Abstract
Aims
Second opinions in pathology improve patient safety by reducing diagnostic errors, leading to more appropriate clinical treatment decisions. Little objective data are available regarding the factors triggering a request for second opinion despite second opinion consultations being part of the diagnostic system of pathology. Therefore we sought to assess breast biopsy cases and interpreting pathologists characteristics associated with second opinion requests.
Methods
Collected pathologist surveys and their interpretations of 60 test set cases were used to explore the relationships between case characteristics, pathologist characteristics and case perceptions, and requests for second opinions. Data were evaluated by logistic regression and generalised estimating equations.
Results
115 pathologists provided 6900 assessments; pathologists requested second opinions on 70% (4827/6900) of their assessments 36% (1731/4827) of these would not have been required by policy. All associations between case characteristics and requesting second opinions were statistically significant, including diagnostic category, breast density, biopsy type, and number of diagnoses noted per case. Exclusive of institutional policies, pathologists wanted second opinions most frequently for atypia (66%) and least frequently for invasive cancer (20%). Second opinion rates were higher when the pathologist had lower assessment confidence, in cases with higher perceived difficulty, and cases with borderline diagnoses.
Conclusions
Pathologists request second opinions for challenging cases, particularly those with atypia, high breast density, core needle biopsies, or many co-existing diagnoses. Further studies should evaluate whether the case characteristics identified in this study could be used as clinical criteria to prompt system-level strategies for mandating second opinions.
BACKGROUND
Second opinions in pathology improve patient safety by reducing diagnostic errors, leading to more appropriate clinical treatment decisions.1,2 Pathologists frequently request second opinions for pathological interpretations of breast specimens, particularly for new cancer diagnoses and when surgery is performed at referral hospitals.3–7 In a recent survey of US pathologists participating in the Breast Pathology Study (B-Path), 81% of respondents reported obtaining second opinions in their clinical practice on at least some breast pathology cases that did not require second opinions due to mandated institutional policies.8 The vast majority of surveyed pathologists also agreed that second opinions improve their diagnostic accuracy and protect them from malpractice suits. Few objective data are available regarding the factors triggering a request for second opinion despite second opinion consultations being part of the diagnostic system of pathology.9 Additional data from practicing pathologists may inform system-level future policy.
The purpose of this study was to determine whether specific characteristics of breast biopsy cases were associated with requesting second opinions, and how these associations varied by specific diagnoses. In addition, we explored the relationship between requesting a second opinion and pathologists’ perceptions of the case, including confidence in their assessment, whether they considered a case difficult, and whether they considered a case borderline between two diagnoses. Finally, we compared the association between these variables and whether the request for second opinion was based on institutional policy or desired for diagnostic reasons regardless of policy.
METHODS
This observational cross-sectional study is part of the larger B-Path Study,10–12 which was designed to evaluate diagnostic variation in the interpretation of breast biopsies among practicing pathologists. Two hundred and forty breast specimens were randomly selected from two state pathology registries (NH, VT) that are part of the National Cancer Institute sponsored Breast Cancer Surveillance Consortium.13 Selection was stratified by age (49% age 40–49 years, 51% age ≥50 years), breast density (51% with heterogeneously or extremely dense breast tissue based on mammography), and biopsy type (58% core needle, 42% excisional). The cases were divided into four test sets of 60 cases as described in a previous publication.10 Each case was represented by one glass slide, which was carefully checked for quality. Participants were instructed to assume that the single slide demonstrated the best diagnostic features of the case.
Participating pathologists
Pathologists from eight US states (Alaska, Maine, Minnesota, New Hampshire, New Mexico, Oregon, Vermont and Washington) were invited to participate. Details of their identification and recruitment have been described elsewhere.10,14 Participating pathologists completed a web-based survey followed by interpreting their assigned test set of 60 cases.
Physician survey
Pathologists self-reported demographic and clinical practice characteristics, including age, gender, expertise in breast pathology, professional and academic affiliations, fellowship training in surgical and breast pathology, number of years interpreting breast pathology, and proportion of caseload devoted to breast specimens.
Diagnostic histology data collection
Participants completed an online histology data collection form10 for each case, and were asked to interpret the cases using the same diagnostic criteria they would use in regular clinical practice. We categorised their interpretations on each case into one of four primary diagnostic categories (benign without atypia, atypia (atypical ductal hyperplasia (ADH) or ADH in a papilloma), ductal carcinoma in situ (DCIS), and invasive carcinoma) as detailed elsewhere.10 There were 14 unique possible diagnoses comprising the four primary diagnostic categories; we calculated the sum of total unique diagnoses used for each case to create a cumulative diagnosis value as a surrogate measure of case complexity. The histology form also asked pathologists if they considered the case borderline between two diagnoses. Pathologists rated their perceived levels of diagnostic challenge and their confidence in their diagnosis for each test case. A six-point Likert scale ranging from 1 (‘very easy’) to 6 (‘very challenging’) was provided for the question ‘Rate your opinion of the level of diagnostic difficulty of this case’, and a six-point Likert scale from 1 (‘very confident’) to 6 (‘not confident at all’) was used to rate confidence in their assessment. Likert responses were collapsed into binary outcomes: ‘low degree of challenge’ (Likert 1, 2, 3) versus ‘high degree of challenge’ (Likert 4, 5, 6); and ‘high confidence’ (Likert 1, 2, 3) versus ‘low confidence’ (Likert 4, 5, 6).
Finally, pathologists recorded whether they would have asked for a second pathologist’s opinion of the case before finalising the report if they were interpreting the case in clinical practice. They could choose from the following responses: (1) Yes, I would want a second pathologist’s opinion for diagnostic reasons; (2) Yes, because it is our policy to get a second opinion in cases with this diagnosis; (3) Yes, I would want a second pathologist’s opinion for diagnostic reasons and yes, because it is our policy to get a second opinion in cases with this diagnosis (ie, both response 1 and 2 were checked); and (4) No, I do not want a second opinion.
Case characteristics
The woman’s age at the time of biopsy and biopsy type were available to the pathologists for each case. The registry provided patient age, while biopsy type was determined by review of the original case slides and pathology report. Radiologists provided mammographic breast density according to the BIRADS mammographic density classifications. For analysis, we dichotomised mammographic density to high (very dense or heterogeneously dense) and low (scattered fibroglandular densities or almost entirely fat).
Statistical analysis
Frequencies and percentages for each of four response categories for second opinions were calculated. Associations between the dependent variable, request for second opinion, and pathologist and case characteristics (including diagnostic category) as single covariates were tested using repeated measures logistic regression with and without adjustment under PROC GENMOD in SAS software. To assess the impact these characteristics had on the dependent variable, responses to the request for a second opinion were dichotomised by grouping all three affirmative responses together as ‘Yes’ compared with ‘No, I do not want a second opinion’. Second opinion rates were calculated using a generalised estimating equation (GEE) with a binomial distribution and independent correlation structure, accounting for clustered responses within each participant. Estimates and SEs of least square (LS) means were computed and transformed back to the original response scale via the inverse-link function to provide rates of second opinion and their 95% CIs. An additional sensitivity analysis was conducted for the dichotomous outcome of requesting a second opinion after removing second opinion requests that were based on policy alone. Wald-based p values and 95% CIs were computed using a two-sided significance level of 0.05. Statistical analyses were performed using SAS software V.9.4 for the Windows Operating System (SAS Institute Inc, Cary, North Carolina, USA).
RESULTS
One hundred and fifteen pathologists completed the survey and each reviewed 60 breast biopsy cases that included more cases of ADH and DCIS than in clinical practice. Among the 6900 independent case assessments, pathologists reported that they would request a second opinion (either as required by policy and/or desired by the pathologist) for 70% (4827/6900). Of cases for which the pathologists requested a second opinion, just over one-third (36%; 1731/4827) would not have been required by laboratory policies in their clinical practices (table 1).
Table 1.
Demographic and clinical experience of pathologists by second opinion during the independent assessment of breast biopsy cases (N = 115 participants, 6900 independent assessments)
| Would you ask for a second pathologist’s opinion of this case before finalising the report? (Assume a pathologist is available) | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Combined yes responses rate (95% CI) |
Response options N (%) |
|||||||
|
|
|
|||||||
| Pathologist characteristics * |
Number of pathologists |
Number of independent assessments |
Rate of second opinion † |
p Value ‡ |
Yes, because I would want a second pathologist’s opinion for diagnostic reasons |
Yes, because it is our policy to get a second opinion in cases with this diagnosis |
Yes to both because I would want it and because it is our policy |
No, I do not want a second opinion |
| Total | 115 | 6900 | 70 (65 to 75) | − | 1731 (25) | 2376 (34) | 720 (10) | 2073 (30) |
| Demographics | ||||||||
| Age at survey (years) | ||||||||
| 33–39 | 16 | 960 | 77 (65 to 89) | 0.69 | 164 (17) | 381 (40) | 195 (20) | 220 (23) |
| 40–49 | 41 | 2460 | 68 (59 to 76) | 589 (24) | 916 (37) | 165 (7) | 790 (32) | |
| 50–59 | 42 | 2520 | 69 (61 to 77) | 775 (31) | 704 (28) | 260 (10) | 781 (31) | |
| 60+ | 16 | 960 | 71 (57 to 85) | 203 (21) | 375 (39) | 100 (10) | 282 (29) | |
| Gender | ||||||||
| Female | 46 | 2760 | 74 (67 to 81) | 0.19 | 812 (29) | 951 (34) | 273 (10) | 724 (26) |
| Male | 69 | 4140 | 67 (61 to 74) | 919 (22) | 1425 (34) | 447 (11) | 1349 (33) | |
| Clinical practice and breast pathology expertise | ||||||||
| Have you received fellowship training in breast pathology? | ||||||||
| No | 109 | 6540 | 71 (66 to 75) | 0.36 | 1696 (26) | 2256 (34) | 665 (10) | 1923 (29) |
| Yes | 6 | 360 | 58 (31 to 86) | 35 (10) | 120 (33) | 55 (15) | 150 (42) | |
| Affiliation with academic medical centre | ||||||||
| No | 87 | 5220 | 73 (68 to 78) | 0.021 | 1324 (25) | 1895 (36) | 602 (12) | 1399 (27) |
| Yes | 28 | 1680 | 60 (49 to 70) | 407 (24) | 481 (29) | 118 (7) | 674 (40) | |
| Do your colleagues consider you an expert in breast pathology? | ||||||||
| No | 90 | 5400 | 74 (69 to 79) | 0.003 | 1411 (26) | 1916 (35) | 665 (12) | 1408 (26) |
| Yes | 25 | 1500 | 56 (44 to 67) | 320 (21) | 460 (31) | 55 (4) | 665 (44) | |
| How many years have you been interpreting breast pathology cases (not including residency/fellowship training)? | ||||||||
| <5 | 22 | 1320 | 75 (65 to 85) | 0.47 | 252 (19) | 548 (42) | 193 (15) | 327 (25) |
| 5–9 | 23 | 1380 | 74 (65 to 82) | 363 (26) | 480 (35) | 176 (13) | 361 (26) | |
| 10–19 | 34 | 2040 | 65 (55 to 76) | 488 (24) | 661 (32) | 187 (9) | 704 (35) | |
| ≥20 | 36 | 2160 | 68 (60 to 77) | 628 (29) | 687 (32) | 164 (8) | 681 (32) | |
| What percentage of your caseload includes interpreting breast specimens? | ||||||||
| <10% | 59 | 3540 | 70 (63 to 77) | 0.34 | 953 (27) | 1093 (31) | 434 (12) | 1060 (30) |
| 10–24% | 45 | 2700 | 73 (66 to 79) | 683 (25) | 1000 (37) | 283 (10) | 734 (27) | |
| ≥25% | 11 | 660 | 58 (37 to 78) | 95 (14) | 283 (43) | 3 (0) | 279 (42) | |
| Estimate the number of breast cases you interpret during an average week | ||||||||
| <5 | 31 | 1860 | 71 (62 to 80) | 0.58 | 579 (31) | 494 (27) | 253 (14) | 534 (29) |
| 5–9 | 44 | 2640 | 72 (64 to 79) | 645 (24) | 935 (35) | 314 (12) | 746 (28) | |
| 10–19 | 31 | 1860 | 71 (62 to 79) | 463 (25) | 716 (38) | 134 (7) | 547 (29) | |
| ≥20 | 9 | 540 | 54 (30 to 79) | 44 (8) | 231 (43) | 19 (4) | 246 (46) | |
Row percentages might not add up to 100 due to rounding.
By self-report on baseline survey.
Binary variable created from all three affirmative responses where 1=yes, 0=no. LS means and CIs estimated on logit scale and back transformed on the scale of the mean using the inverse link function.
Probability >χ2, Wald statistics for type 3 GEE analysis.
GEE, generalised estimating equation;
LS, least square.
Only two pathologists’ characteristics were statistically significantly associated with requesting second opinions. Requesting second opinions occurred less frequently for pathologists with academic medical centre affiliations (60% vs 73%, p = 0.021) and among pathologists considered experts in breast pathology by their peers (56% vs 74%, p = 0.003) compared with pathologists without these characteristics (table 1).
All of the case characteristics evaluated were significantly associated with whether or not a second opinion was requested (table 2).
Table 2.
Characteristics of test set cases by whether a participant pathologist would request a second opinion (N = 115 participants, 6900 independent assessments)
| Would you ask for a second pathologist’s opinion of this case before finalising the report? (Assume a pathologist is available.) | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Combined yes response rate (95% CI) |
Response options N (%) |
|||||||
|
|
|
|||||||
| Case characteristics* |
Number of cases |
Number of assessments |
Rate of second opinion for combined responses† |
p Value‡ | Yes, because I would want a second pathologist’s opinion for diagnostic reasons |
Yes, because it is our policy to get a second opinion in cases with this diagnosis |
Yes to both, because I would want it and because it is our policy |
No, I do not want a second opinion |
| Total | 240 | 6900 | 70 (65 to 75) | − | 1731 (25) | 2376 (34) | 720 (10) | 2073 (30) |
| Patient characteristics for breast biopsy cases | ||||||||
| Patient age (years)§ | ||||||||
| 40–49 | 118 | 3391 | 71 (66 to 76) | 0.038 | 856 (25) | 1188 (35) | 356 (10) | 991 (29) |
| 50–59 | 67 | 1924 | 70 (65 to 75) | 495 (26) | 663 (34) | 195 (10) | 571 (30) | |
| 60–69 | 29 | 833 | 67 (60 to 73) | 171 (21) | 295 (35) | 88 (11) | 279 (33) | |
| 70+ | 26 | 752 | 69 (63 to 75) | 209 (28) | 230 (31) | 81 (11) | 232 (31) | |
| Breast density§ | ||||||||
| Low density | 118 | 3391 | 68 (63 to 73) | <0.001 | 786 (23) | 1184 (35) | 340 (10) | 1081 (32) |
| High density | 122 | 3509 | 72 (67 to 77) | 945 (27) | 1192 (34) | 380 (11) | 992 (28) | |
| Biopsy type§,¶ | ||||||||
| Core needle biopsy | 138 | 3953 | 72 (67 to 77) | 0.006 | 969 (25) | 1415 (36) | 459 (12) | 1110 (28) |
| Excisional biopsy | 102 | 2947 | 67 (62 to 73) | 762 (26) | 961 (33) | 261 (9) | 963 (33) | |
| Case characteristics assessed by participant pathologists | ||||||||
| Cumulative number of unique sub-diagnoses given to a case** | ||||||||
| <4 | 50 | 1436 | 64 (58 to 71) | <0.001 | 141 (10) | 702 (49) | 80 (6) | 513 (36) |
| 4–7 | 137 | 3938 | 70 (66 to 75) | 1090 (28) | 1240 (31) | 445 (11) | 1163 (30) | |
| ≥8 | 53 | 1526 | 74 (69 to 79) | 500 (33) | 434 (28) | 195 (13) | 397 (26) | |
| Degree of challenge | ||||||||
| Low | − | 4829 | 59 (53 to 66) | <0.001 | 701 (15) | 1879 (39) | 292 (6) | 1957 (41) |
| High | − | 2071 | 94 (92 to 97) | 1030 (50) | 497 (24) | 428 (21) | 116 (6) | |
| Confidence in assessment | ||||||||
| High Confidence | − | 5640 | 65 (59 to 70) | <0.001 | 1107 (20) | 2071 (37) | 464 (8) | 1998 (35) |
| Low confidence | − | 1260 | 94 (91 to 97) | 624 (50) | 305 (24) | 256 (20) | 75 (6) | |
| Case considered borderline | ||||||||
| Yes | − | 1803 | 95 (93 to 97) | <0.001 | 954 (53) | 366 (20) | 398 (22) | 85 (5) |
| No | − | 5097 | 61 (55 to 67) | 777 (15) | 2010 (39) | 322 (6) | 1988 (39) | |
| Participant diagnosis | ||||||||
| Benign w/o atypia | − | 2658 | 55 (49 to 61) | <0.001 | 579 (22) | 708 (27) | 167 (6) | 1204 (45) |
| Atypia | − | 1336 | 88 (83 to 93) | 647 (48) | 292 (22) | 236 (18) | 161 (12) | |
| DCIS | − | 2186 | 77 (71 to 83) | 413 (19) | 998 (46) | 269 (12) | 506 (23) | |
| Invasive | − | 720 | 72 (65 to 79) | 92 (13) | 378 (53) | 48 (7) | 202 (28) | |
By self-report on baseline survey.
Row percentages might not add up to 100 due to rounding.
Binary variable created from all three affirmative responses where 1=yes, 0=no. LS means and CIs estimated on logit scale and back transformed on the scale of the mean using the inverse link function.
Probability > χ2, Wald statistics for type 3 GEE analysis.
Women’s age and biopsy type were provided to participants during specimen assessment; breast density was not provided.
Low density (≤50 fibroglandular; BIRADS category 1 and 2) and high density (≤51% fibroglandular; BIRADS category 3 and 4; breast density was not provided to participants during specimen assessment).
Number of unique diagnostic subtypes at the level of each case as determined by participants.
DCIS, ductal carcinoma in situ; GEE, generalised estimating equation; LS, least square.
Cases in which women had high versus low mammographic breast density (72% vs 68%; p≥0.001) were more likely to have a second opinion requested. Cases from core needle biopsies compared with excisional biopsies (72% vs 67%; p = 0.006), and cases with increasing cumulative unique diagnoses as indicated by the pathologists who interpreted the cases (<4 (64%), 4–7 (70%) and ≥8 (74%); p≤0.001) were also associated with more frequent requests for second opinions.
Pathologists were more likely to request second opinions for cases they considered challenging (94%), had low confidence in their assessments (94%), or considered borderline (95%), regardless of whether their decisions were based on policy and/ or for diagnostic reasons (all p≤0.001) (table 2). Pathologists requested a second opinion for diagnostic reasons alone for 50% of the cases when they considered them challenging or when confidence in their assessment was low, and 53% when they considered the case borderline between two diagnoses.
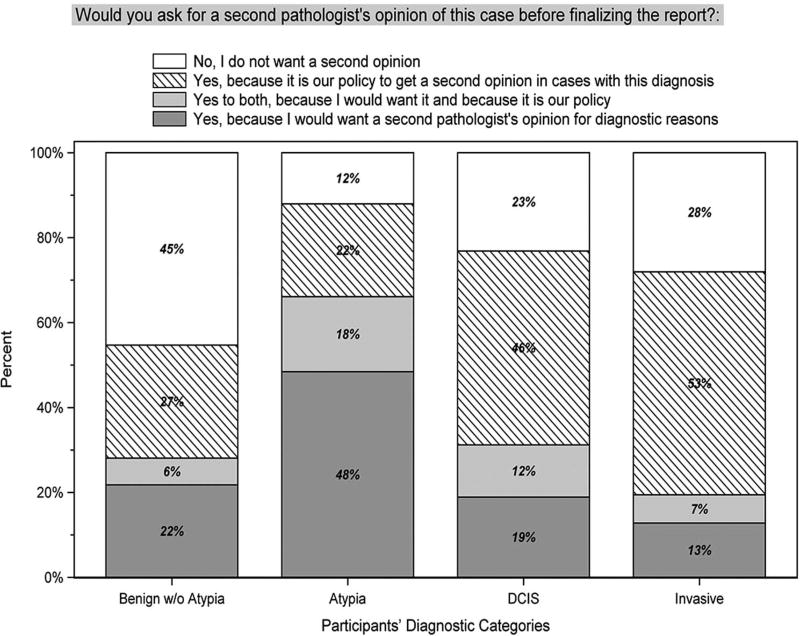
Figure 1 shows the reasons pathologists requested second opinions for each of the cases interpreted, according to the diagnosis that they indicated for the case. The most frequent request for a second opinion for either policy and/or diagnostic reasons was for cases of atypia; pathologists requested a second opinion on 88% of all cases that they interpreted as atypia. Atypia was the most frequent diagnosis for which a second opinion was desired for personal diagnostic reasons (66% of all cases interpreted as atypia). In contrast, pathologists were least likely to request a second opinion for diagnostic reasons for cases of invasive carcinoma (20% of all invasive cases). However, as expected, invasive carcinoma was the most common diagnostic category for which pathologists noted that a second opinion would be required by policy in their own practices (60% of all invasive cases).
Figure 1.
Requests for second opinion by participating pathologists’ diagnostic categories.
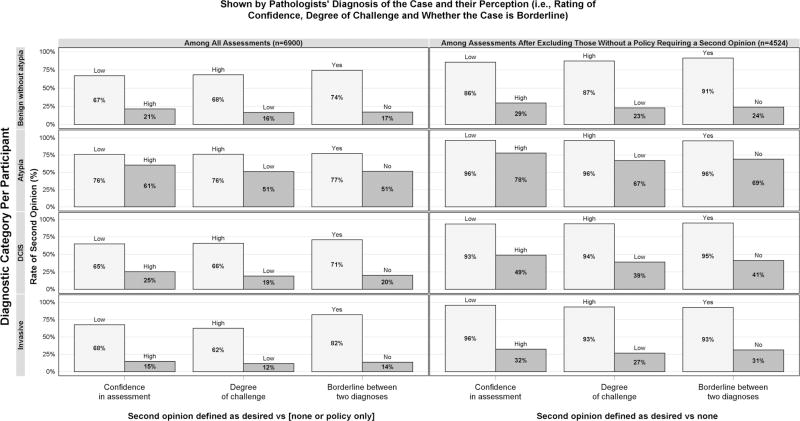
To better understand how perceptions of a case and diagnostic categories were related to the second opinion requests for diagnostic reasons (and not for policy reasons) we used a comparison group combining the responses ‘No, I don’t want a second opinion’ and ‘Yes, I want a second opinion because it is a policy’ (left side of figure 2 and see online supplementary table S1). Pathologists’ perception of a case mattered when they checked off whether or not they desired a second opinion for diagnostic reasons. Pathologists were significantly more likely to want a second opinion when they had low confidence in their assessment, when the case was perceived as challenging, or when it was considered borderline (p<0.001). These statistically significant differences were noted regardless of the pathologists’ diagnosis of the case. The atypia diagnosis category was distinct from the other three diagnostic categories; pathologists desired a second opinion for more than 50% of the cases they interpreted as atypia even when the pathologist was confident, ranked the case a low degree of challenge, and did not consider it borderline. The most frequent request for a second opinion for diagnostic reasons was for invasive cancer that was considered borderline (82%, CI 69% to 90%); the most frequent alternative diagnoses selected for these borderline cases were DCIS (60%), sclerosing adenosis (19%) and radial scar (17%). The least frequent request for a second opinion was for invasive cases in which the case was ranked low in degree of challenge (12%, CI 8% to 17%).
Figure 2.
Proportion of second opinions requested for the test set cases by case-level pathologists’ perceptions and their diagnostic categories.
When comparing interpretations for which a second opinion was desired for diagnostic reasons with those for which a second opinion was not desired (excluding from the analysis second opinions indicated only due to policy), comparison of rates of second opinions was statistically significantly associated only with cases considered borderline across all diagnostic categories (right side of figure 2; p = 0.005). When the pathologists’ confidence in the assessment was low, pathologists desired a second opinion most frequently for the diagnosis of atypia (96%, CI 92% to 98%) and invasive cancer (96%, CI 77% to 99%) (see online supplementary table S2). However, pathologists desired second opinions for over 67% of cases (data not shown) of atypia despite feeling confident in their diagnoses, indicating the case was easy, and noting that the case was not borderline.
DISCUSSION
In this study of interpretations of breast biopsy cases, pathologists indicated frequent requests for second opinions when they were less confident in their assessments, found the case challenging, and identified the case as borderline, even when their laboratory policies did not require second opinions. As expected, pathologists affiliated with academic medical centres or considered experts in breast pathology by their peers were less likely to request second opinions than pathologists without these characteristics. However, characteristics of the case, rather than the pathologist, were more often associated with requests for second opinions.
The diagnosis of breast epithelial atypia (ADH and ADH in a papilloma) had the highest rate of second opinion requests by the participating pathologist within the four diagnostic categories evaluated. Notably, these requests were observed regardless of the pathologists’ confidence in assessment, diagnostic challenge of the case, or presence of borderline diagnostic features. When we excluded cases where the pathologist indicated the only reason for a second opinion was a laboratory policy, the rates for second opinion requests increased in all diagnostic categories. As expected, rates were high (86–96%) when pathologists indicated they were not confident in the diagnosis, the case was challenging, or the case was borderline between two categories. In contrast to the other diagnostic categories, cases with atypia had high rates of second opinion requests (67–78%) even when pathologists indicated they were confident, the case was easier, and the case did not have borderline features.
These findings suggest that pathologists frequently desire and likely obtain second opinions in clinical practice, particularly for cases with atypia. Considering the low diagnostic agreement rates for atypia that have been reported,10 diagnostic accuracy might be improved if second opinions were obtained for all cases with atypia. More widespread adoption of second opinion policies and guidelines may improve diagnostic accuracy and provide the support that practicing pathologists seem to want.
A decade ago, an external review of the UK National Health Service Breast Screening Programme (NHSBSP) reported several areas in breast pathology that could be improved but concluded that the diagnosis of atypical hyperplasia, which they found to have very poor concordance, cannot be improved.15 In the evaluation of the NHSBSP they noted that the diagnostic criteria for atypical hyperplasia, which at that time had been recently updated, did not improve the diagnosis and they did not recommend any other avenues for improvement. However, others have suggested that obtaining second opinions on these challenging cases might improve accuracy.16
Increased mammographic breast density was associated with higher rates of requests for second opinions in the present study, as well as with lower diagnostic agreement among pathologists in a prior B-Path Study.10 Breast density is primarily attributable to fibrous tissue of the breast.17–19 However, breast fibrosis is not a factor considered in the diagnosis of epithelial proliferations pathologically. To further explore the potential effect of density, we also evaluated whether the spectrum of epithelial proliferation present in a case might be associated with increased requests for second opinion and noted that requests increased for cases with higher cumulative unique diagnoses attributed to the case by the multiple pathologists who independently interpreted the case. Thus, we hypothesise that epithelial breast complexity, by inference, is associated with breast density.
This work presents new findings of the B-Path Study, which was originally designed to evaluate diagnostic variation in the interpretation of breast biopsies among practicing pathologists by collecting data related to diagnostic accuracy. The present study describes in detail pathologists’ desires for second opinion when interpreting breast biopsy cases and evaluates whether intrinsic features of the breast biopsy specimen and characteristics of pathologists were associated with pathologists’ requests for consultative second opinions. To our knowledge, this is the first study to examine these associations of case and pathologists’ characteristics with obtaining second opinions. Most studies examining the use of second opinions focus on changes in histological diagnoses3–7,20 and do not report the pathologists’ underlying perceptions of the case or characteristics associated with cases where they desire second opinions. Although some studies have reported case characteristics, such as diagnoses and oestrogen-progesterone receptors and HER2 status, none have related them to the use of second opinion.15,20
The strengths of this study include the participation of a large number of practicing pathologists (N = 115) from across the US, each interpreting 60 cases and providing independent diagnostic assessments and their perceptions regarding challenges in interpreting these cases. These data were then linked to pathologist demographic and clinical practice characteristics and case characteristics. The results of this study could guide educational interventions for practicing pathologists and trainees, as well as inform policy changes to improve diagnostic systems by establishing system-level strategies for when second opinions should be obtained.
There are several limitations to this study. While this study used a single slide to improve efficiency and enhance participation of practicing pathologists, it does not replicate clinical practice, where the initial pathologist evaluating a case may have access to additional slides or special stains and the option to consult with other pathologists. Interpreting cases in this situation, especially when the cases included more atypia and DCIS than typically observed in clinical practice, may also alter interpretive performance. This may have led to more assessments rated as challenging.
CONCLUSIONS
In conclusion, breast biopsies are challenging to interpret10 and likely lead to frequent second opinions in clinical practice regardless of institutional policy.8 Clinical systems may need to be optimised to support pathologists and their desires for the use of second opinions. In addition, broader reimbursement may be needed for second opinion if future research shows that second opinions lead to improvements in clinical care. We identified breast biopsy case characteristics that are strongly associated with whether practicing pathologists desire second opinions. Pathologists frequently request second opinions for challenging cases, particularly for cases with atypia, high breast density, core needle biopsies, or many co-existing diagnoses. Further studies should evaluate whether the case characteristics identified in this study could be used as clinical criteria to prompt second opinions. The ultimate goal of these efforts is to improve support for practicing pathologists, laboratory efficiency, and outcomes for patients.
Supplementary Material
Take home messages.
-
▸
Breast biopsy case characteristics such as patient age, core needle biopsy and dense mammographic breast tissue were significantly associated with requests for a second opinion.
-
▸
Pathologists frequently requested second opinions when they were less confident in their assessments, found the case challenging, and/or identified the case as borderline between two diagnostic categories, even when their laboratory policies did not require second opinions.
-
▸
Second opinions were most frequently requested for diagnoses of atypical ductal hyperplasia.
-
▸
Adoption of broader second opinion guidelines and policies may improve diagnostic accuracy and provide the support that practicing pathologists seem to desire.
Acknowledgments
Funding This work was supported by the National Cancer Institute of the National Institutes of Health (R01 CA140560, R01 CA172343, U01CA86082, U01CA70013); and by the National Cancer Institute-funded Breast Cancer Surveillance Consortium (HHSN261201100031C). The content is solely the responsibility of the authors and does not necessarily represent the views of the National Cancer Institute or the National Institutes of Health.
Footnotes
Contributors BMG, HDN, PDF, JGE conceived and designed the study. DLW, KHA, HDN, BMG, JGE, PAC, TLO, AT contributed to the development of the survey and the acquisition of data. BMG, HDN, DLW, JGE, PDF contributed to the analysis. DLW, KHA, HDN, BMG, JGE, PAC, TLO, ANAT contributed to the interpretation of data. BMG, HDN, JGE, TLO, PDF contributed to drafting the manuscript. DLW, KHA, HDN, BMG, JGE, PAC, TLO, ANAT, PDF contributed to revising it critically for important intellectual content as well as approving the final version.
Competing interests None declared.
Ethics approval The Institutional Review Boards of Dartmouth College, the Fred Hutchinson Cancer Research Center, Providence Health & Services of Oregon, the University of Vermont, and the University of Washington approved all study procedures. All participating pathologists signed an informed consent form.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The collection of cancer and vital status data used in this study was supported in part by several state public health departments and cancer registries throughout the US. For a full description of these sources, please see: http://www.breastscreening.cancer.gov/work/acknowledgement.html. Please contact the authors directly if you would like to discuss data.
References
- 1.Middleton LP, Feeley TW, Albright HW, et al. Second-opinion pathologic review is a patient safety mechanism that helps reduce error and decrease waste. J Oncol Pract. 2014;10:275–80. doi: 10.1200/JOP.2013.001204. [DOI] [PubMed] [Google Scholar]
- 2.Elmore JG, Tosteson ANA, Pepe MS, et al. Evaluation of 12 strategies for obtaining second opinions to improve interpretation of breast histopathology: simulation study. BMJ. 2016;353:i3069. doi: 10.1136/bmj.i3069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manion E, Cohen M, Weydert J. Mandatory second opinion in surgical pathology referral material: clinical consequences of major disagreements. Am J Surg Path. 2008;32:732–7. doi: 10.1097/PAS.0b013e31815a04f5. [DOI] [PubMed] [Google Scholar]
- 4.Kronz J, Westra W, Epstein J. Mandatory second opinion surgical pathology at a large referral hospital. Cancer. 1999;86:2426–35. [PubMed] [Google Scholar]
- 5.Gupta D, Layfield L. Prevalence of inter-institutional anatomic pathology slide review. Am J Surg Pathol. 2000;24:280–4. doi: 10.1097/00000478-200002000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Tomaszewski J, Bear H, Connally J, et al. Consensus conference on second opinion in diagnostic anatomic pathology: Who, what, and when. Am J Clin Pathol. 2000;114:329–35. doi: 10.1093/ajcp/114.3.329. [DOI] [PubMed] [Google Scholar]
- 7.Renshaw A, Gould EW. Measuring the value of review of pathology material by a second pathologist. Am J Cin Pathol. 2006;125:737–9. doi: 10.1309/6A0R-AX9K-CR8V-WCG4. [DOI] [PubMed] [Google Scholar]
- 8.Geller B, Nelson H, Carney P, et al. Second opinion in breast pathology: policy, practice and perception. J Clin Pathol. 2014;67:955–60. doi: 10.1136/jclinpath-2014-202290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finn WG, Holladay E. Discordant interpretations of breast biopsy specimens by pathologists. JAMA. 2015;314:82–82. doi: 10.1001/jama.2015.6230. [DOI] [PubMed] [Google Scholar]
- 10.Elmore J, Longton G, Carney P, et al. Diagnostic concordance among pathologists interpreting breast biopsy specimens. JAMA. 2015;313:1122–32. doi: 10.1001/jama.2015.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oster N, Carney P, Allison K, et al. Development of a diagnostic test set to assess agreement in breast pathology: practical application of the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) BMC Womens Health. 2013;13:3. doi: 10.1186/1472-6874-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elmore J, Nelson H, Pepe M, et al. Variability of pathologists’ interpretations of individual breast biopsy slides: a population perspective. Ann Intern Med. 2016;164:649–55. doi: 10.7326/M15-0964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ballard-Barbash R, Taplin S, Yankaskas B, et al. Breast cancer surveillance consortium: a national mammography screening and outcomes database. Am J Roentgenol. 1997;169:1001–8. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 14.Onega T, Weaver D, Geller B, et al. Digitized whole slides for breast pathology interpretation: current practices and perceptions. J Digit Imaging. 2014;27:642–8. doi: 10.1007/s10278-014-9683-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellis I, Coleman D, Wells C, et al. Impact of a national external quality assessment scheme for breast pathology in the UK. J Clin Pathol. 2006;59:138–45. doi: 10.1136/jcp.2004.025551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davidson N, Rimm D. Expertise vs evidence in assessment of breast biopsies: an atypical science. JAMA. 2015;313:1109–10. doi: 10.1001/jama.2015.1945. [DOI] [PubMed] [Google Scholar]
- 17.Lin S, Cawson J, Hill P, et al. Image-guided sampling reveals increased stroma and lower glandular complexity in mammographically dense breast tissue. Breast Cancer Res Treat. 2011;128:505–16. doi: 10.1007/s10549-011-1346-0. [DOI] [PubMed] [Google Scholar]
- 18.Alowami S, Troup S, Al-Haddad S, et al. Mammographic density is related to stroma and stromal proteoglycan expression. Breast Cancer Res. 2003;5:R29–35. doi: 10.1186/bcr622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li T, Sun L, Miller N, et al. The association of measured breast tissue characteristics with mammographic density and other risk factors for breast cancer. Cancer Epidemiol Biomarkers Prev. 2005;14:343–9. doi: 10.1158/1055-9965.EPI-04-0490. [DOI] [PubMed] [Google Scholar]
- 20.Marco V, Muntal T, García-Hernandez F, et al. Changes in breast cancer reports after pathology second opinion. Breast J. 2014;20:295–301. doi: 10.1111/tbj.12252. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.