Abstract
BACKGROUND
Hip fractures are a significant source of morbidity, mortality and costs among US nursing home (NH) residents. Understanding variation in hip fracture rates across NH facilities and states is important for guiding quality improvement and policymaking efforts.
OBJECTIVES
To quantify the variation in hip fracture incidence across US NH facilities and states, and examine how hip fracture incidence varies according to facility- and state-level characteristics.
DESIGN
Retrospective cohort using linked national Minimum Data Set assessments; Online Survey, Certification and Reporting records; and Medicare claims.
SETTING
US NHs with ≥ 100 beds.
PARTICIPANTS
201,892 NH residents who qualified as long-stay between May 1, 2007 and April 30, 2008, across 1,481 facilities and 46 US states.
MEASUREMENTS
Incident hip fractures were ascertained using Medicare Part A diagnostic codes. Each resident was followed for up to 2 years.
RESULTS
The mean adjusted incidence rate of hip fractures across facilities was 3.13 (95% CI, 3.01–3.26) per 100 person-years, and ranged from 1.20 (95% CI, 1.15–1.26) to 6.40 (95% CI, 6.07–6.77). Facilities with the highest rates of hip fracture had greater percentages of residents taking psychoactive medications (27.17% versus 24.77% for top versus bottom tertile), and fewer nursing and direct care hours/resident/day (3.43 versus 3.53 and 3.22 versus 3.29 for top versus bottom tertile, respectively). The combination of state and facility characteristics explained 6.7% of the variation in hip fracture, while resident characteristics explained 7.6%.
CONCLUSIONS
Much of the variation in hip fracture incidence remained unexplained, though these findings indicate that potentially modifiable state and facility characteristics like psychoactive drug prescribing and minimum staffing requirements could be addressed to help reduce the rates of hip fracture in US NHs.
Keywords: Nursing homes, long-term care, hip fracture, Medicare, health services research
INTRODUCTION
Prior studies suggest that nursing home (NH) facility characteristics and care practices influence the risk of adverse events among nursing home (NH) residents.[1–3] Recent studies have shown that differences in antipsychotic prescribing, hospitalization rates, and other health care events across NH facilities cannot fully be explained by differences in resident characteristics.[1, 4–6] Facility characteristics such as profit status, nurse staffing, NH size, and chain affiliation are likely contributors to NH residents’ risk of adverse outcomes.[1, 2, 7]
Facility practices are influenced locally by the medical director and other NH staff, and also by state regulations. Local practices, such as use of an intervention to reduce recurrent falls, may influence adverse events in a specific facility or chain.[8, 9] State regulations, such as the minimum staffing level required in NHs, could influence the ability of facilities in a state to provide the level of care necessary to prevent falls and fractures.[10] Policies and regulations vary considerably across states.[11]
Hip fractures are significant adverse events in US NHs given their high associated morbidity, mortality and expense.[12, 13] Resident specific risk factors for hip fracture have been well established and overlap with risk factors for falls, as hip fractures often occur in the setting of a fall.[14–17] Prior work has documented meaningful variation in the rates of hip fracture among NH residents across US states and geographic regions, even after adjusting for resident age and sex.[16, 18] While resident characteristics are likely the major determinants of variation in hip fracture, facility policies and state regulations also may explain some of the variation. It is important to identify facility and state practices because these factors may be more modifiable than person-level characteristics.
Therefore, the objectives of our study were to 1) determine whether variation exists in hip fracture rates across US NH facilities after adjusting for individual risk factors for hip fracture, 2) identify facility-level and state-level practices associated with higher hip fracture rates, and 3) quantify the variation in hip fracture that is attributable to measured resident, facility and state level characteristics. We hypothesized that differences among facility or state practices will explain much of the observed variation in hip fracture, thereby helping to identify potentially modifiable targets for interventions that aim to prevent injurious falls and hip fractures in US NHs.
METHODS
Data Source
We linked 100% of 2007–2010 Medicare Part A claims to NH resident assessments (Minimum Data Set (MDS), version 2.0) as well as the Online Survey, Certification and Reporting (OSCAR) data for the NH facilities, using unique, individual identifiers for all NH residents enrolled in a fee-for-service Medicare program.[19] The MDS is a comprehensive, clinical assessment instrument used to regularly document health status of NH residents, including demographic, medical, functional status, psychological, and cognitive status information.[20–22] The OSCAR data were used to characterize state- and facility-level policies, including NH staffing levels and various quality measures.[23, 24] A previously validated residential history file algorithm was used to track the timing and location of health service use.[19]
Study Design and Population
This was a nationally representative retrospective cohort study. The study sample included 892,843 eligible long-stay residents, defined as those with ≥100 days in the same nursing facility with no more than 10 consecutive days outside the facility between May 1, 2007 and April 30, 2008. These individuals had at least 6 months of Medicare Part A enrollment, were at least 65 years of age, had an MDS assessment within 100 days of study entry (the day they became long-stay), and were not enrolled in hospice. More details about this cohort have been previously published.[12] For the current study, we excluded residents in facilities with less than 100 residents, as most NH standards and regulations apply to facilities with more than 100 residents or beds.[25] Rates of hip fracture are greatest in the first 100 days following NH admission while in subacute care.[12] Therefore, upon examining the distribution of the number of admissions per bed[26], we excluded residents in facilities that had greater than 2% of unique admissions per bed in an effort to exclude facilities with large post-acute populations since our focus was on the long-stay NH resident population.[26] The final study sample included 201,892 long-stay residents across 1,481 NH facilities and 46 US states. Figure 1 provides the study enrollment flow chart and Supplementary Table S1 the distribution of facilities by state.
Figure 1.
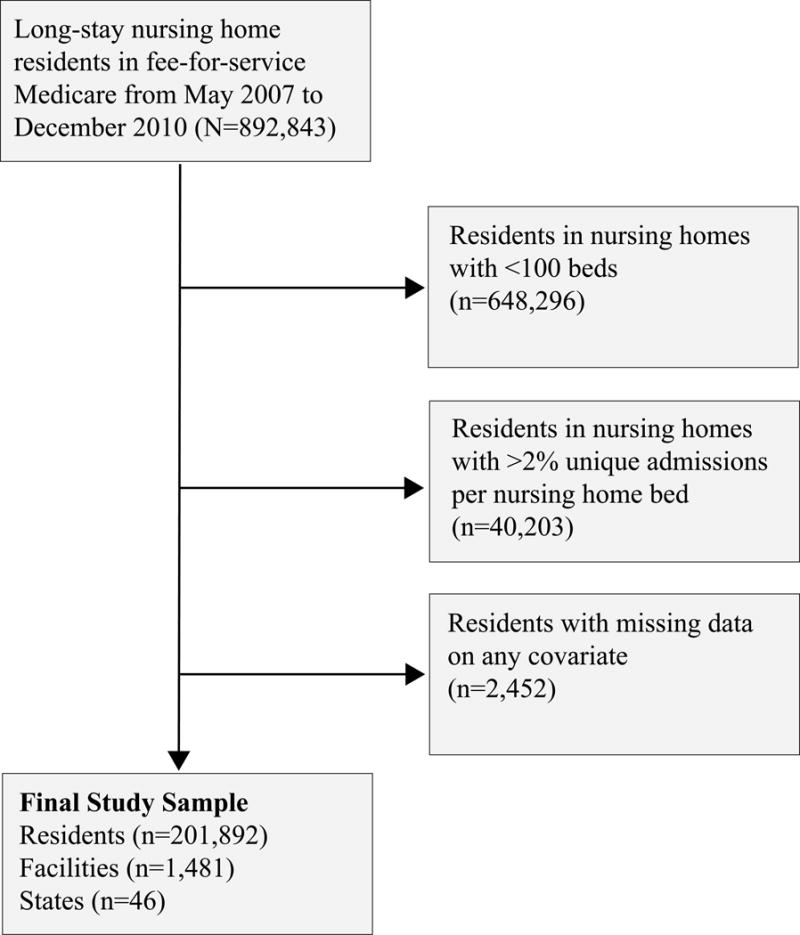
Study Sample Selection
Hip Fracture Ascertainment and Follow-up
The outcome was incident hospitalized hip fractures, which were ascertained using Medicare Part A claims. A hip fracture was defined as a hospitalization with the principal or secondary International Classification of Diseases, Ninth Revision (ICD-9) discharge diagnosis of 820.xx (fracture of the neck of femur). Follow-up for hip fractures began on the date a resident qualified as long-stay (i.e., day 100 in the same nursing facility; the index date). Residents were followed from the index date until the first event of incident hip fracture, death, 2 years of follow-up, or the end of the study period (April 30, 2010). The 2-year duration of follow-up was selected based on data availability and for consistency with prior published work.[12, 18, 27] Since most hospitalizations are short (<10 days) and long-stay residents return to their NH facilities, residents continued to contribute person-time during hospitalizations for reasons other than hip fracture. To isolate new (rather than prevalent) fractures, we excluded prior hospitalized hip fracture events that occurred within the 100 days prior to the index date.
Measures of Resident Characteristics
Details about the measurement of resident characteristics have been previously described.[12, 16] In order to adjust for resident case-mix, we calculated a validated hip fracture summary risk score for each resident in the study population using the Fracture Risk Assessment in Long term care (FRAiL) model.[16] The FRAiL model has good discrimination and excellent calibration.[16] The pre-index-date variables included in the FRAiL score and thus adjusted for in our analyses were age, race, cognition (cognitive performance score), activities of daily living (ADL) dependence, locomotion dependence, urinary continence, previous fall history, transfer dependence, being easily distracted, wandering, presence of pressure ulcers, body mass index, and diagnosis of osteoarthritis or diabetes. The FRAiL model is calculated separately for men and women, so sex was not included in the calculation. By using a summary score to adjust for resident characteristics in our analyses, we avoided the potential convergence problems that can occur when including an uncommon outcome and a large number of covariates in multilevel models.[4]
Measures of Facility and State Characteristics
State survey agencies are responsible for certifying that NH facilities meet the conditions for participation in Medicare and Medicaid insurance programs, and OSCAR is a compilation of comprehensive data collected by surveyors during their inspections of NH facilities.[28] We identified and ascertained facility-level variables from the OSCAR data based on substantive knowledge and prior literature.[1, 29–31] Facility characteristics included in this study were: percent of residents receiving antipsychotic, antidepressant, antianxiety, psychoactive, and hypnotic drugs; percent of residents who were restrained, or indwelling catheter use; percent receiving a bladder training program, tube feedings, and having advanced directives; total nursing hours/resident/day, total registered nurses/100 beds, average number of prescription drugs per resident, ratio of registered nurses to total nurses, and a count of the number of quality of life deficiencies. These deficiency citations may be used as a measure of NH quality, as facilities are cited when they violate any of the approximately 180 federal requirements/standards.[32]
We additionally examined the state-level variables for each NH facility. We considered the following state-level aggregate characteristics from OSCAR: the percent of facilities that were part of a chain, percent of facilities that were hospital based, occupancy rates, total number of beds, percent of residents paid by Medicaid and Medicare, and percent of facilities that were for profit.[25, 33, 34] Most importantly, we assessed the minimum number of nursing hours/resident legislatively mandated by each state.[25, 33, 34]
Statistical Analyses
After employing descriptive statistics to characterize residents, we calculated the FRAiL case-mix summary score (described above) for each resident with a Fine and Gray competing risk regression model.
Initially, we modeled hip fracture as a count, which allowed us to calculate the hip fracture incidence rate (IR) and 95% CI for each facility using a Poisson regression model. We adjusted estimates for sex and the FRAiL case-mix summary risk score. We graphically illustrated the magnitude of difference in the rate of experiencing a hip fracture when living in a facility one or two standard deviations above and below the mean IR of hip fracture. We classified facilities and states into tertiles, according to their mean adjusted IR of hip fracture. Bivariable analyses were conducted to determine which facility and state characteristics were associated with greater incidence of hip fracture.
We then modeled hip fracture as a dichotomous dependent variable. Doing so allowed us to describe the variation in the incidence of hip fracture due to patient, facility, and state effects versus variation due to random error or “chance”. We constructed multilevel logistic regression models using a three-level structure of residents (level 1) within facilities (level 2) within states (level 3). This model included resident sex and the FRAiL summary risk score as fixed factors. Important facility characteristics, defined as any facility and state level characteristics that were significant at the p ≤ 0.05 level in the bivariable analyses, were also included as fixed factors. The proportions of variance attributable to patient characteristics, facility practices, and state policy characteristics were calculated by dividing the total explained variance from the null model by the explained variance in a given level from conditional models.[35]
Data were analyzed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC) and R, version 3.4 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics Approval
The institutional review board at Hebrew SeniorLife approved the study protocol.
RESULTS
A total of 201,892 long-stay residents were included in our study (Figure 1). The mean age of the residents in the cohort was 84 years (SD 8.0), and 74.5% were women. A total of 80.2% were white, 15.5% were black, and 4.3% identified as other race. During a mean follow-up of 1.5 years (SD, 0.7; median [IQR], 2.0 [0.8–2.0]), 3.1% of the long-stay NH residents experienced a hip fracture.
The mean adjusted IR of hip fractures across facilities was 3.13 (95% CI, 3.01–3.26) per 100 person-years. The adjusted hip fracture IR by facility ranged from 1.20 (95% CI, 1.15–1.26) to 6.40 (95% CI, 6.07–6.77) hip fractures per 100 person-years. A total of 752 facilities had adjusted IRs above the overall mean (mean IR for facilities above the overall mean=3.68 hip fractures/100 person-years, 95% CI 3.53–3.83), while 724 facilities fell below (mean IR for facilities below the overall mean=2.63 hip fractures/100 person-years, 95% CI 2.54–2.74). This distribution of facilities with IRs below and above the mean (i.e., ranked from low to high by IR) is shown in Figure 2. Adjusted hip fracture rates were 1.25 (95% CI 1.19–1.29) times greater in facilities one standard deviation above the mean versus facilities one standard deviation below the mean. The corresponding rate was 1.85 (95% CI 1.76–1.95) times greater for facilities two standard deviations above versus two standard deviations below the mean.
Figure 2.
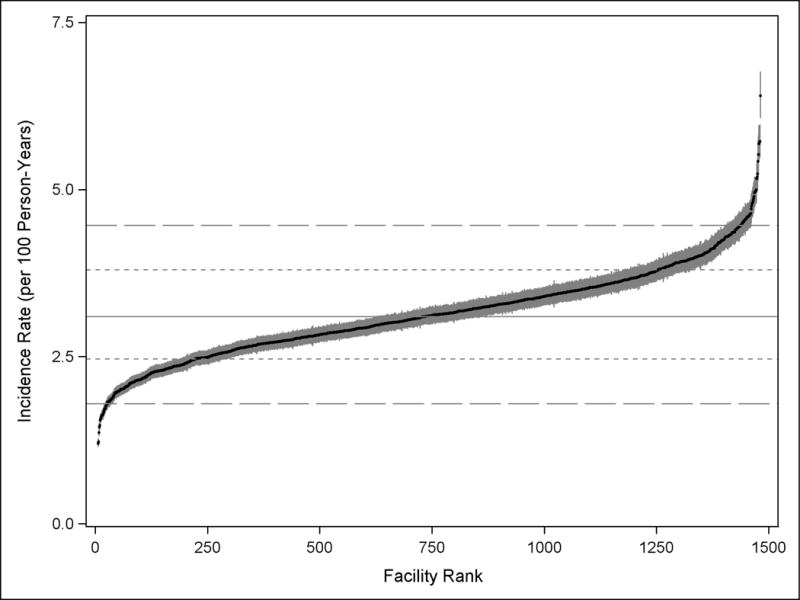
Distribution of Adjusteda Hip Fracture Incidence Rates across Facilities.
Footnotes:
aAdjusted for resident sex and FRAiL summary risk score for hip fracture[16].
bVertical lines represent 95% confidence intervals.
cHorizontal line represents mean facility hip fracture rate of 3.1 hip fractures per 100 person-years.
dHorizontal line using short dashes represents one standard deviation above and below the mean
eHorizontal line using long dashes represents two standard deviations above and below the mean
The relationship between facility and state characteristics and adjusted hip fracture incidence rates are presented in Table 1. Facilities with the highest rates of hip fracture had higher percentages of residents taking antipsychotic, antidepressant, antianxiety, and psychoactive medications, as well as a greater percentage of residents with advanced directives. Facilities with the highest rates of hip fracture also had the fewest hours of total nursing and total direct care hours/resident/day. On average, a 100-bed facility in the top tertile would provide 7 fewer hours of direct care/day than a 100-bed facility in the bottom tertile, which translates into about one fewer staff full time equivalent/day. Conversely, the facilities had smaller proportions of residents who were physically restrained, had been catheterized, and were receiving tube feedings. The facilities with the highest hip fracture rates were located in states that had, on average, lower occupancy rates and fewer beds.
Table 1.
Distribution of Facility and State Characteristics Stratified by Tertile of Adjusteda Average Hip Fracture Incidence Rate
| Facility-Level Characteristics | Lowest Tertile | Middle Tertile | Highest Tertile | P |
|---|---|---|---|---|
| Percentage of residents receiving antipsychotics, mean | 24.77 | 26.65 | 27.17 | <0.01 |
| Percentage of residents receiving antidepressants, mean | 43.66 | 49.03 | 50.77 | <0.01 |
| Percentage of residents receiving antianxiety drugs, mean | 17.12 | 18.36 | 18.69 | 0.02 |
| Percentage of residents receiving psychoactive drugs, mean | 60.72 | 65.83 | 66.91 | <0.01 |
| Percentage of residents receiving hypnotic drugs, mean | 6.30 | 5.91 | 5.77 | 0.21 |
| Number of prescription drugs/resident, mean | 10.47 | 10.47 | 10.34 | 0.35 |
| Total direct care hours/resident/day, mean | 3.29 | 3.34 | 3.22 | 0.02 |
| Total nursing hours/resident/day, mean | 3.53 | 3.55 | 3.43 | 0.03 |
| Ratio of registered nurses to total nurses, mean | 0.26 | 0.28 | 0.29 | 0.01 |
| Percentage of residents physically restrained, mean | 5.55 | 5.33 | 5.25 | 0.72 |
| Percentage of residents receiving bladder training, mean | 8.56 | 7.88 | 6.28 | 0.02 |
| Percentage of residents with catheter, mean | 5.89 | 5.62 | 5.00 | <0.01 |
| Number of quality-of-life deficiencies, mean | 0.72 | 0.75 | 0.77 | 0.76 |
| Percentage of residents receiving tube feedings, mean | 9.02 | 5.96 | 4.09 | <0.01 |
| Percentage of residents with advance directives, mean | 55.08 | 63.98 | 68.44 | <0.01 |
| State-Level Characteristics | ||||
| Proportion of facilities in a chain, mean | 0.49 | 0.52 | 0.52 | 0.79 |
| Proportion of hospital-based facilities, mean | 0.10 | 0.13 | 0.13 | 0.86 |
| Facility occupancy rate (proportion), mean | 0.89 | 0.86 | 0.81 | <0.01 |
| Number of facility beds, mean | 107.4 | 106.2 | 88.8 | 0.05 |
| Percentage of Medicaid beneficiaries, mean | 60.49 | 61.12 | 60.72 | 0.96 |
| Percentage of Medicare beneficiaries, mean | 14.73 | 16.23 | 13.99 | 0.19 |
| Proportion of for-profit facilities, mean | 0.62 | 0.63 | 0.61 | 0.95 |
| Hours/resident/day state regulatory staffing requirement, mean | 2.77 | 2.38 | 2.34 | 0.12 |
Adjusted for resident sex and FRAiL summary risk score for hip fracture[16]
The proportions of explained variance that were attributable to the different components of our multilevel model are illustrated in Figure 3. The amount of variation in hip fracture rates explained by the facility effect was 3.7% and by the state effect was 3.0%. Resident characteristics continued to account for most of the explained variation in hip fracture rates: 7.6%. The majority of the variation in hip fracture rates, (approximately 85.7%) remained unexplained by the full model.
Figure 3.
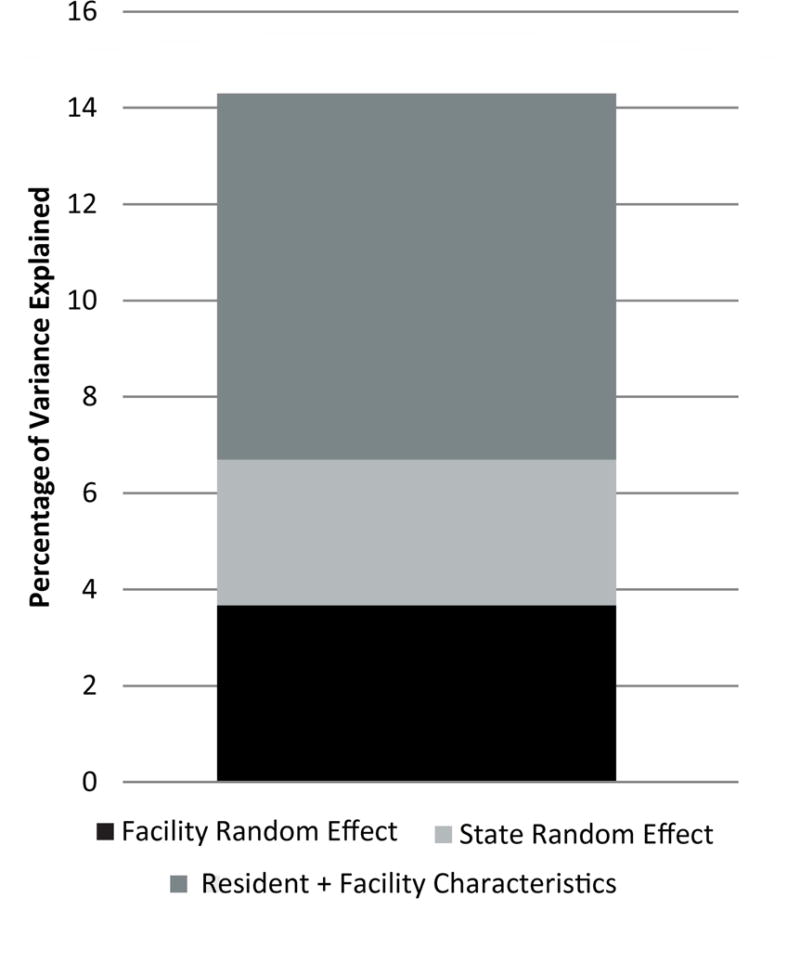
Partitioning of Variance in Multilevel Model Adjusting for Resident, Facility, and State Characteristics.
DISCUSSION
In this nationally representative cohort study, we found considerable variation in the IR of hip fracture across US NH facilities, ranging from 1.20 to 6.40 hip fractures per 100 person-years. Differences in resident case-mix accounted for much of the explained variation, which is unsurprising and consistent with prior studies. Both facility and state characteristics also appeared to meaningfully contribute to the observed variation. Our analyses identified a number of modifiable facility-level characteristics as potential intervention targets to decrease rates of hip fracture across NH facilities. However, despite considering these and other resident characteristics in our multilevel model, the majority of the variation in the risk of hip fracture remained unexplained.
Consistent with previous studies, our study suggests that facilities with more residents who are mobile have the greatest rates of hip fracture.[36–39] We observed similar resident-level associations during the development of the FRAiL model, which demonstrates that residents who were mobile were more likely to experience a hip fracture.[16] Such residents should be targeted for fracture prevention interventions. Many of the facility-level OSCAR variables that were associated with hip fracture rates may ultimately describe the underlying and less modifiable characteristics of the residents in a facility.
Surprisingly few data are available about the contribution of facility-level characteristics to the occurrence of hip fractures in NHs, though prior studies have examined the contribution of such characteristics to post-fracture outcomes.[3, 40] We identified several modifiable facility-level characteristics that were associated with greater rates of hip fracture. These included the percentages of residents prescribed antipsychotic, antidepressant, antianxiety, and psychoactive medications. This is consistent with prior literature, which suggests that facilities reporting higher rates of psychoactive medication also report higher rates of falls, which can ultimately result in hip fractures.[41] Though NH facilities often have detailed guidelines for prescribing medications to residents, particularly regarding the use of high-risk medications, studies have shown that only providers specifically trained in geriatrics were less likely to prescribe risky medications.[42]
Of concern, we found that facilities with greater rates of hip fracture also had fewer hours of direct care and nursing care/resident/day. This is consistent with the literature suggesting that a primary reason for poor quality care in NH facilities is inadequate nurse staffing levels.[25, 33, 43] Adequate staffing may free up time for monitoring of circumstances that could result in falls and fracture risk factor surveillance by frontline staff like certified nursing assistants (CNAs). Adding CNAs may be particularly effective at reducing fracture for at least two reasons: 1) CNAs often have the most direct contact with the residents, and 2) many fall-related fractures occur during toileting and CNAs often support bladder training programs, safe toileting, and toileting rounds.[44] Using the fall-related items on version 3.0 of the MDS, facilities could target medication management and staffing-related interventions to residents with documented falls or fall-related injuries.
Interestingly, we found that facilities with more advanced directive documentation had greater rates of hip fracture. Advanced care planning documentation has been considered a proxy for higher quality care, and one might have expected to see an inverse relationship with fracture. We suspect that facilities that are encouraging advance care planning are also promoting mobilization and attempting to preserve resident function. This illustrates the challenge and potential danger of using a single metric to evaluate quality in NH facilities.
States play a large role in regulation of health care, and their willingness and ability to address federally mandated NH policies varies widely.[28, 45] It is has been suggested that the stringency of state regulatory enforcement of NH quality is associated with facility size, occupancy rates, and the generosity of facility reimbursement rate policies.[28] In some cases, states are less likely to implement stringent quality enforcement for smaller facilities and facilities with lower occupancy rates.[46] We found that states with lower facility occupancy rates and with smaller facilities (lower numbers of total beds) had higher rates of hip fractures. This suggests that greater enforcement of state regulations for smaller facilities may reduce hip fracture rates.
It is worth noting that while the state staffing regulations for nursing hours per resident day were not independently associated with hip fracture rates,[47] worse staff to resident ratio was associated with higher rates of hip fracture. The average difference in the direct care hours/resident/day between facilities in the top tertile and lowest tertile of hip fracture rates was 0.07 hours, or for a 100 bed facility, 7 hours/resident/day. Although small, this difference of approximately 1 staff FTE is likely meaningful in an effort to prevent fractures.[44] Policy tools that only influence staffing standards may not modify facility hip fracture rates because standards are only one of many factors that ultimately affect staffing levels.[47]
This study has several important limitations. First, despite the comprehensive list of characteristics that we considered, we were only able to explain approximately 14% of the variation in hip fracture rates. The fact that the fraction of total variation attributable to facility random effects did not appreciably decrease upon inclusion of important facility characteristics suggests the presence of either other important unmeasured characteristics that may be driving the variation or appreciable measurement error in the included characteristics. Second, Part D drug dispensing claims were unavailable and therefore resident-level use of medications was not included in the models. The absence of claims-based medication use may inflate the variation attributable to facilities and exaggerate the association between facility antipsychotic prescribing and hip fracture rates. Third, we only ascertained hospitalized hip fractures using Medicare inpatient claims. It is possible that some facilities avoided hospitalizing residents, and this may have influenced our results.[48, 49] Use of other non-Medicare non-Medicaid insurance coverage is likely to be rare, and would not have a strong influence on the ascertainment of fracture or other key characteristics as measured by the MDS or OSCAR. Fourth, we restricted our study to facilities with ≥100 beds because facilities that had 100 or fewer residents contribute little information to the estimation of between-facility variability in hip fracture rates. The restriction also helped to stabilize estimates of hip fracture by ensuring there was a large enough denominator in each facility. Our results may generalize only to larger NH facilities. Future work should focus on using more years of data in combination with a lower (or no) facility size threshold to overcome this limitation. Fifth, we did not account for censoring when examining hip fracture variation with multilevel logistic regression modeling, which could result in bias if censoring events were differential by facility.
In summary, although the Centers for Medicare and Medicaid Services have determined that the proportion of residents that experience injurious falls is an important NH quality measure[50], we caution against the use of hip fracture rates as a similar quality measure. Even after accounting for a comprehensive list of patient, state, and facility level characteristics, 85.7% of the variation in hip fracture rates remained unexplained. The paradoxical relationship between advance directives and the rates of hip fracture that we observed further points out the challenges with using a single quality metric in this setting. Nonetheless, reporting hip fracture rates per facility may be useful. We would urge facilities with high rates of hip fracture to consider examining their staffing practices and medication prescribing practices in an effort to prevent hip fracture.
Supplementary Material
Supplementary Table S1 - Number of Nursing Home Facilities in the Study Sample Stratified by State.
Impact Statement.
We certify that this work is novel. It is the first nationally representative examination of US nursing home facility-level and state-level determinants of hip fracture incidence rates among older adults, and identifies several important potential targets for policy interventions to reduce rates, including increased facility staffing and reduced antipsychotic prescribing.
Acknowledgments
Dr. Zullo is a U.S. Government employee; the views expressed in this article are those of the author and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Funding: Financial support for this study was provided by the National Institute on Aging (5R01AG045441). Dr. Zullo is supported by an Agency for Healthcare Research and Quality award (5K12HS022998) and a Veterans Affairs Office of Academic Affiliations Advanced Fellowship in Health Services Research and Development.
Conflict of Interest Disclosures
| Elements of Financial/Personal Conflicts | A.R.Z. | T.Z. | G.B. | Y.L. | K.W.M. | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | X | |||||
| Grants/Funds | X | X | X | X | X | |||||
| Honoraria | X | X | X | X | X | |||||
| Speaker Forum | X | X | X | X | X | |||||
| Consultant | X | X | X | X | X | |||||
| Stocks | X | X | X | X | X | |||||
| Royalties | X | X | X | X | X | |||||
| Expert Testimony | X | X | X | X | X | |||||
| Board Member | X | X | X | X | X | |||||
| Patents | X | X | X | X | X | |||||
| Personal Relationship | X | X | X | X | X | |||||
| Elements of Financial/Personal Conflicts | D.P.K | L.A.D. | V.M. | S.D.B. | ||||
| Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | X | X | X | X | ||||
| Grants/Funds | X | X | X | X | ||||
| Honoraria | X | X | X | X | ||||
| Speaker Forum | X | X | X | X | ||||
| Consultant | X | X | X | X | ||||
| Stocks | X | X | X | X | ||||
| Royalties | X | X | X | X | ||||
| Expert Testimony | X | X | X | X | ||||
| Board Member | X | X | X | X | ||||
| Patents | X | X | X | X | ||||
| Personal Relationship | X | X | X | X | ||||
Conflict of Interest Explanations
V.M.
V.M.’s research is in a related area to that of several different paid activities. V.M. also periodically serves as a paid speaker at national conferences where he discusses trends and research findings in long term and post-acute care. V.M. holds stock of unknown value in PointRight, Inc. an information services company providing advice and consultation to various components of the long term care and post-acute care industry, including suppliers and insurers. PointRight sells information on the measurement of nursing home quality to nursing homes and liability insurers. V.M. was a founder of the company but has subsequently divested much of his equity in the company and relinquished his seat on board. In addition, V.M. Chairs the Independent Quality Committee for HRC Manor Care, Inc., a nursing home chain, for which he receives compensation in the $20,000-$40,000 range. V.M. also serves as chair of a Scientific Advisory Committee for NaviHealth, a post-acute care service organization, for which he also receives compensation in the $20,000–40,000 per year range. V.M. serves as a Technical Expert Panel member on several Centers for Medicare/Medicaid quality measurement panels. V.M. is a member of the board of directors of Tufts Health Plan Foundation; Hospice Care of Rhode Island; and The Jewish Alliance of Rhode Island.
D.P.K.
D.P.K. serves as an author for the “Falls” chapters in UpToDate and receives royalties from Wolters Kluwer for this. D.P.K. also served as editor for the book “Osteoporosis in Older Persons” and received an honorarium from Springer for this activity.
S.D.B.
S.D.B. serves as an author for the “Falls” chapters in UpToDate and receives royalties from Wolters Kluwer for this.
Footnotes
DR. ANDREW R. ZULLO (Orcid ID : 0000-0003-1673-4570)
Prior Presentation: None.
Author Contributions: Study concept and design: Zullo, Banerjee, Berry. Acquisition of data: Berry, Mor, Zullo, Lee. Analysis of data: Banerjee, Lee, Zhang, Zullo. Interpretation of results: All authors. Preparation of initial draft of manuscript: Banerjee, Zhang, Zullo, Berry. Critical review of manuscript: All authors.
Sponsor’s Role: The funding organization had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
References
- 1.Carter MW, Porell FW. Variations in Hospitalization Rates Among Nursing Home Residents: The Role of Facility and Market Attributes. The Gerontologist. 2003;43:175–91. doi: 10.1093/geront/43.2.175. [DOI] [PubMed] [Google Scholar]
- 2.Intrator O, Carter MW, Mor V. Facility Characteristics Associated with Hospitalization of Nursing Home Residents: Results of a National Study. Medical Care. 1999;37:228–37. doi: 10.1097/00005650-199903000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Gozalo P, Leland NE, Christian TJ, et al. Volume Matters: Returning Home After Hip Fracture. Journal of the American Geriatrics Society. 2015;63:2043–51. doi: 10.1111/jgs.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huybrechts KF, Rothman KJ, Brookhart MA, et al. Variation in antipsychotic treatment choice across US nursing homes. Journal of clinical psychopharmacology. 2012;32:11–7. doi: 10.1097/JCP.0b013e31823f6f46. [DOI] [PubMed] [Google Scholar]
- 5.Neuman MD, Wirtalla C, Werner RM. Association between skilled nursing facility quality indicators and hospital readmissions. JAMA : the journal of the American Medical Association. 2014;312:1542–51. doi: 10.1001/jama.2014.13513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fain KM, Castillo-Salgado C, Dore DD, et al. Inappropriate Fentanyl Prescribing Among Nursing Home Residents in the United States. Journal of the American Medical Directors Association. 2017;18:138–44. doi: 10.1016/j.jamda.2016.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen JW, Spector WD. The effect of Medicaid reimbursement on quality of care in nursing homes. Journal of health economics. 1996;15:23–48. doi: 10.1016/0167-6296(95)00030-5. [DOI] [PubMed] [Google Scholar]
- 8.Vlaeyen E, Coussement J, Leysens G, et al. Characteristics and effectiveness of fall prevention programs in nursing homes: a systematic review and meta-analysis of randomized controlled trials. Journal of the American Geriatrics Society. 2015;63:211–21. doi: 10.1111/jgs.13254. [DOI] [PubMed] [Google Scholar]
- 9.Ray WA, Taylor JA, Meador KG, et al. A Randomized Trial of a Consultation Service to Reduce Falls in Nursing Homes. JAMA. 1997:278. [PubMed] [Google Scholar]
- 10.O’Neill C, Harrington C, Kitchner M, et al. Quality of Care in Nursing Homes: An Analysis of Relationships among Profit, Quality, and Ownership. Medical Care. 2003;41:1318–30. doi: 10.1097/01.MLR.0000100586.33970.58. [DOI] [PubMed] [Google Scholar]
- 11.Harrington C, Kovner C, Mezey M, et al. Experts Recommend Minimum Nurse Staffing Standards for Nursing Facilities in the United States. The Gerontologist. 2000;40:5–16. doi: 10.1093/geront/40.1.5. [DOI] [PubMed] [Google Scholar]
- 12.Berry SD, Lee Y, Zullo AR, et al. Incidence of Hip Fracture in U.S. Nursing Homes. The journals of gerontology Series A, Biological sciences and medical sciences. 2016;71:1230–4. doi: 10.1093/gerona/glw034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Killington M, Walker R, Crotty M. The chaotic journey: Recovering from hip fracture in a nursing home. Archives of gerontology and geriatrics. 2016;67:106–12. doi: 10.1016/j.archger.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Wiklund R, Toots A, Conradsson M, et al. Risk factors for hip fracture in very old people: a population-based study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2016;27:923–31. doi: 10.1007/s00198-015-3390-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age and ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- 16.Berry SD, Zullo AR, Lee Y, et al. Fracture Risk Assessment in Long-term Care (FRAiL): Development and Validation of a Prediction Model. The journals of gerontology Series A, Biological sciences and medical sciences. 2017 doi: 10.1093/gerona/glx147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spector W, Shaffer T, Potter DE, et al. Risk factors associated with the occurrence of fractures in U.S. nursing homes: resident and facility characteristics and prescription medications. Journal of the American Geriatrics Society. 2007;55:327–33. doi: 10.1111/j.1532-5415.2007.01081.x. [DOI] [PubMed] [Google Scholar]
- 18.Banerjee G, Zullo AR, Berry SD, et al. Geographic Variation in Hip Fracture Among United States Long-Stay Nursing Home Residents. Journal of the American Medical Directors Association. 2016;17:865e1–3. doi: 10.1016/j.jamda.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Intrator O, Hiris J, Berg K, et al. The residential history file: studying nursing home residents’ long-term care histories(*) Health services research. 2011;46:120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Straker JK, Bailer AJ. A review and characterization of the MDS process in nursing homes. Journal of gerontological nursing. 2008;34:36–44. doi: 10.3928/00989134-20081001-01. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services. Long-Term Care Facility Resident Assessment Instrument 2.0 User’s Manual. 2009 [Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIMDS20.html.
- 22.Aboussouan LS, Khan SU, Banerjee M, et al. Objective measures of the efficacy of noninvasive positive-pressure ventilation in amyotrophic lateral sclerosis. Muscle & nerve. 2001;24:403–9. doi: 10.1002/1097-4598(200103)24:3<403::aid-mus1013>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 23.Feng Z, Katz PR, Intrator O, et al. Physician and nurse staffing in nursing homes: the role and limitations of the Online Survey Certification and Reporting (OSCAR) system. Journal of the American Medical Directors Association. 2005;6:27–33. doi: 10.1016/j.jamda.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Kash BA, Hawes C, Phillips CD. Comparing staffing levels in the Online Survey Certification and Reporting (OSCAR) system with the Medicaid Cost Report data: are differences systematic? The Gerontologist. 2007;47:480–9. doi: 10.1093/geront/47.4.480. [DOI] [PubMed] [Google Scholar]
- 25.Harrington C, Choiniere J, Goldmann M, et al. Nursing home staffing standards and staffing levels in six countries. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing. 2012;44:88–98. doi: 10.1111/j.1547-5069.2011.01430.x. [DOI] [PubMed] [Google Scholar]
- 26.Mor V, Gruneir A, Feng Z, et al. The effect of state policies on nursing home resident outcomes. Journal of the American Geriatrics Society. 2011;59:3–9. doi: 10.1111/j.1532-5415.2010.03230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McConeghy KW, Lee Y, Zullo AR, et al. Influenza illness and hip fracture hospitalizations in nursing home residents: are they related? The journals of gerontology Series A, Biological sciences and medical sciences. 2017 doi: 10.1093/gerona/glx200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrington C, Mullan JT, Carrillo H. State Nursing Home Enforcement Systems. Journal of Health Politics, Policy, and Law. 29:44–74. doi: 10.1215/03616878-29-1-43. [DOI] [PubMed] [Google Scholar]
- 29.Zinn JS, Aaronson WE, Rosko MD. Variations in the Outcomes of Care Provided in Pennsylvania Nursing Homes: Facility and Environmental Correlates. Medical Care. 1993;31:475–87. doi: 10.1097/00005650-199306000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Chiu Y, Bero L, Hessol NA, et al. A literature review of clinical outcomes associated with antipsychotic medication use in North American nursing home residents. Health policy. 2015;119:802–13. doi: 10.1016/j.healthpol.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 31.Elkassabany NM, Passarella M, Mehta S, et al. Hospital Characteristics, Inpatient Processes of Care, and Readmissions of Older Adults with Hip Fractures. Journal of the American Geriatrics Society. 2016;64:1656–61. doi: 10.1111/jgs.14256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hyer K, Thomas KS, Branch LG, et al. The influence of nurse staffing levels on quality of care in nursing homes. Gerontologist. 2011;51:610–6. doi: 10.1093/geront/gnr050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harrington C. Nursing Home Staffing Standards in State Statutes and Regulations. 2010 [Google Scholar]
- 34.Mukamel DB, Haeder SF, Weimer DL. Top-down and bottom-up approaches to health care quality: the impacts of regulation and report cards. Annual review of public health. 2014;35:477–97. doi: 10.1146/annurev-publhealth-082313-115826. [DOI] [PubMed] [Google Scholar]
- 35.Genberg BL, Rogers WH, Lee Y, et al. Prescriber and pharmacy variation in patient adherence to five medication classes measured using implementation during persistent episodes. Pharmacoepidemiology and drug safety. 2016;25:790–7. doi: 10.1002/pds.4025. [DOI] [PubMed] [Google Scholar]
- 36.Girman CJ, Chandler JM, Zimmerman SI, et al. Prediction of fracture in nursing home residents. J Am Geriatr Soc. 2002;50:1341–7. doi: 10.1046/j.1532-5415.2002.50354.x. [DOI] [PubMed] [Google Scholar]
- 37.Nakamura K, Oyama M, Takahashi S, et al. Fracture incidence in nursing homes in Japan. Osteoporos Int. 2010;21:797–803. doi: 10.1007/s00198-009-1015-x. [DOI] [PubMed] [Google Scholar]
- 38.Colon-Emeric CS, Biggs DP, Schenck AP, et al. Risk factors for hip fracture in skilled nursing facilities: who should be evaluated? Osteoporos Int. 2003;14:484–9. doi: 10.1007/s00198-003-1384-5. [DOI] [PubMed] [Google Scholar]
- 39.Jerez-Roig J, Santos MM, Souza DL, et al. Prevalence of urinary incontinence and associated factors in nursing home residents. Neurourology and urodynamics. 2016;35:102–7. doi: 10.1002/nau.22675. [DOI] [PubMed] [Google Scholar]
- 40.Neuman MD, Silber JH, Passarella MR, et al. Comparing the Contributions of Acute and Postacute Care Facility Characteristics to Outcomes After Hospitalization for Hip Fracture. Medical care. 2017;55:411–20. doi: 10.1097/MLR.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Damian J, Pastor-Barriuoso R, Valderrama-Gama E, et al. Factors associated with falls among older adults living in institutions. BMC Geriatrics. 2013:13. doi: 10.1186/1471-2318-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Monroe T, Carter M, Parish A. A case study using the beers list criteria to compare prescribing by family practitioners and geriatric specialists in a rural nursing home. Geriatric nursing. 2011;32:350–6. doi: 10.1016/j.gerinurse.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harrington C, Schnelle JF, McGregor M, et al. The Need for Higher Minimum Staffing Standards in U.S. Nursing Homes. Health services insights. 2016;9:13–9. doi: 10.4137/HSI.S38994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leland NE, Gozalo P, Teno J, et al. Falls in newly admitted nursing home residents: a national study. Journal of the American Geriatrics Society. 2012;60:939–45. doi: 10.1111/j.1532-5415.2012.03931.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paek SC, Zhang NJ, Wan TT, et al. The Impact of State Nursing Home Staffing Standards on Nurse Staffing Levels. Medical care research and review : MCRR. 2016;73:41–61. doi: 10.1177/1077558715594733. [DOI] [PubMed] [Google Scholar]
- 46.Li Y, Harrington C, Spector WD, et al. State regulatory enforcement and nursing home termination from the medicare and medicaid programs. Health services research. 2010;45:1796–814. doi: 10.1111/j.1475-6773.2010.01164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mueller C, Arling G, Kane R, et al. Nursing Home Staffing Standards: Their Relationship to Nurse Staffing Levels. The Gerontologist. 2006;46:74–80. doi: 10.1093/geront/46.1.74. [DOI] [PubMed] [Google Scholar]
- 48.Berry SD, Zullo AR, McConeghy K, et al. Defining hip fracture with claims data: outpatient and provider claims matter. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2017 doi: 10.1007/s00198-017-4008-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berry SD, Zullo AR, McConeghy K, et al. Administrative health data: guilty until proven innocent. Response to comments by Levy and Sobolev. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2017 doi: 10.1007/s00198-017-4244-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Centers for Medicare and Medicaid Services. Nursing Home Quality Initiative–Quality Measures. :2017. [Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIQualityMeasures.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1 - Number of Nursing Home Facilities in the Study Sample Stratified by State.


