Abstract
BACKGROUND:
Primary care networks are designed to facilitate access to inter-professional, team-based care. We compared health outcomes associated with primary care networks versus conventional primary care.
METHODS:
We obtained data on all adult residents of Alberta who visited a primary care physician during fiscal years 2008 and 2009 and classified them as affiliated with a primary care network or not, based on the physician most involved in their care. The primary outcome was an emergency department visit or nonelective hospital admission for a Patient Medical Home indicator condition (asthma, chronic obstructive pulmonary disease, heart failure, coronary disease, hypertension and diabetes) within 12 months.
RESULTS:
Adults receiving care within a primary care network (n = 1 502 916) were older and had higher comorbidity burdens than those receiving conventional primary care (n = 1 109 941). Patients in a primary care network were less likely to visit the emergency department for an indicator condition (1.4% v. 1.7%, mean 0.031 v. 0.035 per patient, adjusted risk ratio [RR] 0.98, 95% confidence interval [CI] 0.96–0.99) or for any cause (25.5% v. 30.5%, mean 0.55 v. 0.72 per patient, adjusted RR 0.93, 95% CI 0.93–0.94), but were more likely to be admitted to hospital for an indicator condition (0.6% v. 0.6%, mean 0.018 v. 0.017 per patient, adjusted RR 1.07, 95% CI 1.03–1.11) or all-cause (9.3% v. 9.1%, mean 0.25 v. 0.23 per patient, adjusted RR 1.08, 95% CI 1.07–1.09). Patients in a primary care network had 169 fewer all-cause emergency department visits and 86 fewer days in hospital (owing to shorter lengths of stay) per 1000 patient-years.
INTERPRETATION:
Care within a primary care network was associated with fewer emergency department visits and fewer hospital days.
In Alberta, primary care networks were established in 2005 to help facilitate both access to primary care and adoption of the Patient Medical Home model of care, which focuses on chronic disease management, health maintenance and prevention. 1,2 Although there is no one structure for primary care networks (varying from one co-located clinic to several offices in a geographic area), Alberta Health Services provides funding to each network ($50 per patient in 2008; $62 per patient in 2017 in addition to the usual fee-for-service payments to the physicians) for the hire of nonphysician health care providers to help provide coordinated primary health care to a roster of patients. This additional funding cannot be used to support the implementation of electronic medical records — that is the remit of other programs in Alberta that are not tied into participating in primary care networks. Primary care networks vary in the deployment of their nonphysician funding and the frequency with which nonphysician providers see patients. Further details are available at www.health.alberta.ca/services/primary-care-networks.html (last accessed Aug. 31, 2017). Primary care network involvement is voluntary; in 2017, more than 80% of primary care physicians in Alberta were affiliated with a primary care network.
The impact of primary care teams on health care utilization is uncertain, with published reports showing benefits that range from negligible3–9 to very modest.1,2,10–13 An early evaluation of the first wave of Alberta primary care networks reported that individuals with newly diagnosed diabetes had better glycemic control and lower rates of emergency department visits or hospital admissions for hyper- or hypoglycemia in 2007 if treated in 1 of the 18 primary care networks at that time.1 However, the benefits were small: glycated hemoglobin (HbA1C) was 0.07 lower and the absolute reduction in emergency department visits or hospital admissions was 0.7 per 1000 patient-months. It is unknown whether benefits would accrue for patients with other chronic diseases managed within primary care networks or whether the improvements would be seen when the primary care networks rolled out beyond the early adopters (who may well practise differently than others).
We designed this study to examine whether patients of primary care networks had fewer visits to the emergency department and acute care hospital admissions than patients cared for by primary care physicians who are not affiliated with a primary care network (“conventional primary care”). We explored all-cause visits or hospital admissions, but also focused on those conditions where primary care is felt to have potentially the greatest impact on patients’ health status: asthma, chronic obstructive pulmonary disease, heart failure, coronary disease, hypertension and diabetes (hereafter referred to as Patient Medical Home indicator conditions).14
Methods
Design and setting
Alberta has a government-funded health care system that provides more than 4.4 million people with universal access to hospital, emergency department and physician services and is free at the point of care. In this prospective cohort study, we focused on the fiscal years 2008 and 2009, being the period when approximately half of Alberta primary care physicians were affiliated with primary care networks.
Data sources
This study used the Discharge Abstract Database, which records the admission date, discharge date, most responsible diagnosis and up to 24 other diagnoses for all acute care hospital admissions; the Ambulatory Care Database, which records all patient visits to the offices of hospital-based physicians or to emergency departments, with coding for of up to 10 conditions, including the most responsible diagnosis; the Physician Claims Database, which tracks all physician claims for outpatient services and includes up to 3 diagnoses per encounter; and the Alberta Health Care Insurance Registry.
Study cohort and identification of exposure
We identified all Albertans aged 20 years or older who were seen by a primary care physician at least once in fiscal years 2008 or 2009. We stratified them into affiliation with a primary care network or not, based on the physician who provided most of their outpatient primary care in the 2 years of the study. Alberta Health renews its list of physicians affiliated with a primary care network each fiscal year. We assigned each patient an index date (their first visit to a primary care physician during the study period) and analyzed all events in the first year after the index date.
Covariates
We used International Classification of Diseases, 9th Revision (ICD-9) and 10th Revision (ICD-10) codes from the Discharge Abstract Database for any hospital admissions, any emergency department visits and any outpatient visits in the 2 years before the index visit, to identify comorbidities. The validity of diagnoses captured in these data sets using 2 hits in the outpatient or emergency department records or 1 hit in the Discharge Abstract Database has been established in Alberta.15,16
Outcomes
Our primary outcome was the proportion of patients having an emergency department visit or hospital admission for nonelective acute care for a most responsible diagnosis linked to any of the Patient Medical Home indicator conditions (Appendix 1, available at www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.170385/-/DC1) — these are the same as the Ambulatory Care Sensitive Conditions defined by the Canadian Institute for Health Information, but do not include epilepsy. Secondary outcomes included the proportion of patients with an all-cause emergency department visit or hospital admission, the individual components of the primary outcome, hospital length of stay for those hospitalized, 30-day readmission rates after hospital discharge and 30-day repeat emergency department visits, using previously published definitions.17 All events for each patient were counted, but visits to the emergency department that resulted in a hospital admission during the same encounter or transfers between emergency departments or hospitals in the same episode of care were counted as only 1 event.
In order to further explore rates of readmission to hospital, emergency department visits, or death for patients who were recently admitted to hospital and who were actively engaged with their primary care physician, we conducted a sensitivity analysis for those patients who had been discharged within 90 days of their index visit to a physician as an outpatient. This cohort was divided into 3 risk groups based on their comorbidity level (a summary score based on clinical risk groupings for all hospital admissions in the previous year). Low-risk groups are defined as those with a total comorbidity factor of 0%–24%; moderate-risk groups with comorbidity scores of 25%–50%; and high-risk groups as those with > 50% comorbidity levels in the Canadian Institute for Health Information Discharge Abstract Database file.
Statistical analyses
We compared patient baseline characteristics and examined the association between care through a primary care network and outcomes using a series of zero-inflated Poisson models with total emergency department utilization and hospital admission for Patient Medical Home indicator conditions and all causes. Additionally, we created a series of logistic regression models for the individual indicator conditions. In the first set of models for each analysis, the covariates we adjusted for included age, sex and all of the clinical comorbidities listed in Table 1. In the second set of models, we included health system factors including the number of visits with a primary care physician, the geographic zone in which the primary care network was situated (the province is divided into 5 zones within Alberta Health Services) and socioeconomic factors (whether the patient had a rural or urban residence and the postal code–based Pampalon material and social deprivation index: www.cihi.ca/en/deprivation-in-canadian-cities-an-analytical-tool, last accessed Aug. 31, 2017).18
Table 1:
Characteristics of patients cared for by primary care physicians in Alberta 2008–2010
| Characteristic | No. of patients in a primary care network* (%)† n = 1 502 916 |
No. of patients in conventional primary care (%)† n = 1 109 940 |
Standardized difference‡ |
|---|---|---|---|
| Age, mean ± SD | 46.1 ± 18.4 | 44.0 ± 19.5 | −0.11 |
| Male | 684 482 (45.4) | 548 047 (49.4) | 0.08 |
| Rural residence | 218 064 (14.51) | 174 291 (15.70) | 0.03 |
| Charlson Comorbidity Index score, mean ± SD | 0.34 ± 1.01 | 0.32 ± 1.02 | −0.02 |
| Median number of physician visits in previous year (IQR) | 3 (1–6) | 2 (1–6) | −0.08 |
| Patient Medical Home indicator conditions | |||
| Diabetes | 85 857 (5.71) | 57 409 (5.17) | −0.02 |
| Heart failure | 14 134 (0.94) | 10 148 (0.91) | 0.00 |
| Hypertension | 219 082 (14.58) | 140 726 (12.68) | −0.06 |
| Chronic obstructive pulmonary disease | 87 324 (5.81) | 62 008 (5.60) | −0.01 |
| Asthma | 47 554 (3.16) | 32 035 (2.89) | −0.02 |
| Coronary artery disease (previous myocardial infarction, coronary artery bypass graft, percutaneous intervention, or chronic angina) | 23 029 (1.53) | 15874 (1.43) | −0.02 |
| Other chronic conditions | |||
| Anemia | 36 314 (2.42) | 24 056 (2.17) | −0.02 |
| Cerebrovascular disease | 15 957 (1.06) | 10 746 (0.97) | −0.01 |
| Renal disease | 9803 (0.65) | 7458 (0.67) | 0.00 |
| Cancer | 16 611 (1.11) | 11 797 (1.06) | 0.00 |
| Peripheral vascular disease | 9004 (0.60) | 5681 (0.51) | −0.01 |
| Dementia | 10 015 (0.67) | 6664 (0.60) | −0.01 |
| Atrial fibrillation | 28 644 (1.91) | 15 752 (1.42) | −0.04 |
| Cardiogenic shock | 17 621 (1.17) | 8217 (0.74) | −0.04 |
| Stroke | 12 850 (0.86) | 8547 (0.77) | −0.01 |
| Pneumonia | 24 818 (1.65) | 18 674 (1.68) | 0.00 |
| Protein calorie malnutrition | 507 (0.03) | 281 (0.03) | 0.00 |
| Hemiparesis or paralysis | 3752 (0.25) | 2866 (0.26) | 0.00 |
| Solid tumour | 4527 (0.30) | 4082 (0.37) | 0.01 |
| Trauma | 286 012 (19.03) | 221 549 (19.96) | 0.02 |
| Psychiatric disorder | 224 109 (14.91) | 141 004 (12.70) | −0.06 |
| Severe liver disease | 1210 (0.08) | 1032 (0.09) | 0.00 |
| Fluid imbalance | 21 603 (1.44) | 15 920 (1.43) | 0.00 |
| Skin ulcer | 2658 (0.18) | 1669 (0.15) | 0.01 |
| Gastrointestinal bleed | 8727 (0.58) | 5927 (0.53) | −0.01 |
| Nephritis | 6458 (0.43) | 5141 (0.46) | 0.01 |
| Nonmetastatic cancer | 24 096 (1.60) | 15 855 (1.43) | −0.01 |
| Drug abuse | 24 292 (1.62) | 22 990 (2.07) | 0.03 |
| Depression | 174 485 (11.61) | 107 348 (9.67) | −0.06 |
| Arthritis | 15 172 (1.01) | 9315 (0.84) | −0.02 |
| HIV | 712 (0.05) | 576 (0.05) | 0.00 |
| Pampalon Material Deprivation Index quintiles,§ % | 0.18 | ||
| 1 | 16.87 | 21.26 | |
| 2 | 16.33 | 20.66 | |
| 3 | 19.38 | 19.07 | |
| 4 | 20.28 | 17.65 | |
| 5 (most deprived) | 22.56 | 17.93 | |
| Pampalon Social Deprivation Index quintiles,¶ % | 0.07 | ||
| 1 | 12.92 | 16.23 | |
| 2 | 15.88 | 17.32 | |
| 3 | 19.26 | 19.77 | |
| 4 | 23.56 | 23.05 | |
| 5 (most deprived) | 23.77 | 20.2 | |
Note: HIV = human immunodeficiency virus, IQR = interquartile range, SD = standard deviation.
Patients seen by a physician affiliated with a primary care network.
Unless otherwise specified.
Standardized differences greater than 0.1 are considered clinically meaningful.
Pampalon Material Deprivation Index — reflects the deprivation of goods and conveniences. Includes the following indicators: average household income, unemployment rate and high school education rate.18
Pampalon Social Deprivation Index — reflects the deprivation of relationships among individuals in the family, the workplace and the community. Includes the following indicators: proportion of the population separated, divorced or widowed; proportion of the population that lives alone; and proportion of the population that has moved in the past 5 years.18
We accounted for clustering within primary care networks by incorporating the primary care network identification number as a random-effect variable. We also conducted a sensitivity analysis in which we included only patients with at least 2 visits to a primary care physician in the previous year and we compared results in the 2 cohorts (primary care network v. conventional primary care) matched by age, sex and geographic zone and Charlson Comorbidity Index score. As we did not have information on date of death (only whether a patient was alive or not during each fiscal year), we explored the impact of mortality as a competing risk by conducting a sensitivity analysis that excluded any patients who had died or emigrated during the study period.
Ethics approval
This retrospective cohort study received ethics approval from the University of Alberta (Pro00048445) with a waiver of informed consent because we were using de-identified data.
Results
In fiscal years 2008 and 2009, there were 30 primary care networks in Alberta involving 1709 physicians with 2 257 111 patients on their rosters: 1 502 916 Albertan adults received outpatient care from a primary care physician affiliated with a primary care network, and 1 109 941 received conventional primary care. Patients in a primary care network were older (46 v. 44 yr), had more chronic conditions, had higher comorbidity burdens and saw their primary care physician more frequently (Table 1).
Patients receiving outpatient care from physicians affiliated with a primary care network were less likely to present to an emergency department for any cause (25.5% v. 30.5%, absolute risk difference 5.0%, number needed to treat 20; mean emergency department visits 0.55 v. 0.72 per patient; both p < 0.001) or for an indicator condition (1.4% v. 1.7%, mean emergency department visits 0.03 v. 0.04 per patient, both p < 0.001).
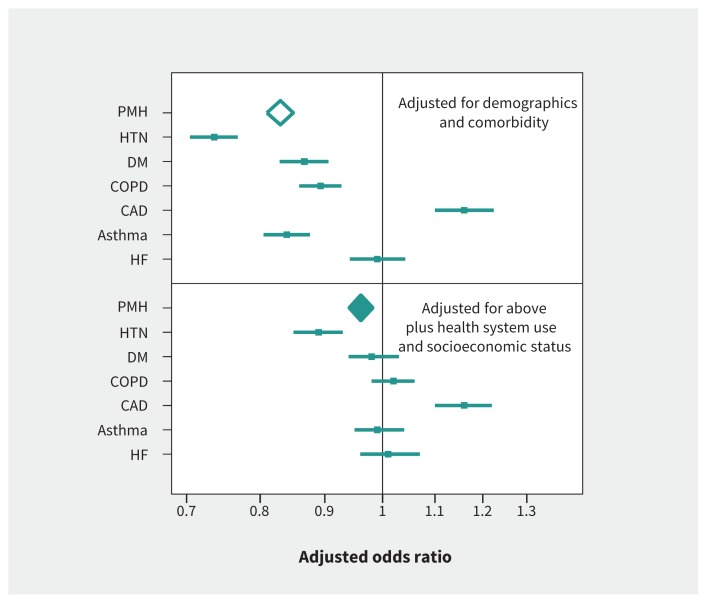
Adjusting for socioeconomic status and health system factors (frequency of visits, rural or urban residence, health authority zone) in the Poisson models (in addition to patient demographics and clinical covariates) resulted in less pronounced but still significant associations between primary care network affiliation and lower risk of emergency department visits for any cause or for indicator conditions (Table 2). Similar significant associations were also seen in the matched cohort analysis. Including “outpatient visits with an internal medicine specialist” did not alter the magnitude of the associations (data not shown). The association between receiving care from a physician affiliated with a primary care network and lower rates of visits to emergency departments or hospital admissions was significant for 4 of the indicator conditions in the multivariable model adjusting for demographics and clinical comorbidities, but in only 2 (lower for hypertension, higher for coronary artery disease) after also adjusting for health system use and socioeconomic status (Figure 1).
Table 2:
Twelve-month outcomes for patients cared for by primary care physicians in Alberta 2008–2010
| Outcomes | No. of events in patients in a primary care network* n = 1 502 916 |
No. of events in patients in conventional primary care n = 1 109 940 |
Crude RR (95% CI) | Clinically adjusted RR† (95% CI) | Fully adjusted RR‡ (95% CI) | Matched§ cohort analysis with conditional RR (95% CI) |
|---|---|---|---|---|---|---|
| Emergency department visit | ||||||
| Patient Medical Home indicator conditions | n = 1 502 916 | n = 1 109 940 | ||||
| Patients with event | 21 655 (1.4%) | 18 830 (1.7%) | ||||
| Total events | 29 679 | 26 160 | 0.83 (0.81–0.85) | 0.89 (0.88–0.90) | 0.98 (0.96–0.99) | 0.87 (0.86–0.89) |
| Mean per patient | 0.031 | 0.035 | ||||
| All-cause | n = 1 502 916 | n = 1 109 940 | ||||
| Patients with event | 382 819 (25.5%) | 337 983 (30.5%) | ||||
| Total events | 830 260 | 800 039 | 0.81 (0.80–0.81) | 0.84 (0.83–0.84) | 0.93 (0.93–0.94) | 0.83 (0.83–0.83) |
| Mean per patient | 0.55 | 0.72 | ||||
| Hospital admission | ||||||
| Patient Medical Home indicator conditions | n = 1 502 916 | n = 1 109 940 | ||||
| Patients with event | 8557 (0.57%) | 6876 (0.62%) | ||||
| Total events | 11 072 | 8769 | 1.07 (1.03–1.10) | 0.93 (0.90–0.96) | 1.07 (1.03–1.11) | 0.95 (0.92–0.98) |
| Mean per patient | 0.018 | 0.017 | ||||
| All-cause | n = 1 502 916 | n = 1 109 940 | ||||
| Patients with event | 139 394 (9.3%) | 101 068 (9.1%) | ||||
| Total events | 155 631 | 121 929 | 1.06 (1.05–1.07) | 0.98 (0.97–0.99) | 1.08 (1.07–1.09) | 1.11 (1.10–1.12) |
| Mean per patient | 0.25 | 0.23 | ||||
| After excluding patients who died or emigrated from Alberta during the study period | ||||||
| Emergency department visit | ||||||
| Patient Medical Home indicator conditions | n = 1 466 259 | n = 1 067 579 | ||||
| Patients with event | 19 171 (1.3%) | 16 444 (1.5%) | ||||
| Total events | 25 625 | 22 384 | 0.90 (0.88–092) | 0.81 (0.79–0.82) | 0.96 (0.94–0.99) | 0.86 (0.84–0.88) |
| Mean per patient | 0.025 | 0.031 | ||||
| All-cause | n = 1 466 259 | n = 1 067 579 | ||||
| Patients with event | 366 475 (25%) | 319 750 (30.0%) | ||||
| Total events | 783 994 | 749 799 | 0.84 (0.84–0.84) | 0.78 (0.77–0.79) | 0.92 (0.92–0.93) | 0.81 (0.80–0.81) |
| Mean per patient | 0.53 | 0.70 | ||||
| Hospital admission | ||||||
| Patient Medical Home indicator conditions | n = 1 466 259 | n = 1 067 579 | ||||
| Patients with event | 6797 (0.5%) | 5116 (0.5%) | ||||
| Total events | 8248 | 6238 | 1.10 (1.05–1.14) | 0.90 (0.87–0.94) | 1.04 (1.00–1.09) | 1.00 (0.96–1.04) |
| Mean per patient | 0.014 | 0.012 | ||||
| All-cause | n = 1 466 259 | n = 1 067 579 | ||||
| Patients with event | 127 933 (8.7%) | 88 885 (8.3%) | ||||
| Total events | 135 284 | 101 762 | 1.09 (1.08–1.10) | 0.99 (0.99–1.00) | 1.08 (1.07–1.10) | 1.11 (1.10–1.12) |
| Mean per patient | 0.22 | 0.20 | ||||
Note: CI = confidence interval, RR = risk ratio.
Patients seen by a physician affiliated with a primary care network.
RR adjusted for patient demographics and clinical comorbidities.
RR adjusted for patient demographics, comorbidities, number of visits, socioeconomic status and geographic zone.
Matched on age, sex, Charlson Comorbidity Index score and geographic zone, and restricted to patients with 2 or more visits per year.
Figure 1:
Association between affiliation with a primary care network and health care utilization (emergency department visits or hospital admissions) for Patient Medical Home indicator conditions as the most responsible diagnosis. Comorbidity adjustment was for the Charlson Comorbidity Index score. Note: CAD = coronary artery disease, COPD = chronic obstructive pulmonary disease, DM = diabetes mellitus, HF = heart failure, HTN = hypertension, PMH = Patient Medical Home indicator conditions.
Hospital admissions were more likely for patients in a primary care network, both for indicator conditions (0.6% v. 0.6%, and mean 0.018 v. 0.017 per patient, adjusted risk ratio [RR] 1.07, 95% confidence interval [CI] 1.03–1.11) and for any cause (9.3% v. 9.1%, mean 0.25 v. 0.23 per patient, adjusted RR 1.08, 95% CI 1.07–1.09). This excess risk persisted even after excluding patients who had died during the study period (4.7% of those cared for by physicians affiliated with a primary care network and 8.4% of those cared for in conventional primary care) and those who emigrated out of province during the study period (1.3% and 2.0%, respectively). All-cause hospital admissions (adjusted RR 1.11, 95% CI 1.10–1.12) remained significantly higher for patients in a primary care network, and all-cause emergency department visits remained significantly lower (adjusted RR 0.96, 95% CI 0.95–0.96).
The number of days in hospital (986 v. 1072, p < 0.0001) and the number of emergency department visits (552 v. 721, p < 0.0001) per 1000 patient-years were significantly lower for patients in a primary care network. Mean length of stay for patients in hospital (6.99 v. 7.52 d, p = 0.001), mean inpatient cost per patient ($1102 v. $1254, p = 0.001), 30-day readmissions (7.8% v. 9.0%, adjusted odds ratio [OR] 0.86 [95% CI 0.83–8.88]), and repeat emergency department visits within 30 days (24.5% v. 29.1%, adjusted OR 0.79 [0.78–0.80]) were all lower for patients in a primary care network. Restricting this analysis to only those patients who had been admitted to hospital within 90 days of their index visit to primary care as an outpatient confirmed that 30-day rates of readmission or mortality (4.1% v. 6.3%, adjusted OR 0.64, 95% CI 0.60–0.68) or emergency department visits (43.3% v. 46.8%, adjusted OR 0.94, 95% CI 0.92–0.97) were lower for patients actively engaged with a primary care network, with the magnitude of difference being greatest for patients with more comorbidities (Table 3).
Table 3:
Thirty-day outcomes of patients seeing a primary care physician in Alberta 2008–2010 within 90 days of hospital discharge
| Characteristic | No. of patients in a primary care network* (%)† | No. of patients in conventional primary care (%)† | Adjusted OR (95% CI)‡ |
|---|---|---|---|
| All patients | n = 41 056 | n = 57 087 | |
| 30 d readmission or death | 2351 (4.1) | 2606 (6.3) | 0.64 (0.60–0.68) |
| 30 d readmission | 2331 (4.1) | 2420 (5.9) | 0.70 (0.65–0.74) |
| 30 d death after discharge | 45 (0.1) | 444 (1.1) | 0.07 (0.05–0.09) |
| 30 d ED visit after discharge | 24 721 (43.3) | 19 206 (46.78) | 0.94 (0.92–0.97) |
| Patients with the highest comorbidity load (> 50%) | n = 4268 (7.5) | n = 3556 (8.7) | |
| 30 d readmission or death | 378 (8.9) | 499 (14.0) | 0.59 (0.51–0.68) |
| 30 d readmission | 367 (8.6) | 429 (12.1) | 0.69 (0.59–0.80) |
| 30 d death after discharge | 16 (0.4) | 153 (4.3) | 0.08 (0.05–0.13) |
| 30 d ED visit after discharge | 2257 (52.9) | 1943 (54.6) | 0.98 (0.89–1.07) |
| Patients with 25%–50% comorbidity load | n = 4580 (8.0) | n = 3654 (8.9) | |
| 30 d readmission or death | 300 (6.6) | 339 (9.3) | 0.67 (0.57–0.79) |
| 30 d readmission | 298 (6.5) | 312 (8.5) | 0.73 (0.62–0.87) |
| 30 d death after discharge | 8 (0.2) | 77 (2.1) | 0.08 (0.04–0.16) |
| 30 d ED visit after discharge | 2292 (50.0) | 1872 (51.3) | 1.00 (0.92–1.10) |
| Patients with the lowest comorbidity load (< 25%) | n = 48 239 (84.5) | n = 33 846 (82.4) | |
| 30 d readmission or death | 1673 (3.5) | 1768 (5.2) | 0.67 (0.62–0.72) |
| 30 d readmission | 1666 (3.5) | 1679 (5.0) | 0.71 (0.66–0.76) |
| 30 d death after discharge | 21 (0.04) | 214 (0.6) | 0.07 (0.04–0.10) |
| 30 d ED visit after discharge | 20 172 (41.8) | 15 391 (45.5) | 0.93 (0.91–0.93) |
Note: CI = confidence interval, ED = emergency department, OR = odds ratio.
Patients seen by a physician affiliated with a primary care network.
Unless otherwise specified.
Adjusted for age, sex, Charlson Comorbidity Index score, socioeconomic status and geographic zone.
Of the emergency department visits, most (56.7% for patients in a primary care network and 55.9% for patients in conventional primary care) occurred outside of normal working hours (08:00–17:00 Monday to Friday). The association between affiliation with a primary care network and lower emergency department visit rates was similar whether looking at after-office hours (RR 0.80, 95% CI 0.79–0.80) or during-office hours (RR 0.78, 95% CI 0.77–0.78).
Interpretation
We found that patients who received outpatient care from physicians affiliated with primary care networks were significantly less likely to present to an emergency department for any reason or for Patient Medical Home indicator conditions, suggesting improved access to primary care. Although patients of physicians affiliated with primary care networks were slightly more likely to be admitted to hospital for nonelective causes, lengths of stay were shorter, such that patients affiliated with a primary care network spent 86 fewer days in hospital per 1000 patient-years. After adjustment for health system use, socioeconomic status and region, as well as clinical covariates, the only Patient Medical Home indicator conditions with statistically significant results were fewer emergency department visits or hospital admissions for hypertension, but more for chronic coronary disease (not acute coronary syndromes). We suspect this reflects increased frequency of contact (allowing more frequent checks of blood pressure and thus better hypertension control v. more frequent contact, which increases the likelihood of a patient reporting chest pain, leading to a recommendation to attend an emergency department), but it may also just be chance. Moreover, 30-day readmission rates and repeat emergency department visits were all significantly lower after hospital discharge in patients affiliated with primary care networks.
Comparison with other studies
Another Canadian province, Ontario, has taken a different tack in its efforts at primary care reform. Its analysis of family health teams (akin to Alberta primary care networks with interprofessional teams and blended capitation physician payments) reported no statistically significant differences in emergency department visits or hospital admission rates for chronic conditions compared with 4 other primary care models in the same province between 2004 and 2012.19 Further research that focuses on process differences between Ontario family health teams and Alberta primary care networks is needed to explore the reasons for these differential effects.
On the other hand, our findings are similar to those reported by Intermountain Healthcare in Utah, where team-based care was associated with significantly lower rates of all-cause emergency department visits (incidence rate ratio [IRR] 0.77, 95% CI 0.74–0.80) and ambulatory care–sensitive emergency department visits or hospital admissions (IRR 0.77, 95% CI 0.70–0.85) compared with traditional primary care practices, with similar absolute differences to those we observed (5.4% absolute reduction in emergency department visits).10 However, unlike in our study, they found that the rate of all-cause hospital admissions was significantly lower (IRR 0.89, 95% CI 0.85–0.94, absolute risk difference 1.2 per 100 person-years). Although this may be attributable to the substantial clinical decision support technology and standardized chronic disease management pathways in their system, it may also be because they had a higher proportion of hospital admissions owing to Patient Medical Home indicator conditions than we did (one-sixth v. one-sixteenth in our cohort). Our proportion of admissions that are related to Patient Medical Home indicator conditions is closer to that reported by the Seattle Group Health Cooperative,12 which found no significant difference in all-cause hospital admissions (but a 29% relative reduction in all-cause emergency department visits) with a team-based primary care model similar to Alberta’s Primary Care Networks.
Although the Utah,10 Seattle13 and Ontario20 groups reported higher rates of some quality-of-care measures in team-based practices, it is important to note that not all process measures were improved in any of the settings — for example, blood pressure control rates were lower with team-based care in Utah and cancer screening rates were lower in Ontario. We were unable to examine quality of care in this study, although such an evaluation is currently ongoing in Alberta.
It is unclear to what extent our findings may be a result of better continuity of care in primary care networks. Primary care studies in multiple settings (including Europe, the United Kingdom, the United States and Australia) have shown that patients with greater physician continuity are less likely to use emergency departments or require hospital admissions, especially patients with chronic conditions or multiple comorbidities.21–24 Future studies should evaluate continuity metrics for patients treated in primary care networks, particularly in light of studies suggesting that older patients see a median of 2 primary care physicians and 5 specialists per year.25
Limitations
Although we were able to analyze all health care interactions for an entire Canadian province, there are some limitations to our study. Most importantly, we cannot infer causation, as unmeasured confounders (including patient health behaviours and provider demographics) may have differed between patients treated in primary care networks and conventional primary care. Second, although the amount of nonphysician team care provided likely differed between primary care networks, we do not have data on the frequency of visits to nonphysician health care providers and thus cannot comment on the incremental benefits of particular care elements. Third, we were unable to evaluate timeliness of access or patient satisfaction, and without access to actual laboratory values or physical measures, we cannot comment on the quality of care delivered to this cohort of patients. Fourth, we have no information on whether physicians affiliated with a primary care network were more likely to have electronic medical records; nor do we have any data on the quality of communication or coordination between different members of the health care team in primary care network practices. Finally, as the data were provided to us by Alberta Health in de-identified fashion, with the primary care network designation assigned to the patient file without details of their specific provider(s), we cannot create propensity scores for provider factors or adjust for potential clustering at the level of individual physicians, or the length of time particular physicians have been practising in a primary care network.
Conclusion
Our analysis suggests that a province-wide program to promote team-based primary care is a feasible and effective way to reduce use of emergency departments for Patient Medical Home indicator conditions or for any cause (a potential marker of improved access to care). Although physician pay for performance is often emphasized in efforts to reform primary care,26 the potential impact on the population seen with the Alberta primary care network natural experiment (169 fewer emergency department visits and 86 fewer hospital days per 1000 patient-years) is larger than has been seen with incentive payments for primary care physicians in various settings.27–29 Although the primary care network model holds substantial promise, a similar model in Ontario was not associated with similar effects. Thus, further research is required to explore the variation in implementation and process between Ontario family health teams and Alberta primary care networks, which may account for these differences.
Acknowledgements
This study is based in part on data provided by Alberta Health and Alberta Health Services. The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the Government of Alberta or Alberta Health Services. Neither the Government of Alberta nor Alberta Health Services expresses any opinion in relation to this study.
Footnotes
Competing interests: Brad Bahler and Richard Lewanczuk hold positions with Alberta Health Services. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Finlay McAlister was responsible for study conception and the first draft of the manuscript. Jeffrey Bakal assisted with the acquisition of data and analysis. All authors contributed to the study design, interpretation of analyses and revision of the manuscript. All of the authors gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Funding: No funding was received for this study. Infrastructure support was provided by the Alberta SPOR Support Unit Data Platform. Finlay McAlister holds the University of Alberta Chair in Cardiovascular Outcomes Research. These organizations were not involved in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or decision to submit the manuscript for publication.
References
- 1.Manns BJ, Tonelli M, Zhang J, et al. Enrolment in primary care networks: impact on outcomes and processes of care for patients with diabetes. CMAJ 2012; 184:E144–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson GL, Powers BJ, Chatterjee R, et al. Improving patient care. The patient-centered medical home: a systematic review. Ann Intern Med 2013;158:169–78. [DOI] [PubMed] [Google Scholar]
- 3.Smith SM, Wallace E, O’Dowd T, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;3:CD006560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hogg W, Lemelin J, Dahrouge S, et al. Randomized controlled trial of anticipatory and preventive multidisciplinary team care: for complex patients in a community- based primary care setting. Can Fam Physician 2009;55:e76–85. [PMC free article] [PubMed] [Google Scholar]
- 5.Katon WJ, Lin EHB, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med 2010;363:2611–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sommers LS, Marton KI, Barbaccia JC, et al. Physician, nurse and social worker collaboration in primary care for chronically ill seniors. Arch Intern Med 2000;160: 1825–33. [DOI] [PubMed] [Google Scholar]
- 7.Boult C, Reider L, Leff B, et al. The effect of guided care teams on the use of health services: results from a cluster-randomized controlled trial. Arch Intern Med 2011;171: 460–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedberg MW, Schneider EC, Rosenthal MB, et al. Association between participation in a multipayer medical home intervention and changes in quality, utilization, and costs of care. JAMA 2014;311:815–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Werner RM, Duggan M, Duey K, et al. The patient-centered medical home: an evaluation of a single private payer demonstration in New Jersey. Med Care 2013;51: 487–93. [DOI] [PubMed] [Google Scholar]
- 10.Reiss-Brennan B, Brunisholz KD, Dredge C, et al. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 2016;316:826–34. [DOI] [PubMed] [Google Scholar]
- 11.Rosenthal MB, Friedberg MW, Singer SJ, et al. Effect of a multipayer patient-centered medical home on health care utilization and quality: the Rhode Island chronic care sustainability initiative pilot program. JAMA Intern Med 2013;173:1907–13. [DOI] [PubMed] [Google Scholar]
- 12.Reid RJ, Coleman K, Johnson EA, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29:835–43. [DOI] [PubMed] [Google Scholar]
- 13.Riverin BD, Li P, Naimi AI, et al. Team-based versus traditional primary care models and short-term outcomes after hospital discharge. CMAJ 2017;189:E585–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Annis Emeott A, Markovitz A, Mason MH, et al. Four year evolution of a large, state-wide patient-centred medical home designation program in Michigan. Med Care 2013;51:846–53. [DOI] [PubMed] [Google Scholar]
- 15.Quan H, Li B, Saunders LDIMECCHI Investigators. Assessing validity of ICD-9-CM and ICD-10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res 2008;43:1424–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tonelli M, Wiebe N, Fortin M, et al. Alberta Kidney Disease Network. Methods for identifying 30 chronic conditions: application to administrative data. BMC Med Inform Decis Mak 2015;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McAlister FA, Bakal J, Majumdar SR, et al. Safely and effectively reducing inpatient length of stay: a controlled study of the General Internal Medicine Care Transformation Initiative. BMJ Qual Saf 2014;23:446–56. [DOI] [PubMed] [Google Scholar]
- 18.Pampalon R, Hamel D, Gamache P, et al. An area-based material and social deprivation index for public health in Québec and Canada. Can J Public Health 2012;103 (Suppl 2):S17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glazier RH, Hutchison B, Kopp A. Comparison of family health teams to ther Ontario primary care models, 2004/05 to 2011/12. Toronto: Institute for Clinical Evaluative Sciences; 2015. [Google Scholar]
- 20.Kiran T, Kopp A, Moineddin R, et al. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ 2015;187:E494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hussey PS, Schneider EC, Rudin RS, et al. Continuity and the costs of care for chronic disease. JAMA Intern Med 2014;174:742–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Walraven C, Oake N, Jennings A, et al. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract 2010;16:947–56. [DOI] [PubMed] [Google Scholar]
- 23.Nyweide DJ, Anthony DL, Bynum JPW, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med 2013;173: 1879–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weir DL, McAlister FA, Majumdar SR, et al. The interplay between continuity of care, multimorbidity, and health outcomes in patients with diabetes. Med Care 2016;54:386–93. [DOI] [PubMed] [Google Scholar]
- 25.Pham HH, Schrag D, O’Malley AS, et al. Care patterns in Medicare and their implications for pay for performance. N Engl J Med 2007;356:1130–9. [DOI] [PubMed] [Google Scholar]
- 26.Nuckols TK. With the Merit-Based Incentive Payment System, pay for performance is now national policy. Ann Intern Med 2017;166:368–9. [DOI] [PubMed] [Google Scholar]
- 27.Lavergne MR, Law MR, Peterson S, et al. A population-based analysis of incentive payments to primary care physicians for the care of patients with complex disease. CMAJ 2016;188:E375–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrison MJ, Dusheiko M, Sutton M, et al. Effect of a national primary care pay for performance scheme on emergency hospital admissions for ambulatory care sensitive conditions: controlled longitudinal study. BMJ 2014;349: g6423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Houle SK, McAlister FA, Jackevicius C, et al. Does performance-based remuneration for individual health care practitioners affect patient care? A systematic review. Ann Intern Med 2012;157:889–99. [DOI] [PubMed] [Google Scholar]