Abstract
Background
Antibiotics are frequently prescribed to patients discharged to hospice care despite the shift in goals of care from curative to palliative therapy.
Objective
We aimed to better understand the clinical intentions for antibiotic prescribing on discharge from acute care to hospice care.
Design
Retrospective cohort study.
Setting
544-bed academic, acute-care, tertiary referral hospital in Portland, Oregon.
Participants
149 adult (age ≥18 years) patients who received an outpatient prescription for antibiotics on discharge from an acute care hospital to hospice care between January 1, 2009 and December 31, 2011.
Measurements
We determined whether antibiotics were indicated for treatment of an active infection, palliative treatment, prophylaxis, and/or prescribed per family or patient preference.
Results
Antibiotics were prescribed to 17.6% (n=149) of patients discharged to hospice care over the 3-year study period. Antibiotics were most frequently prescribed for pneumonia (19.5%), urinary tract (18.9%), and gastrointestinal tract infections (17.0%). The explicit rationale for antibiotic prescription was only documented for 72 prescriptions (45.3%). For 84 (52.8%) patients, antibiotics were used to treat an active infection in the hospital. Among prescriptions with a documented rationale, 37.5% indicated that the intent was curative, 26.4% indicated that the intent was prophylaxis, and 22.2% indicated that the intent was to suppress an infection. Additionally, for 19.4% of prescriptions, patient and/or their family members specifically wanted to be treated with antibiotics. Only 9.7% of prescriptions specifically indicated that antibiotics were prescribed for palliative reasons.
Conclusion
Antibiotics were frequently prescribed for treatment of active infection among patients discharged to hospice care. Further research is needed to document antibiotic benefits and risks and optimize medication management for patients at the end of life.
Introduction
Antibiotics are frequently used in hospice care. Approximately 27% of hospice patients receive a least one antibiotic in the final week of life.1 Despite this high prevalence of use, healthcare providers have minimal guidance to support antibiotic decision-making for terminally-ill patients who have forgone further curative therapy. Although medication use in hospice care focuses primarily on symptom management rather than curative therapy, the effectiveness of antibiotics to improve symptoms and quality of life remains largely unkown.2–4 Thus, decisions to use antibiotics must take into account differences in preferences between patients, family members and hospice providers as well as increased risk for adverse events, potential for antibiotic resistance, and costs to the healthcare system.
Several previous studies have described antibiotics use in hospice care.1,5–8 These studies suggest that antibiotics are frequently prescribed for patients with urinary tract, respiratory tract (including pneumonia), skin and soft tissue, and bloodstream infections. However, our analysis of data from a nationally-representative sample of hospice patients observed that only 15% of patients who received antibiotics have a documented infectious diagnosis.1
We previously described the characteristics of patients who received a prescription for antibiotics on discharge to hospice care because these medications are often continued following hospice admission.5 In that study, we also observed that the most frequently prescribed antibiotics were inconsistent with the distribution of documented infections in those patients. Our previous study did not clarify why patients received antibiotics on discharge to hospice care. In this study, we quantified the documented clinical intentions for antibiotics prescribed to patients on discharge from acute care to hospice care. A better understanding of these intentions and contextual variables around these prescribing decisions may inform interventions to optimize their use in patients at the end of life.
Methods
Study Design and Patient Population
This was a retrospective cohort study of adult (age ≥18 years) patients that received an outpatient prescription for antibiotics on discharge from Oregon Health & Science University Hospital (OHSU) to hospice care between January 1, 2009 and December 31, 2011. During this period, OHSU was a 544-bed academic, acute-care, tertiary referral hospital in Portland, Oregon. These patients and patient characteristics have been described in a previous study.5 Briefly, patients were identified using discharge disposition data collected by the Department of Care Management and medication data on the patients’ discharge summary in the electronic medical record. If patients had multiple discharges to hospice during the study period only the first discharge was included for each patient. We excluded patients who died prior to discharge, whose discharge disposition was unknown, or that were admitted to the hospital for less than 24 hours. This study was approved by the OHSU Institutional Review Board.
Data Collection and Variables
We comprehensively reviewed each patient’s medical record in including daily progress notes, infectious disease and palliative care service consultation notes, and discharge summaries. Data were collected via manual medical record review using a standardized data extraction form created using the Research Electronic Data Capture (REDCap) application.9 Additional administrative, demographic, and comorbidity data were collected from the Pharmacy Research Repository (PHARR), a longitudinal repository of patient healthcare data created in partnership with the Oregon Clinical and Translational Institute (OCTRI) Research Data Warehouse (RDW) at OHSU. We defined aggregate comorbidity burden using the Charlson comorbidity index.10
Our primary outcomes of interest were the infectious indication, documented rationale, and contextual variables (e.g. whether antibiotics were to continue to treat an existing infection, known patient or family preferences) of each antibiotic prescription. Although patients may have had multiple infections during their hospital stay, we specifically focused on the primary indication or indications for which antibiotics were prescribed on discharge to hospice care. Indication data were documented and classified into the following categories: bloodstream infections, septicemia or endocarditis, pneumonia, urinary tract infections, sepsis, gastrointestinal infections, pressure ulcers and skin and soft tissue infections, respiratory tract infections, and other infections. We also documented if patients were prescribed a single antibiotic to treat more than one infection.
We specifically examined the documented rationale for antibiotics, which we categorized as treatment of an active infection or prophylaxis. When the rationale for antibiotic use was not explicitly documented, we made inferences based on documentation of symptoms, diagnoses, and microbiological culture data. We defined prophylactic therapy as receiving antibiotic treatment without a documented infectious indication, with negative culture or lack of culture data, and with no documentation of infectious signs or symptoms. We defined active treatment as receiving antibiotics for a documented infection or for patients with a positive culture and documented associated signs and symptoms of infection. For patients with active infections, we also recorded any additional documented rationale or intention for treatment. Intention of treatment could be classified as curative, palliative, suppressive, and/or prescribed per family or patient preference. Note that these categories were not mutually exclusive.
We determined if the antibiotics prescribed on discharge were a continuation of treatment initiated in the hospital or initiated on discharge to hospice, whether antibiotics were prescribed empirically, and if palliative care specialists were consulted on whether to use antibiotics. Continuation of therapy started in the hospital was defined as antibiotics received in the hospital and on discharge for the same indication and rationale. If the infectious indication or intent for antibiotic treatment upon discharge was not documented, continuation of therapy was determined based on continuation of the current antibiotic at the same dose as prescribed during the hospital visit or documented conversion to another antibiotic. We defined empiric therapy as treatment in the absence of culture data and presence of an active infection based on documented signs and symptoms of infection. Lastly, we assessed whether the palliative care service was consulted or if notes from the palliative care service indicated involvement with discharge medications.
We also examined patient preferences for the intensity of end-of-life care interventions using responses on Physician Orders for Life Sustaining Treatment (POLST) forms. POLST forms are medical orders that clarify patient preferences and direct treatment decisions for patients at end-of-life.11–13 The current POLST form does not directly address use of antibiotics, but had included a specific section on antibiotic use until May 2011. During that time, patients could select from three out-of-hospital orders for antibiotic use: “No antibiotics, use other measures to relieve symptoms”, “Determine use or limitation of antibiotic when infection occurs”, and “Use antibiotics if medically indicated.”
Lastly, we documented the duration of antibiotic use based on the number of days remaining in the antibiotic course at discharge. Total duration of antibiotics (including those prescribed at discharge) was determined from medical record review and the number of days since antibiotic therapy initiation. The number of refills authorized on the discharge prescription was also recorded.
Statistical Analysis
All analyses were descriptive and results are presented as means with standard deviations (SDs), medians with interquartile ranges (IQRs), and frequencies with percentages as appropriate. All analysis was performed using SAS statistical software (version 9.2, Cary, NC).
Results
Among 845 patients discharged to hospice care over the 3-year study period, 149 patients (17.6%) received 159 antibiotic prescriptions on discharge. Individual patient characteristics are described in Table 1. Briefly, mean (SD) age was 63.6 (14.2) years, 91 (61.1%) had a hospice diagnosis of cancer, and 121 (81.2%) were discharged to a community-based hospice. Most patients (84.8%) had a palliative care consultation during their admission prior to hospital discharge; however only 61.7% of palliative care consultations specifically addressed discharge medications.
Table 1.
Characteristics of patients discharged to hospice care with a prescription for antibiotics (n=149).
| Characteristic | n (%) |
|---|---|
| Mean (standard deviation) age, years | 63.6 (14.2) |
| Male sex | 78 (52.4) |
| Charlson Comorbidity Index Score; Median (Interquartile range) | 8.0 (5.0 to 10.0) |
| Cancer as hospice admission diagnosis | 91 (61.1) |
| Discharged to an inpatient hospice | 28 (18.8) |
| Palliative care consultation on index admission | 128 (84.8) |
| Length of index hospital stay > 7 days | 69 (46.4) |
| POLST form completed and on file with medical record | 92 (61.7) |
| Physician Orders for Life Sustaining Treatment (POLST) (n = 92) | |
| Cardiopulmonary Resuscitation (CPR) | |
| Attempt Resuscitation/CPR | 11 (12.0) |
| Do Not Attempt Resuscitation | 81 (88.0) |
| Medical Interventions (n=90) | |
| Comfort Measures Only | 58 (64.4) |
| Limited Treatment | 24 (26.7) |
| Full Treatment | 8 (8.9) |
| Artificially-administered Nutrition (n=83) | |
| Long-term artificial nutrition by tube | 9 (10.8) |
| Defined trial period of artificial nutrition by tube | 12 (14.5) |
| No artificial nutrition by tube | 62 (74.7) |
| Antibiotics (n=72) | |
| Use antibiotics when medically indicated | 34 (47.2) |
| Determine use/limitation of antibiotics when infection occurs | 31 (43.1) |
| No Antibiotics. Use other measures to relieve symptoms | 7 (9.7) |
A POLST form was documented as having been completed for 104 (70.3%) patients. However, only 92 patients (61.7%) had a POLST form available to view in the medical record that included specific orders for the degree of life-sustaining measures they would like implemented. Documented POLST orders are displayed in Table 1. Orders for antibiotic use were only available for 75 (48.3%) patients in our study. Most forms documented orders to use antibiotics if medically indicated (47.2%) or to determine use and limitations of antibiotics at the time an infection occurred (43.1%). Only 7 forms (9.7%) contained orders to avoid future antibiotic use.
The explicit rationale for antibiotic prescription on discharge was only documented in the medical record for 72 (45.3%) prescriptions (data not shown). In the majority (79.9%) of cases, antibiotics prescribed on discharge were to continue a course started in the hospital, and 141 patients (72.3%) were continued on the same class of antibiotics. However, only half (50.3%) of these patients had an infection that was verified by culture data before discharge. For 84 (52.8%) patients, antibiotics were given for treatment of an active infection in the hospital. In 25 patients (15.7%), antibiotics were prescribed as prophylaxis based on our definition. Among prescriptions with an explicit rationale documented in the medical record, 37.5% (n=27) indicated that the intent was curative, 26.4% (n=19) indicated that the intent was prophylaxis, and 22.2% (n=16) indicated that the intent was to suppress an infection. Additionally, for 19.4% (n=14) of prescriptions, patients and/or their family members specifically wanted treatment with antibiotics. Only 9.7% (n=7) of prescriptions specifically indicated that antibiotics were prescribed for palliative reasons.
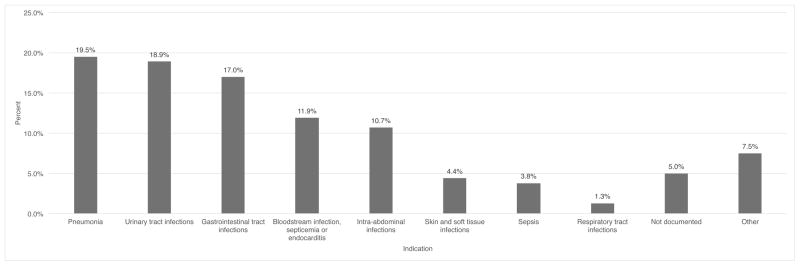
The distribution of indications for antibiotic prescriptions is displayed in the Figure. These data are also displayed stratified by active infection status along with the intended duration of treatment in Table 2. The most frequently documented indications were pneumonia (19.5%), UTIs (18.9%), and gastrointestinal infections (17.0%). However, a significant proportion of patients also received prescriptions for typically more serious infections including intra-abdominal infections (10.7%) and bloodstream infections, septicemia or endocarditis (11.9%). The median duration of antibiotic prescriptions ranged from 8.5 to 26 days and varied by indication.
Figure.
Distribution of indications for antibiotics prescribed on discharge to hospice care (n=159)
Table 2.
Indication for antibiotics prescribed on discharge to hospice care stratified by active infection status and intended duration of treatment (n=159)
| Total | No Infection | Active Infection | Intended Duration of Treatment (days) | |
|---|---|---|---|---|
| (n = 159) | (n = 75) | (n = 84) | Median (IQR) | |
| Pneumonia | 31 (19.5) | 9 (12.0) | 22 (26.2) | 10 (7–14) |
| Urinary tract infections | 30 (18.9) | 7 (9.3) | 23 (27.4) | 8.5 (7–14) |
| Gastrointestinal tract infections | 27 (17.0) | 9 (12.0) | 18 (21.4) | 14 (10–24) |
| Bloodstream infection, septicemia or endocarditis | 19 (11.9) | 12 (16.0) | 7 (8.3) | 19 (14–23) |
| Intra-abdominal infections | 17 (10.7) | 12 (16.0) | 5 (6.0) | 26.5 (10.5–34.5) |
| Skin and soft tissue infections | 7 (4.4) | 4 (5.3) | 3 (3.6) | 12 (10–20) |
| Sepsis | 6 (3.8) | 5 (6.7) | 1 (1.2) | 21 (18–30) |
| Respiratory tract infections | 2 (1.3) | 1 (1.3) | 1 (1.2) | 20 (10–30) |
| Not documented | 8 (5) | 7 (9.3) | 1 (1.2) | 17 (7–30) |
| Other | 12 (7.5) | 9 (12.0) | 3 (3.6) | 21 (10–30) |
Discussion
We aimed to better understand the clinical intentions of antibiotics prescribed to patients on discharge to hospice care. Improving this understanding could help to guide medication decisions and optimize transitions of care in this patient population. We observed that patients were frequently prescribed antibiotics to continue or complete treatment that was initiated in the hospital and that most patients received antibiotics for treatment of an active infection. Furthermore, most patients lacked explicit documentation of the rationale for antibiotic treatment. Among patients with explicit documentation, the most common clinical rationales for antibiotic prescriptions were curative or suppressive treatment or prophylaxis. In addition, clinical notes frequently indicated a patient or family member preference for antibiotic use. In contrast, we rarely observed specific intentions to manage symptoms of an infection.
The most frequently documented indications were pneumonia, UTIs and gastrointestinal infections. However, a significant proportion of patients also received prescriptions for typically more serious infections including intra-abdominal infections and bloodstream infections or endocarditis. The intended duration of antibiotic prescriptions varied by indication. Interestingly, patients receiving treatment for intra-abdominal infections and bloodstream infections were less likely to have an active infection, but more likely to receive treatment for a longer duration. In patients with chronic liver disease, long-term treatment with antibiotics is often indicated for secondary prevention of spontaneous bacterial peritonitis which is consistent with our observed data.
A clear understanding of the rationale for continued antibiotic treatment may be especially important for a patient population during the transitions to hospice care and as goals of care change. Previous studies have attempted to identify patients most often prescribed antibiotics at end-of-life.1,5,6 However, few studies have described the clinical intentions of antibiotic prescribed on transition to hospice care. Furthermore, there are few standards of care which provide guidance for use of antibiotics in patients on hospice or at the last stages of life.15 Symptom relief among patients with UTIs and sepsis has been previously documented; however, there is limited evidence on the risks and benefits of antibiotics for other indications in this patient population.4, 14 Similarly, there are limited data regarding the optimal duration of antibiotic treatment. In the absence of these data, documentation of the rationale for continued treatment and emphasis on goal-directed patient education and shared decision making may help to optimize antibiotic use for patients transitioning to hospice care.
Incorporating antibiotic preferences as part of the advanced care planning process may also help optimize antibiotic use in hospice care.13,15 Data from completed POLST forms suggested that most patients either wanted to receive antibiotics if medically indicated or to determine use at the time an infection occurred. Furthermore, clinical notes indicated that nearly 20% of patients and or family members specifically wanted to be treated with antibiotics. Infections are common near the end of life, and may often be the final cause of death. A collaborative evaluation of the patient/family preferences expected benefits, potential adverse effects, and treatment burden would help to improve medication management and align treatment with the patient’s preferences and goals.15–17 Collaborative evaluation and shared decision making between patients, caregivers and providers may be especially important for patients who lack documented rationale for antibiotics or for patients and families who do not specifically request continuation of antibiotics.
The primary limitation of this study was that we relied on documentation in patients’ medical records to discern the rationale and clinical intentions of antibiotics prescriptions. This required us to make some assumptions to determine the rationale for prescribing antibiotics. Our use of standardized abstraction forms aimed to minimize subjective interpretation and misclassification; however, because our definitions were based on information obtained through medical record review and this information was often lacking, some misclassification likely occurred. Hospice care providers relying on patients’ medical records to understand patient care decisions also face this challenge. Furthermore, many factors may contribute to medication decisions on discharge to hospice, which may not be documented in the medical record. Patient and family preferences, symptom severity, and patient prognosis may all contribute to these decisions. In addition, patient preferences and goals of care may change with changes in health status and during or following discussions with providers, palliative care specialists, and family or loved ones. A second limitation is that our data reflect practices at a single academic health center between 2009 and 2011 and thus may not be representative of present time or other hospitals or regions. Furthermore, few patients had a documented clinical rationale for antibiotic use, which limits interpretation of these results. Further research may help characterize rationale for use, benefits of treatment, and risks associated with antibiotic therapy.
In conclusion, our study suggests that acute care providers frequently prescribe antibiotics to patients on discharge to hospice care with the intention of curing infections despite a shift from curative to palliative goals of care. Antibiotics were also frequently prescribed in the absence of culture data and to treat serious, systemic infections. Future work should address clinical outcomes of this patient population and possible adverse events of antibiotic use including antibiotic–resistant infections, readmission to the hospital, and time until death.
Impact Statement.
We certify that this work is novel. To our knowledge, no previous study has described the clinical intentions of antibiotics prescribed to patients on discharge to hospice care. Given the paucity of existing data to support the safety and effectiveness of antibiotic use in hospice patients, these data may inform interventions to optimize their use in patients transitioning to hospice care.
Acknowledgments
Funding Source: This study was supported by the Oregon Clinical and Translational Research Institute funded by National Center for Advancing Translational Sciences award number UL1TR000128.
Footnotes
Conflict of Interest
SAS: No conflicts.
BNN: No conflicts.
EKF: No conflicts.
JPF is a paid consultant for Merck & Co. and Shionogi Inc. and has received research grants and speaking honoraria from Merck & Co.
Author Contributions
Study concept and design (all authors), acquisition of subjects, data, analysis and interpretation of data (all authors), and preparation of manuscript (all authors).
Previous Presentation of Data: These data were for presented in part at the 2015 American Society for Health-System Pharmacists Midyear Clinical Meeting, December 2015, New Orleans, LA.
Sponsor’s Role
This project was supported by a National Institutes of Health Clinical and Translational Science Award. Infrastructure under this award supported data collection, but not the study design, analysis, or preparation of the manuscript.
References
- 1.Albrecht JS, McGregor JC, Fromme EK, et al. A nationwide analysis of antibiotic use in hospice care in the final week of life. J Pain Symptom Manage. 2013;46(4):483–490. doi: 10.1016/j.jpainsymman.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagy-Agren S, Haley H. Management of infections in palliative care patients with advanced cancer. J Pain Symptom Manage. 2002;24(1):64–70. doi: 10.1016/s0885-3924(02)00420-7. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg JH, Albrecht JS, Fromme EK, et al. Antimicrobial use for symptom management in patients receiving hospice and palliative care: a systematic review. J Palliat Med. 2013;16(12):1568–1574. doi: 10.1089/jpm.2013.0276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Nordennen RT, Lavrijsen JC, Vissers KC, et al. Decision making about change of medication for comorbid disease at the end of life: an integrative review. Drug &; Aging. 2014;31(7):501–512. doi: 10.1007/s40266-014-0182-4. [DOI] [PubMed] [Google Scholar]
- 5.Furuno JP, Noble BN, Horne KN, et al. Frequency of outpatient antibiotic prescription on discharge to hospice care. Antimicrob Agents Chemother. 2014;58(9):5473–5477. doi: 10.1128/AAC.02873-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Merel SE, Meier CA, McKinney CM, et al. Antimicrobial use in patients on a comfort care protocol: A retrospective cohort study. J Palliat Med. 2016;19(11):1210–1214. doi: 10.1089/jpm.2016.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stiel S, Krumm N, Pestinger M, et al. Antibiotics in palliative medicine--results from a prospective epidemiological investigation from the HOPE survey. Support Care Cancer. 2012;20(2):325–333. doi: 10.1007/s00520-011-1084-1. [DOI] [PubMed] [Google Scholar]
- 8.Chun ED, Rodgers PE, Vitale CA, et al. Antimicrobial use among patients receiving palliative care consultation. Am J Hosp Palliat Care. 2010;27(4):261–265. doi: 10.1177/1049909109352336. [DOI] [PubMed] [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 11.Hickman SE, Tolle SW, Brummel-Smith K, et al. Use of the physician orders for life-sustaining treatment program in Oregon nursing facilities: beyond resuscitation status. J Am Geriatr Soc. 2004;52(9):1424–1429. doi: 10.1111/j.1532-5415.2004.52402.x. [DOI] [PubMed] [Google Scholar]
- 12.Hickman SE, Keevern E, Hammes BJ. Use of the physician orders for life-sustaining treatment program in the clinical setting: A systematic review of the literature. J Am Geriatr Soc. 2015;63(2):341–350. doi: 10.1111/jgs.13248. [DOI] [PubMed] [Google Scholar]
- 13.The National POLST Paradigm Program. [Accessed August 25, 2017];2017 [on-line]. Available at www.polst.org.
- 14.Helde-Frankling M, Bergqvist J, Bergman P, et al. Antibiotic treatment in end-of-life cancer patients—A retrospective observational study at a palliative care center in Sweden. Cancers. 2016;8(9) doi: 10.3390/cancers8090084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juthani-Mehta M, Malani PN, Mitchell SL. Antimicrobials at the end of life: An opportunity to improve palliative care and infection management. JAMA. 2015;314(19):2017–2018. doi: 10.1001/jama.2015.13080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holmes HM, Todd A. The role of patient preferences in deprescribing. Clin Geriatr Med. 2017;33(2):165–175. doi: 10.1016/j.cger.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 17.Furuno JP, Noble BN, Fromme EK. Should we refrain from antibiotic use in hospice patients? Expert Rev Anti Infect Ther. 2016:1–4. doi: 10.1586/14787210.2016.1128823. [DOI] [PubMed] [Google Scholar]