Abstract
Purpose
Women have a higher prevalence of post-traumatic stress disorder (PTSD) than men, with a peak during the reproductive years. PTSD during pregnancy adversely impacts maternal and infant health outcomes. The objectives of this study were to estimate the prevalence of antepartum PTSD symptoms in a population of pregnant Peruvian women and to examine the impact of number of traumatic events and type of trauma experienced.
Methods
The Traumatic Events Questionnaire was used to collect data about traumatic exposures. The Post-traumatic Stress Disorder Checklist-Civilian Version (PCL-C) was used to assess PTSD. Multivariable logistic regression procedures were used to estimate adjusted odds ratios (aOR) and 95% confidence intervals (95% CI).
Results
3,372 pregnant women were interviewed. Of the 2,920 who reported experiencing one or more traumatic events, 41.8% met criteria for PTSD (PCL-C score ≥26). A quarter of participants had experienced four or more traumas, and 60.5% of those women had PTSD. Interpersonal trauma was most strongly associated with PTSD (aOR, 3.20; 95% CI, 2.74–3.74), followed by unspeakable trauma (aOR, 2.87; 95% CI, 2.35–3.50), and structural trauma (aOR, 1.39; 95% CI, 1.15–1.67).
Conclusions
These findings indicate the high prevalence of PTSD during pregnancy in the Peruvian population, which is relevant to other countries suffering from terrorism, war, or high rates of violence. This underscores the importance of screening for PTSD in pregnancy.
Keywords: PTSD, pregnancy, trauma, Peru, TEQ
Introduction
Post-traumatic stress disorder (PTSD) is characterized by clinically significant distress or functional impairment, as a result of directly experiencing, witnessing, or learning of a loved one’s experience of a traumatic event (e.g., threatened death, serious injury, or sexual violence) (American Psychiatric Association, 2013). Symptoms include re-experiencing the traumatic event, avoiding reminders of the trauma, hyper-arousal, and negative mood states. The lifetime prevalence of PTSD in the United States (US) has been estimated at 6–8% (Kessler et al., 2005; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Pietrzak, Goldstein, Southwick, & Grant, 2011). The global prevalence of PTSD has not been well-characterized, but the World Mental Health (WMH) surveys have identified prevalence in a number of countries ranging from 1–10% (Atwoli, Stein, Koenen, & McLaughlin, 2015; Koenen et al., 2016).
The prevalence of exposure to trauma has been estimated at 50–80%, approximately ten times that of PTSD (Atwoli et al., 2015; Benjet et al., 2016). Trauma exposure is thus more frequent than PTSD, and researchers have begun to focus on the question of what confers susceptibility and resistance. The total burden of trauma experienced has been associated with PTSD. When individuals have had prior traumatic exposures, they are more likely to develop PTSD following a subsequent trauma (Bremner, Southwick, Johnson, Yehuda, & Charney, 1993; Breslau, Chilcoat, Kessler, & Davis, 1999; Karam et al., 2014). PTSD risk is particularly elevated following trauma in adulthood among individuals who suffered severe childhood abuse (Breslau et al., 2014). Trauma type is another variable that impacts the risk of PTSD, with higher rates and greater symptom severity associated with interpersonal trauma (Kessler et al., 2014).
Women are at particularly elevated risk for PTSD during their reproductive years, with a peak around the time of childbirth (Onoye et al., 2013). There are likely hormonal as well as psychological reasons for this (Leeners, Richter-Appelt, Imthurn, & Rath, 2006; Onoye et al., 2013; Seedat, Stein, & Carey, 2005). For women with histories of sexual abuse, the bodily changes, sensations, and obstetric care during pregnancy can trigger memories of abuse (Leeners et al., 2006). Some women become hypervigilant to these experiences, while others report dissociation (Heritage, 1998).
PTSD during pregnancy has been associated with a number of risk behaviors and health consequences. It has been associated with inadequate prenatal care (Kim et al., 2006), smoking during pregnancy (Lopez, Konrath, & Seng, 2011), pre-term birth and low birth weight (Lipkind, Curry, Huynh, Thorpe, & Matte, 2010; Seng, Low, Sperlich, Ronis, & Liberzon, 2011). However, the prevalence of PTSD during pregnancy has not been well-characterized. Two studies have reported the prevalence as 2.3% (Soderquist, Wijma, & Wijma, 2004) and 7.7% (Loveland Cook et al., 2004). A systematic review found that the prevalence of PTSD symptoms during pregnancy has been reported to be as high as 25% (Ross & McLean, 2006). The impact of overall trauma burden and trauma type on antepartum PTSD has not been described. Our group has previously studied the impact of depression and suicidal ideation during pregnancy (Zhong et al., 2016). However, it is not known how number of exposures and type of trauma influence the presence and severity of PTSD in this population. Moreover, few studies have documented the prevalence of trauma exposure and PTSD in pregnant women and even fewer in LMICs (low- and middle-income countries). The prevalence of PTSD among Peruvian women of child-bearing age has not been described in the literature. The objectives of this study were to estimate the prevalence of PTSD symptoms in pregnant Peruvian women and to examine the extent to which number and type of trauma were associated with antepartum PTSD in this population.
Materials & Methods
Participants and Procedure
Participants in this cross-sectional study were women who received prenatal care at the Instituto Nacional Materno Perinatal (INMP) from February 2012 through March 2014 and who enrolled in the ongoing Pregnancy Outcomes, Maternal and Infant Cohort Study (PrOMIS). The INMP is the primary reference establishment for maternal and perinatal care operated by the Ministry of Health of the Peruvian Government. It serves low-income women who are publicly-insured. According to the World Bank, 21.8% of Peruvians were living in poverty in 2015 (World Bank Group, 2016). In the same year, 18,512 women gave birth at INMP. Eligible participants were pregnant women who were at least 18 years of age, initiated prenatal care prior to16 weeks of gestational age, and could speak and read Spanish. Pregnant women were excluded if they were pregnant with twins, had known fetal malformation or had a history of intellectual disability, chronic hypertension, diabetes mellitus, sepsis or renal failure. All participants provided written informed consent prior to interview. The institutional review boards of the INMP, Lima, Peru and the Harvard T. H. Chan School of Public Health, Office of Human Research Administration, Boston, MA, approved all procedures used in this study.
Our study population is derived from information collected from participants who enrolled in the PrOMIS cohort. During the study period, a total of 3,372 participants completed the structured interview, approximately 81% of eligible women who were approached. Details of the study setting and data collection procedures have been described previously (Barrios et al., 2015). Briefly, each participant was interviewed in a private setting at INMP by trained research personnel using a structured questionnaire, which was completed by the interviewer. The questionnaire was used to elicit information regarding maternal sociodemographic and lifestyle characteristics; traumatic exposures and PTSD symptoms. For the analysis described here, we excluded participants who did not endorse any traumatic exposures in their lifetime (N=409) because, by definition, they could not be diagnosed with PTSD (American Psychiatric Association, 2013). The final analysis included 2,920 participants who endorsed at least one traumatic event. Excluded participants did not differ from the rest of the cohort with regard to sociodemographic variables.
Measures
The Traumatic Events Questionnaire (TEQ) was used to collect data about traumatic exposures. The TEQ is an 11-item instrument that assesses nine different types of events (see Table 3), as well as other trauma and unspeakable trauma. For this study, the following item was added to assess pregnancy-related trauma: “Have you ever experienced pregnancy complications (e.g., stillbirth, miscarriage, abruption placentae, or serious genetic abnormality)?” For each event endorsed, participants were asked about the frequency, age at the time of the event, degree of injury, degree of life threat, degree of distress, and degree of how traumatizing the event was at the time of the assessment, using a 7-point Likert scale (Vrana & Lauterbach, 1994). The TEQ was translated into Spanish by a team of bilingual Peruvian clinicians, including co-author SES. It was then back-translated into English and the process was repeated until there was agreement among the translators.
Table 3.
Prevalent PTSD according to lifetime exposure to any specific type of traumatic events (N = 2,920)
| Traumatic events | No PTSD (PCL-C < 26) N = 1699 |
PTSD (PCL-C ≥ 26) N = 1221 | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| N | % | N | % | Unadjusted OR (95% CI) | Adjusted OR (95% CI) 1 | |
| Any specific type of traumatic events | ||||||
| Serious accident, fire, or explosion | ||||||
| No | 1349 | 79.40 | 930 | 76.17 | Reference | Reference |
| Yes | 348 | 20.48 | 289 | 23.67 | 1.21 (1.01, 1.44) | 1.23 (1.03, 1.48) |
| Natural disaster | ||||||
| No | 1398 | 82.28 | 996 | 81.57 | Reference | Reference |
| Yes | 301 | 17.72 | 225 | 18.43 | 1.05 (0.87, 1.27) | 1.09 (0.90, 1.32) |
| Rape, robbery, or assault | ||||||
| No | 1076 | 63.33 | 714 | 58.48 | Reference | Reference |
| Yes | 623 | 36.67 | 507 | 41.52 | 1.23 (1.06, 1.43) | 1.22 (1.05, 1.43) |
| As a child, sexual or physical abuse | ||||||
| No | 1388 | 81.70 | 687 | 56.27 | Reference | Reference |
| Yes | 309 | 18.19 | 532 | 43.57 | 3.48 (2.94, 4.11) | 3.43 (2.89, 4.07) |
| As an adult, unwanted sexual experiences | ||||||
| No | 1629 | 95.88 | 1037 | 84.93 | Reference | Reference |
| Yes | 70 | 4.12 | 184 | 15.07 | 4.13 (3.10, 5.50) | 4.06 (3.03, 5.43) |
| Adult physical abuse | ||||||
| No | 1037 | 61.04 | 844 | 69.12 | Reference | Reference |
| Yes | 184 | 10.83 | 377 | 30.88 | 2.32 (1.95, 2.77) | 2.31 (1.93, 2.77) |
| Witness a violent death | ||||||
| No | 1464 | 86.17 | 954 | 78.13 | Reference | Reference |
| Yes | 235 | 13.83 | 267 | 21.87 | 1.74 (1.44, 2.12) | 1.77 (1.45, 2.15) |
| In serious danger of losing life or of being seriously injured | ||||||
| No | 1404 | 82.64 | 857 | 70.19 | Reference | Reference |
| Yes | 295 | 17.36 | 363 | 29.73 | 2.02 (1.69, 2.40) | 2.03 (1.70, 2.43) |
| Received news of the mutilation, serious injury, or violent or unexpected death of someone close to them | ||||||
| No | 1099 | 64.69 | 708 | 57.99 | Reference | Reference |
| Yes | 600 | 35.31 | 513 | 42.01 | 1.33 (1.14, 1.54) | 1.30 (1.11, 1.51) |
| Pregnancy complications | ||||||
| No | 859 | 50.56 | 601 | 49.22 | Reference | Reference |
| Yes | 840 | 49.44 | 620 | 50.78 | 1.06 (0.91, 1.22) | 1.08 (0.93, 1.26) |
| Other traumatic events | ||||||
| No | 1612 | 94.88 | 1114 | 91.24 | Reference | Reference |
| Yes | 86 | 5.06 | 107 | 8.76 | 1.80 (1.34, 2.42) | 1.76 (1.30, 2.37) |
| Traumatic events unwilling to specify | ||||||
| No | 1578 | 92.88 | 955 | 78.21 | Reference | Reference |
| Yes | 119 | 7.00 | 266 | 21.79 | 3.69 (2.93, 4.65) | 3.51 (2.78, 4.43) |
Abbreviations: TEQ, traumatic event questionnaire; PTSD, Post-Traumatic Stress Disorder; PCL-C, PTSD CheckList – Civilian; OR, odds ratio; CI, confidence interval
Adjusted for maternal age (continuous), race/ethnicity (other vs. Mestizo), and difficulty paying for the very basics (hard vs. not very hard)
The Spanish-language version of the Post-traumatic Stress Disorder Checklist-Civilian Version (PCL-C) was used to assess PTSD symptomatology during the past month. The PCL-C uses 17 items designed to assess PTSD according to the Diagnostic and Statistical Manual of Mental Disorders (DMS-IV) criteria (Weathers, 1991). Each item assesses PTSD symptoms experienced over the past month on a 5-point Likert scale, with a total score ranging from 17–85. The PCL-C has demonstrated internal consistency, inter-rater reliability, test-retest reliability, and convergent validity among both clinical and non-clinical populations (Wilkins, Lang, & Norman, 2011). The Spanish-language version has been found to have similar psychometric properties to the English-language version (Miles, Marshall, & Schell, 2008). A previous study in this population indicated that a score of 26 had good diagnostic efficiency, with a sensitivity of 0.86 and a specificity of 0.63 (Gelaye et al., under review). Therefore, we used a score of 26 or greater to denote significant PTSD symptoms, to which we will refer as prevalent PTSD. Recent data from our team support that a PCL-C score of 26 or higher on the Spanish-language version is associated with an 86% sensitivity and 63% specificity in diagnosing PTSD in a Peruvian population using the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) criteria (Gelaye et al, in review; available upon request). Further, we also examined PTSD using the established cutoff score of 44 or higher, which has a sensitivity of 0.94 and a specificity of 0.86 (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996).
Sociodemographic and other maternal characteristics were categorized as follows: age (18–19, 20–29, 30–34, and ≥35 years); educational attainment (≤6, 7–12, >12 completed years of schooling); maternal ethnicity (Mestizo vs. others); marital status (married/living with partner vs. others); employment during pregnancy (employed vs. not employed); access to basics including food (very hard/hard/somewhat hard vs. not very hard); planed pregnancy (yes vs. no); nulliparous (yes vs. no), and gestational age at interviews (weeks). Maternal early pregnancy body mass index (BMI) was calculated as weight in kilogram divided by in square meters by height (kg/m2). Early pregnancy BMI was categorized as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), or obese (≥30 kg/m2).
Data Analysis
We examined the frequency distributions of maternal characteristics according to PSTD symptoms. When comparing categorical variables, we used Chi-square test, while Student’s t test was used for continuous variables (e.g., maternal age and gestational age). We used two analytical approaches to examine the association between prevalent PTSD and history of traumatic events using logistic regression procedures. First, we evaluated the odds of prevalent PTSD in relation to number of traumatic events as a continuous variable. Next, we assessed the odds of prevalent PTSD across the three groups of traumatic events (1–3, 4–6, ≥7 traumatic events) using logistic regression procedures. Women who endorsed 1–3 traumatic events comprised the reference group with which women in the other two categories were compared. We evaluated the linear trend in the odds of PTSD by treating the three groups as a continuous variable after assigning a score (i.e., 1, 2, 3) for successive groups. Finally, we explored the possibility of non-linear relationship between number of traumatic events and PTSD risk by fitting a multivariate logistic regression that implemented as generalized additive modeling (GAM) procedures with cubic spline functions between the number of traumatic events and prevalent PTSD. Statistical analyses were performed using SAS 9.4 (SAS Institute, 2016) and R software version 3.1.2 (R Foundation for Statistical Computing, 2015). All reported confidence intervals were calculated at the 95% level. All reported p-values are two-tailed and deemed statistically significant at α=0.05.
Results
Selected sociodemographic data and reproductive characteristics of participants are presented in Table 1. The mean age of participants was 28.3 years (Standard Deviation, SD 6.3 years), and the mean gestational age was 9.2 weeks (SD 3.5 weeks). The majority of participants were Mestizo (75.1%), married (80.5%), and with ≤12 years of education (58.1%). Difficulty accessing basic needs, including food, was reported by 51.4% of participants, and 58.5% reported unplanned pregnancy. Approximately 26% of study participants reported at least 4 types of traumatic events in their lifetime. Of the 2,920 who reported experiencing one or more traumatic events in their lives, 41.8% met criteria for PTSD (PCL-C score ≥26). Characteristics of study participants by PTSD are also presented in Table 1. Overall, those with PTSD were more likely to be younger, non-Mestizo ethnicity and to report difficulty accessing basic needs. Those with PTSD were also more likely to report unplanned pregnancy, multiparity, and high frequencies of traumatic events.
Table 1.
Characteristics for women with at least one traumatic event measured by the TEQ (N = 2,920)
| Characteristics | All participants (N = 2,920) | No PTSD (PCL-C < 26) (N = 1,699) | PTSD (PCL-C ≥ 26) (N = 1,221) | P-value | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| n | % | n | % | n | % | ||
| Maternal age (years)1 | 28.3 ± 6.3 | 28.4 ± 6.2 | 28.1 ± 6.4 | 0.32 | |||
| Maternal age (years) | |||||||
| 18–19 | 154 | 5.3 | 71 | 4.2 | 83 | 6.8 | 0.02 |
| 20–29 | 1603 | 54.9 | 942 | 55.4 | 661 | 54.1 | |
| 30–34 | 624 | 21.4 | 370 | 21.8 | 254 | 20.8 | |
| ≥35 | 539 | 18.5 | 316 | 18.6 | 223 | 18.3 | |
| Education (years) | |||||||
| ≤6 | 127 | 4.3 | 65 | 3.8 | 62 | 5.1 | 0.27 |
| 7–12 | 1570 | 53.8 | 918 | 54.0 | 652 | 53.4 | |
| >12 | 1216 | 41.6 | 711 | 41.8 | 505 | 41.4 | |
| Mestizo Ethnicity | 2194 | 75.1 | 1343 | 79.0 | 851 | 69.7 | <0.0001 |
| Married/living with partner | 2350 | 80.5 | 1386 | 81.6 | 964 | 79.0 | 0.10 |
| Employed during pregnancy | 1341 | 45.9 | 802 | 47.2 | 539 | 44.1 | 0.10 |
| Access to basic foods | |||||||
| Hard | 1501 | 51.4 | 789 | 46.4 | 712 | 58.3 | <0.0001 |
| Not very hard | 1418 | 48.6 | 909 | 53.5 | 509 | 41.7 | |
| Planned pregnancy | 1212 | 41.5 | 742 | 43.7 | 470 | 38.5 | 0.006 |
| Nulliparous | 1407 | 48.2 | 863 | 50.8 | 544 | 44.6 | 0.0008 |
| Gestational age (weeks) at interview1 | 9.2 ± 3.5 | 9.3 ± 3.4 | 9.2 ± 3.5 | 0.45 | |||
| Early pregnancy body mass index (kg/m2) | |||||||
| <18.5 | 53 | 1.8 | 32 | 1.88 | 21 | 1.7 | 0.31 |
| 18.5–24.9 | 1370 | 46.9 | 783 | 46.09 | 587 | 48.1 | |
| 25–29.9 | 1082 | 37.1 | 622 | 36.61 | 460 | 37.7 | |
| ≥30 | 380 | 13.0 | 237 | 13.95 | 143 | 11.7 | |
| Number of traumatic events2 | |||||||
| 1–3 traumatic events | 2045 | 70.0 | 1353 | 79.64 | 692 | 56.67 | <0.0001 |
| 4–6 traumatic events | 745 | 25.5 | 324 | 19.07 | 421 | 34.48 | |
| ≥7 traumatic events | 130 | 4.4 | 22 | 1.29 | 108 | 8.85 | |
Abbreviations: TEQ, traumatic event questionnaire; PTSD, Post-Traumatic Stress Disorder; PCL-C, PTSD CheckList – Civilian Version;
mean ± SD (standard deviation)
409 women without any traumatic event were excluded from this analysis
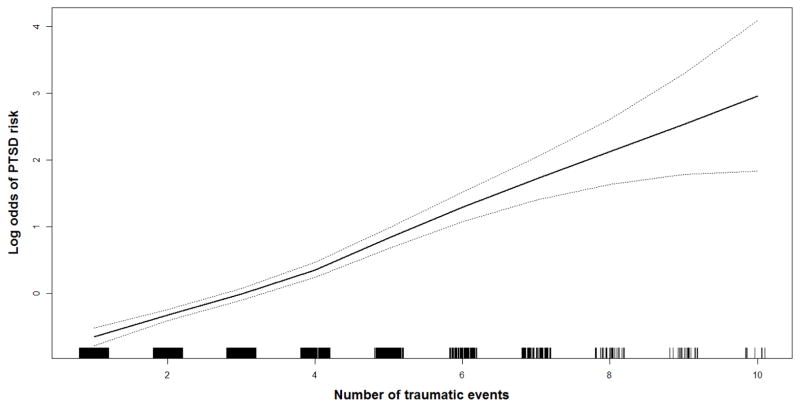
The association between number of traumatic events experienced and prevalent PTSD is presented in Table 2. First we evaluated traumatic events as a continuous score. After adjusting for confounders, a one traumatic event increase was associated with a 46% increased odds of prevalent PTSD (aOR=1.46; 95%CI 1.39–1.54). Next, we assessed the odds of prevalent PTSD across the three groups of traumatic events (1–3, 4–6, ≥7 traumatic events). Participants who reported 4–6 traumatic events had a 2.58-fold increased odds (aOR=2.58; 95%CI 2.16–3.07) of having prevalent PTSD, compared with those who reported only 1–3 traumatic events; those who experienced 7 or more traumatic events had 9.33-fold increased odds (aOR=9.33; 95%CI 5.82–14.97) of prevalent PTSD. The regression splines demonstrated the non-linear associations between the log odds of prevalent PTSD and number of traumatic events (Figure 1). The Akaike information criterion (AIC) for the logistic regression model (Kleinbaum, Kupper, Nizam, & Rosenberg, 2014) was 3700.2 while the AIC for the spline model was 3699.349. This indicates that the spline model is slightly better than the logistic regression using number of traumatic events as a continuous score.
Table 2.
Prevalent PTSD according to lifetime exposure to traumatic events (N = 2,920)
| Number of traumatic events | No PTSD (PCL-C < 26)<br1>N = 1,699 | PTSD (PCL-C ≥ 26)<br1>N = 1,221 | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| N | % | N | % | Unadjusted OR (95% CI) | Adjusted OR (95% CI) 1 | |
| Number of traumatic events2 | 2 [1, 3] | 3 [2, 5] | 1.46 (1.39, 1.53) | 1.46 (1.39, 1.54) | ||
| Number of traumatic events | ||||||
| 1–3 traumatic events | 1353 | 79.64 | 692 | 56.67 | Reference | Reference |
| 4–6 traumatic events | 324 | 19.07 | 421 | 34.48 | 2.54 (2.14, 3.02) | 2.58 (2.16, 3.07) |
| ≥7 traumatic events | 22 | 1.29 | 108 | 8.85 | 9.60 (6.01, 15.32) | 9.33 (5.82, 14.97) |
| P-value for trend | <0.0001 | <0.0001 | ||||
Abbreviations: PTSD, Post-Traumatic Stress Disorder; PCL-C, PTSD CheckList – Civilian; OR, odds ratio; CI, confidence interval
Adjusted for maternal age (continuous), race/ethnicity (other vs. Mestizo), and difficulty paying for the very basics (hard vs. not very hard)
median [first quartile, third quartile]
Figure 1. Relation between number of traumatic events and odds of PTSD (solid line) with 95% CI (dotted lines).
Abbreviations: PTSD, Post-Traumatic Stress Disorder; CI, confidence interval. Vertical bars along X axis indicate distribution of study subjects.
The results remained similar using PCL-C cut-off score of 44 to identify PTSD (Supplementary Table 2). For instance, after adjusting for confounders, women who suffered from 4–6 traumatic events had a 3.55-fold increased odds of PTSD (95% CI: 2.59–4.86) as compared to women with 1–3 traumatic events. Women who suffered 7 or more traumatic events had a 7.89-fold increased odds of PTSD (95% CI: 4.88–12.73) as compared to women with 1–3 traumatic events.
We next evaluated the association of specific types of traumatic events with PTSD. These findings are presented in Table 3. The events that were most frequently experienced by participants with prevalent PTSD were pregnancy complications (50.8%), child physical or sexual abuse (43.6%), receiving news of the mutilation, serious injury or unexpected death of a loved one (42.0%), and rape, robbery or assault (41.5%). Among the 2,920 participants who had experienced one or more traumatic events, unwanted sexual contact as an adult was associated with a 4.06-fold increased odds (aOR=4.06; 95%CI 3.03–5.43) of having PTSD. Child physical or sexual abuse was associated with a 3.43-fold increased odds (aOR=3.43; 95%CI 2.89–4.07) of having PTSD. Adult physical abuse was associated with a 2.31-fold increased odds (aOR=2.31; 95%CI 1.93–2.77) of having PTSD. Life-threatening injury was associated with a 2.03-fold increased odds (aOR=2.03; 95%CI 1.70–2.43) of having PTSD. Witnessing a violent death was associated with a 1.77-fold increased odds (aOR=1.77; 95%CI 1.45–2.15) of having PTSD. Experiencing a serious accident was associated with a 1.23-fold increased odds (aOR=1.23; 95%CI 1.03–1.48) of having PTSD. Random violence, such as robbery or assault, was associated with a 1.22-fold increased odds (aOR=1.22; 95%CI 1.05–1.43) of having PTSD. Experiencing a natural disaster was not statistically significantly associated with developing PTSD, nor was experiencing pregnancy complications. In the additional item assessing for pregnancy complications, on average, participants rated the event’s traumatic intensity when it occurred as 7 on a scale from 1 to 7 and as 3, at the time of the assessment. This was the same as random violence and only slightly less traumatic than adult sexual abuse, which was 7 when it occurred and 4 at the time of the assessment.
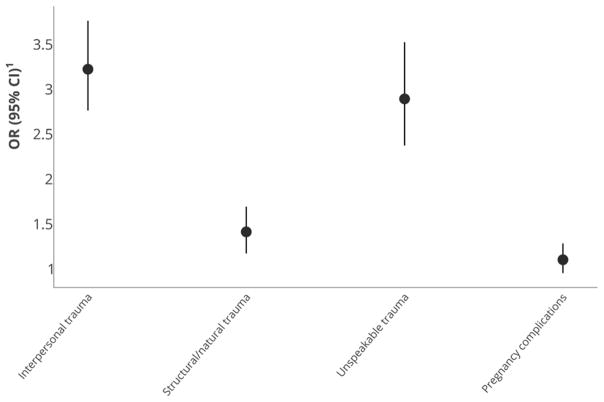
Interpersonal trauma included child and adult physical and sexual abuse; structural trauma included all other specified trauma types: natural disaster, serious accident, fire, explosion, rape, robbery, assault, witness a violent death, in serious danger of losing life, receiving news of violence done to someone close. As shown in Figure 2, interpersonal trauma was most strongly associated with PTSD (aOR=3.20; 95%CI 2.74–3.74), followed by unspeakable trauma (aOR=2.87; 95%CI 2.35–3.50) and structural trauma (aOR=1.39; 95%CI 1.15–1.67).
Figure 2. Prevalent PTSD according to lifetime exposure to types of traumatic events (N = 2,920).
Abbreviations: PTSD, Post-Traumatic Stress Disorder; OR, odds ratio; CI, confidence interval
1Adjusted for maternal age (continuous), race/ethnicity (other vs. Mestizo), and difficulty paying for the very basics (hard vs. not very hard)
Discussion
The prevalence of PTSD symptomatology in our study population was 36.2%, more than four times the lifetime prevalence that has been reported in the US and globally (Atwoli et al., 2015; Kessler et al., 2005; Kessler et al., 1995; Pietrzak et al., 2011). It is 5–15 times the prevalence that has been reported during pregnancy (Loveland Cook et al., 2004; Ross & McLean, 2006; Soderquist et al., 2004). While the trauma exposure rate of 86.6% was slightly higher than what has been previously reported (50–80%) (Atwoli et al., 2015), the rate of PTSD per exposed individual (41.8%) was more than twice that of previous estimates (2–20%) (Atwoli et al., 2015; Breslau, Peterson, Poisson, Schultz, & Lucia, 2004). The causes of this are likely multifactorial, relating to quantity of trauma experienced, type of trauma, pregnancy-specific factors, and sociocultural factors. For over thirty years, Perü has been a country affected by numerous acts of terrorism and violence incited by the communist group Sendero Luminoso (“Shining Path”), which sought the removal of the existing Peruvian government (Borba et al., 2015). 69,280 victims were killed in the internal conflict between 1980–2000 (Barrientos Hernandez & Church, 2003), contributing to a culture of violence and collective trauma.
The women in our study experienced a high burden of trauma. A quarter (25.9%) of participants had experienced four or more different types of traumatic events, and a majority of those women (60.5%) reported experiencing symptoms of PTSD. This is consistent with previous findings that suggest that more traumatic exposures increases PTSD risk (Bremner et al., 1993; Breslau et al., 1999; Post & Weiss, 1998). Our study also found higher prevalence of PTSD associated with interpersonal trauma; women who reported interpersonal trauma had a 3.20-fold increased risk of PTSD compared to women who experienced any trauma. This is consistent with what previous studies have documented (Frans, Rimmo, Aberg, & Fredrikson, 2005; Kessler et al., 2014; Seedat, le Roux, & Stein, 2003). Frans et al found that sexual assault was associated with a five-fold increase (OR=5.02; 95%CI 2.87–8.87) in PTSD risk in the general population in Sweden. We also found that unspeakable trauma, events that participants declined to specify, was associated with a 2.87-fold increased risk of PTSD, nearly as high as interpersonal trauma, compared with structural trauma (1.39-fold) and pregnancy complications (1.08-fold). This finding has not been described in the literature. We speculate that because of the similar impact upon PTSD, as well as the shame associated with interpersonal trauma and the fear of retaliation by the perpetrator, interpersonal trauma is more likely to be experienced as unspeakable than other types of trauma. With 11.4% of participants reporting such experiences, the actual rate of interpersonal trauma may be even higher than estimated.
Childhood physical and sexual abuse in particular were strong predictors of PTSD in our study population, which can be explained by the finding that women with histories of childhood sexual abuse report flashbacks and other re-experiencing symptoms during pregnancy (Leeners et al., 2006). This has been linked both to the physical sensations of pregnancy and childbirth and the anxiety women have about what may happen to their children, given what they experienced during childhood (Buist, 1998; Farber, Herbert, & Reviere, 1996; Heritage, 1998; Leeners et al., 2006). Adult sexual abuse was associated with a higher odds of PTSD than childhood physical and sexual abuse. Given our prior findings demonstrating that childhood abuse as a significant predictor of adult abuse and re-victimization (Barrios et al., 2015), it is likely that the subset of child abuse survivors who experienced the most severe psychological sequelae went on to suffer further abuse as adults and to develop PTSD.
There were a number of limitations to this study. First, history of trauma and PTSD symptoms were assessed based on self-report. There is a risk of systematic non-disclosure leading to misclassification. There is also a risk of non-systematic recall bias, which could lead to underestimating the association. Previous studies have reported that individuals are likely to minimize past trauma in the interview setting (Ellsberg, Winkvist, Pena, & Stenlund, 2001). For example, longitudinal studies of adults whose childhood abuse was documented have found that participants tend to underestimate actual experiences of childhood abuse (Della Femina, Yeager, & Lewis, 1990; Williams, 1995). PTSD symptoms can also increase reporting of trauma, leading to an over-estimation of the association between trauma and PTSD (Koenen, Stellman, Dohrenwend, Sommer, & Stellman, 2007).
To mitigate the risk of systematic reporting errors, a standard questionnaire was used to collect information from all study participants. Second, the research team worked to make sure that neither the interviewers nor study participants were aware of the research hypotheses. Third, this is a prospective cohort study that will collect data on pregnancy and fetal outcomes, but that data is not available at this time. We did not have information on the temporal relationship between the onset and end of the reported trauma exposures, which precludes the determination of causality in this relationship. Nor did we have data on onset of PTSD or lifetime history of PTSD. Finally, results from our hospital-based study may not be applicable to the general population of women because women seeking care at INMP are primarily from a low socioeconomic background and may have high-risk pregnancies. However, our study provides data on an important population in Peru, a population of pregnant women that has been documented to have a high burden of social, medical and mental health problems (Barrios et al., 2015; Cripe, Sanchez, Gelaye, Sanchez, & Williams, 2011; Gelaye, Lam, Cripe, Sanchez, & Williams, 2010; Perales et al., 2009; Zhong et al., 2016)
Conclusions
These findings indicate that a greater trauma burden and exposure to interpersonal trauma, particularly sexual trauma, are both predictive of PTSD in pregnant women. Further research is needed to determine whether other pregnant populations with lower rates of trauma exposure have the same risk factors for PTSD. Identifying and treating PTSD in pregnant women is important to prevent risk behaviors and negative health consequences to women and their offspring, including pre-term birth and low birth weight (Lipkind et al., 2010; Seng et al., 2011). It is noteworthy that while structural trauma, like natural disasters, draws international attention, interpersonal trauma is associated with greater psychological impact. However, individuals who have already suffered PTSD in association with previous trauma are more likely to develop symptoms following subsequent trauma exposure. Thus, in a setting where interpersonal violence is common and treatment resources are limited, the consequences of a structural trauma in those who have experienced interpersonal violence would likely be more devastating than they would be in a setting with a lower incidence of interpersonal violence, illustrating how physical and sexual abuse can have extensive unanticipated downstream effects.
Supplementary Material
Acknowledgments
This research was supported by awards from the National Institutes of Health (T32-MH-093310 and R01-HD-059835). The NIH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication. The authors wish to thank the dedicated staff members of Asociacion Civil Proyectos en Salud (PROESA), Peru and Instituto Materno Perinatal, Peru for their expert technical assistance with this research.
Footnotes
Compliance with Ethical Standards
Disclosure of potential conflicts of interest: No disclosures.
Research involving human participants: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Atwoli L, Stein DJ, Koenen KC, McLaughlin KA. Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr Opin Psychiatry. 2015;28(4):307–311. doi: 10.1097/YCO.0000000000000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrientos Hernandez DH, Church AL. Terrorism in Peru. Prehosp Disaster Med. 2003;18(2):123–126. doi: 10.1017/s1049023x0000087x. [DOI] [PubMed] [Google Scholar]
- Barrios YV, Gelaye B, Zhong Q, Nicolaidis C, Rondon MB, Garcia PJ, … Williams MA. Association of childhood physical and sexual abuse with intimate partner violence, poor general health and depressive symptoms among pregnant women. PLoS One. 2015;10(1):e0116609. doi: 10.1371/journal.pone.0116609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, … Koenen KC. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol Med. 2016;46(2):327–343. doi: 10.1017/S0033291715001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Borba CP, Gelaye B, Zayas L, Ulloa M, Lavelle J, Mollica RF, Henderson DC. Making strides towards better mental health care in Peru: Results from a primary care mental health training. Int J Clin Psychiatry Ment Health. 2015;3(1):9–19. doi: 10.12970/2310-8231.2015.03.01.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry. 1993;150(2):235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156(6):902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Koenen KC, Luo Z, Agnew-Blais J, Swanson S, Houts RM, … Moffitt TE. Childhood maltreatment, juvenile disorders and adult post-traumatic stress disorder: a prospective investigation. Psychol Med. 2014;44(9):1937–1945. doi: 10.1017/S0033291713002651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC. Estimating post-traumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychol Med. 2004;34(5):889–898. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- Buist A. Childhood abuse, postpartum depression and parenting difficulties: a literature review of associations. Aust N Z J Psychiatry. 1998;32(3):370–378. doi: 10.3109/00048679809065529. [DOI] [PubMed] [Google Scholar]
- Cripe SM, Sanchez SE, Gelaye B, Sanchez E, Williams MA. Association between intimate partner violence, migraine and probable migraine. Headache. 2011;51(2):208–219. doi: 10.1111/j.1526-4610.2010.01777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Della Femina D, Yeager CA, Lewis DO. Child abuse: adolescent records vs. adult recall. Child Abuse Negl. 1990;14(2):227–231. doi: 10.1016/0145-2134(90)90033-p. [DOI] [PubMed] [Google Scholar]
- Ellsberg MC, Winkvist A, Pena R, Stenlund H. Women’s strategic responses to violence in Nicaragua. J Epidemiol Community Health. 2001;55(8):547–555. doi: 10.1136/jech.55.8.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farber EW, Herbert SE, Reviere SL. Childhood abuse and suicidality in obstetrics patients in a hospital-based urban prenatal clinic. Gen Hosp Psychiatry. 1996;18(1):56–60. doi: 10.1016/0163-8343(95)00098-4. [DOI] [PubMed] [Google Scholar]
- Frans O, Rimmo PA, Aberg L, Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr Scand. 2005;111(4):291–299. doi: 10.1111/j.1600-0447.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- Gelaye B, Lam N, Cripe SM, Sanchez SE, Williams MA. Correlates of violent response among Peruvian women abused by an intimate partner. J Interpers Violence. 2010;25(1):136–151. doi: 10.1177/0886260508329127. [DOI] [PubMed] [Google Scholar]
- Heritage C. Working with childhood sexual abuse survivors during pregnancy, labor, and birth. J Obstet Gynecol Neonatal Nurs. 1998;27(6):671–677. doi: 10.1111/j.1552-6909.1998.tb02637.x. [DOI] [PubMed] [Google Scholar]
- Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, … Koenen KC. Cumulative traumas and risk thresholds: 12-month PTSD in the World Mental Health (WMH) surveys. Depress Anxiety. 2014;31(2):130–142. doi: 10.1002/da.22169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Rose S, Koenen KC, Karam EG, Stang PE, Stein DJ, … Bromet E. How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO World Mental Health Surveys. world psychiatry. 2014;13:265–274. doi: 10.1002/wps.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kim HG, Mandell M, Crandall C, Kuskowski MA, Dieperink B, Buchberger RL. Antenatal psychiatric illness and adequacy of prenatal care in an ethnically diverse inner-city obstetric population. Arch Womens Ment Health. 2006;9(2):103–107. doi: 10.1007/s00737-005-0117-5. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, Kupper LL, Nizam A, Rosenberg ES. Applied regression analysis and other mutlivariable methods. 5. Boston, MA: Cengage Learning; 2014. [Google Scholar]
- Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Stein DJ, Karam EG, … Kessler RC. Posttraumatic Stress Disorder in the World Mental Health Surveys. Depress Anxiety. 2016 In press. [Google Scholar]
- Koenen KC, Stellman SD, Dohrenwend BP, Sommer JF, Jr, Stellman JM. The consistency of combat exposure reporting and course of PTSD in Vietnam War veterans. J Trauma Stress. 2007;20(1):3–13. doi: 10.1002/jts.20191. [DOI] [PubMed] [Google Scholar]
- Leeners B, Richter-Appelt H, Imthurn B, Rath W. Influence of childhood sexual abuse on pregnancy, delivery, and the early postpartum period in adult women. J Psychosom Res. 2006;61(2):139–151. doi: 10.1016/j.jpsychores.2005.11.006. [DOI] [PubMed] [Google Scholar]
- Lipkind HS, Curry AE, Huynh M, Thorpe LE, Matte T. Birth outcomes among offspring of women exposed to the September 11, 2001, terrorist attacks. Obstet Gynecol. 2010;116(4):917–925. doi: 10.1097/AOG.0b013e3181f2f6a2. [DOI] [PubMed] [Google Scholar]
- Lopez WD, Konrath SH, Seng JS. Abuse-related post-traumatic stress, coping, and tobacco use in pregnancy. J Obstet Gynecol Neonatal Nurs. 2011;40(4):422–431. doi: 10.1111/j.1552-6909.2011.01261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loveland Cook CA, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME. Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstet Gynecol. 2004;103(4):710–717. doi: 10.1097/01.AOG.0000119222.40241.fb. [DOI] [PubMed] [Google Scholar]
- Miles JN, Marshall GN, Schell TL. Spanish and English versions of the PTSD Checklist-Civilian version (PCL-C): testing for differential item functioning. J Trauma Stress. 2008;21(4):369–376. doi: 10.1002/jts.20349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F. Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Arch Womens Ment Health. 2013;16(6):453–463. doi: 10.1007/s00737-013-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perales MT, Cripe SM, Lam N, Sanchez SE, Sanchez E, Williams MA. Prevalence, types, and pattern of intimate partner violence among pregnant women in Lima, Peru. Violence Against Women. 2009;15(2):224–250. doi: 10.1177/1077801208329387. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25(3):456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post RM, Weiss SR. Sensitization and kindling phenomena in mood, anxiety, and obsessive-compulsive disorders: the role of serotonergic mechanisms in illness progression. Biol Psychiatry. 1998;44(3):193–206. doi: 10.1016/s0006-3223(98)00144-9. [DOI] [PubMed] [Google Scholar]
- R Foundation for Statistical Computing. R software (Version 3.1.2) Vienna, Austria: 2015. [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. J Clin Psychiatry. 2006;67(8):1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS Analytics Pro 9.4. Cary, NC: SAS Institute Inc; 2016. [Google Scholar]
- Seedat S, le Roux C, Stein DJ. Prevalence and characteristics of trauma and post-traumatic stress symptoms in operational members of the South African National Defence Force. Mil Med. 2003;168(1):71–75. [PubMed] [Google Scholar]
- Seedat S, Stein DJ, Carey PD. Post-traumatic stress disorder in women: epidemiological and treatment issues. CNS Drugs. 2005;19(5):411–427. doi: 10.2165/00023210-200519050-00004. [DOI] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. BJOG. 2011;118(11):1329–1339. doi: 10.1111/j.1471-0528.2011.03071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderquist J, Wijma K, Wijma B. Traumatic stress in late pregnancy. J Anxiety Disord. 2004;18(2):127–142. doi: 10.1016/S0887-6185(02)00242-6. [DOI] [PubMed] [Google Scholar]
- Vrana S, Lauterbach D. Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J Trauma Stress. 1994;7(2):289–302. doi: 10.1007/BF02102949. [DOI] [PubMed] [Google Scholar]
- Weathers FH, JA, Keane TM. PCL-C for DSM-IV. Boston: 1991. [Google Scholar]
- Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety. 2011;28(7):596–606. doi: 10.1002/da.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM. Recovered memories of abuse in women with documented child sexual victimization histories. J Trauma Stress. 1995;8(4):649–673. doi: 10.1007/BF02102893. [DOI] [PubMed] [Google Scholar]
- World Bank Group. Country Data Peru. 2016 Retrieved from: http://data.worldbank.org/country/Peru.
- Zhong QY, Wells A, Rondon MB, Williams MA, Barrios YV, Sanchez SE, Gelaye B. Childhood abuse and suicidal ideation in a cohort of pregnant Peruvian women. Am J Obstet Gynecol. 2016;215(4):501.e501–508. doi: 10.1016/j.ajog.2016.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.