Abstract
Introduction
Over-distension of urinary bladder in a high spinal cord injury patient is a triggering factor for autonomic dysreflexia. Removing triggering factors is vital to prevent autonomic dysreflexia.
Case presentation
A 36-year-old tetraplegic patient, who was managed by intermittent catheterizations performed by caregivers, developed recurrent autonomic dysreflexia during a week due to: 1) carers not performing intermittent catheterizations every night; 2) infrequent catheterizations during the day, leading to distension of urinary bladder. A day before his demise, carer attempted routine catheterization; but was unable to insert the catheter; blood pressure rose to 192/109 mmHg. Nifedipine 10 mg was administered. Thirty minutes later, blood pressure was 181/113 mmHg; second dose of Nifedipine was not given. Forty minutes elapsed before a senior carer came and catheterized successfully. Meanwhile, patient developed pounding headache; became drowsy; was talking incoherently. Four and half hours after unsuccessful catheterization, carers contacted emergency services and the patient was taken to Accident and Emergency; CT of head revealed very large acute intracranial hemorrhage in the right frontal and parietal lobes. The patient expired a day later. The Coroner’s verdict: “Patient died of massive intracranial hemorrhage caused by autonomic dysreflexia, a known complication of high spinal cord injury. Emergency protocols to manage autonomic dysreflexia were not followed in the days leading up to his death.”
Conclusion
Failed urethral catheterization is a potentially life-threatening emergency; every patient should have a care plan explicitly describing what should be done when catheterization is not successful. Preventive measures rather than episodic treatment of autonomic dysreflexia should be the guiding principle.
Keywords: spinal cord injury, autonomic dysreflexia, brain hemorrhage, tetraplegia, intermittent catheterization
Introduction
Autonomic dysreflexia is a syndrome of a massive imbalance of reflex sympathetic discharge occurring in spinal cord injury patients with lesions above the splanchnic outflow (T-6). It is characterized by acute hypertension, intense headache, sweating and facial flushing. Episodes of autonomic dysreflexia are triggered by various noxious and non-noxious stimuli below the level of spinal cord injury. Bladder distension alone accounts for up to 85% of cases; bowel distension due to fecal impaction accounts for 13%–19% of cases.1 A list of events or conditions that can cause episodes of autonomic dysreflexia and detailed pathophysiology of autonomic dysreflexia are available in a recent review by Stephenson and Berliner.2 Autonomic dysreflexia is more likely to be severe and readily activated if more than one peripheral stimulus is present simultaneously.
We report the case of a 36-year-old male tetraplegic patient, in whom carers were unable to insert a catheter for intermittent catheterization and there was delay before catheterization could be performed successfully. During this interval, the patient developed full bladder, which triggered autonomic dysreflexia and cerebral hemorrhage. We wish to convey that in addition to recognizing symptoms of autonomic dysreflexia and treating high blood pressure (e.g., sublingual administration of 5–10 mg of Nifedipine) promptly, removal of noxious stimuli that trigger autonomic dysreflexia is vital to prevent persistence of dysreflexia.
Case presentation
An 18-year-old male patient sustained fracture at C1–C2 in a road traffic accident in 1998; he developed tetraplegia (American Spinal Injury Association grade A) at the C1/C2 level. This patient underwent phrenic pacer implantation for diaphragmatic breathing; he had stented tracheostomy and baclofen pump implantation for intrathecal administration of baclofen to control spasticity. He developed diabetes mellitus; he was managed in the community by 24-hour carers. Carers were advised to perform intermittent urethral catheterizations every 4 hours.
In July 2016, this patient developed recurrent episodes of autonomic dysreflexia during a week due to carers not performing intermittent catheterizations during every night, which led to over-distension of urinary bladder. Furthermore, he did not have regular 4 hourly catheterizations during the day, which resulted in distension of urinary bladder. (Table 1) The day before this patient’s demise, a carer performed routine catheterization; but it failed; blood pressure rose to 192/109 mmHg. Nifedipine 10 mg was administered. The patient was communicating normally; then he complained of “banging head”. Thirty minutes later, blood pressure was 181/113 mmHg; second dose of Nifedipine was not given. Forty minutes elapsed before a senior carer came and catheterized successfully. The patient developed pounding headache and became drowsy and was talking incoherently. Bowel evacuation was then performed. During this period, the patient had fluctuating level of consciousness. Blood pressure was 141/94 mmHg.
Table 1.
Chronological record of events culminating in severe autonomic dysreflexia and demise of this patient
| Days before death and time | Symptoms | Signs | BP, HR | Procedure done | Treatment given |
|---|---|---|---|---|---|
| 6 days, 0750 hours | Feeling unwell; sweating | Urine: offensive smell | HR: 30–32 | Urethral catheterization; drained 1000 mL | Paracetamol 1 g |
| 5 days, 0700 hours | Headache; did not feel well | BP: 129/93; HR: bradycardia | GP contacted; advised to consult spinal unit. Spinal unit: patient was having dysreflexic episodes and advised 4 hourly catheterizations. Catheterization was done at 1800, 2200 and 0800 hours. Penile sheath was applied overnight but no urine was drained. No catheterization between 2200 and 0800 hours | Paracetamol at 0915 hours and at 1300 hours | |
| 4 days | Sweating; excessive spasms | BP not recorded | 4 hourly catheterizations until 2000 hours; intermittent catheterization was not performed overnight; sheath drained 800 mL urine | Paracetamol at 2245 hours | |
| 3 days | “Urine was concentrated.” | ||||
| 2 days | Headache at 1000 hours | Had a restless night | 115/87 | Raised temperature at 2240 hours | Paracetamol at 0200, 1000 and 2240 hours |
| 1 day, 0500 hours | Headache | 192/109; HR: 49 | Catheterization attempted but failed; patient became unconscious | Nifedipine 10 mg | |
| 1 day, 0530 hours | Patient in and out of consciousness | 181/113 | BP was not rechecked after 5 minutes; the second dose of Nifedipine was not administered. | ||
| 1 day, 0540 hours | “Pounding headache” | Drowsy – unconscious | 180/110 | Catheterization was successfully performed. | No further doses of Nifedipine were administered. |
| 1 day, 0600 hours | Not fully awake and alert | Bowel care was administered without consent of patient. | Carer was advised by a senior carer not on site that Nifedipine could make a patient drowsy. | ||
| 1 day, 0735 hours | Very drowsy and was talking but not making any sense. | 141/94 | Nifedipine was not administered. | ||
| 1 day, 0902 hours | Spinal unit was contacted – advised to call 999. At 0928 hours, 999 was called; arrived in hospital at 0955 hours; CT scan was performed at 1046 hours. Cerebral hemorrhage |
Abbreviations: BP, blood pressure; HR, heart rate.
Four and half hours after unsuccessful catheterization, emergency services were contacted. In the Accident and Emergency, CT of the head was performed. CT head showed very large acute intracranial hemorrhage in the right frontal and parietal lobes. (Figure 1) There was extension into the ventricular system with large amount of fresh blood present in the right lateral ventricle and fresh blood layering in the occipital horns of both lateral ventricles. There was fresh blood in the third and fourth ventricles (Figure 2). There was mild dilatation of the ventricular system; significant mass effect with global effacement of surface cerebral sulci and moderate midline shift to the left (Figure 3).
Figure 1.
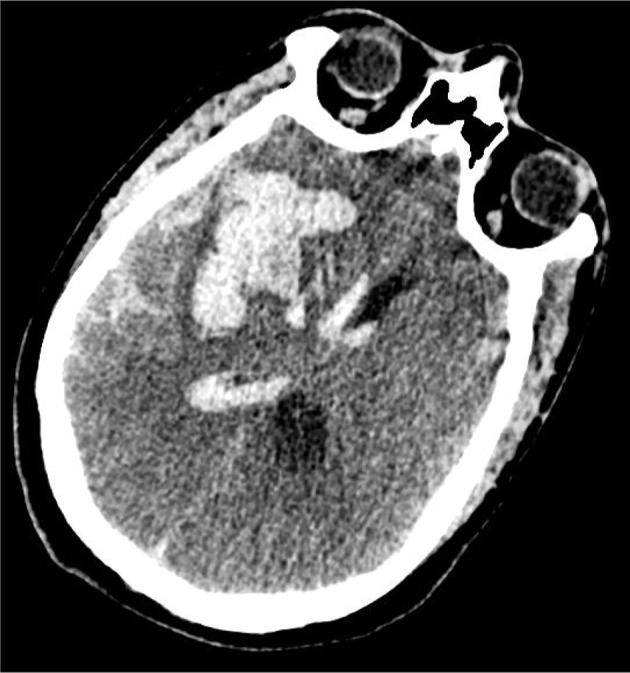
CT of head: Axial image showing large right intra-cerebral hemorrhage with extension into the ventricular system and subarachnoid space.
Figure 2.
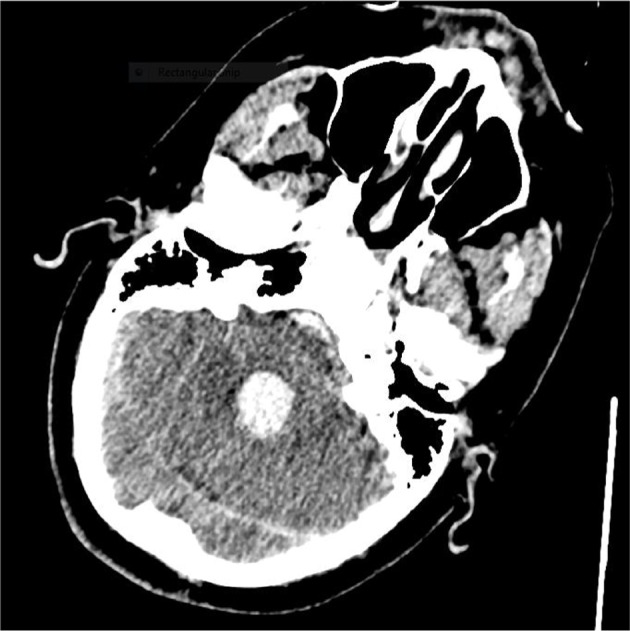
CT of head: Axial image showing hemorrhage extending down into dilated fourth ventricle.
Figure 3.
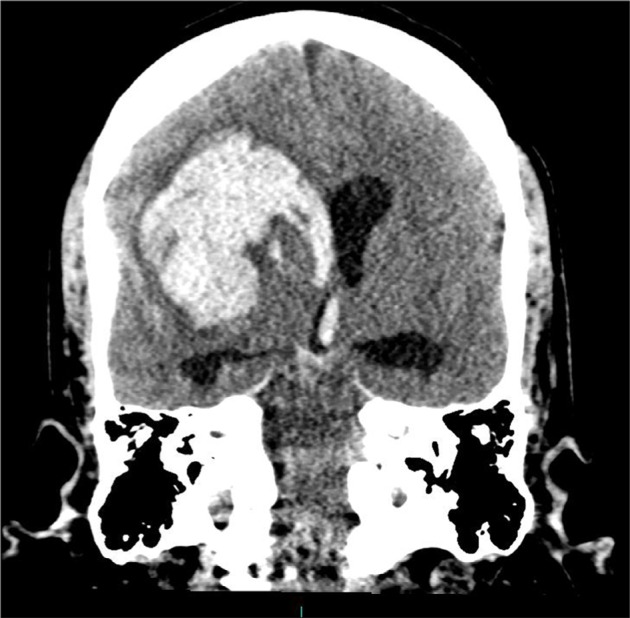
CT of head: Coronal reformat showing large right intra-cerebral hemorrhage extending in to right lateral and third ventricles; mass effect with effacement of sulci and midline shift to the left.
The patient was deeply unconscious. Neurosurgical team advised no surgical intervention in view of massive intracranial hemorrhage. He was declared “not for cardiopulmonary resuscitation”. Phrenic pacemaker supported breathing; otherwise, he was totally apneic. His wish was not to be permanently connected to artificial ventilator support. A second opinion from a neurosurgical colleague was sought on management of this patient. Mother (next of kin) and carers were aware of the very poor outcome. The patient was pronounced dead the following day.
Post-mortem examination was not performed. There was an inquest by Coroner. The Coroner concluded that the patient died of massive intracranial hemorrhage caused by autonomic dysreflexia, a known complication of a high spinal injury. Emergency protocols to manage this condition were not followed in the days leading up to his death.
Consent
The leading author discussed the publication of this case report with the mother of the deceased; she kindly agreed for publication of her son’s case report and images in an open access journal so that health professionals can read and learn from what happened to her son.
Discussion
Autonomic dysreflexia is a life-threatening complication of chronic traumatic spinal cord injury. Location of hemorrhage in autonomic dysreflexia-induced cases is similar to that in the general population.3 Wan and Krassioukov reviewed literature to identify documented cases of autonomic dysreflexia associated with life-threatening outcomes and death.4 Thirty-two cases of death or life-threatening complications of autonomic dysreflexia were found. Twenty-three (72%) cases were central nervous system-related, 7 (22%) were cardiovascular-related, and 2 (6%) were pulmonary-related.
Yoo and associates described a 45-year-old quadriplegic male who suffered left basal ganglia and thalamic hemorrhage associated with autonomic dysreflexia during surgery for pressure sore defects in the prone position under local anesthesia.5 Early and removal of triggering factors for dysreflexia failed to bring blood pressure under control. The patient continued to deteriorate neurologically and died 9 days after the attack. This case illustrates that a preventive measure rather than treatment of autonomic dysreflexic episode is vital to avoid life-threatening complications of dysreflexia.
Management of autonomic dysreflexia starts primarily with its prevention.6 Prompt recognition of autonomic dysreflexia, quick control of blood pressure, and removal of the triggering factors of autonomic dysreflexia, are important to get favorable outcome.3 In our patient, autonomic dysreflexia was detected and 10 mg of Nifedipine was administered by carers. But the triggering factor (distended urinary bladder) was not removed immediately. Continued presence of triggering factor for nearly 40 minutes resulted in persistent autonomic dysreflexia; along with inadequate control of blood pressure, persistent dysreflexia led to cerebral hemorrhage that proved fatal.
Villanueva and Hemstreet reviewed and compared the different methods to overcome difficult male urethral catheterization in able-bodied individuals, and identified 6 main approaches, which include blind passage or under direct vision of a filiform, guide wire, Glidewire or hydrophilic catheter; and technique of instillation of 60 cc of saline through the catheter as it is advanced.7 Instillation of 10–20 mL of 1% lidocaine jelly per urethra as the lubricant can make the procedure more tolerable for the patient and may prevent sphincter spasm. Perineal pressure by another person during catheter insertion helps direct the catheter into the prostatic urethra. Coude catheters prevent injury to the membranous and bulbar urethra.8
In high spinal cord injury patients, mechanical stretch of the anal sphincter (anal stretch) reduces the activity of external urethral sphincter and leads to relaxation of both detrusor and external sphincter muscles.9 Wu and associates suggested that this technique can be useful in clinical practice for aiding catheterization in patients with spastic urethral sphincter.10
In spinal cord injury patients in whom urethral catheterization is unsuccessful because of spastic sphincter, we explain anal stretching technique to the patient and take informed consent for performing this procedure. We carry out this maneuver by inserting a finger in anal canal and stretching the anal sphincter. The health professional stretches the anal sphincter with the index finger; simultaneously pressure is applied cephalad over the perineum with the thumb. The patient is asked to take a deep breath and relax. Then a catheter is advanced through urethra. If the patient has not moved bowels, inserting a finger in rectum and stretching anal sphincter can predispose to bowel emptying and soiling of perineum. The health professional should wear appropriate attire in anticipation of this eventuality. If bowel emptying occurs, full manual evacuation is completed before proceeding with urethral catheterization.
Patients who manage neurogenic lower urinary tract dysfunction by intermittent catheterization should have a care plan explicitly describing what should be done in situations, when carer is not able to insert a catheter per urethra in the community as well as the time frame for action. We practice the following steps:
Catheterization should be performed urgently by an experienced carer.
If intermittent catheterization is done through penile sheath, the penile sheath should be removed before attempting catheterization. If catheterization is done using a catheter with a protective sheath, it is advisable to use a different catheter that does not have such a sheath. Holding the penis directly without a penile sheath and inserting a naked catheter without protective sheath enable the person who performs catheterization to get better purchase of penis as well as the catheter. Improved grip of the penis without the penile sheath and increased tactile sensation to fingers holding and inserting a naked catheter, greatly aid in achieving successful catheterization in challenging clinical situation.
If the patient is very tense, or has lot of spasms, it is likely that urethral sphincter also may be spastic. Drugs to relax pelvic musculature (Diazepam 5–10 mg intra-muscularly or Midazolam 10 mg through buccal administration) may be helpful to get a catheter inserted past the spastic sphincter. When possible, patients are reassured and encouraged to relax.
Penis is held securely with the non-dominant hand with sterile gauze around it; penis is held pointing at a 45° angle. The catheter is detached from the bag to allow ease of insertion and better sensitivity at detecting when passing through the external sphincter and prostate.
Instilling 2% lidocaine gel in urethra before catheterization helps to prevent sphincter spasm.
Coudé-tipped catheter or Tiemann catheter, which is angled upward at the tip to assist in negotiating the upward bend in the male urethra, or Carson Foley catheter with medium olive coude tip to assist in navigation of restrictions in urethra, should be used.
In male patients, just before inserting a catheter, another carer inserts a finger in anal canal and stretches anal sphincter; stretching of anal sphincter relaxes urethral sphincter and facilitates passage of catheter through spastic urethral sphincter.
In female patients, a carer separates the labia and holds them apart. The person who performs catheterization inserts a finger in vagina and lifts anterior vaginal wall, then inserts catheter per urethra with the other hand.
If bladder drainage cannot be achieved without delay, the patient should be taken to the nearest Accident and Emergency immediately. Bladder puncture can be performed with a fine needle and a syringe by a trained caregiver; urine aspiration can relieve the situation sufficiently until the patient reaches the nearest Accident and Emergency.
What is new in this article?
The strength of this report is the description of the preventing measures and the techniques to overcome catheterization problems in spinal cord injury patients. Table 2 summarizes what this article adds to the literature.
Table 2.
What is new in this article?
| This article | What is available in literature |
|---|---|
| Autonomic dysreflexia due to bladder over-distension caused by failure to perform intermittent catheterization by a carer | No such case has been reported. Autonomic dysreflexia caused by blocked indwelling Foley catheter has been described but not due to failure to perform intermittent catheterization. |
| Death as a result of delay in performing intermittent catheterization by carer | No such case has been reported. |
| Specific treatment plan for managing clinical situation in community (e.g., patient’s home), when a caregiver is unable to insert catheter per urethra for routine intermittent catheterization | Managing failed urethral catheterization in able body individuals in a hospital set-up is available. What to do in case of a spinal cord injury patient in patient’s home, when a caregiver is unable to insert a catheter for intermittent catheterization, is new in this publication. This is the strength of this article. |
| Take-home message of this article: When carers are trained to perform intermittent catheterization, they should be given a care-plan to manage the situation when they are unable to perform intermittent catheterization. | There appears to be a vacuum in the literature on this particular aspect of care given to spinal cord injury patients. |
| This article explicitly states that in addition to recognizing symptoms of autonomic dysreflexia and treating high blood pressure promptly, removal of noxious stimuli which trigger autonomic dysreflexia is vital to prevent persistence of dysreflexia. | Although such message is available in a few scholarly publications, probably it is worth repeating, as health professionals appear to lay emphasis on treatment rather than prevention of autonomic dysreflexia. |
Learning points
Over-distension of urinary bladder should be avoided in high spinal cord injury patients to prevent autonomic dysreflexia; if it does occur, bladder should be drained promptly. Patients, who manage neuropathic bladder by intermittent catheterization, should have a care plan explicitly describing what should be done when carer is not able to insert a catheter per urethra.
Preventive measures rather than episodic treatment of autonomic dysreflexia should be the guiding principle of managing high spinal cord injury patients.
Acknowledgments
The authors are grateful to Mr BM Soni, Clinical Director, and Ms Emily Hoban, Directorate Manager, of Regional Spinal Injuries Centre, for their valuable help in the payment of the article processing fee for this manuscript.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Lindan R, Joiner E, Freehafer AA, Hazel C. Incidence and clinical features of autonomic dysreflexia in patients with spinal cord injury. Paraplegia. 1980;18(5):285–92. doi: 10.1038/sc.1980.51. [DOI] [PubMed] [Google Scholar]
- 2.Stephenson RO, Berliner J. Autonomic Dysreflexia in Spinal Cord Injury. [Accessed April 18, 2017]. Available from: http://emedicine.medscape.com/article/322809-overview.
- 3.Pan SL, Wang YH, Lin HL, Chang CW, Wu TY, Hsieh ET. Intracerebral haemorrhage secondary to autonomic dysreflexia in a young person with incomplete C8 tetraplegia: a case report. Arch Phys Med Rehabil. 2005;86(3):591–593. doi: 10.1016/j.apmr.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 4.Wan D, Krassioukov AV. Life-threatening outcomes associated with autonomic dysreflexia: a clinical review. J Spinal Cord Med. 2014;37(1):2–10. doi: 10.1179/2045772313Y.0000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoo KY, Jeong CW, Kim WM, et al. Fatal cerebral hemorrhage associated with autonomic hyperreflexia during surgery in the prone position in a quadriplegic patient: a case report. Minerva Anestesiol. 2010;76(7):554–558. [PubMed] [Google Scholar]
- 6.Gunduz H1, Binak DF. Autonomic dysreflexia: an important cardiovascular complication in spinal cord injury patients. Cardiol J. 2012;19(2):215–219. doi: 10.5603/cj.2012.0040. [DOI] [PubMed] [Google Scholar]
- 7.Villanueva C, Hemstreet GP., 3rd Difficult male urethral catheterization: a review of different approaches. Int Braz J Urol. 2008;34(4):401–411. doi: 10.1590/s1677-55382008000400002. discussion 412. [DOI] [PubMed] [Google Scholar]
- 8.Cancio LC, Sabanegh ES, Jr, Thompson IM. Managing the Foley catheter. Am Fam Physician. 1993;48(5):829–836. [PubMed] [Google Scholar]
- 9.Huang YH, Chen SL, Tsai SJ, Bih LI, Lew HL. Urodynamic responses to anal stretch in patients with detrusor sphincter dyssynergia. Arch Phys Med Rehabil. 2008;89(9):1748–1752. doi: 10.1016/j.apmr.2007.12.051. [DOI] [PubMed] [Google Scholar]
- 10.Wu YC, Nanninga JB, Hamilton BB. Inhibition of the external urethral sphincter and sacral reflex by anal stretch in spinal cord injured patients. Arch Phys Med Rehabil. 1986;67(2):135–136. doi: 10.1016/0003-9993(86)90129-2. [DOI] [PubMed] [Google Scholar]


