Summary
In a cohort of South African HIV-infected women initiating antiretroviral therapy in pregnancy with frequent viral load monitoring, 70% maintained viral suppression while 22% experienced at least 1 viremic episode >1000 copies/mL through 12 months postpartum.
Keywords: HIV, viral load, antiretroviral therapy, pregnancy, postpartum
Abstract
Background.
The numbers of human immunodeficiency virus (HIV)–infected women initiating antiretroviral therapy (ART) in pregnancy are increasing rapidly with global policy changes. There are widespread concerns about ART adherence during pregnancy and postpartum but few data on viral suppression (VS) over time in these populations.
Methods.
We followed a cohort of 523 women in Cape Town, South Africa, initiating ART in pregnancy (once-daily tenofovir 300 mg, emtricitabine 200 mg, and efavirenz 600 mg) and achieving VS (<50 copies/mL). Participants provided specimens through 12 months postpartum for batched viral load (VL) testing separate from routine care. Analyses described the incidence of major (>1000 copies/mL) and minor (50–1000 copies/mL) viremic episodes (VEs) and factors associated with major VEs.
Results.
In the cohort (median age, 28 years; median pre-ART VL, 3.99 copies/mL; 3% previously defaulted ART; 24% with previous exposure to short-course antiretrovirals), the median time of follow-up from VS was 322 days. Overall, 70% maintained VS throughout follow-up, 8% experienced minor VEs only, and at least 1 major VE was documented in 22% of women. In women with VEs, peak viremia (median, 3.79 log10 copies/mL) was linearly related to pre-ART VL. The incidence of major VEs after initial VS was independently associated with younger age, ART initiation during the third trimester, previous defaulting on ART, and postpartum follow-up.
Conclusions.
Viremia appears to occur frequently, particularly postpartum, among HIV-infected women after initial VS in this setting. More intensive VL monitoring is warranted in this population; the immediate causes and long-term implications of VE require investigation.
The past 5 years have witnessed major policy shifts in eligibility for antiretroviral therapy (ART) for prevention of mother-to-child human immunodeficiency virus (HIV) transmission (PMTCT) in low- and middle-income countries. In settings adopting the World Health Organization’s (WHO) “Option B+” strategy, calling for universal initiation of lifelong ART in all pregnant and postpartum women regardless of CD4 cell count or HIV disease stage, the numbers of HIV-infected women starting ART in pregnancy or postpartum have increased by ≥3-fold [1, 2]. In addition to their implications for PMTCT programs, experiences implementing Option B+ services are particularly important in light of new policy recommendations for universal ART initiation in all HIV-infected individuals [3].
However, there are notable concerns around ART adherence in pregnant and postpartum women [4]. Studies from routine care settings across Africa have demonstrated that retention of women on ART worsens in the postpartum period [5, 6]. This raises the possibility that disengagement from care and nonadherence could contribute to loss of viral control, with viremia undermining the benefits of ART in terms of both vertical transmission risk and long-term maternal health. Despite these issues, there are no data from low- and middle-income countries documenting viremia under policies of universal ART during pregnancy and the postpartum period. With viral load (VL) monitoring emerging as a standard of care for ART services, and pregnant and postpartum women identified as a priority population for VL monitoring, there is an urgent need to understand viral control in pregnant and postpartum women on ART in routine care [3, 7]. We examined patterns of viremia after initial suppression in women starting ART during pregnancy in routine health services in Cape Town, South Africa.
METHODS
Data were drawn from the Maternal & Child Health – Antiretroviral Therapy (MCH-ART) study, an implementation science study investigating optimal ART services for pregnant and postpartum women (ClinicalTrials.gov identifier NCT01933477). The design and methods have been described previously [8]. In brief, between April 2013 and May 2014, we recruited a cohort of 620 consecutive ART-eligible HIV-infected pregnant women at their first antenatal care (ANC) visit at a large public-sector primary care facility and followed participants up to 12 months postpartum. From April to June 2013, ART eligibility was determined by clinical and/or immunological status (based on WHO stage III/IV disease or CD4 count ≤350 cells/µL); from July 2013 to May 2014, all HIV-infected pregnant women were ART eligible regardless of CD4 cell count or disease status (Option B+) [9]. ART initiation and clinical follow-up took place as part of routine healthcare services, with all women initiating a once-daily, fixed-dose combination of tenofovir 300 mg, emtracitabine 300 mg, and efavirenz 600 mg.
In parallel, participants attended up to 9 study visits, organized separately from routine care, at regular intervals during pregnancy and postpartum. Cohort enrollment and the first study visit for all women was the day of the first ANC visit. In women making their first ANC visit at or before 30 weeks’ gestation, the next study visit was scheduled for 2 weeks after their first ANC visit, and then between 34 and 36 weeks’ gestation. For women making their first ANC visit from 31 to up to 35 weeks’ gestation, a second study visit was scheduled for between 34 and 36 weeks’ gestation. For women making their first study visit at or after 36 weeks’ gestation, there were no further antenatal study visits. Postpartum follow-up visits were carried out on a fixed schedule of 6 visits held at 7 days and 6 weeks postpartum, then every 3 months from 3 to 12 months postpartum. If participants were late or early to a scheduled study visit, we allowed visit windows up to the midpoint of the interval to the preceding or following visit, as appropriate.
At study visits, participants completed brief questionnaires collecting demographic and clinical information (including age and obstetric and medical history including previous antiretroviral exposure), and additional clinical data were abstracted from routine clinic records. Separate from VL monitoring conducted as part of routine care [10], at each study visit participants provided 5 mL of venous blood for de-identified batched testing using the Abbott RealTime HIV-1 assay (Abbott Laboratories, Chicago, Illinois) conducted by the South African National Health Laboratory Service. De-identification took place through use of a participant identification number generated separately from patient clinical folder numbers or other unique identifiers, with an access-controlled identification log used to link participant data during analysis. All women provided written consent prior to enrollment, with approval from the research ethics committees of the University of Cape Town and Columbia University.
Analyses were conducted using Stata software version 13.0 (StataCorp, College Station, Texas) or R version 3.2 (R Core Team, Vienna, Austria). All analyses were restricted to women with documented viral suppression (VS; defined as <50 copies/mL) during follow-up. After initial suppression, we categorized each subsequent VL measure as suppressed or elevated to minor (50–1000 copies/mL) or major (>1000 copies/mL) viremic episodes, following the guidelines used for clinical decision making in South African [10], US [11], and WHO [3] policy, and based on the observation that mother-to-child transmission risk appears to be substantially lower in patients with viral loads <1000 copies/mL [12, 13]. Sensitivity analyses modeled a binary definition of viremic episodes based on >50 copies/mL and then >400 copies/mL.
The incidence of viremic episodes was estimated per 100 woman-months on ART. Product-limit methods were used to estimate the cumulative proportion of women experiencing viremia over time. Mixed-effects Poisson models compared incidence rates in subgroups of participants; results are expressed as incidence rate ratios (IRRs) with 95% confidence intervals (CIs).
RESULTS
In 620 women initiating ART during pregnancy, 523 (84%) had viral load data available following initial VS during follow-up and are included in this analysis. The main reasons for exclusion were failure to achieve VS during the observation period (n = 85, including 11 individuals on whom observation stopped due to death or pregnancy loss, 18 women lost to follow-up during the study, and 56 women on whom observation was censored immediately after delivery by design), or no viremia detected pre-ART due to suspected ART use prior to enrollment (n = 12).
Among 523 women achieving viral suppression, the median age in the cohort was 28 years; the median gestation at ART initiation was 21 weeks; 24% of the cohort had previous exposure to short-course antiretrovirals for PMTCT whereas 3% had defaulted ART and were restarting therapy; the median pre-ART CD4 cell count was 345 cells/µL and the median pre-ART VL was 3.99 copies/mL (Table 1). After initial VS, a total of 5092 woman-months of observation were accrued in the cohort (median time of follow-up from VS, 322 days [interquartile range, 141–410 days]); 86% of observations took place postpartum (4385 vs 707 woman-months antepartum). A total of 2636 VL tests were conducted in this period (median number per woman, 5).
Table 1.
Description of Women Included in the Analysis Initiating Tenofovir, Emtricitabine, and Efavirenz During Pregnancy and Achieving Viral Suppression—Cape Town, South Africa
| Characteristic | No. (%) |
|---|---|
| No. | 523 (100) |
| Age, y, median (IQR) | 28 (24–32) |
| Parity: nulliparous | 100 (19) |
| Gestation at ART initiation, wk | |
| Median | 21 |
| ≤14 | 82 (16) |
| >14–28 | 330 (63) |
| >28 | 111 (21) |
| Previous antiretroviral exposure | |
| None | 374 (72) |
| NVP only | 6 (1) |
| ZDV + NVP | 121 (23) |
| Triple-drug therapy | 18 (3) |
| Pre-ART CD4 count, cells/µL | |
| Median | 345 |
| <200 | 83 (16) |
| 200–350 | 177 (34) |
| 350–500 | 116 (22) |
| >500 | 147 (28) |
| Pre-ART VL, log10 copies/mL | |
| Median | 3.99 |
| <3.0 | 72 (14) |
| 3.0–4.0 | 194 (37) |
| 4.0–5.0 | 206 (39) |
| >5.0 | 51 (10) |
| Time from ART initiation to VL suppression, d, median (IQR) | 91 (28–130) |
| Time of follow-up from suppression, d, median (IQR) | 322 (141–410) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: ART, antiretroviral therapy; IQR, interquartile range; NVP, nevirapine; VL, viral load; ZDV, zidovudine.
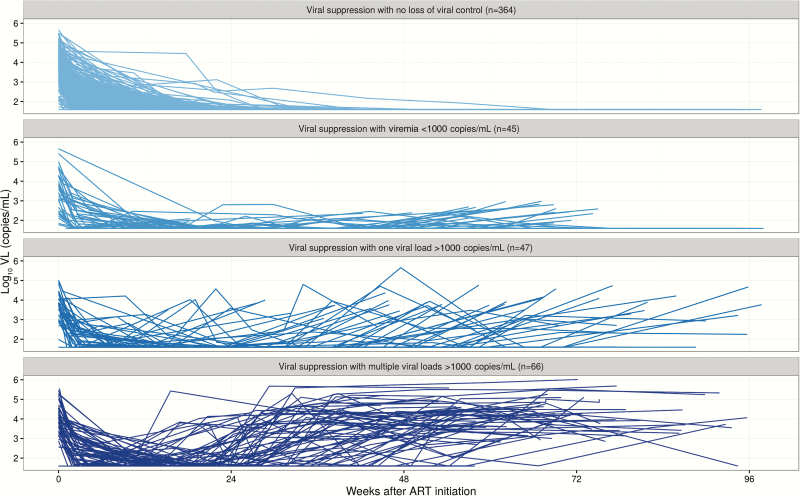
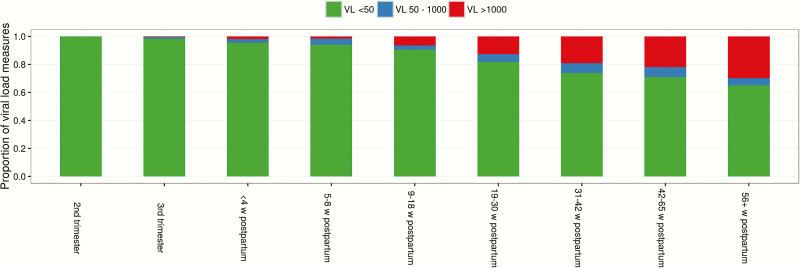
Figure 1 shows the patterns of virologic responses after ART initiation. Overall, 70% of the cohort (n = 364/523) sustained VS throughout the follow-up period, whereas an additional 8% (n = 45/523) experienced minor viremic episodes only. At least 1 major viremic episode was documented in 22% of women, and the majority of these episodes (58%) involved >1 VL measure >1000 copies/mL. Figure 2 shows the distribution of VL results by timing before and after delivery. The proportion of elevated VL measures increased steadily with increasing time after initial VS; cumulatively, by 1 year postpartum, 37% of women in the cohort had experienced at least 1 viremic episode >1000 copies/mL. In women with any viremia postsuppression, peak viremia (median, 3.79 log10 copies/mL) was linearly related to pre-ART VL (P < .001).
Figure 1.
Results of sequential viral load (VL) testing in a cohort of 523 women initiating antiretroviral therapy (ART) during pregnancy and achieving viral suppression in Cape Town, South Africa. Plots are of VL trajectories for individual patients from the time of ART initiation, divided by category of VL response; each participant is shown in only 1 plot based on observed VL response.
Figure 2.
Distribution of viral load (VL) test results during select intervals of time during pregnancy and postpartum; each column shows results for all tests conducted in the cohort during that interval.
During follow-up, 117 major and 56 minor episodes of viremia were observed after initial VS (incidence, 2.3 and 1.1 per 100 woman-months, respectively); incidence did not vary by calendar time of PMTCT policy. In a mixed-effects model adjusted for pre-treatment VL and duration of ART use (Table 2), the incidence of major viremic episodes after initial VS was independently associated with younger age (IRR for 18–22 years of age vs ≥34 years of age, 3.67 [95% CI, 1.78–7.56]), ART initiation during the third trimester (IRR vs first trimester, 2.21 [95% CI, 1.13–4.34]), previous defaulting on ART (IRR, 2.94 [95% CI, 1.29–6.69]), and postpartum follow-up (IRR vs antenatal follow-up, 6.41 [95% CI, 1.54–26.69]). In addition, in a model adjusted for all the covariates shown in Table 2 but restricted to person-time during the postpartum period, each additional month postpartum was associated with an 11% increase in the incidence of viremia (IRR, 1.11 [95% CI, 1.07–1.15]). In sensitivity with viremic episodes defined as either >50 copies/mL or >400 copies/mL, the results did not differ appreciably (Supplementary Table 1).
Table 2.
Results of Mixed-Effects Log-Linear Modeling of the Relative Incidence of Raised Viral Load (>1000 Copies/mL)
| Variable | A | B | ||||
|---|---|---|---|---|---|---|
| IRR | (95% CI) | P Value | IRR | (95% CI) | P Value | |
| Age, y | ||||||
| 18–22 | 3.23 | (1.57–6.63) | .001 | 3.67 | (1.78–7.56) | <.001 |
| 23–25 | 2.48 | (1.20–5.11) | .014 | 2.66 | (1.31–5.41) | .007 |
| 26–29 | 1.91 | (.97–3.77) | .061 | 2.18 | (1.12–4.24) | .021 |
| 30–33 | 1.61 | (.79–3.28) | .192 | 1.58 | (.78–3.20) | .207 |
| ≥34 | 1.0 | (reference) | 1.0 | (reference) | ||
| Gestation at ART initiation, wk | ||||||
| ≤14 | 1.0 | (reference) | 1.0 | (reference) | ||
| >14–28 | 1.48 | (.80–2.76) | .212 | 1.35 | (.72–2.52) | .346 |
| >28 | 2.51 | (1.29–4.91) | .007 | 2.21 | (1.13–4.34) | .021 |
| Previous ART | ||||||
| None | 1.0 | (reference) | 1.0 | (reference) | ||
| ZDV ± NVP (short course) | 1.23 | (.79–1.89) | .359 | 1.50 | (.96–2.34) | .073 |
| Triple-drug therapy | 2.97 | (1.30–6.81) | .010 | 2.94 | (1.29–6.69) | .010 |
| Pre-ART CD4 count, cells/µL | ||||||
| <200 | 1.0 | (reference) | 1.0 | (reference) | ||
| 200–350 | 0.72 | (.42–1.24) | .239 | 0.90 | (.51–1.59) | .791 |
| 350–500 | 0.80 | (.45–1.42) | .448 | 0.88 | (.48–1.60) | .673 |
| >500 | 0.50 | (.27–0.91) | .023 | 0.63 | (.33–1.20) | .156 |
| Pre-ART VL, copies/mL | ||||||
| <3.0 log10 | 1.0 | (reference) | 1.0 | (reference) | ||
| 3.0–4.0 log10 | 2.01 | (.97–4.14) | .060 | 1.84 | (.91–3.69) | .085 |
| 4.0–5.0 log10 | 2.00 | (.96–1.15) | .062 | 1.44 | (.69–3.00) | .333 |
| >5.0 log10 | 4.00 | (1.64–9.79) | .002 | 2.66 | (1.09–6.45) | .031 |
| Time from VL suppression to VL measurement, mo | 1.13 | (1.09–1.17) | <.001 | 1.11 | (1.07–1.15) | <.001 |
| Follow-up | ||||||
| Antenatal period | 1.0 | (reference) | 1.0 | (reference) | ||
| Postpartum period | 7.83 | (1.89–32.51) | .005 | 6.41 | (1.54–26.69) | .011 |
“A” shows crude associations involving single variables adjusted only for time after initial viral suppression; “B” shows a single model including all covariates shown.
Abbreviations: ART, antiretroviral therapy; CI, confidence interval; IRR, incidence rate ratio; NVP, nevirapine; VL, viral load; ZDV, zidovudine.
DISCUSSION
These are among the first data documenting the frequent loss of viral control after ART initiation and viral suppression in public-sector Option B+ PMTCT programs in Africa. The key findings are that up to one-third of women who achieve initial viral suppression experience viremia within 1 year postpartum, and that most of these women experience VL >1000 copies/mL, often with repeated episodes over time.
These findings should be generalized with caution. The results are from a single urban setting of South Africa, and while the participants are patients receiving routine public-sector healthcare, the frequency of viremic episodes may differ across programs and countries. Yet the high incidence of viremia on ART in routine care documented here is of clear concern and has significant implications for the population-level impact of policies for universal ART. The levels of sustained VS up to 12 months postpartum (70%) are substantially less than global targets of 90% [3]. In turn, it is clear that the benefits of universal ART initiation for pregnant women, including reduced risk of vertical and horizontal transmission as well as long-term optimization of maternal health, may be jeopardized at a population level.
There are at least 2 broad explanations for the viremia after initial viral suppression demonstrated here. The association between incident viremia and younger age—found previously in studies of nonretention under Option B+ services—may point to short-term, behavioral drivers [14]. In addition, the findings for increased frequency of viremia in the postpartum period is consistent with the hypothesis that women’s motivations for ART adherence in the antenatal period may be linked more directly to PMTCT, but motivations may wane with time postpartum. We also found that previous defaulting of triple-drug ART prior to restarting in pregnancy appears associated with increased rate of viremic episodes, which may suggest underlying antiretroviral resistance in this population or, alternatively, established behavioral patterns of nonadherence. While we did not have measures of adherence or resistance in this analysis, the etiology of viremia during pregnancy and postpartum needs careful elucidation to inform the most appropriate strategies for both investigation and management.
Interestingly, the levels of viremia documented here are broadly similar to those found in routine care cohorts in Europe and North America. For example, in an analysis of women initiating ART during pregnancy in England and Ireland who were virally suppressed at delivery, 35% had evidence of viral rebound (>200 copies/mL) up to 6 months postpartum [15]. Similarly, in a cohort of women in the United States, 56% of women who were suppressed at delivery had VL >1000 copies/mL at 12 months postpartum [16]. The parallels across countries in findings for high levels of viremia in HIV-infected women during the postpartum period despite access to ART are striking, and may point to cross-cutting psychological, social, and/or behavioral drivers of ART nonadherence during this phase of women’s lives; understanding why levels of viremia on ART appear so consistent across settings in this patient population remains a critical question for optimizing HIV treatment programs globally.
These data raise important questions regarding postnatal transmission through breastfeeding. Previously we described early mother-to-child transmission that appeared to be heavily influenced by maternal viremia at delivery [17]. Although we do not have data available on transmission in breastfed infants after 12 weeks of age, the dose-response association between maternal VL and vertical transmission risk suggests that there may be increased transmission to infants of viremic women breastfed for longer periods [18–20]. In light of recent recommendations that all HIV-infected women on ART breastfeed for at least 12 and up to 24 months [21], these data highlight the importance of effective detection and management of postpartum viremia to reduce the incidence of HIV in infants.
With VL emerging as the standard of care for ART monitoring in low- and middle-income countries, these data have important implications for monitoring in pregnant and postpartum women. The high incidence of viremia >1000 copies/mL in this population points to the likely yield of VL monitoring in these populations, while programs that conduct VL monitoring in pregnant and postpartum women only annually—as is widely promulgated for adults outside of the context of pregnancy [7, 22]—are likely to delay detection of elevated VL. Based on these data, VL monitoring at regular intervals during the first year postpartum (ie, at 6 and/or 12 months postpartum) may be likely to have a substantial yield. However, precisely when and how frequently monitoring should take place requires research attention in terms of both optimal clinical outcomes and the cost-effectiveness of different monitoring schemes [23]. And whereas earlier and/or more frequent VL testing for pregnant and postpartum women may be required to detect loss of viral control as early as possible, effective interventions to prevent and manage viremia are required [24].
In summary, these novel data show that viremic episodes following initial viral suppression occur frequently in women initiating ART during pregnancy under Option B+ policies. Based on this finding, there is an urgent need to understand better the causes of viremia as well as the optimal VL monitoring and intervention strategies for pregnant and postpartum women to maximize the benefits of universal ART policies toward maternal and child health.
Supplementary Material
Notes
Financial support. This work was supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant number 1R01HD074558).
Potential conflicts of interest. Authors certify no potential conflicts of interest. The authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Disease Control and Prevention. Impact of an innovative approach to prevent mother-to-child transmission of HIV—Malawi, July 2011–September 2012. MMWR Morb Mortal Wkly Rep 2013; 62:148–51. [PMC free article] [PubMed] [Google Scholar]
- 2. Myer L, Phillips T, Manuelli V, McIntyre J, Bekker LG, Abrams EJ. Evolution of antiretroviral therapy services for HIV-infected pregnant women in Cape Town, South Africa. J Acquir Immune Defic Syndr 2015; 69:57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization. WHO consolidated guidelines on the use of antiretrovirals for treating and preventing HIV infection. 2nd ed Geneva, Switzerland: WHO, 2016. [Google Scholar]
- 4. Nachega JB, Uthman OA, Anderson J, et al. Adherence to antiretroviral therapy during and after pregnancy in low-income, middle-income, and high-income countries: a systematic review and meta-analysis. AIDS 2012; 26:2039–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Phillips T, Thebus E, Bekker LG, Mcintyre J, Abrams EJ, Myer L. Disengagement of HIV-positive pregnant and postpartum women from antiretroviral therapy services: a cohort study. J Int AIDS Soc 2014; 17:19242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haas AD, Tenthani L, Msukwa MT, et al. Retention in care during the first 3 years of antiretroviral therapy for women in Malawi’s option B+ programme: an observational cohort study. Lancet HIV 2016; 3:e175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Working Group on Modelling of Antiretroviral Therapy Monitoring Strategies in Sub-Saharan Africa. Sustainable HIV treatment in Africa through viral-load-informed differentiated care. Nature 2015; 528:S68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Myer L, Phillips TK, Zerbe A, et al. Optimizing antiretroviral therapy (ART) for maternal and child health (MCH): rationale and design of the MCH-ART study. J Acquir Immune Defic Syndr 2016; 72:S189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. Geneva, Switzerland: WHO; 2013. [PubMed] [Google Scholar]
- 10. South African National Department of Health (NDOH). National consolidated guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in children, adolescents and adults. Pretoria, South Africa: NDOH, 2015. [Google Scholar]
- 11. Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for use of antiretroviral drugs in pregnant HIV-1- infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. Available at: http://aidsinfo.nih.gov/contentfiles/lvguidelines/PerinatalGL.pdf Accessed 1 December 2016.
- 12. Garcia PM, Kalish LA, Pitt J, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. N Engl J Med 1999; 341:394–402. [DOI] [PubMed] [Google Scholar]
- 13. Davis NL, Miller WC, Hudgens MG, et al. Maternal and breast milk viral load: impacts of adherence on peri-partum HIV infections averted—the BAN study [manuscript published online ahead of print 1 August 2016]. J Acquir Immune Defic Syndr 2016. doi: 10.1097/QAI.0000000000001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hodgson I, Plummer ML, Konopka SN, et al. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS One 2014; 9:e111421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Huntington S, Thorne C, Newell ML, et al. ; UK Collaborative HIV Cohort (UK CHIC) Study and the UK and Ireland National Study of HIV in Pregnancy and Childhood (NSHPC) The risk of viral rebound in the year after delivery in women remaining on antiretroviral therapy. AIDS 2015; 29:2269–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adams JW, Brady KA, Michael YL, Yehia BR, Momplaisir FM. Postpartum engagement in HIV care: an important predictor of long-term retention in care and viral suppression. Clin Infect Dis 2015; 61:1880–7. [DOI] [PubMed] [Google Scholar]
- 17. Myer L, Phillips TK, McIntyre JA, et al. HIV viraemia and mother-to-child transmission risk after antiretroviral therapy initiation in pregnancy in Cape Town, South Africa [manuscript published online ahead of print 28 June 2016]. HIV Med 2016. doi: 10.1111/hiv.12397. [DOI] [PubMed] [Google Scholar]
- 18. Mwapasa V, Rogerson SJ, Kwiek JJ, et al. Maternal syphilis infection is associated with increased risk of mother-to-child transmission of HIV in Malawi. AIDS 2006; 20:1869–77. [DOI] [PubMed] [Google Scholar]
- 19. Jamieson DJ, Sibailly TS, Sadek R, et al. HIV-1 viral load and other risk factors for mother-to-child transmission of HIV-1 in a breast-feeding population in Cote d’Ivoire. J Acquir Immune Defic Syndr 2003; 34:430–6. [DOI] [PubMed] [Google Scholar]
- 20. Chasela C, Chen YQ, Fiscus S, et al. Risk factors for late postnatal transmission of human immunodeficiency virus type 1 in sub-Saharan Africa. Pediatr Infect Dis J 2008; 27:251–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization. Guideline: updates on HIV and infant feeding. Geneva, Switzerland: WHO, 2016. [PubMed] [Google Scholar]
- 22. Centers for Disease Control and Prevention. Scale-up of HIV viral load monitoring—seven sub-Saharan African countries. MMWR Morb Mortal Wkly Rep 2013; 64:1287–90. [DOI] [PubMed] [Google Scholar]
- 23. Ouattara EN, Robine M, Eholié SP, et al. Laboratory monitoring of antiretroviral therapy for HIV infection: cost-effectiveness and budget impact of current and novel strategies. Clin Infect Dis 2016; 62:1454–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roberts T, Cohn J, Bonner K, Hargreaves S. Scale-up of routine viral load testing in resource-poor settings: current and future implementation challenges. Clin Infect Dis 2016; 62:1043–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.