Abstract
Transoral laser microsurgery applies to the piecemeal removal of malignant tumours of the upper aerodigestive tract using the CO2 laser under the operating microscope. This method of surgery is being increasingly popularised as a single modality treatment of choice in early laryngeal cancers (T1 and T2) and occasionally in the more advanced forms of the disease (T3 and T4), predominantly within the supraglottis.
Thomas Kuhn, the American physicist turned philosopher and historian of science, coined the phrase ‘paradigm shift’ in his groundbreaking book The Structure of Scientific Revolutions. He argued that the arrival of the new and often incompatible idea forms the core of a new paradigm, the birth of an entirely new way of thinking. This article discusses whether Steiner and colleagues truly brought about a paradigm shift in oncological surgery.
By rejecting the principle of en block resection and by replacing it with the belief that not only is it oncologically safe to cut through the substance of the tumour but in doing so one can actually achieve better results, Steiner was able to truly revolutionise the management of laryngeal cancer. Even though within this article the repercussions of his insight are limited to the upper aerodigestive tract oncological surgery, his willingness to question other peoples’ dogma makes his contribution truly a genuine paradigm shift.
Keywords: Head and neck, Oncology, Paradigm
Introduction
Transoral laser microsurgery (TLM) applies to the piecemeal removal of malignant tumours of the upper aero-digestive tract using the CO2 laser under the operating microscope. This method of surgery is being increasingly popularised as a single modality treatment of choice in early laryngeal cancers (T1 and T2) and occasionally in the more advanced forms of the disease (T3 and T4), predominantly within the supraglottis. In addition, there is growing evidence of its efficacy in treating carcinomas arising from other anatomical subsites such as the pharynx and oral cavity, either as single modality in early disease or in combination with radiotherapy in more advanced disease.1–9
In early glottic carcinoma, TLM offers a credible alternative to radiotherapy, which was the mainstay of treatment, and achieves comparable local recurrence rates with acceptable functional results.4,5 The path of progress of this new approach has not been without contention and remains controversial in some quarters. In fact, the technique was strongly resisted, even derided at the beginning. Traditional laser micro-laryngoscopy had already been accepted by the time TLM appeared and it was not the usual worries about the introduction of new techniques or technology that were of concern but more the particular way in which these established tools were being used to perform the resection. The TLM approach stipulates violating the integrity of the cancerous growth by cutting directly through it, thus raising concerns that cancer cells would be seeded or spread to other parts of the body. We believe that the discarding of such myths and the associated dramatic change in attitude of what constitutes a safe oncological resection may represent a paradigm shift in oncological surgery.
What is a paradigm and how can it be shifted?
The traditional conception of scientific advancement is one of slow, gradual and incremental progression. People often think that new knowledge and ideas are gathered together piecemeal, much like building bricks to erect the edifice of modern understanding. Thomas Kuhn, the American physicist turned philosopher and historian of science, realised and subsequently outlined in his groundbreaking book, The Structure of Scientific Revolutions, that this only applies to what he described as ‘normal science’. Kuhn perceived normal science as a stepwise progression in knowledge and understanding.10 During periods of normal science, Kuhn argued, the task of the scientist is to work within the confines of the prevailing core idea to a point of disregarding results which could threaten it.10 In essence, the aim of research including thought and instrumentation is directed towards achieving a perceived goal, which must always be consistent with the core idea.10 Occasionally, however, major breakthroughs in understanding can occur not through the usual stepwise accumulation of ideas but by the outright rejection of the core idea itself and its replacement with a new one. The arrival of the new and often incompatible idea forms the core of a new paradigm, the birth of an entirely new way of thinking.11 Such a change represents nothing less than a scientific revolution and, quite understandably, is usually met with strong resistance from the scientific community and is not easily adopted. An example of such a paradigm shift would be Copernicus’s conception of the heliocentric model with a motionless Sun being orbited by planets, in contrast to the Ptolemaic viewpoint prevalent at the time, which placed a stationary Earth at the centre of the Universe. Kuhn referred to some of the great paradigm shifts in astronomy, physics and biology – those we associate with the scientific revolutions of Copernicus, Newton or Darwin – as ‘one conceptual world view being replaced by another’.
What was the prevailing core idea in cancer surgery?
It is generally agreed that when it comes to cancer surgery it is imperative that the tumour be resected en bloc and that cutting into the substance of the tumour should be avoided at all costs. This basic oncological rule arguably constitutes the core idea that underpins the whole of surgical oncology, although its origins are difficult to trace. In the modern era, one of the famous fathers of surgery, William Stewart Halstead, developed the radical mastectomy for breast cancer.12 In the late 19th century, Halstead noticed that women who had undergone lumpectomies only suffered more recurrences of the disease. Halstead’s ideas stemmed from W Sampson Handley, a surgeon working in London, who believed that cancer invaded outwards from a central core. The principle of encompassing a large cuff of normal tissue while the cancer was retained intact within it was adopted, a belief that is still held strongly to this very day. En-bloc resection of cancers is regarded as oncologically safe and represents the gold standard, as it is thought to prevent local recurrence, tumour seeding and spread.
Transoral laser surgery (Steiner technique)
Horace Green, in 1852, was the first reported surgeon to remove a lesion in the laryngeal ventricle transorally.13 In 1915, Lynch described the resection of nine laryngeal lesions through an endoscopic technique.14 It was not until the introduction of the operating microscope that endoscopic laryngeal techniques became popularised. In the 1970s, Strong and Jako used the CO2 laser in endoscopic laryngeal resection.15,16 These lesions may have been cancerous but as long as the basic oncological principle that they should always be removed en-bloc was adhered to, the endoscopic approach was deemed an acceptable clinical practice. The possibility of piecemeal resection was not even considered as an option at the time because it was contrary to the core oncological principle that the substance of the tumour should never be breeched. TLM, which breaks this rule, only gained acceptance following a landmark paper published by Wolfgang Steiner.4 The study was conducted between 1979 and 1985 and included 240 patients with laryngeal cancer without prior treatment and managed with curative intent. Patients with glottic cancers (Tis, T1 and T2 lesions), were all treated with transoral endoscopic laser resection. There were six local recurrences, with one patient needing total laryngectomy. Adjusted five-year survival rates were 100%.
The goals of oncological surgery are the same for both conventional en-block resection and for TLM: complete tumour excision with sufficiently clear resection margins and the accurate histological assessment of these margins. The methods of reaching these goals, however, differ dramatically between the two methods. TLM cuts through the tumour under the microscope, a bespoke approach, rather than excising a large block of normal tissue (i.e. the vocal cord) with the tumour contained within. In TLM, cutting through tumour allows assessment of the depth of the tumour, thus tailoring the extent of the resection to the specific needs of the individual patient. This compares with en-bloc resection, where a large cuff of normal tissue is excised unnecessarily with the tumour contained within or a whole organ such as the larynx is sacrificed to remove the cancer within the organ (Fig 1).
Figure 1.
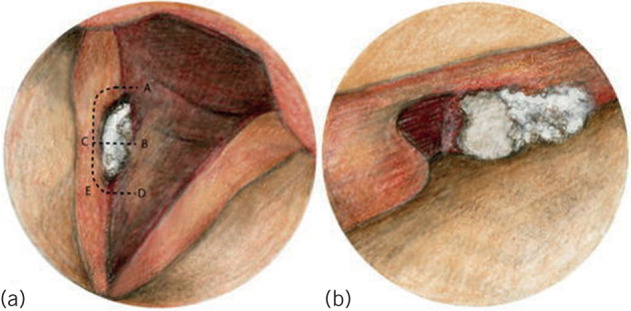
Depiction of a right vocal cord tumour: (a) tumour on the right vocal cord; (b) tumour after it has been split (through dotted line ‘B’) and the anterior portion has been excised. Rather than the traditional en-bloc resection, the tumour is split first (dotted line B, picture a). This allows for depth of tumour to be determined. Following the tumour split both sections are then excised under the microscope (source: Rubinstein M, Armstrong WB. Transoral laser microsurgery for laryngeal cancer: a primer and review of laser dosimetry. Lasers Med Sci 2011; 26: 113–124; reproduced with permission).
The technique of laser resection differs from the conventional en-bloc resection as the tumour is being breached, which is why TLM is thought to violate the principles of oncological surgery. Even though it breaks a basic rule of oncological surgery, Steiner’s technique offers many advantages as compared with the approach it replaced. By cutting through tumour until disease-free tissue is reached under microscopic guidance, the surgeon can properly assess the depth of invasion and can thereby achieve better deep-margin clearance than would otherwise have been possible through an en-block resection, even if access were not an issue. This is the core idea behind TLM. The piecemeal resection allows the removal of these tumours through the relatively narrow aperture of a rigid laryngoscope. If there are any areas of concern (such as margin status) while performing TLM, frozen section analysis may be performed.
In the words of Steiner, TLM is: ‘Oncologically radical, but less surgically radical’. The laser technique theoretically seals blood vessels and lymphatics, preventing the conventional concern about regional and distant spread. In the case of TLM, the surgeon and not the pathologist defines the margin status. The surgeon is operating through a microscope, giving a high-definition view of tumour and normal tissue, hence the surgeon deciphers the difference and can tailor the resection accordingly. Together with the visual aspect of differentiating between normal and cancerous tissue comes the ‘feel’ of the tissue and how it cuts with the laser. These factors interplay, allowing the surgeon to decide whether tumour clearance has been obtained. If the specimen margin status is positive on conventional histological techniques, a second-look procedure may show no residual tumour as the laser often vaporises the cut margin of tissue. The management choice is then to either rely on the surgeon’s experience or to use histological assessment of marginal biopsies. Other considerations are organ-specific factors; for example, tumours of the tongue are known to have finger-like submucosal extensions compared with the vocal cords, where this is not generally the case. Transoral laser resection of tumours of the larynx is possible because the desmoplastic stromal response is thought to equal the underlying invading tumour, thus generally preventing under- or over-resection. There is a paucity of lymphatics within Reinke’s space and hence T1 vocal fold tumours are thought to ‘never’ metastasise, allowing for limited resection within the larynx. Taking an extra centimetre of pharyngeal tissue will not have the same effects as taking more vocal cord tissue in a professional singer. The risk factors for these tumours are also taken into consideration; chronic alcohol and cigarette use is known to produce a field change, so larger areas of tissue are taken. The experience of the surgeon is also paramount in achieving a successful outcome.
The hallmark of malignancy is its ability to invade adjacent normal tissue. At the site of primary invasion many epithelial tumours induce a desmoplastic response of the host tissues.17 This stromal response is complex, involving fibroblasts, inflammatory cells, proliferating vascular structures, as well as normal parenchymal cells undergoing atrophy at the invasive edge. This response is particularly important when considering laser resection. Some tumours may outgrow the stromal response and may be found invading seemingly normal healthy tissue, making it difficult to obtain clear margins. The converse is also possible, with some tumours showing an intense desmoplastic stromal response, in which case a very large area of tissue needs to be excised containing relatively small tumour volume within it. This scenario poses particular challenges in endoscopic laser resection of laryngeal tumours as the preservation of tissue is one of its most important advantages.
At the time that Steiner was undertaking his work on transoral laser surgery, many other surgeons were performing open surgery in the form of partial laryngectomy. This type of surgery kept to the basic oncological principles, produced very low rates of locoregional recurrence and showed good five-year survival rates. However, entering the larynx through an external approach requires a laryngofissure combined with a tracheotomy. This means long recovery times, the need for nasogastric feeding, prolonged hospital stay and risks serious complications, such as poor wound healing and the development of a laryngocutaneous fistula. Such serious complications can be avoided by TLM, with the added benefits of a better functional outcome and greatly reduced hospital stay (most TLM procedures can be done as day cases).
In the following year. Steiner and colleagues published details of their work on hypopharyngeal cancer.6 This technique can be applied to virtually any area of the upper aerodigestive tract. Indeed, the authors of this article have applied TLM to the oral cavity and oropharynx.
Conclusion
Steiner’s contribution to the surgical management of laryngeal cancer is clearly significant but can we really describe it as a true paradigm shift? Is it not simply a modification, admittedly an important one, to an existing surgical technique, just like any of a myriad of others that pervade modern surgical practice? Can we really compare it to the great paradigm shifts in astronomy, physics and biology, examples of which we gave earlier? In response, we need to appreciate that it is not the technique itself that is under consideration here but the conceptual breakthrough. Steiner was prepared to reject a whole way of thinking, abandoning the previously cherished and seeming inviolable idea of what constitutes sound oncological surgery, coupled with his ability to replace it with a new one that was its exact opposite. His main insight was that by adhering to the principle of en-block resection, surgeons were limiting the role of laser surgery to a small minority of early laryngeal carcinomas and had to resort to either radical radiotherapy or radical open surgery to deal with the rest. By rejecting the principle of en-block resection and by replacing it with the belief that not only is it oncologically safe to cut through the substance of the tumour but in doing so one can actually achieve better results, Steiner was able to truly revolutionise the management of laryngeal cancer. Even though within this article the repercussions of his insight are limited to the upper aerodigestive tract oncological surgery, his willingness to question other peoples’ dogmas makes his contribution truly a genuine paradigm shift.
References
- 1.Sandulache VC, Kupferman ME. Transoral laser surgery for laryngeal cancer. Rambam Maimonides Med J 2014; (2): e0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canis M, Ihler F, Martin A et al. . Organ preservation in T4a laryngeal cancer: is transoral laser microsurgery an option? Eur Arch Otorhinolaryngol 2013; (10): 2,719–2,727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Takes RP, Strojan P, Silver CE et al. . Current trends in initial management of hypopharyngeal cancer: The declining use of open surgery. Head Neck 2012; (2): 270–281. [DOI] [PubMed] [Google Scholar]
- 4.Steiner W. Results of curative laser microsurgery of laryngeal carcinomas. Am J Otolaryngol 1993; (2): 116–121. [DOI] [PubMed] [Google Scholar]
- 5.Higgins KM, Shah MD, Ogaick MJ, Enepekides D. Treatment of early-stage glottic cancer: meta-analysis comparison of laser excision versus radiotherapy. J Otolaryngol Head Neck Surg 2009; (6): 603–612. [PubMed] [Google Scholar]
- 6.Steiner W. Therapy of hypopharyngeal carcinoma. Part V. Discussion of long-term results of trans-oral laser microsurgery of hypopharyngeal carcinoma. HNO 1994; : 116–121. [PubMed] [Google Scholar]
- 7.Grant DG, Salassa JR, Hinni ML et al. . Carcinoma of the tongue base treated by transoral laser microsurgery, part one: untreated tumors, a prospective analysis of oncologic and functional outcomes. Laryngoscope 2006; (12): 2,150–2,155. [DOI] [PubMed] [Google Scholar]
- 8.Werner J, Benedikt J. Transoral laser microsurgery in carcinomas of the oral cavity, pharynx, and larynx. Cancer Control 2002; (5): 379–386. [DOI] [PubMed] [Google Scholar]
- 9.Rigby MH, Taylor SM. Review of transoral laser microsurgery for cancer of the upper aerodigestive tract. J Otolaryngol Head Neck Surg 2011; (2): 113–121. [PubMed] [Google Scholar]
- 10.Kuhn T. The Structure of Scientific Revolutions. Chicago, IL: University of Chicago Press; 1962. [Google Scholar]
- 11.Bird A. Thomas Kuhn : Zalta EN, The Stanford Encyclopedia of Philosophy. Stanford, CA: Stanford University Metaphysics Research Lab; 2013. [Google Scholar]
- 12.Osborne MP. William Stewart Halsted: his life and contributions to surgery. Lancet Oncol 2007; (3): 256–265. [DOI] [PubMed] [Google Scholar]
- 13.Green H. Morbid growths within the larnx : On the Surgical Treatment of Polypi of the Larynx, and Oedema of the Glottis. New York, NY: Putnam; 1852, pp46–65. [Google Scholar]
- 14.Lynch R. Suspension laryngoscopy and its accomplishments. Ann Otol Rhinol Laryngol 1915; : 429–478. [Google Scholar]
- 15.Strong M, Jako G. Laser surgery in the larynx: early clinical experience with continuous CO2 laser. Ann Otol Rhinol Laryngol 1972; : 791–798. [DOI] [PubMed] [Google Scholar]
- 16.Strong M. Laser excision of carcinoma of the larynx. Laryngoscope 1975; : 1,286–1,289. [DOI] [PubMed] [Google Scholar]
- 17.Iacobuzio-Donahue CA, Argani P, Hempen PM et al. . The desmoplastic response to infiltrating breast carcinoma: gene expression at the site of primary invasion and implications for comparisons between tumor types. Cancer Res 2002; (18): 5,351–5,357. [PubMed] [Google Scholar]


