Abstract
Abortion is legal in South Africa, but over half of abortions remain unsafe there. Evidence suggests women who are (Black) African, of lower socioeconomic status, living with HIV, or residents of Gauteng, KwaZulu-Natal, or Limpopo provinces are disproportionately vulnerable to morbidity or mortality from unsafe abortion. Negative attitudes toward abortion have been documented in purposively sampled studies, yet it remains unclear what attitudes exist nationally or whether they differ across sociodemographic groups, with implications for inequities in service accessibility and health. In the current study, we analysed nationally representative data from 2013 to estimate the prevalence of negative abortion attitudes in South Africa and to identify racial, socioeconomic and geographic differences. More respondents felt abortion was ‘always wrong’ in the case of family poverty (75.4%) as compared to foetal anomaly (55%), and over half of respondents felt abortion was ‘always wrong’ in both cases (52.5%). Using binary logistic regression models, we found significantly higher odds of negative abortion attitudes among non-Xhosa African and Coloured respondents (compared to Xhosa respondents), those with primary education or less, and residents of Gauteng and Limpopo (compared to Western Cape). We contextualise and discuss these findings using a human rights-based approach to health.
Keywords: Abortion attitudes, South Africa, sociodemographics, abortion stigma, unsafe abortion
Introduction
While access to safe abortion services is considered a human right (United Nations 2016), approximately half of all abortions worldwide are unsafe (for example, self-induced, with an undertrained provider or using medically inappropriate protocols) – often in countries where abortion is illegal (Åhman and Shah 2011). In contrast, the legalisation of abortion is associated with reduction in abortion-related morbidity and mortality. For example, abortion was (largely) illegal in South Africa from 1975 until the Choice on Termination of Pregnancy Act was passed after Apartheid ended in 1996, granting legal access to abortion upon request until 12 weeks of pregnancy (Singh et al. 2012; Trueman and Magwentshu 2013; Vincent 2012). This caused a dramatic 91% decline in abortion-related mortality from 1994 to 2000 (Jewkes and Rees 2005).
Unsafe abortion can persist in legal settings, however, when access to safe services is difficult or inequitable. In South Africa today, over half of abortions are still estimated to be unsafe (Sedgh et al. 2012; Singh et al. 2012, 12). National maternal death reports, which notably no longer distinguish abortion from spontaneous miscarriage, suggest mortality from ‘miscarriage/abortion’ surged 62% between 2002–2004 and 2011–2013 (National Committee for the Confidential Enquiries into Maternal Deaths 2014). Evidence further suggests that women who are of lower socioeconomic status (Harries et al. 2015; Trueman and Magwentshu 2013), (Black) African (Constant et al. 2014), living with HIV (National Committee for the Confidential Enquiries into Maternal Deaths 2014; Orner et al. 2011; Stevens 2012) and/or residing in Gauteng, Limpopo or KwaZulu-Natal (National Committee for the Confidential Enquiries into Maternal Deaths 2014) are at higher risk of unsafe abortion and its health consequences than women who are more affluent, White, living without HIV and/or residing in other provinces. South African women have identified a number of barriers to safe abortion care including fear of discrimination or confidentiality breech, abuse and neglect by health workers, a dearth of abortion providers, waiting lists, gestational limits, long distances, insufficient knowledge about abortion laws and financial constraints (Constant et al. 2014; Cooper et al. 2004; Grossman et al. 2011; Harries et al. 2007, 2015; Jewkes et al. 2005; Trueman and Magwentshu 2013; Stevens 2012; Vincent 2012). Many researchers attribute these barriers to weaknesses of the South African health system generally and to abortion stigma specifically – a social process that ascribes negative attributes to women who access abortion care, to abortion providers and to others associated with abortion (Harris et al. 2011; Kumar, Hessini, and Mitchell 2009; Link and Phelan 2001; Norris et al. 2011).
While abortion stigma is a complex phenomenon that unfolds through a number of mechanisms at the macro and micro levels, negative individual-level attitudes toward abortion can be conceptualised as potential predictors of stigmatisation and resulting unsafe abortion (Gresh and Maharaj 2014; Harries, Stinson, and Orner 2009; Mwaba and Naidoo 2006; Varga 2002). In South Africa, researchers have documented negative attitudes toward abortion, but these are highly variable across the specific dimension of abortion (for example, moral compared to legal acceptability), circumstances of pregnancy, gender group, gender attitudes, religion and religiosity (Gresh and Maharaj 2014; Harries, Stinson, and Orner 2009; Harries et al. 2007; Macleod, Sigcau, and Luwaca 2011; Mwaba and Naidoo 2006; Patel and Johns 2009; Patel and Kooverjee 2009; Varga 2002; Vincent 2012; Wheeler et al. 2012). Most evidence to date has come from qualitative work and non-representative surveys among health workers in the Western Cape (Harries, Stinson, and Orner 2009; Harries et al. 2007), adolescents and students in KwaZulu-Natal (Gresh and Maharaj 2014; Mwaba and Naidoo 2006; Patel and Johns 2009; Patel and Kooverjee 2009; Wheeler et al. 2012) and community members in the rural Eastern Cape (Macleod, Sigcau, and Luwaca 2011). Broadly, South Africans seem to hold positive attitudes toward availability of abortion while still harboring strongly negative attitudes toward moral acceptability of abortion or women’s autonomy to choose an abortion (Patel and Johns 2009; Patel and Kooverjee 2009). Attitudes tend to be more positive or lenient when: pregnancy is the result of rape, there is risk of severe foetal anomaly, a woman is HIV positive, a woman’s health is in danger or it is her first abortion, as compared to when a woman is low income, having a so-called ‘repeat abortion’, unmarried or adolescent (Harries, Stinson, and Orner 2009, 7; Mwaba and Naidoo 2006; Vincent 2012; Wheeler et al. 2012). Notably, young and unmarried women in South Africa are simultaneously faced with the expectation of sexual availability for heterosexual partnerships, severe stigma against adolescent pregnancy and particularly restricted access to safe abortion options (Edin et al. 2016; Varga 2002; Waxman et al. 2016). Many in South Africa attribute their disapproval of abortion to religion, morality or culture (Gresh and Maharaj 2014; Macleod, Sigcau, and Luwaca 2011; Ronco 2014; Varga 2002), but researchers warn such static and homogeneous framing of culture ignores pre-colonial, indigenous abortion traditions and reinforces existing gender inequities (Macleod, Sigcau, and Luwaca 2011). Even after controlling for religion and religiosity, attitudes toward abortion accessibility and women’s autonomy to choose abortion (but not the moral acceptability of abortion) differ by gender, with women holding more egalitarian attitudes than men (Patel and Johns 2009; Patel and Kooverjee 2009).
To our knowledge, however, no studies have analysed abortion attitudes in a nationally representative sample from South Africa or explored differences by race/ethnicity, socioeconomic status or geography that might underlie observed differences in unsafe abortion risk. The purpose of the current study was to assess the prevalence of negative attitudes toward abortion nationally and identify any differences by race/ethnicity, socioeconomic status or geography while controlling for other covariates.
Theoretical framework
In this study we utilised a human rights-based approach to health (Shah, Åhman, and Ortayli 2014; United Nations 2014) that includes safe abortion as one of a comprehensive list of social, economic and other human rights aimed at women’s equity and empowerment. To the extent that negative abortion attitudes are tied to the limited availability of safe abortion and resulting health consequences, abortion attitudes are a human rights issue. According to the World Health Organization, a human rights-based approach to health applies seven key principles: availability, accessibility, acceptability, quality of facilities and services, participation, non-discrimination and accountability (United Nations 2014, 76). Researchers in South Africa have previously described how negative abortion attitudes can carry consequences for the availability, accessibility, quality and acceptability of abortion services and how those consequences are inequitably patterned by race, socioeconomic status, HIV status and region (Constant et al. 2014; Harries et al. 2015; National Committee for the Confidential Enquiries into Maternal Deaths 2014; Orner et al. 2011; Trueman and Magwentshu 2013). A human rights-based approach to health, in turn, places these abortion-related indicators in the broader context of women’s rights to comprehensive healthcare, personal dignity and non-discrimination by gender or other social categorisation (United Nations 2014). This approach informed many post-Apartheid South African policies, which simultaneously legalised abortion and promised access to contraception, maternity care and child support grants as part of social justice and economic development for all (African National Congress 1994a, 1994b; Baker 2010; Chopra et al. 2009; Coovadia et al. 2009). This broader vision of abortion and human rights – which the South African Minister of Social Development Bathabile Dlamini and others have called ‘reproductive justice’ (Dlamini 2014; Macleod and Hansjee 2013, 1007; Ross 2006, 2014) – is one based on equity rather than equality as it ‘considers gendered, raced, classed (and other) power relations in terms of the obstacles that people have to overcome … and the compensations that are required for outcomes to be equal’ (Macleod and Hansjee 2013, 1007). Such a theoretical framework is particularly well-suited for the current investigation of racial/ethnic, socioeconomic and geographical differences in abortion attitudes in South Africa.
Methods
Data and measurement
We used data from the most recent South African Social Attitudes Survey (SASAS) in 2013 (Human Sciences Research Council 2015). This is a nationally representative survey conducted annually and sampled from 500 census enumeration areas stratified by province, urbanicity and population group (Human Sciences Research Council 2015). Each face-to-face interview was conducted in the respondent’s household and lasted an average of 60–90 minutes.
Descriptive statistics of the weighted sample are presented in Table 1 (n = 2885). The SASAS only asked two questions about abortion attitudes, which we used as dependent variables: ‘Do you personally think it is wrong or not wrong for a woman to have an abortion if there is a strong chance of serious defect in the baby?’ and ‘Do you personally think it is wrong or not wrong for a woman to have an abortion if a family has a low-income and cannot afford any more children?’ Responses were measured using a Likert scale (‘not wrong at all’, ‘only wrong sometimes’, ‘almost always wrong’ and ‘always wrong’). As responses were heavily skewed (see Table 2) and we were most interested in those who are unequivocally opposed to abortion, we dichotomised these outcomes with ‘always wrong’ coded as 1 and all other categories coded as 0. We first analysed abortion attitudes in the two unique cases separately, and then constructed a third combined variable with feeling abortion is ‘always wrong’ in both cases coded as 1 and all other response patterns coded as 0.
Table 1.
The (weighted) South African Social Attitudes Survey sample in 2013.
| Variable | Value | Weighted percent |
|---|---|---|
| Race/ethnicity | African-isiXhosa | 17.8 |
| African-isiZulu | 23.5 | |
| African-Sepedi | 9.2 | |
| African-Sesotho | 8.9 | |
| African-Setswana | 8.0 | |
| African-other African language | 10.8 | |
| Coloured-Afrikaans | 6.7 | |
| Coloured-English | 2.4 | |
| Indian-any language | 2.9 | |
| White-Afrikaans | 5.8 | |
| White-English | 4.1 | |
| Educational attainment | Primary or less | 18.3 |
| Some secondary | 40.1 | |
| Matric or equivalent | 31.5 | |
| Tertiary education | 10.2 | |
| Economic class | Lower class | 41.9 |
| Working class | 22.7 | |
| Middle/upper class | 35.4 | |
| Province | Western Cape | 11.9 |
| Eastern Cape | 11.8 | |
| Northern Cape | 2.2 | |
| Free State | 5.3 | |
| KwaZulu-Natal | 18.6 | |
| North West | 6.7 | |
| Gauteng | 26.2 | |
| Mpumalanga | 7.5 | |
| Limpopo | 9.9 | |
| Urbanicity | Urban-formal | 63.5 |
| Urban-informal | 9.1 | |
| Rural | 27.3 | |
| Religion | Not religious | 15.0 |
| Christian | 69.5 | |
| Other | 15.5 | |
| Political ideology | Extremely Liberal/Left | 8.5 |
| Liberal/Left | 13.3 | |
| Slightly Liberal/Left | 12.1 | |
| Moderate | 23.9 | |
| Slightly Conservative/Right | 7.5 | |
| Conservative/Right | 6.5 | |
| Extremely Conservative/Right | 3.3 | |
| Don’t know | 25 |
Table 2.
Abortion attitudes in the case of serious foetal anomaly, family poverty and in both cases combined among South Africans in 2013 (weighted % of respondents).
| Attitude | Serious anomaly | Family poverty | Both cases |
|---|---|---|---|
| Not wrong at all | 22.5 | 9.1 | 22.0 |
| Wrong only sometimes | 14.1 | 7.3 | |
| Almost always wrong | 8.5 | 8.2 | |
| Always wrong | 55.0 | 75.4 | 52.5 |
We were primarily interested in sociodemographic variables that might explain observed differences in unsafe abortion risk in South Africa: race/ethnicity, socioeconomic status and geography. Researchers have previously defined race/ethnicity as ‘common geographic origins, ancestry, family patterns, language, cultural norms, traditions and the social history of particular groups’ (Williams et al. 2010, 70). On the 2013 SASAS, population groups were ‘Black African’, ‘Coloured’, ‘Indian/Asian’ and ‘White’. We combined this with the respondent’s language spoken at home and developed an 11-category variable representing race/ethnicity: African-isiXhosa, African-isiZulu, African-Sesotho, African-Setswana, African-Sepedi, African-Other (we collapsed Siswati, isiNdebele, Xitsonga, Tshivenga/Lemba and other African languages due to few respondents); Coloured-Afrikaans, Coloured-English, Indian, White-Afrikaans and White-English.
We operationalised socioeconomic status as level of educational attainment and self-reported economic class. In the 2013 SASAS, highest level of education was reported as ‘no schooling’, ‘primary’, ‘some secondary’, ‘matriculation or equivalent’, ‘tertiary education’ or ‘other/don’t know’. We combined the categories of ‘no schooling’ and ‘primary’ then used this as the reference group in multivariate analyses. The respondents who selected ‘other/don’t know’ were excluded from analyses. Because household income, employment and other common measures of economic status were significantly under-reported (as much as 27% missing data), we used self-reported economic class as a proxy. This was measured as ‘lower class’ (reference group), ‘working class’, ‘middle class’ or ‘upper class’. Due to small subsamples, we collapsed ‘middle class’ and ‘upper class’.
Geographical region was operationalised as province and urbanicity. Provinces were Western Cape (reference), Eastern Cape, Northern Cape, Free State, KwaZulu-Natal, North West, Gauteng, Mpumalanga or Limpopo. Urbanicity was measured as ‘urban-formal’, ‘urban-informal’, ‘rural-traditional’ or ‘rural-formal’ area. We collapsed the rural categories, creating a three-category variable, and used ‘urban-formal’ as the reference.
We controlled for additional covariates: gender, religion, age, and political attitudes. On the 2013 SASAS, respondents self-reported their sex as either ‘male’ or ‘female,’ which we used as an imperfect proxy for gender. Researchers on the SASAS also asked whether respondents belonged to any religion and, if so, which denomination from a list of over 25 options. Due to sampling constraints, we operationalised this as ‘not religious’ (reference), ‘Christian’ or ‘other’. We used the SASAS measure of age, which was a continuous variable ranging from 16 to 92 years, and political attitudes: ‘extremely Conservative/Right’, ‘Conservative/Right’, ‘slightly Conservative/Right’, ‘Moderate’, ‘slightly Liberal/Left’, ‘Liberal/Left’, ‘extremely Liberal/Left’ (reference) or ‘don’t know’.
Analyses
We first assessed the prevalence of negative abortion attitudes as the percent of respondents reporting abortion is ‘always wrong’ in the case of serious foetal anomaly, in the case of familial poverty and in both cases together. We then estimated binary logistic regression models (Long 1997; Long and Freese 2005) for the attitudes toward abortion in the two different cases separately and in the two cases combined. All variables were entered simultaneously into the models. We calculated odds ratios for race/ethnicity, education, economic class, province and urbanicity, while controlling for the covariates described above. All analyses were conducted in Stata v. 14 (StataCorp 2014) using sample weighting. Sensitivity analyses were also conducted in order to assess robustness of our results. These included other measures for race/ethnicity, economic class, religion, political attitudes and age. We also conducted ordinal regression models for each individual abortion attitude and a multinomial model of both attitudes combined. Results across these sensitivity analyses were similar to those described below.
Results
Prevalence of negative abortion attitudes
Attitudes toward abortion differed by circumstance of pregnancy (see Table 2). When asked about abortion in the case of serious foetal anomaly, about half of South Africans surveyed said it was ‘always wrong’. Attitudes toward abortion in the case a family is low-income were significantly more negative, with over three-quarters saying it was ‘always wrong’. When we combined the attitudes toward abortion in both cases, about half of respondents said abortion was ‘always wrong’.
Bivariate analyses
We found that several sociodemographic factors were related to both abortion attitudes at the bivariate level (see Table 3). Looking at the two cases combined, respondents were less likely to say abortion is ‘always wrong’ if they were African and spoke isiXhosa or isiZulu at home or if they were White and spoke English at home. African respondents who spoke Setswana, Sesotho or another African language at home were more likely to report abortion is ‘always wrong’. Respondents who completed their secondary education or who had any tertiary education were less likely to report abortion is ‘always wrong’. Those who self-reported as lower economic class were more likely to feel abortion is ‘always wrong’. In bivariate analyses, respondents in the Western Cape, KwaZulu-Natal and Mpumalanga were less likely to report abortion is ‘always wrong’, while those living in Gauteng, Northwest and Limpopo were more likely to report abortion is ‘always wrong’. Slightly liberal respondents were less likely and extremely conservative respondents more likely to report abortion as ‘always wrong’. Gender, age, religion and urbanicity were not associated with abortion attitudes at the bivariate level.
Table 3.
Bivariate analyses of reporting abortion is ‘always wrong’ in South Africa in 2013.
| Variable | Foetal anomaly | Family poverty | Both cases |
|---|---|---|---|
| African-isiXhosa | 12.51*** | 34.14*** | 11.5*** |
| African-isiZulu | 2.65 | 2 | 4.41* |
| African-Sepedi | 12.32*** | 5.29* | 11.58** |
| African-Setswana | 6.12* | 12.33*** | 10.23** |
| African-Sesotho | 7.8** | 11.16*** | 5.23* |
| African-other African | 4.04* | 0.85 | 3.99* |
| Coloured-Afrikaans | 0.06 | 0.15 | 0.06 |
| Coloured-English | 0.01 | 3.93* | 0.04 |
| Indian-any | 1.75 | 4.47* | 2.63 |
| White-Afrikaans | 1.8 | 0.083 | 0.893 |
| White-English | 12.44*** | 6.25* | 9.45** |
| Primary education or less | 5.55* | 3.19 | 0.26 |
| Some secondary education | 0.74 | 1.97 | 0.773 |
| Completed secondary education | 0.42 | 4.16* | 10.49** |
| Some tertiary education | 12.15*** | 1.52 | 6.24* |
| Lower class | 6.24 | 0.28 | 6.27* |
| Working class | 1.13 | 0.47 | 1.32 |
| Middle/upper class | 3.48 | 1.56 | 2.98 |
| Western Cape | 12.93*** | 28.32*** | 11.59*** |
| Eastern Cape | 2.77 | 9.69** | 3.42 |
| Northern Cape | 1.91 | 5.13* | 1.99 |
| Free State | 0.043 | 12.3*** | 0.01 |
| KwaZulu-Natal | 16.6*** | 0.24 | 21.7*** |
| Northwest | 4.58* | 6.21* | 6.25* |
| Gauteng | 14.53*** | 4.82* | 16.67*** |
| Mpumalanga | 1.86 | 3.32 | 3.91* |
| Limpopo | 30.15*** | 10.43** | 29.54*** |
| Urban-formal | 2.18 | 1.67 | 1.76 |
| Urban-informal | 0.88 | 0.39 | 1.66 |
| Rural | 0.88 | 1 | 0.18 |
| Female | 2.56 | 3.4 | 3.82 |
| Not religious | 0.41 | 0.54 | 0.34 |
| Christian | 0.05 | 0.51 | 0.05 |
| Other religion | 0.61 | 0.09 | 0.54 |
| Extremely Liberal/Left | 0.17 | 0.92 | 0.35 |
| Liberal/Left | 0.67 | 0.09 | 0.23 |
| Slightly Liberal/Left | 7.03** | 8.01** | 9.25** |
| Moderate | 0.58 | 0.01 | 0.15 |
| Slightly Conservative/Right | 0.08 | 0.85 | 0.02 |
| Conservative/Right | 0.57 | 3.35 | 1.04 |
| Extremely Conservative | 6.58* | 0.45 | 5.38* |
| Don’t know | 2.03 | 0.02 | 0.84 |
F-statistics are presented (e.g., African-Xhosa compared to all others).
p < .001;
p < .01;
p < .05.
Significantly greater proportions bolded, lower proportions italicised.
Multivariate analyses
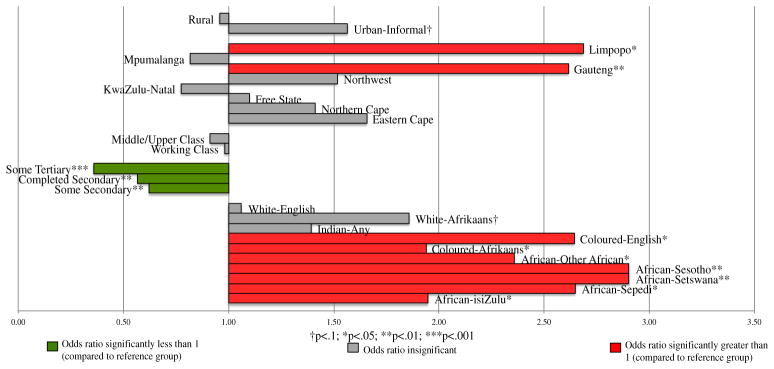
We present the binary logistic regression models for abortion attitudes in the case of foetal anomaly, in the case of familial poverty and for both cases combined in Table 4. Odds ratios for sociodemographic factors significantly associated with abortion attitudes in both cases combined are shown in Figure 1. In comparison to African respondents who spoke isiXhosa at home, we found that respondents were more likely to report abortion is ‘always wrong’ in both cases if they were African and spoke isiZulu, Sepedi, Setswana, Sesotho or another African language or if they were Coloured. Compared to those with a primary-level education or less, respondents who received any secondary, completed secondary or received any tertiary education were significantly less likely to report abortion is ‘always wrong’ in both cases. Respondents living in Gauteng and Limpopo provinces were more likely to feel abortion is ‘always wrong’ in both cases, compared to the Western Cape. When considering both cases together, respondents’ gender, age, religion and political attitudes were not associated with attitudes toward moral acceptability of abortion.
Table 4.
Adjusted odds ratios of reporting abortion is ‘always wrong’ in South Africa in 2013.
| Variable | Foetal anomaly*** | Poverty*** | Both cases*** | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| (n= 2477) | (n = 2481) | (n = 2459) | ||||
|
|
|
|
||||
| OR | SD | OR | SD | OR | SD | |
| Race/ethnicity (African-isiXhosa ref) | ||||||
| African-isiZulu | 2.08* | 0.43 | 3.59** | 0.43 | 1.95* | 0.43 |
| African-Sepedi | 2.74* | 0.3 | 4.24** | 0.30 | 2.65* | 0.30 |
| African-Setswana | 2.49* | 0.29 | 5.29*** | 0.29 | 2.90** | 0.29 |
| African-Sesotho | 3.59** | 0.27 | 5.03*** | 0.27 | 2.90** | 0.27 |
| African-other | 2.38* | 0.31 | 3.72** | 0.31 | 2.36* | 0.31 |
| Coloured-Afrikaans | 2.02* | 0.24 | 3.14*** | 0.24 | 1.94* | 0.24 |
| Coloured-English | 2.87* | 0.16 | 2.07 | 0.15 | 2.64* | 0.15 |
| Indian-any | 1.64 | 0.17 | 1.38 | 0.17 | 1.39 | 0.17 |
| White-Afrikaans | 1.82 | 0.23 | 2.86** | 0.23 | 1.86 | 0.23 |
| White-English | 1.03 | 0.19 | 1.21 | 0.19 | 1.06 | 0.19 |
| Education (primary or less ref) | ||||||
| Some secondary | 0.69* | 0.49 | 0.99 | 0.49 | 0.62** | 0.49 |
| Completed secondary | 0.63* | 0.47 | 0.65 | 0.47 | 0.57** | 0.47 |
| Some tertiary | 0.39** | 0.30 | 0.63 | 0.30 | 0.36*** | 0.30 |
| Economic class (lower class ref) | ||||||
| Working class | 0.97 | 0.42 | 1.27 | 0.42 | 0.98 | 0.42 |
| Middle/upper class | 0.87 | 0.48 | 1.08 | 0.48 | 0.91 | 0.48 |
| Province (Western Cape ref) | ||||||
| Eastern Cape | 1.71 | 0.34 | 2.29* | 0.32 | 1.66 | 0.32 |
| Northern Cape | 1.58 | 0.14 | 2.50* | 0.13 | 1.41 | 0.13 |
| Free State | 0.93 | 0.23 | 3.10** | 0.23 | 1.10 | 0.23 |
| KwaZulu-Natal | 0.81 | 0.41 | 1.87 | 0.39 | 0.77 | 0.39 |
| Northwest | 1.56 | 0.25 | 2.11 | 0.25 | 1.52 | 0.25 |
| Gauteng | 2.55** | 0.40 | 2.31** | 0.44 | 2.61** | 0.44 |
| Mpumalanga | 0.89 | 0.27 | 0.92 | 0.26 | 0.82 | 0.27 |
| Limpopo | 2.58* | 0.33 | 2.55 | 0.31 | 2.69* | 0.31 |
| Urbanicity (urban-formal ref) | ||||||
| Urban-informal | 1.38 | 0.29 | 1.32 | 0.29 | 1.57 | 0.29 |
| Rural | 1.05 | 0.45 | 0.95 | 0.45 | 0.96 | 0.45 |
All models controlled for gender, age, religion and political attitudes.
OR = odds ratio; SD = standard deviation.
p < .001;
p < .01;
p < .05;
Significantly greater odds are bolded and significantly lower odds italicised.
Figure 1.
Adjusted odds ratios of reporting abortion is ‘always wrong’ (in both cases combined) in South Africa in 2013.
Some differences in abortion attitudes were noted across circumstances of pregnancy. Compared to African respondents who spoke isiXhosa at home, White respondents who spoke Afrikaans at home were significantly more likely to report abortion is ‘always wrong’ in the case of poverty but not in the case of foetal anomaly. Coloured respondents who spoke English at home were equally as likely as Xhosa respondents to report abortion is ‘always wrong’ in the case of family poverty but were more likely to in the case of foetal anomaly. Education was not significantly associated with abortion attitudes in the case of poverty, although it was in the case of foetal anomaly and when both cases were combined. Residents in the Eastern Cape, Northern Cape and Free State were significantly more likely to report abortion is ‘always wrong’ in the case of poverty but not in the case of severe foetal anomaly or in both cases combined. Specifically in the case of poverty, increasing age was also associated with increased odds of reporting abortion is ‘always wrong’ (odds ratio not shown: 1.01, p < .05). Finally, extremely conservative respondents were significantly more likely than extremely liberal respondents to report abortion is always wrong in the case of foetal anomaly (odds ratio not shown: 1.99; p < .05), while slightly (as compared to extremely) liberal respondents were significantly less likely to report abortion is ‘always wrong’ in the case of poverty (odds ratio not shown: 0.45; p < .05).
Discussion
Our analyses of the 2013 SASAS show negative attitudes toward abortion are common in South Africa – over half of respondents felt abortion was always wrong in both cases (foetal anomaly and poverty) combined. We also found that attitudes vary by race/ethnicity, education, province and circumstances of pregnancy. Non-Xhosa African respondents, Coloured respondents who speak Afrikaans, individuals of lower educational attainment and those living in Gauteng and Limpopo provinces held significantly and consistently more negative attitudes toward abortion in both cases presented. These sociodemographic differences in abortion attitudes – to the extent they may limit access to safe abortion services and increase risk of abortion-related complications and mortality – carry important implications for human rights and health equity and they offer insight into opportunities for research and intervention in South Africa.
Respondents were more likely to feel that abortion is always wrong in the case of family poverty as compared to when there is a strong chance of serious foetal anomaly. This finding is consistent with previous evidence in South Africa and other settings that has suggested attitudes toward abortion differ across the circumstances of pregnancy (Gresh and Maharaj 2014; Macleod, Sigcau, and Luwaca 2011; Mwaba and Naidoo 2006; Patel and Johns 2009; Patel and Kooverjee 2009; Ronco 2014; Varga 2002; Vincent 2012; Wheeler et al. 2012). Our findings echo previous qualitative and subpopulation surveys that demonstrated the risk of birth defects or other disabilities is considered a relatively acceptable reason for abortion (Gresh and Maharaj 2014; Mwaba and Naidoo 2006; Patel and Kooverjee 2009; Varga 2002). While close-ended questions and responses on the SASAS limit interpretability, these more lenient attitudes toward abortion in the case of serious foetal anomaly are likely tied to stigmatisation of disability throughout South Africa – as documented in previous regionally-specific South Africa studies (Gresh and Maharaj 2014; Varga 2002). Researchers in other settings have also suggested that some circumstances of abortion, including foetal anomaly and endangerment of the woman’s health, are viewed as random events outside a woman’s control (Huang et al. 2016). Abortion in such cases might not be perceived as women’s agentic resistance to traditional gender roles, which could facilitate social permissibility and reduce stigmatisation.
Attitudes toward abortion in the case of familial poverty were more pervasively negative across all racial/ethnic groups, levels of education and provinces. This is consistent with most research on the subject, which has shown poverty is typically seen as a relatively less acceptable reason for abortion as compared to foetal anomaly, rape or risk to the woman’s health (Mwaba and Naidoo 2006; Patel and Johns 2009; Patel and Kooverjee 2009; Vincent 2012). Some qualitative research has contrastingly suggested, however, that poverty can be seen as a justifiable reason for abortion in some sub-populations. Our results might differ from these studies because we relied on close-ended survey questions and our sample is nationally representative rather than purposively chosen from health workers in the Western Cape (Harries, Stinson, and Orner 2009) or adolescents in KwaZulu-Natal (Varga 2002). We did find that attitudes toward abortion in the case of poverty were less negative in the Western Cape and with younger respondents. Additional qualitative research is needed to fully understand the mechanisms underlying these abortion attitudes.
Hypothetically, our results could reflect what others have called intersectional stigma (Earnshaw and Kalichman 2013). Derived in part from the theory of intersectionality (Crenshaw 1989), this conceptualisation suggests that each stigmatised status intersects with and is shaped by existing social hierarchies (Earnshaw and Kalichman 2013). For example, the discrimination experienced by low-income women seeking abortion may be simultaneously driven by both abortion and economic stigma – both of which constitute human rights issues. Alternatively, our results could reflect a particular importance that is placed on motherhood for low-income and otherwise marginalised women who have limited access to normative forms of status-building, identity-development and meaning-making (Cooper et al. 2007; Walker 1995). Future studies might investigate the relationships between abortion attitudes and those toward poverty and motherhood more generally.
Our results also suggest that additional sociocultural factors may increase the likelihood of negative abortion attitudes in South Africa above and beyond socioeconomic status, gender, age, religion, political attitudes and geography. Collectively, the differences in abortion attitudes we observed across racial/ethnic groups likely reflect South African heterogeneity in social norms and cultural ideologies related to gender, reproduction and motherhood. For example, medical historians have documented that abortion was widespread in pre-colonial Xhosa society with general social acceptance (Bradford 1991), and the particularly patriarchal anti-abortion norms of Zulu and Afrikaner societies have been extensively documented (Bradford 1991; Gresh and Maharaj 2014; Hodes 2013; Varga 2002). Additional studies are needed to better understand the various sociocultural mechanisms of abortion attitude formation and if these attitude differences might contribute to observed unsafe abortion inequities by race/ethnicity.
Controlling for other factors, respondents living in Gauteng and Limpopo provinces were consistently more likely to express negative abortion attitudes, which underscores the role of province-level factors above and beyond sociocultural or individual-level characteristics in the patterning of South African abortion attitudes. Notably, both negative abortion attitudes and abortion-related mortality (National Committee for the Confidential Enquiries into Maternal Deaths 2014) are significantly higher in Gauteng and Limpopo as compared to the national average, although further research is needed to document if and how attitudes might predict unsafe abortion behaviours and outcomes. In-depth studies at the province-level might be useful for investigating the ways in which these and other characteristics contextualise abortion attitudes and outcomes, particularly since access to abortion services varies so much across provinces (Health Systems Trust 2015) and between rural and urban areas (Cooper et al. 2005). Overall, we did not find urbanicity to be a significant factor, in contrast to previously reported findings that negative abortion attitudes are more pervasive in rural areas (Varga 2002).
Respondents with a secondary or post-secondary education were significantly less likely to report negative attitudes toward abortion. This finding echoes previous work around the world, which has demonstrated increasingly positive attitudes toward abortion with greater education (Jelen and Wilcox 2003; Patel and Johns 2009; Patel and Kooverjee 2009). From our cross-sectional analysis, it remains unclear if higher educational attainment predicted more positive abortion attitudes or, conversely, if more positive abortion attitudes predicted greater educational attainment. Future qualitative studies could illuminate pathways above and beyond direct knowledge of abortion laws through which education might be associated with abortion attitudes, and why abortion attitudes in the case of poverty do not vary by level of education. Notably, education was the only significant socioeconomic predictor – self-reported economic class was not associated with abortion attitudes. This suggests that higher risk of unsafe abortion among low-income women cannot be attributed simply to more negative abortion attitudes – alternatively the disparity might result from inequitable access to safe, more expensive services.
Ultimately, our findings reiterate the need for a continuing human rights-based approach that addresses the structural and social conditions influencing women’s abortion decisions and health outcomes including poverty, weak health and social welfare systems, and stigma. In South Africa today, as under Apartheid, African women continue to experience lower wages and higher unemployment as compared to their male and non-African female counterparts (Statistics South Africa 2013, 2015). Health system strengthening also remains a critical structural intervention needed to improve access to and integration of safe abortion care, HIV prevention and treatment, and high-quality contraceptive counselling and services. Improved structural support systems for persons with disability are needed particularly for those pregnant women who oppose abortion but lack the financial, institutional or emotional resources needed to raise a child with disability. Finally, interventions are needed to address ongoing social stigma against abortion that threatens human rights both theoretically (by reducing women, providers and others associated with abortion to less than whole and dignified humans) and practically (by reducing access to safe health services).
There are several limitations to the current study. First, the SASAS questions and response categories used to measure abortion attitudes were close-ended and do not fully capture the full spectrum of abortion ideologies or their contexts. It is possible that even the wording of response categories in the survey – framing abortion as ‘always/almost always/sometimes wrong’ rather than ‘always/almost always/sometimes right’ – influenced participants’ answers (for example, by sending implicit cues that abortion is a non-normative and stigmatised behaviour). Moreover, abortion stigma is a much broader, complex social phenomenon that cannot be adequately captured by close-ended abortion attitude measurements. Additionally, all of our conclusions are based on cross-sectional data and, therefore, represent statistical associations and not causal linkages. Because of limited sample size, we could not stratify models nor conduct interactional analyses – for example, between race/ethnicity and socioeconomic status. Furthermore, our analysis of solely quantitative SASAS data prevents in-depth analyses, including interviewer-respondent dynamics, household dynamics affecting the interview and non-structured reactions to sensitive topics. Nevertheless, our results provide an initial investigation into abortion attitudes from a nationally representative sample in South Africa.
Moving forward, researchers, policy-makers and advocates, health workers and public health professionals can build on the evidence presented here to address unsafe abortion, and social inequities therein. Future quantitative studies might analyse trends in abortion attitudes over time in relation to race/ethnicity, education and province, while interaction models could also be used to disentangle the ways these sociodemographic factors individually and jointly modify pathways. Researchers could also employ qualitative research methods to elicit open-ended responses about abortion attitudes more broadly, including tensions and contingencies, mechanisms of formation in various groups, implications for abortion stigma and unsafe abortion and the role of historical contexts. Contemporary abortion attitudes are likely to be influenced by the largely illegal and often lethal condition of abortion under Apartheid, when unsafe abortion caused over 400 maternal deaths among impoverished African women each year (Hodes 2013; Klausen 2015). Qualitative approaches could also shed light on complicated dynamics of the interview process itself when investigating sensitive topics like abortion.
Policy-makers and advocates must improve access to free and safe abortion services in South Africa, while also committing time and resources to improving the social and economic conditions of women more broadly. Healthcare provider training institutions could re-commit to comprehensive, safe abortion services and patient-focused, evidence-based counselling by including abortion care and values clarification as a fundamental part of their curricula. Effective interventions for healthcare providers have already been developed and evaluated in South Africa including Health Workers for Choice (Varkey, Fonn, and Ketlhapile 2001) and Health Workers for Change (Fonn and Xaba 2001). For example, in 2002 a series of values clarification workshops based on Health Workers for Choice and Health Workers for Change was conducted in Limpopo province, and a retrospective evaluation in 2004 observed significantly increased knowledge of abortion legislation, compassion and empathy for abortion clients and providers, and supportive behaviours including advocacy and improvement of reproductive healthcare services (Trueman and Gabriel 2005). Public health professionals could simultaneously foster community-led de-stigmatising abortion campaigns such as the community equivalent of Health Workers for Choice called Communities for Choice (Varkey and Ketlhapile 2001), while also partnering to address other health concerns in the community that might be rooted in poverty or racial/ethnic marginalisation (for example, HIV). The continuing application of a comprehensive human rights-based approach to abortion in South Africa will be needed to ensure all women are equitably supported to have safe abortions, to have children and to raise their children with dignity as they so choose.
Acknowledgments
Funding
This work was supported by the University of Michigan Rackham Graduate School with funding support through the Rackham Merit Fellowship and by the NICHD grant (R24 HD041028) to the Population Studies Center.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- African National Congress. African National Congress Constitution of 1994. Johannesburg, South Africa: African National Congress; 1994a. http://www.anc.org.za/show.php?id=210. [Google Scholar]
- African National Congress. A National Health Plan for South Africa. Johannesburg, South Africa: African National Congress; 1994b. http://whqlibdoc.who.int/publications/1994/0958386714.pdf. [Google Scholar]
- Ǻhman E, Shah IH. New Estimates and Trends regarding Unsafe Abortion Mortality. International Journal of Gynecology & Obstetrics. 2011;115(2):121–126. doi: 10.1016/j.ijgo.2011.05.027. [DOI] [PubMed] [Google Scholar]
- Baker PA. From Apartheid to Neoliberalism: Health Equity in Post-Apartheid South Africa. International Journal of Health Services. 2010;40(1):79–95. doi: 10.2190/HS.40.1.e. [DOI] [PubMed] [Google Scholar]
- Bradford H. Herbs, Knives and Plastic: 150 Years of Abortion in South Africa. In: Meade T, Walker M, editors. Science, Medicine, and Cultural Imperialism. New York: St. Martin’s Press Inc; 1991. pp. 120–147. [Google Scholar]
- Chopra M, Daviaud E, Pattinson R, Fonn S, Lawn JE. Saving the Lives of South Africa’s Mothers, Babies, and Children: Can the Health System Deliver? The Lancet. 2009;374(9692):835–846. doi: 10.1016/S0140-6736(09)61123-5. [DOI] [PubMed] [Google Scholar]
- Constant D, Grossman D, Lince N, Harries J. Self-Induction of Abortion among Women Accessing Second-Trimester Abortion Services in the Public Sector, Western Cape Province, South Africa: An Exploratory Study. South African Medical Journal. 2014;104(4):302–305. doi: 10.7196/samj.7408. [DOI] [PubMed] [Google Scholar]
- Cooper D, Morroni C, Orner P, Moodley J, Harries J, Cullingworth L, Hoffman M. Ten Years of Democracy in South Africa: Documenting Transformation in Reproductive Health Policy and Status. Reproductive Health Matters. 2004;12(24):70–85. doi: 10.1016/s0968-8080(04)24143-x. [DOI] [PubMed] [Google Scholar]
- Cooper D, Dickson K, Blanchard K, Cullingworth L, Mavimbela N, von Mollendorf C, van Bogaert L, Winikoff B. Medical Abortion: The Possibilities for Introduction in the Public Sector in South Africa. Reproductive Health Matters. 2005;13(26):35–43. doi: 10.1016/S0968-8080(05)26203-1. [DOI] [PubMed] [Google Scholar]
- Cooper D, Harries J, Myer L, Orner P, Bracken H. ‘Life is Still Going On’: Reproductive Intentions among HIV-Positive Women and Men in South Africa. Social Science & Medicine. 2007;65(2):274–283. doi: 10.1016/j.socscimed.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The Health and Health System of South Africa: Historical Roots of Current Public Health Challenges. The Lancet, Health in South Africa. 2009;374:817–834. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- Crenshaw K. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. University of Chicago Legal Forum. 1989;1989(1):139–169. [Google Scholar]
- Dlamini B. Minister Dlamini to the United Nations General Assembly on Sexual and Reproductive Health in Africa. New York: South African National Government; 2014. http://www.gov.za/address-minister-social-development-ms-bathabile-dlamini-mp-occasion-united-nations-general-assembly. [Google Scholar]
- Earnshaw VA, Kalichman SC. Stigma Experienced by People Living with HIV/AIDS. In: Liamputtong P, editor. Stigma, Discrimination and Living with HIV/AIDS. Dordrecht: Springer Netherlands; 2013. pp. 23–38. [Google Scholar]
- Edin K, Nilsson B, Ivarsson A, Kinsman J, Norris SA, Kahn K. Perspectives on Intimate Relationships among Young People in Rural South Africa: The Logic of Risk. Culture, Health & Sexuality. 2016;18(9):1010–1024. doi: 10.1080/13691058.2016.1155749. [DOI] [PubMed] [Google Scholar]
- Fonn S, Xaba M. Health Workers for Change: Developing the Initiative. Health Policy and Planning. 2001;16(Suppl 1):13–18. doi: 10.1093/heapol/16.suppl_1.13. [DOI] [PubMed] [Google Scholar]
- Gresh A, Maharaj P. Termination of Pregnancy: Perspectives of Female Students in Durban, South Africa. African Population Studies. 2014;28(1):681–690. [Google Scholar]
- Grossman D, Constant D, Lince N, Alblas M, Blanchard K, Harries J. Surgical and Medical Second Trimester Abortion in South Africa: A Cross-Sectional Study. BMC Health Services Research. 2011;11(1) doi: 10.1186/1472-6963-11-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harries J, Orner P, Gabriel M, Mitchell E. Delays in Seeking an Abortion until the Second Trimester: A Qualitative Study in South Africa. Reproductive Health. 2007;4(1) doi: 10.1186/1742-4755-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harries J, Stinson K, Orner P. Health Care Providers’ Attitudes towards Termination of Pregnancy: A Qualitative Study in South Africa. BMC Public Health. 2009;9(1) doi: 10.1186/1471-2458-9-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harries J, Gerdts C, Momberg M, Foster DG. An Exploratory Study of What Happens to Women Who Are Denied Abortions in Cape Town, South Africa. Reproductive Health. 2015;12(1) doi: 10.1186/s12978-015-0014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris LH, Debbink M, Martin L, Hassinger J. Dynamics of Stigma in Abortion Work: Findings from a Pilot Study of the Providers Share Workshop. Social Science & Medicine. 2011;73(7):1062–1070. doi: 10.1016/j.socscimed.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Health Systems Trust. Terminations of Pregnancy. 2015 http://indicators.hst.org.za/healthstats/47/data.
- Hodes R. The Medical History of Abortion in South Africa, C. 1970–2000. Journal of Southern African Studies. 2013;39(3):527–542. [Google Scholar]
- Huang Y, Davies PG, Sibley CG, Osborne D. Benevolent Sexism, Attitudes toward Motherhood, and Reproductive Rights a Multi-Study Longitudinal Examination of Abortion Attitudes. Personality and Social Psychology Bulletin. 2016;42(7):970–984. doi: 10.1177/0146167216649607. [DOI] [PubMed] [Google Scholar]
- Human Sciences Research Council. South African Social Attitudes Survey (SASAS) 2015 http://www.hsrc.ac.za/en/departments/sasas.
- Jelen TG, Wilcox C. Causes and Consequences of Public Attitudes toward Abortion: A Review and Research Agenda. Political Research Quarterly. 2003;56(4):489–500. [Google Scholar]
- Jewkes R, Rees H. Dramatic Decline in Abortion Mortality due to the Choice on Termination of Pregnancy Act: Scientific Letter. South African Medical Journal. 2005;95(4):250. [PubMed] [Google Scholar]
- Jewkes RK, Gumede T, Westaway MS, Dickson K, Brown H, Rees H. Why Are Women Still Aborting outside Designated Facilities in Metropolitan South Africa? BJOG: An International Journal of Obstetrics & Gynaecology. 2005;112(9):1236–1242. doi: 10.1111/j.1471-0528.2005.00697.x. [DOI] [PubMed] [Google Scholar]
- Klausen S. Abortion under Apartheid. New York: Oxford University Press; 2015. [Google Scholar]
- Kumar A, Hessini L, Mitchell EMH. Conceptualising Abortion Stigma. Culture, Health & Sexuality. 2009;11(6):625–639. doi: 10.1080/13691050902842741. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing Stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Long JS. Regression Models for Categorical and Limited Dependent Variables. Vol. 7. United States: SAGE Publications Inc; 1997. [Google Scholar]
- Long JS, Freese J. Regression Models for Categorical Outcomes Using Stata. College Station, TX: Stata Press; 2005. [Google Scholar]
- Macleod CI, Hansjee J. Men and Talk about Legal Abortion in South Africa: Equality, Support and Rights Discourses Undermining Reproductive ‘Choice’. Culture, Health & Sexuality. 2013;15(8):997–1010. doi: 10.1080/13691058.2013.802815. [DOI] [PubMed] [Google Scholar]
- Macleod C, Sigcau N, Luwaca P. Culture as a Discursive Resource Opposing Legal Abortion. Critical Public Health. 2011;21(2):237–245. [Google Scholar]
- Mwaba K, Naidoo P. Knowledge, Beliefs and Attitudes regarding Abortion in South Africa among a Sample of University Students. Journal of Psychology in Africa. 2006;16(1):53–58. [Google Scholar]
- National Committee for the Confidential Enquiries into Maternal Deaths. Saving Mothers 2011–2013: Sixth Report on the Confidential Enquiries into Maternal Deaths in South Africa. South Africa: Department of Health; 2014. http://www.hst.org.za/publications/saving-mothers-2008-2010-fifth-report-confidential-enquiries-maternal-deaths-south-afri. [Google Scholar]
- Norris A, Bessett D, Steinberg JR, Kavanaugh ML, De Zordo S, Becker D. Abortion Stigma: A Reconceptualization of Constituents, Causes, and Consequences. Women’s Health Issues. 2011;21(3):S49–S54. doi: 10.1016/j.whi.2011.02.010. [DOI] [PubMed] [Google Scholar]
- Orner PJ, de Bruyn M, Barbosa RM, Boonstra H, Gatsi-Mallet J, Cooper DD. Access to Safe Abortion: Building Choices for Women Living with HIV and AIDS. Journal of the International AIDS Society. 2011;14(1):54. doi: 10.1186/1758-2652-14-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel CJ, Johns L. Gender Role Attitudes and Attitudes to Abortion: Are There Gender Differences? The Social Science Journal. 2009;46(3):493–505. [Google Scholar]
- Patel CJ, Kooverjee T. Abortion and Contraception: Attitudes of South African University Students. Health Care for Women International. 2009;30(6):550–568. doi: 10.1080/07399330902886105. [DOI] [PubMed] [Google Scholar]
- Ronco C. Discursive Constructs of Abortion amongst a Group of Male and Female Students at the University of the Witwatersrand. 2014 http://mobile.wiredspace.wits.ac.za/handle/10539/13974.
- Ross L. Understanding Reproductive Justice. Atlanta, Georgia: SisterSong; 2006. http://www.trustblackwomen.org/our-work/what-is-reproductive-justice/9-what-is-reproductive-justice. [Google Scholar]
- Ross L. Amandla! South African Minister Underscores Reproductive Justice as a Global Framework. Reproductive Health Reality Check. 2014 Sep 23; http://rhrealitycheck.org/article/2014/09/23/amandla-south-african-minister-underscores-reproductive-justice-global-framework/
- Sedgh G, Singh S, Shah IH, Åhman E, Henshaw SK, Bankole A. Induced Abortion: Incidence and Trends Worldwide from 1995 to 2008. The Lancet. 2012;379(9816):625–632. doi: 10.1016/S0140-6736(11)61786-8. [DOI] [PubMed] [Google Scholar]
- Shah I, Åhman E, Ortayli N. Access to Safe Abortion: Progress and Challenges since the 1994 International Conference on Population and Development (ICPD) ICPD Beyond 2014 Expert Meeting on Women’s Health – Rights, Empowerment and Social Determinants. 2014 doi: 10.1016/j.contraception.2014.04.004. http://icpdbeyond2014.org/uploads/browser/files/access_to_safe_abortion.pdf. [DOI] [PubMed]
- Singh S, Sedgh G, Bankole A, Hussain R, London S. Making Abortion Services Accessible in the Wake of Legal Reforms: A Framework and Six Case Studies. New York: Guttmacher Institute; 2012. http://clacaidigital.info:8080/xmlui/handle/123456789/288. [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software (Version 14) College Station, TX: StataCorp LP; 2014. [Google Scholar]
- Statistics South Africa. Gender Statistics in South Africa 2011. Pretoria, South Africa: Statistics South Africa; 2013. http://www.statssa.gov.za/publications/Report-03-10-05/Report-03-10-052011.pdf. [Google Scholar]
- Statistics South Africa. Statistical Release P0211. South Africa: 2015. Quarterly Labour Force Survey: Quarter 4, 2014. http://www.statssa.gov.za/publications/P0211/P02114thQuarter2014.pdf. [Google Scholar]
- Stevens M. Maternal Mortality: HIV and Unsafe Abortion – A Silent Epidemic. Agenda. 2012;26(2):44–50. [Google Scholar]
- Trueman K, Gabriel M. Building Alliances from Ambivalence: Evaluation of Abortion Values Clarification Workshops with Stakeholders in South Africa. African Journal of Reproductive Health. 2005;9(3):89. [PubMed] [Google Scholar]
- Trueman KA, Magwentshu M. Abortion in a Progressive Legal Environment: The Need for Vigilance in Protecting and Promoting Access to Safe Abortion Services in South Africa. American Journal of Public Health. 2013;103(3):397–399. doi: 10.2105/AJPH.2012.301194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. Framework of Actions for the Follow-up to the Programme of Action of the International Conference on Population and Development beyond 2014. United Nations Population Fund; 2014. http://icpdbeyond2014.org/uploads/browser/files/93632_unfpa_eng.pdf. [Google Scholar]
- United Nations. News. UN News Centre; 2016. Jan 18, UN Announces That Peru Will Compensate Women in Historic Human Rights Abortion Case. http://www.un.org/apps/news/story.asp?NewsID=53033#.V5VEf67llpQ. [Google Scholar]
- Varga CA. Pregnancy Termination among South African Adolescents. Studies in Family Planning. 2002;33(4):283–298. doi: 10.1111/j.1728-4465.2002.00283.x. [DOI] [PubMed] [Google Scholar]
- Varkey SJ, Ketlhapile M. Communities for Choice: A Manual to Improve Access to AbortionServices. Johannesburg, South Africa: University of Witwatersrand School of Public Health Women’s Health Project; 2001. [Google Scholar]
- Varkey SJ, Fonn S, Ketlhapile M. Health Workers for Choice: A Manual to Improve the Quality of Abortion Services. Johannesburg, South Africa: University of Witwatersrand School of Public Health Women’s Health Project; 2001. [Google Scholar]
- Vincent L. Shaking a Hornets’ Nest: Pitfalls of Abortion Counselling in a Secular Constitutional Order – A View from South Africa. Culture, Health & Sexuality. 2012;14(2):125–138. doi: 10.1080/13691058.2011.627469. [DOI] [PubMed] [Google Scholar]
- Walker C. Conceptualising Motherhood in Twentieth Century South Africa. Journal of Southern African Studies. 1995;21(3):417–437. [Google Scholar]
- Waxman AM, Humphries H, Frohlich J, Dlamini S, Ntombela F. Young Women’s Life Experiences and Perceptions of Sexual and Reproductive Health in Rural KwaZulu-Natal South Africa. Culture, Health & Sexuality. 2016;18(10):1122–1136. doi: 10.1080/13691058.2016.1182215. [DOI] [PubMed] [Google Scholar]
- Wheeler SB, Zullig LL, Reeve BB, Buga GA, Morroni C. Attitudes and Intentions regarding Abortion Provision among Medical School Students in South Africa. International Perspectives on Sexual and Reproductive Health. 2012;38(3):154–163. doi: 10.1363/3815412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, Socioeconomic Status, and Health: Complexities, Ongoing Challenges, and Research Opportunities: Race, SES, and Health. Annals of the New York Academy of Sciences. 2010;1186(1):69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]