Abstract
Introduction
The number of adolescents with a severe chronic disease has increased in high-income countries due to improvements in the prognosis of childhood-onset chronic conditions. The transition from childhood to adulthood is a critical period that may be associated with increased mortality and morbidity. We aimed to estimate the prevalence of adolescents with a long-term disease (LTD) in France and assess their mortality and hospitalization risks relative to the general population.
Materials and methods
We extracted a population-based cohort from the French national health insurance database that included 61,119 subjects who reached 14 years of age between 2005 and 2014. LTDs are diagnosed by patients’ physicians and then confirmed and registered by a physician of the national health insurance system. We assessed mortality and hospitalizations using data of patients who were between 14 and 21 years-old.
Results
Among 14-year-old adolescents, 3.30% (95% confidence interval: 3.16–3.44) had a LTD. Their mortality rate between the ages of 14 and 21 years was 20.9/10,000 person-years (13.7–32.1) versus 1.9 (1.5–2.5) for adolescents without a LTD. Mortality was higher in males than females in youths without a LTD, but not in those with a LTD. We found a similar pattern for the risk of hospitalization for an external cause. The five-year probability of hospitalization was 61.8% among youths with a LTD versus 42.7% for those without. The rate of planned hospitalizations sharply fell at 19 years-of-age among youths with a LTD, whereas the rate of unplanned hospitalizations remained stable.
Conclusion
The 3% of youths with a LTD have ten-fold higher mortality than those without and a high risk of hospitalization. The decrease in the rate of planned hospitalizations at age 19 among youths with a LTD may indicate differences in medical practice after transfer to adult care or a break in medical care.
Introduction
The prognosis of childhood-onset chronic conditions has improved in recent decades in high-income countries, such that more patients now reach adulthood. For example, the proportion of cystic fibrosis patients reaching adulthood (>18 years of age) increased from 27% to 56% between 1982 and 2007 and is forecasted to reach approximately 75% by 2025 in Western European countries [1,2]. It is estimated that almost 90% of children with congenital heart diseases will survive into adulthood, together with 94% of children with sickle cell anemia [3,4]. The population of perinatally HIV-infected patients is also ageing [5]. Better survival has likely led to an increase in the number of adolescents living with a chronic disease, but little national-level data are available on this subject.
Youths living with a chronic disease since childhood share many concerns during transition to adulthood [6], including taking increasing responsibility for their health and healthcare [7–10]. It is important to study this period of life, because adolescence is a critical period that may be associated with poor outcomes [6]. Epidemiological data on mortality and healthcare use in adolescents and young adults are yet sparse and often limited to a specific disease. Some studies have reported higher rates of healthcare use, either planned, unplanned, or both after entry into adolescence or young adulthood for patients with a childhood-onset chronic disease [11–17]. Conducting non-disease-specific studies could provide researchers and decision makers with original insights on how transition to adulthood is related to prognosis and planned or unplanned healthcare use. Such information could lead to a better understanding of the epidemiology of these diseases in adolescents and young adults and improvements in healthcare organization.
Furthermore, these youths must face the challenges of this period related to physiological, psychological, and socio-economic changes, as all adolescents. Conducting studies comparing youths with or without a chronic disease could help identify the role of the chronic condition in healthcare use versus that of entry into adulthood.
The French national health insurance database is one of the largest databases in the world and has been extensively used to guide public health policies in France, as these data allow systematic follow-up of all medical care received in France, including that of the low-income population [18–20]. With the Universal Health Coverage Act (opening up the right to statutory health insurance coverage on the basis of residence in France), data on almost all French residents, i.e., people living in France (with or without French nationality), are registered in this database. In addition, a list of major groups of chronic diseases, for which the severity and/or chronic nature requires prolonged treatment and costly therapy, has been established by decree as “Affections de Longue Durée” (long-term diseases, LTD) to allow patients to receive full reimbursement for expenditures related to the LTD. This provided the opportunity to estimate the prevalence of adolescents with a LTD diagnosed before 14 years of age at the national level and to describe the mortality and short-stay hospitalization rates between youths from 14 to 21 years of age, with or without a LTD.
Materials and methods
The EGB
The French national health insurance offers access to a large ongoing random sampling of 801,047 (at the time of this study) for research purposes, the Echantillon Généraliste des Bénéficiaires (EGB)[General Beneficiaries Sample] [18,21,22]. The EGB includes exhaustive records of hospitalizations in short-stay units (medical, surgical, obstetrical) from the national hospital discharge database, from 2005 to the end of 2015, and all data on LTD and mortality for subjects insured under the French general health insurance schemes, representing 80% of the population. The other types of hospitalizations (i.e., hospitalizations in psychiatric units, home-hospitalizations, and hospitalization in long-stay units) were not exhaustively recorded in the database during the study period and were thus not analyzed.
Inclusion criteria
We selected all 61,119 adolescents from the EGB insured under the general scheme, who had reached the age of 14 years during the period from 01/03/2005 to 31/12/2014. We did not consider those who reached 14 after 2014 to allow at least 1 year of observation. This represents a sample of the generation born between 01/03/1991 and 31/12/1999 who were still alive and living in France at the age of 14.
Study design
We selected a retrospective cohort using data of youths between the ages of 14 and 21 years to compare mortality and hospitalization rates between adolescents with or without a LTD. This age range, from one year before healthcare adulthood (in France, patients can be managed in adult care from the age of 15 years) to three years after legal adulthood (18 years old), thus covered the period of transition to young adulthood.
Definition and classification of long-term diseases
LTD registration is obtained at the request of a patient’s physician and must be validated by the health insurance system physician, who codes the diagnosis using the International Classification of Diseases version 10 (ICD-10). Thirty-eight diseases registered before the age of 14 in our study population were identified as long-term, based on the LTD diagnosis codes. Trauma and burns were not considered as LTDs, nor tuberculosis, because such a condition should be resolved with antibiotic treatment and not last until adulthood. LTDs were classified into three categories defined in a previous Canadian study exploring youths with chronic health conditions [15]: chronic mental-health conditions, non-complex chronic conditions (chronic conditions typically affecting a single organ system), and complex chronic conditions (chronic medical conditions in which multiple morbidities and/or multi-organ manifestations are common) (S1 Table).
Overall, 2,019 subjects had at least one LTD registration before the age of 14 years, and were thus included in the LTD group for this study. The comparison group (N = 59,100) comprised the subjects without a LTD registration before the age of 14 years. Among them, the follow-up of those registered for a LTD after 14 (N = 879) was censored at LTD registration.
Outcomes
We studied two types of outcomes: 1) all-cause mortality, using data from the national death registry and 2) hospitalizations in short-stay units. Two categories of hospitalizations were considered: unplanned, defined as an admission through an emergency department (ED) and planned, without admission through an ED. We also explored hospitalizations for an external cause, as a proxy of exposure to high-risk situations, such as injuries and road accidents, which are major causes of death in youths. An external cause was defined as a main diagnosis from the ICD-10 chapter “Injury, poisoning, and certain other consequences of external causes”, excluding complications of medical or surgical care, allergies, or intoxication by non-psychotropic drugs, which may be related to the LTD.
Statistical methods
We first estimated the overall and gender-specific prevalence of the subjects with a LTD among adolescents aged 14 years. Then, overall and gender-specific annual mortality rates between the ages of 14 and 21 years were estimated by LTD status. Mortality rates were compared between females and males by estimating rate ratios with a 95% confidence interval (95%CI). The interaction between gender and LTD status towards mortality was tested using a Cox model. We then estimated the probability of being hospitalized by the age of 21 years, using the Kaplan-Meier method, by setting the time scale to age, and performed log-rank tests to compare survival curves. The repartition of the main diagnosis (ICD-10 chapter) of each stay was described by LTD status and gender for planned and unplanned hospitalizations. The evolution of the annual incidence rates of hospitalization by age were described from 14 to 21 years of age. The analyses were performed using SAS Enterprise Guide 4.3 software, SAS Institute Inc., Cary, NC and STATA 13.1 (StataCorp LP Lakeway Drive College Station, Texas 77845 USA).
Ethical approval
A specific ethics committee approval was not required for this study. INSERM, as a health research institute, has been authorized to use the EGB database by the French data protection authority (Commission Nationale de l’Informatique et des Libertés, CNIL), provided that the researcher follows specific training with certification, as the first author (Antoine Rachas) has obtained. Then he has been authorized to access and analyze the EGB database for this study.
Results
Prevalence of long-term diseases at the age of 14 years
Among the 801,047 subjects included in the EGB, 61,119 were eligible and included in this analysis (S1 Fig). Among them, 3.30% (95%CI: 3.16–3.44; N = 2,019) had a LTD at the age of 14 years (Table 1) and 879 were registered for a LTD after the age of 14 years and were censored at date of LTD registration. LTDs were significantly less frequent among females (2.78%) than males (3.80%). A chronic mental health disease was present in 0.81% of subjects (0.43% of females, 1.18% of males), a non-complex chronic condition in 1.10% (0.93% of females, 1.26% of males), and a complex chronic condition in 1.39% (1.42% of females, 1.36% of males). The five most frequent diseases were persistent asthma (0.38%), autism spectrum disorders (0.27%), mental retardation (0.25%), progressive structural scoliosis (0.23%), and neurotic, emotional, and mood disorders (0.22%).
Table 1. Prevalence of subjects with a long-term disease at 14 years of age.
| Category | Group | Conditions | All (N = 61,119) | Females (N = 29,860) | Males (N = 31,259) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Pr, % | (95%CI) | n | Pr, % | (95%CI) | n | Pr, % | (95%CI) | |||
| All | All | All | 2,019 | 3.30 | (3.16;3.44) | 831 | 2.78 | (2.59;2.97) | 1,188 | 3.80 | (3.59;4.01) |
| Mental | All | All | 498 | 0.81 | (0.74;0.88) | 129 | 0.43 | (0.36;0.50) | 369 | 1.18 | (1.06;1.30) |
| Psychiatric diseases | Autism spectrum disorders | 166 | 0.27 | (0.23;0.31) | 39 | 0.13 | (0.09;0.17) | 127 | 0.41 | (0.34;0.48) | |
| Specific personality disorders | 120 | 0.20 | (0.16;0.24) | 28 | 0.09 | (0.06;0.12) | 92 | 0.29 | (0.23;0.35) | ||
| Psychotic disorders | 22 | 0.04 | (0.02;0.06) | 10 | 0.03 | (0.01;0.05) | 12 | 0.04 | (0.02;0.06) | ||
| Neurotic, emotional, mood disorders | 135 | 0.22 | (0.18;0.26) | 37 | 0.12 | (0.08;0.16) | 98 | 0.31 | (0.25;0.37) | ||
| Other psychological development disorder | 54 | 0.09 | (0.07;0.11) | 14 | 0.05 | (0.02;0.08) | 40 | 0.13 | (0.09;0.17) | ||
| Other psychiatric affections | 1 | 0.00 | (0.00;0.00) | 1 | 0.00 | (0.00;0.00) | 0 | 0.00 | (0.00;0.00) | ||
| Non-complex | All | All | 671 | 1.10 | (1.02;1.18) | 278 | 0.93 | (0.82;1.04) | 393 | 1.26 | (1.14;1.38) |
| Endocrine and metabolic diseases | Type 1 and type 2 diabetes | 114 | 0.19 | (0.16;0.22) | 48 | 0.16 | (0.11;0.21) | 66 | 0.21 | (0.16;0.26) | |
| Respiratory diseases | Persistent asthma | 235 | 0.38 | (0.33;0.43) | 88 | 0.29 | (0.23;0.35) | 147 | 0.47 | (0.39;0.55) | |
| Other serious chronic respiratory insufficiency | 17 | 0.03 | (0.02;0.04) | 8 | 0.03 | (0.01;0.05) | 9 | 0.03 | (0.01;0.05) | ||
| Vascular diseases | Chronic arteriopathies with ischemic manifestations | 3 | 0.00 | (0.00;0.00) | 3 | 0.01 | (0.00;0.02) | 0 | 0.00 | (0.00;0.00) | |
| Severe hypertension | 3 | 0.00 | (0.00;0.00) | 1 | 0.00 | (0.00;0.00) | 2 | 0.01 | (0.00;0.02) | ||
| Heart disease | Severe congenital heart disease | 110 | 0.18 | (0.15;0.21) | 48 | 0.16 | (0.11;0.21) | 62 | 0.20 | (0.15;0.25) | |
| Other heart diseases | 23 | 0.04 | (0.02;0.06) | 12 | 0.04 | (0.02;0.06) | 11 | 0.04 | (0.02;0.06) | ||
| Kidney diseases | Severe chronic kidney disease and primitive nephrotic syndrome | 47 | 0.08 | (0.06;0.10) | 24 | 0.08 | (0.05;0.11) | 23 | 0.07 | (0.04;0.10) | |
| Liver diseases | Active chronic liver disease and cirrhosis | 15 | 0.02 | (0.01;0.03) | 8 | 0.03 | (0.01;0.05) | 7 | 0.02 | (0.00;0.04) | |
| Inflammatory Bowel Disease | Progressive Crohn's disease and ulcerative colitis | 26 | 0.04 | (0.02;0.06) | 13 | 0.04 | (0.02;0.06) | 13 | 0.04 | (0.02;0.06) | |
| Malignancies | Malignant tumor, malignant disease of lymphatic tissue or blood | 78 | 0.13 | (0.10;0.16) | 25 | 0.08 | (0.05;0.11) | 53 | 0.17 | (0.12;0.22) | |
| Complex | All | All | 850 | 1.39 | (1.30;1.48) | 424 | 1.42 | (1.29;1.55) | 426 | 1.36 | (1.23;1.49) |
| Chromosome abnormalities | Down syndrome | 45 | 0.07 | (0.05;0.09) | 19 | 0.06 | (0.03;0.09) | 26 | 0.08 | (0.05;0.11) | |
| Other chromosome abnormalities | 15 | 0.02 | (0.01;0.03) | 10 | 0.03 | (0.01;0.05) | 5 | 0.02 | (0.00;0.04) | ||
| Neurological and muscular diseases | Cerebral palsy | 89 | 0.15 | (0.12;0.18) | 37 | 0.12 | (0.08;0.16) | 52 | 0.17 | (0.12;0.22) | |
| Paraplegia | 11 | 0.02 | (0.01;0.03) | 6 | 0.02 | (0.00;0.04) | 5 | 0.02 | (0.00;0.04) | ||
| Severe epilepsy | 94 | 0.15 | (0.12;0.18) | 45 | 0.15 | (0.11;0.19) | 49 | 0.16 | (0.12;0.20) | ||
| Other serious neurological and muscular diseases | 72 | 0.12 | (0.09;0.15) | 30 | 0.10 | (0.06;0.14) | 42 | 0.13 | (0.09;0.17) | ||
| Mental retardation | Mental retardation | 152 | 0.25 | (0.21;0.29) | 48 | 0.16 | (0.11;0.21) | 104 | 0.33 | (0.27;0.39) | |
| Immunodeficiencies | Severe primary immunodeficiency requiring prolonged treatment | 9 | 0.01 | (0.00;0.02) | 1 | 0.00 | (0.00;0.00) | 8 | 0.03 | (0.01;0.05) | |
| HIV infection | 15 | 0.02 | (0.01;0.03) | 6 | 0.02 | (0.00;0.04) | 9 | 0.03 | (0.01;0.05) | ||
| Medullary deficiencies and other chronic cytopenias | 3 | 0.00 | (0.00;0.00) | 1 | 0.00 | (0.00;0.00) | 2 | 0.01 | (0.00;0.02) | ||
| Hemolysis | Hemoglobinopathies | 17 | 0.03 | (0.02;0.04) | 6 | 0.02 | (0.00;0.04) | 11 | 0.04 | (0.02;0.06) | |
| Other constitutional chronic hemolysis, acquired hemolysis | 5 | 0.01 | (0.00;0.02) | 3 | 0.01 | (0.00;0.02) | 2 | 0.01 | (0.00;0.02) | ||
| Rheumatologic and systemic diseases | Progressive rheumatoid arthritis | 5 | 0.01 | (0.00;0.02) | 2 | 0.01 | (0.00;0.02) | 3 | 0.01 | (0.00;0.02) | |
| Juvenile arthritis | 16 | 0.03 | (0.02;0.04) | 8 | 0.03 | (0.01;0.05) | 8 | 0.03 | (0.01;0.05) | ||
| Progressive structural scoliosis | 139 | 0.23 | (0.19;0.27) | 124 | 0.42 | (0.35;0.49) | 15 | 0.05 | (0.03;0.07) | ||
| Vasculitis, systemic lupus erythematosus, systemic scleroderma | 3 | 0.00 | (0.00;0.00) | 2 | 0.01 | (0.00;0.02) | 1 | 0.00 | (0.00;0.00) | ||
| Hemorrhagic diseases | Hemophilia and serious constitutional disorders of hemostasis | 13 | 0.02 | (0.01;0.03) | 3 | 0.01 | (0.00;0.02) | 10 | 0.03 | (0.01;0.05) | |
| Purpura and other hemorrhagic conditions | 11 | 0.02 | (0.01;0.03) | 3 | 0.01 | (0.00;0.02) | 8 | 0.03 | (0.01;0.05) | ||
| Endocrine and metabolic diseases | Inherited metabolic diseases requiring prolonged treatment | 83 | 0.14 | (0.11;0.17) | 46 | 0.15 | (0.11;0.19) | 37 | 0.12 | (0.08;0.16) | |
| Respiratory diseases | Cystic fibrosis | 5 | 0.01 | (0.00;0.02) | 2 | 0.01 | (0.00;0.02) | 3 | 0.01 | (0.00;0.02) | |
| Vascular diseases | Disabling stroke | 21 | 0.03 | (0.02;0.04) | 11 | 0.04 | (0.02;0.06) | 10 | 0.03 | (0.01;0.05) | |
| Multiple diseases | Multiple diseases | 27 | 0.04 | (0.02;0.06) | 11 | 0.04 | (0.02;0.06) | 16 | 0.05 | (0.03;0.07) | |
Abbreviations: 95%CI, 95% confidence interval; Pr, prevalence
Mortality
Twenty-one subjects with a LTD and 56 with no LTD died between the ages of 14 and 21 years (Table 2). The mortality rates per 10,000 person-years were 20.9 [95%CI: 13.7–32.1] and 1.9 [1.5–2.5], respectively. Mortality rate was the highest in the subjects with a complex chronic condition (30.9/10,000 person-years [17.9–53.2]). Among those with no LTD, females were less likely to die than males, with a mortality rate ratio (MRR) of 0.2; 95%CI: 0.1–0.4. This was not the case for those with a LTD (MRR: 1.3; 95%CI: 0.5–3.4). The test for interaction between gender and LTD status was significant (p = 0.001).
Table 2. Overall and gender-specific mortality between 14 and 21 years of age according to long-term disease.
| All (N = 61,119) | Females (N = 29,860) | Males (N = 31,259) | MRR (95%CI), females vs. males | ||||
|---|---|---|---|---|---|---|---|
| n | MR (95%CI), per 10,000 PY | n | MR (95%CI), per 10,000 PY | n | MR (95%CI), per 10,000 PY | ||
| All | 77 | 2.6 (2.1–3.2) | 19 | 1.3 (0.8–2.0) | 58 | 3.8 (2.9–4.9) | 0.3 (0.2–0.6) |
| No LTD | 56 | 1.9 (1.5–2.5) | 9 | 0.6 (0.3–1.2) | 47 | 3.2 (2.4–4.2) | 0.2 (0.1–0.4) |
| LTD | 21 | 20.9 (13.7–32.1) | 10 | 23.9 (12.8–44.3) | 11 | 18.4 (10.2–33.2) | 1.3 (0.5–3.4) |
| Mental | 2 | 8.2 (2.1–32.9) | 1 | 15.0 (2.1–106.6) | 1 | 5.4 (0.8–38.6) | 2.8 (0.0–217.1) |
| Non-complex | 6 | 17.7 (8.0–39.5) | 4 | 29.0 (10.9–77.4) | 2 | 10.0 (2.5–40.1) | 2.9 (0.4–32.0) |
| Complex | 13 | 30.9 (17.9–53.2) | 5 | 23.3 (9.7–55.9) | 8 | 37.1 (18.6–74.3) | 0.6 (0.2–2.2) |
Abbreviations: LTD, long-term disease; MR, mortality rate; MRR, mortality rate ratio; PY, person-year; 95%CI, 95% confidence interval
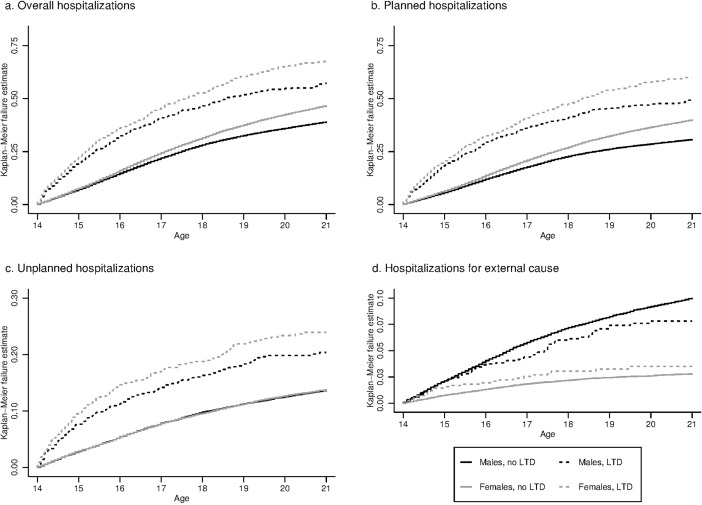
Overall hospitalizations
The probability of being hospitalized at least once between the ages of 14 and 21 years, estimated using the Kaplan-Meier method, was 61.8% for subjects with a LTD and 42.7% for those without (Table 3); log-rank p-value < 0.0001. The probability was the highest for subjects with a complex chronic condition (67.2%). Females were more likely to be hospitalized than males (Fig 1A), in both the LTD (67.5% vs. 57.5%, log-rank p-value < 0.001) and no LTD groups (46.6% vs. 38.9%, log-rank p-value < 0.0001).
Table 3. Overall and gender-specific probabilities of short-stay hospitalizations between the ages of 14 and 21 years according to the presence of a long-term disease.
| Outcome | Group | All (N = 61,119) | Females (N = 29,860) | Males (N = 31,259) | |||
|---|---|---|---|---|---|---|---|
| n | Prob. (95%CI), % | n | Prob. (95%CI), % | n | Prob. (95%CI), % | ||
| ≥ 1 Hospitalization | No LTD | 19,629 | 42.7 (42.2–43.2) | 10,426 | 46.6 (45.9–47.3) | 9,203 | 38.9 (38.3–39.6) |
| LTD | 1,025 | 61.8 (59.1–64.5) | 465 | 67.5 (63.5–71.4) | 560 | 57.5 (53.9–61.0) | |
| Mental | 192 | 50.7 (45.1–56.5) | 65 | 65.6 (55.2–75.8) | 127 | 44.8 (38.4–51.7) | |
| Non-complex | 355 | 62.9 (58.4–67.3) | 159 | 68.5 (61.6–75.1) | 196 | 58.6 (52.9–64.5) | |
| Complex | 478 | 67.2 (63.2–71.2) | 241 | 67.4 (61.9–72.8) | 237 | 67.0 (61.2–72.8) | |
| ≥ 1 Planned hospitalization | No LTD | 16,176 | 35.2 (34.7–35.7) | 8,883 | 39.9 (39.2–40.6) | 7,293 | 30.7 (30.0–31.3) |
| LTD | 902 | 54.0 (51.3–56.7) | 412 | 59.9 (55.9–64.0) | 490 | 49.6 (46.1–53.1) | |
| Mental | 155 | 40.9 (35.5–46.7) | 53 | 54.4 (43.8–65.8) | 102 | 35.8 (29.9–42.5) | |
| Non-complex | 314 | 55.0 (50.6–59.6) | 140 | 60.1 (53.2–67.2) | 174 | 51.4 (45.7–57.3) | |
| Complex | 433 | 60.7 (56.6–64.7) | 219 | 61.4 (55.9–67.1) | 214 | 59.7 (53.9–65.6) | |
| ≥ 1 Unplanned hospitalization | No LTD | 6,338 | 13.7 (13.4–14.0) | 3,123 | 13.7 (13.3–14.2) | 3,215 | 13.6 (13.2–14.1) |
| LTD | 367 | 21.8 (19.8–24.0) | 168 | 23.9 (20.8–27.5) | 199 | 20.4 (17.8–23.2) | |
| Mental | 66 | 17.5 (13.9–22.1) | 26 | 27.0 (18.8–37.7) | 40 | 14.0 (10.3–19.0) | |
| Non-complex | 138 | 24.1 (20.7–28.0) | 66 | 28.1 (22.5–34.7) | 72 | 21.2 (17.1–26.1) | |
| Complex | 163 | 22.6 (19.5–26.0) | 76 | 20.4 (16.5–25.0) | 87 | 24.9 (20.4–30.2) | |
| ≥ 1 Hospitalization for an external cause* | No LTD | 3,016 | 6.4 (6.2–6.7) | 663 | 2.8 (2.6–3.0) | 2,353 | 10.0 (9.6–10.4) |
| LTD | 98 | 6.0 (4.9–7.3) | 25 | 3.5 (2.4–5.2) | 73 | 7.8 (6.2–9.8) | |
| Mental | 25 | 6.7 (4.5–9.9) | 5 | 4.4 (1.8–10.5) | 20 | 7.5 (4.8–11.6) | |
| Non-complex | 38 | 7.0 (5.1–9.6) | 9 | 4.2 (2.1–8.1) | 29 | 9.0 (6.3–12.9) | |
| Complex | 35 | 4.9 (3.5–6.8) | 11 | 2.8 (1.5–5.0) | 24 | 7.0 (4.7–10.5) | |
n represents the number of events. Probabilities were estimated by the Kaplan-Meier method. The total number of subjects with ≥ 1 hospitalization is not the sum of numbers with planned and unplanned hospitalizations, because a subject could have both types of hospitalizations during the study period.
*different from a complication of medical or surgical care, allergy, or intoxication by non-psychotropic drugs.
Abbreviations: LTD, long-term disease; 95%CI, 95% confidence interval.
Fig 1. Probability of hospitalizations in short-stay units by gender and long-term disease status between the ages of 14 and 21 years (N = 61,119).
Planned and unplanned hospitalizations
The probability of planned hospitalization by the age of 21 years was also higher for subjects with a LTD than for those without. It was also higher in females than males in both the LTD (59.9% vs. 49.6%, log-rank p-value = 0.001) and no LTD groups (39.9% vs. 30.7%, log-rank p-value <0.0001) (Fig 1B). The probability of unplanned hospitalization of subjects with a LTD was non-significantly higher for females than males (23.9% vs. 20.4%, log-rank p-value = 0.060), whereas it was almost identical between females and males without a LTD (13.7% vs. 13.6% respectively; log-rank p-value = 0.84) (Fig 1C).
The most frequent primary ICD-10 diagnosis for unplanned hospitalizations was “Injury, poisoning, and certain other consequences of external causes” for both males and females with no LTD (20.3% of stays for females, 41.6% for males) and for males with a LTD (17.5%) (S3 Table). The most frequent diagnosis for females with a LTD was “Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified” (16.4%). “Pregnancy, childbirth and the puerperium” represented 14.9% of the stays for females without a LTD and 4.5% for those with a LTD.
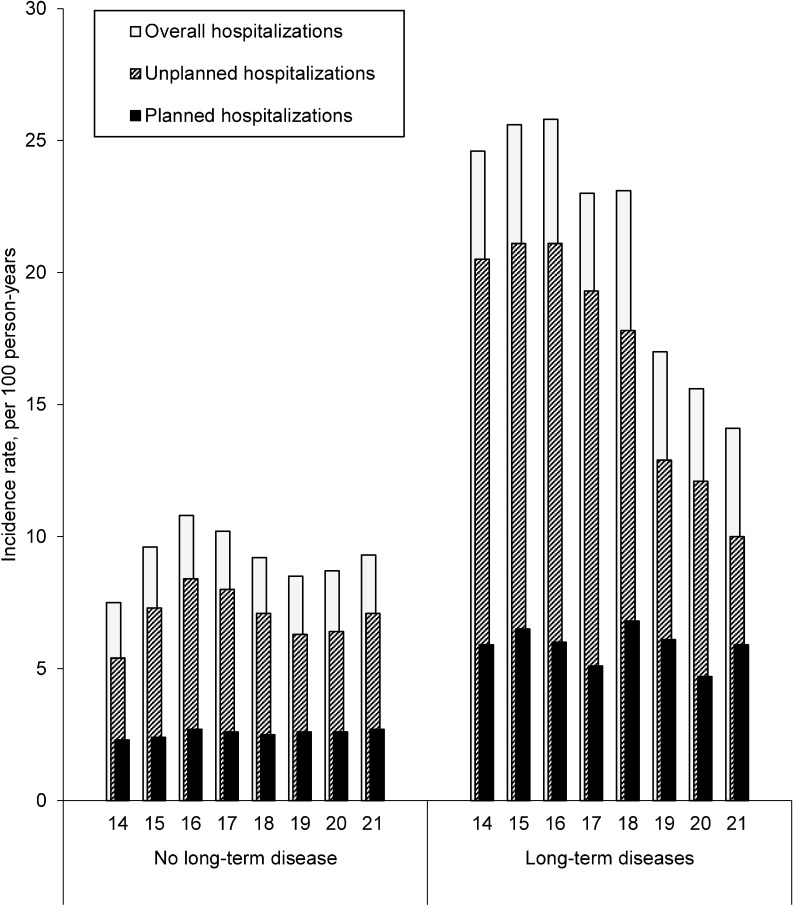
Evolution of hospitalization rates by age
The hospitalization rate for subjects with a LTD remained stable from 14 (24.6 per 100 person-years; 95%CI: 22.2–26.9) to 18 years of age (23.1; 20.2–26.1) and fell sharply at the age of 19 years (17.0; 14.2–19.7) to 14.1 (10.9–17.3) by the age of 21 (Fig 2). This decrease did not occur for subjects with no LTD, for which the rate of hospitalizations was 7.5 (95%CI: 7.2–7.7) at 14, 9.2 (8.9–9.5) at 18, and 9.3 (8.9–9.8) at 21 years of age, per 100 person-years. The overall decrease was the highest for youths with a complex chronic condition (S2 Fig). The fall in the rate at 19 years of age concerned planned, but not unplanned, hospitalizations, which remained stable between the ages of 14 and 21 years.
Fig 2. Evolution of the incidence of hospitalization in short-stay units between 14 and 21 years of age (N = 61,119).
Hospitalization for an external cause
Males in the group with no LTD were approximately 3.5-times more likely than females to be hospitalized for an external cause (10.0% vs. 2.8%; log-rank p-value < 0.0001), whereas the gender difference was smaller in the LTD group (7.8% vs. 3.5%; log-rank p-value < 0.001); p for interaction = 0.033 (Table 3, Fig 1D).
Discussion
This study is the first to provide national estimates for the prevalence of adolescents with a LTD diagnosed before 14 years of age and their mortality and hospitalization rates based on medical data for adolescents living in France.
During the 2005–2014 period, 3.30% (95%CI: 3.16–3.44) of adolescents insured under the French general health insurance scheme had a LTD at 14 years of age. No other national studies have been published concerning the overall prevalence of youths with chronic diseases, except the 2011/2012 household National Survey of Children’s Health [23], which used a very different approach. It was based on parent-reported data and a broad definition of chronic conditions, including, for example, any kind of hearing or speech problems. In our study, the diagnoses of LTDs were double-validated by medical practitioners (the patient’s physician and the health insurance system physician). Based on this medical approach of reporting LTDs, we could focus specifically on chronic diseases that require costly and long-term care, are potentially life-threatening, or lead to handicaps or medical complications.
A strength of this study was the use of a large representative sample of the population insured under the general scheme of the French national health insurance [18], with no selection bias, as the EGB is a random sample with an anonymous procedure that does not require patient agreement. Nevertheless, the prevalence of LTDs may have been slightly underestimated for two reasons. First, some patients have not yet been diagnosed. Second, some patients are eligible for access to free care without requesting LTD registration, but this is unlikely to concern patients with the most severe conditions, who have greater healthcare needs.
A notable strength of our study was the accuracy of mortality estimates, as deaths are exhaustively registered in the French death register. The overall and gender-specific mortality rates were very close to those reported in the French national data.[24]. The mortality rates between the ages of 14 and 21 years for subjects with and without a LTD were 20.9/10,000 person-years (95%CI: 13.7–32.1) and 1.9 (1.5–2.5), respectively. The ten-fold higher mortality rate in adolescents with a LTD was expected given the severity of their diseases. However, it was still very low, even for complex chronic conditions (30.9/10000 person-years; 95%CI; 17.9–53.2). This low mortality rate in adolescents with a LTD may reflect progress in patient medical management, but also the fact that the most severe cases possibly died before the age of 14.
The higher mortality rate of males than females without a LTD is well known and was expected [24]. Mortality in young males in the general population is mostly related to external causes (e.g., trauma), supported by more frequent hospitalizations of males than females among those with no LTD for such causes in our study. This higher risk of external health issues for males reflects a behavioral gender difference in which more adolescent males partake in risky behaviors than females in the general population. Surprisingly, we did not observe such an important gender-gap among youths with a LTD and there was a significant interaction between gender and LTD for both mortality and hospitalization for an external cause. It is possible that adolescent males with a LTD are less exposed to high-risk behaviors related to serious injuries requiring hospitalizations than adolescent males of the general population because of limitations due to their disease. Further research would be needed to address this hypothesis. In addition, we cannot exclude that this result could be explained by a different distribution of more severe diseases between males and females, because detailed analysis by disease was not feasible due to the insufficient number of cases. Similarly, females might have more severe forms of the diseases, either because males with such severe forms died earlier, before 14 years, or because females might be registered for their LTD later. In the coming years, the EGB will include the cause of death, which should allow further investigation of mortality in males and females with a LTD. Stratification by gender is thus needed for any subsequent study on this topic.
Unsurprisingly, the probability of being hospitalized in a short-stay unit between the ages of 14 and 21 was higher for youths with a LTD than those without (61.8% vs. 42.7%). It was not very different or even higher for youths with a non-complex chronic condition than in those with a complex chronic condition, suggesting that non-complex chronic conditions may be very demanding and complex to manage on a daily basis. The classification used here, mainly based on single versus multi-organ diseases, has the advantage of indirectly grouping diseases for which the management is less well-known by specialists of adults, because they are historically pediatric multi-organ and/or rare diseases, whereas medical specialties in adult care are mostly organ-specific. Consequently, it also reflects the difficulty of pediatricians to find specialists in adult care to transfer a young adult patient. Data based on the International Classification of Functioning, Disability, and Health would be more relevant for categorizing patients according to the degree of complexity of their management, but data on activities and daily functioning are not available in the EGB.
We only included short-stay unit hospitalizations, corresponding to non-psychiatric acute health events, and hospitalizations for annual check-up for those with a chronic condition. Long-term stay units are mostly dedicated to rehabilitation and are often preceded by hospitalization in a short-stay unit (e.g., for a surgical intervention). Home-hospitalization concerns mostly dependent elderly patients. Hospitalizations in psychiatric units are not reported here, which may have led to slight underreporting of overall hospitalizations for youths with a chronic mental health condition, not hospitalized in a short-stay unit between the ages of 14 and 21 years. We estimated the one-year probability of overnight hospital stay, i.e., by the age of 15 years in the no LTD group, and found it to be 3.0% (2.8%-3.1%). This probability was quite similar than the probability estimated in a US study, which reported that 2% of 12-17-year-old US teens had experienced at least one overnight hospital stay during the previous 12 months in 2015 [25].
The hospitalization rate was higher in subjects with a LTD than in those without a LTD between the ages of 14 and 21 years and fell sharply at age 19. A decline in the hospitalization rate after 18 years of age among LTD adolescents has already been reported in a Canadian study [15]. However, the decrease for subjects over 18 years of age did not concern hospitalizations through EDs in our study and neither intensive care unit admissions or ED visits in the Canadian study. There may be several reasons for these results. First, healthcare needs may decrease with age for specific diseases, such as asthma, epilepsy, or cured cancers, but this is probably insufficient to explain the sudden fall at 19 years. Second, planned contacts with the healthcare system may decrease with changes in living conditions, as 18 is the age of legal adulthood and the end of secondary school in France. The lack of a decrease in unplanned acute care may reflect delayed regular care. According to the 2007 survey of Adult Transition and Health, adolescents (14–17 years) with special healthcare needs received significantly less timely healthcare as they aged into adulthood (19–23 years) [16]. Third, changes may be related to transfer to adult-oriented care, potentially associated with a lower frequency of medical visits [26,27], gaps in care [28], a lack of compliance with treatment regimens [29,30], or different practices between pediatricians and adult specialists (inpatient versus outpatient care, respectively). Scientific data on this topic are inconsistent [31–33]. We could not explore this issue, as data on the specialty of the department of hospitalization was not available in the French national health insurance database during the study period. However, access to care could be studied in a future analysis by considering data on outpatient care and consultations with private physicians, which are available in the EGB. This could help to determine whether there is a discontinuity in patient care or a transition from inpatient care to outpatient care when the patients become young adults.
Conclusions
This study provides reference epidemiological data on youths living with a LTD in a country that aims to offer free and universal access to healthcare [34]. Approximately 3% of 14-year-old youths had a LTD. Elevated risks have been evaluated in detail for the first time in this population, in terms of mortality patterns and trends in hospitalization rates. Unexpectedly, the rate of planned hospitalization fell after age 18, the age of legal adulthood. This raises many issues, including coping strategies of young patients in high-risk situations and the role of transfer to adult care on patient behavior, prognosis, and clinical practices.
Supporting information
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We warmly thank Dr Lise Duranteau for her review of the manuscript.
Data Availability
The authors are restricted from sharing the data underlying this study because publicly sharing EGB data is forbidden by law according to The French national data protection agency (Commission Nationale de l’Informatique et des LIbertés, CNIL); regulatory decisions AT/CPZ/SVT/JB/DP/CR05222O of June 14, 2005 and DP/CR071761 of August 28, 2007. To request data access please contact The National Institute for Health Data (Institut National des Données de Santé, INDS) (website: http://www.indsante.fr/).
Funding Statement
The authors received no specific funding for this work.
References
- 1.UK CF Registry. Annual Data Report 2008. Cystic Fibrosis Trust; 2009.
- 2.Burgel P-R, Bellis G, Olesen HV, Viviani L, Zolin A, Blasi F, et al. Future trends in cystic fibrosis demography in 34 European countries. Eur Respir J. 2015;46: 133–141. doi: 10.1183/09031936.00196314 [DOI] [PubMed] [Google Scholar]
- 3.Moons P, Bovijn L, Budts W, Belmans A, Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. 2010;122: 2264–2272. doi: 10.1161/CIRCULATIONAHA.110.946343 [DOI] [PubMed] [Google Scholar]
- 4.Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115: 3447–3452. doi: 10.1182/blood-2009-07-233700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hazra R, Siberry GK, Mofenson LM. Growing up with HIV: children, adolescents, and young adults with perinatally acquired HIV infection. Annu Rev Med. 2010;61: 169–185. doi: 10.1146/annurev.med.050108.151127 [DOI] [PubMed] [Google Scholar]
- 6.Michaud P-A, Suris JC, Viner R. The adolescent with a chronic condition: epidemiology, developmental issues and health care provision [Internet]. World Health Organization; 2007. Available: http://apps.who.int/iris/bitstream/10665/43775/1/9789241595704_eng.pdf [Google Scholar]
- 7.Bauman ME, Kuhle S, Bruce A a. K, Bolster L, Massicotte MP. The journey for adolescents and young adults with chronic conditions transitioning to adult care with successful warfarin management. Thromb Res. 2016;141: 183–188. doi: 10.1016/j.thromres.2016.03.019 [DOI] [PubMed] [Google Scholar]
- 8.Javalkar K, Johnson M, Kshirsagar AV, Ocegueda S, Detwiler RK, Ferris M. Ecological Factors Predict Transition Readiness/Self-Management in Youth With Chronic Conditions. J Adolesc Health Off Publ Soc Adolesc Med. 2016;58: 40–46. doi: 10.1016/j.jadohealth.2015.09.013 [DOI] [PubMed] [Google Scholar]
- 9.van Staa A, van der Stege HA, Jedeloo S, Moll HA, Hilberink SR. Readiness to transfer to adult care of adolescents with chronic conditions: exploration of associated factors. J Adolesc Health Off Publ Soc Adolesc Med. 2011;48 doi: 10.1016/j.jadohealth.2010.07.009 [DOI] [PubMed] [Google Scholar]
- 10.Zhang LF, Ho JSW, Kennedy SE. A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatr. 2014;14: 4 doi: 10.1186/1471-2431-14-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mann JR, Royer JA, Mcdermott S, Hardin JW, Ozturk O, Street N. Hospitalizations and emergency room visits for adolescents and young adults with muscular dystrophy living in South Carolina. Muscle Nerve. 2015;52: 714–721. doi: 10.1002/mus.24599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mann JR, Royer JA, Turk MA, McDermott S, Holland MM, Ozturk OD, et al. Inpatient and emergency room visits for adolescents and young adults with spina bifida living in South Carolina. PM R. 2015;7: 499–511. doi: 10.1016/j.pmrj.2014.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shankar SM, Arbogast PG, Mitchel E, Cooper WO, Wang WC, Griffin MR. Medical care utilization and mortality in sickle cell disease: a population-based study. Am J Hematol. 2005;80: 262–270. doi: 10.1002/ajh.20485 [DOI] [PubMed] [Google Scholar]
- 14.Hemker BG, Brousseau DC, Yan K, Hoffmann RG, Panepinto JA. When children with sickle-cell disease become adults: lack of outpatient care leads to increased use of the emergency department. Am J Hematol. 2011;86: 863–865. doi: 10.1002/ajh.22106 [DOI] [PubMed] [Google Scholar]
- 15.Cohen E, Gandhi S, Toulany A, Moore C, Fu L, Orkin J, et al. Health Care Use During Transfer to Adult Care Among Youth With Chronic Conditions. Pediatrics. 2016;137: 1–9. doi: 10.1542/peds.2015-2734 [DOI] [PubMed] [Google Scholar]
- 16.Okumura MJ, Hersh AO, Hilton JF, Lotstein DS. Change in health status and access to care in young adults with special health care needs: results from the 2007 national survey of adult transition and health. J Adolesc Health Off Publ Soc Adolesc Med. 2013;52: 413–418. doi: 10.1016/j.jadohealth.2012.08.005 [DOI] [PubMed] [Google Scholar]
- 17.Berry JG, Rodean J, Hall M, Alpern ER, Aronson PL, Freedman SB, et al. Impact of Chronic Conditions on Emergency Department Visits of Children Using Medicaid. J Pediatr. 2017;182: 267–274. doi: 10.1016/j.jpeds.2016.11.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuppin P, Rudant J, Constantinou P, Gastaldi-Ménager C, Rachas A, de Roquefeuil L, et al. Value of a national administrative database to guide public decisions: From the système national d’information interrégimes de l’Assurance Maladie (SNIIRAM) to the système national des données de santé (SNDS) in France. Rev Epidemiol Sante Publique. 2017; doi: 10.1016/j.respe.2017.05.004 [DOI] [PubMed] [Google Scholar]
- 19.Duflos CM, Solecki K, Papinaud L, Georgescu V, Roubille F, Mercier G. The Intensity of Primary Care for Heart Failure Patients: A Determinant of Readmissions? The CarPaths Study: A French Region-Wide Analysis. PLOS ONE. 2016;11: e0163268 doi: 10.1371/journal.pone.0163268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weill A, Dalichampt M, Raguideau F, Ricordeau P, Blotière P-O, Rudant J, et al. Low dose oestrogen combined oral contraception and risk of pulmonary embolism, stroke, and myocardial infarction in five million French women: cohort study. BMJ. 2016;353: i2002 doi: 10.1136/bmj.i2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blin P, Dureau-Pournin C, Foubert-Samier A, Grolleau A, Corbillon E, Jové J, et al. Parkinson’s disease incidence and prevalence assessment in France using the national healthcare insurance database. Eur J Neurol. 2015;22: 464–471. doi: 10.1111/ene.12592 [DOI] [PubMed] [Google Scholar]
- 22.Bouée S, Emery C, Samson A, Gourmelen J, Bailly C, Cotté F-E. Incidence of venous thromboembolism in France: a retrospective analysis of a national insurance claims database. Thromb J. 2016;14: 4 doi: 10.1186/s12959-016-0078-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Data resource center for child and adolescent health [Internet]. [cited 31 Aug 2016]. Available: http://www.childhealthdata.org/
- 24.Mortality rates by sex and age in 2014. In: Ined—Institut national d’études démographiques [Internet]. [cited 9 Aug 2016]. Available: https://www.ined.fr/fr/tout-savoir-population/chiffres/france/mortalite-cause-deces/taux-mortalite-sexe-age/
- 25.Summary Health Statistics: National Health Interview Survey, 2015. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2015.
- 26.Gleeson H, Davis J, Jones J, O’Shea E, Clayton PE. The challenge of delivering endocrine care and successful transition to adult services in adolescents with congenital adrenal hyperplasia: experience in a single centre over 18 years. Clin Endocrinol (Oxf). 2013;78: 23–28. doi: 10.1111/cen.12053 [DOI] [PubMed] [Google Scholar]
- 27.Busse FP, Hiermann P, Galler A, Stumvoll M, Wiessner T, Kiess W, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67: 132–138. doi: 10.1159/000096583 [DOI] [PubMed] [Google Scholar]
- 28.Rachas A, Lefeuvre D, Meyer L, Faye A, Mahlaoui N, de La Rochebrochard E, et al. Evaluating Continuity During Transfer to Adult Care: A Systematic Review. Pediatrics. 2016;138 doi: 10.1542/peds.2016-0256 [DOI] [PubMed] [Google Scholar]
- 29.Akchurin OM, Melamed ML, Hashim BL, Kaskel FJ, Del Rio M. Medication adherence in the transition of adolescent kidney transplant recipients to the adult care. Pediatr Transplant. 2014;18: 538–548. doi: 10.1111/petr.12289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatr Transplant. 2007;11: 608–614. doi: 10.1111/j.1399-3046.2007.00689.x [DOI] [PubMed] [Google Scholar]
- 31.Bollegala N, Brill H, Marshall JK. Resource utilization during pediatric to adult transfer of care in IBD. J Crohns Colitis. 2013;7 doi: 10.1016/j.crohns.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 32.Samuel SM, Nettel-Aguirre A, Soo A, Hemmelgarn B, Tonelli M, Foster B. Avoidable hospitalizations in youth with kidney failure after transfer to or with only adult care. Pediatrics. 2014;133: e993–1000. doi: 10.1542/peds.2013-2345 [DOI] [PubMed] [Google Scholar]
- 33.McPheeters M, Davis AM, Taylor JL, Brown RF, Potter SA, Epstein RA. Transition Care for Children With Special Health Needs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2014. Available: http://www.ncbi.nlm.nih.gov/books/NBK222123/ [PubMed] [Google Scholar]
- 34.Horton R, Ceschia A. France: a philosophy for health. The Lancet. 2016;387: 2174–2176. doi: 10.1016/S0140-6736(16)30243-4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
The authors are restricted from sharing the data underlying this study because publicly sharing EGB data is forbidden by law according to The French national data protection agency (Commission Nationale de l’Informatique et des LIbertés, CNIL); regulatory decisions AT/CPZ/SVT/JB/DP/CR05222O of June 14, 2005 and DP/CR071761 of August 28, 2007. To request data access please contact The National Institute for Health Data (Institut National des Données de Santé, INDS) (website: http://www.indsante.fr/).