do the genetic or environmental determinants of anxiety and depression change with age? A longitudinal study of Australian twins. Twin Res. 2004;7(1):39–53. doi: 10.1375/13690520460741435. [DOI] [PubMed] [Google Scholar]
- 58.Fichter MM, Quadflieg N, Fischer UC, Kohlboeck G. Twenty-five-year course and outcome in anxiety and depression in the upper Bavarian longitudinal community study. Acta Psychiatr Scand. 2010;122(1):75–85. doi: 10.1111/j.1600-0447.2009.01512.x. [DOI] [PubMed] [Google Scholar]
- 59.de Graaf R, ten Have M, Tuithof M, van Dorsselaer S. First-incidence of DSM-IV mood, anxiety and substance use disorders and its determinants: results from the Netherlands mental health survey and incidence Study-2. J Affect Disord. 2013;149(1–3):100–107. doi: 10.1016/j.jad.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 60.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the wave 2 National Epidemiologic Survey on alcohol and related conditions. Mol Psychiatry. 2009;14(11):1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Markkula N, Marola N, Nieminen T, Koskinen S, Saarni SI, Harkanen T, Suvisaari J. Predictors of new-onset depressive disorders - results from the longitudinal Finnish health 2011 study. J Affect Disord. 2017;208:255–264. doi: 10.1016/j.jad.2016.08.051. [DOI] [PubMed] [Google Scholar]
- 62.Torvik FA, Ystrom E, Gustavson K, Rosenstrom TH, Bramness JG, Gillespie N, Aggen SH, Kendler KS, Reichborn-Kjennerud T. Diagnostic and genetic overlap of three common mental disorders in structured interviews and health registries. Acta Psychiatr Scand. 2018;137(1):54–64. doi: 10.1111/acps.12829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 64.Schaefer JD, Caspi A, Belsky DW, Harrington H, Houts R, Horwood LJ, Hussong A, Ramrakha S, Poulton R, Moffitt TE. Enduring mental health: prevalence and prediction. J Abnorm Psychol. 2016;126:212–24. [DOI] [PMC free article] [PubMed]
- 65.Torvik FA, Rognmo K, Tambs K. Alcohol use and mental distress as predictors of non-response in a general population health survey: the HUNT study. Soc Psychiatry Psychiatr Epidemiol. 2012;47(5):805–816. doi: 10.1007/s00127-011-0387-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kendler KS, Martin NG, Heath AC, Eaves LJ. Self-report psychiatric symptoms in twins and their nontwin relatives: are twins different? Am J Med Genet. 1995;60(6):588–591. doi: 10.1002/ajmg.1320600622. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1 and S2. Prevalence estimates not shown in the main files. (DOCX 30 kb)
Data Availability Statement
The raw data is confidential and cannot readily be shared. Data may be shared with researchers obtaining permissions from The Norwegian Twin Registry and the Regional Committees for Medical and Health Research Ethics. After permissions have been obtained, data can be made available from The Norwegian Twin Registry, contact: Thomas S. Nilsen: ThomasSevenius.Nilsen@fhi.no.


