Abstract
A 59-year-old man with swollen submandibular glands developed an aortic aneurysm requiring aortic prosthesis implantation. Echocardiography performed to evaluate the cardiac function before the surgery incidentally revealed masses around the coronary arteries. The serum IgG4 levels were increased. A post-operational pathological examination of the abdominal aneurysms revealed infiltration of plasma cells, with the ratio of IgG4/IgG-positive cells being >80%. The patient was diagnosed with IgG4-related disease (RD) with coronary artery involvement. He was treated successfully with corticosteroid before any associated cardiovascular events occurred. Given the poor prognosis of IgG4-RD-associated coronary artery involvement, this case emphasizes the importance of the early assessment with echocardiography, even if patients have no cardiovascular symptoms.
Keywords: aortic aneurysm, coronary artery, immunoglobulin, IgG4-related disease, prednisolone
Introduction
Immunoglobulin G4 (IgG4)-related disease (RD) has been recognized recently as a syndrome characterized by enlargement of not only exocrine but also endocrine organs, such as the pituitary gland and pancreas, along with increased serum IgG4 levels (1,2). This syndrome was first reported in 2001, when Hamano et al. (3,4) observed high levels of serum IgG4 and abundant infiltration of IgG4-positive plasma cells in the pancreas.
It is now generally accepted that IgG4-RD involves multiple organs (5,6). The pathological characteristics include diffuse lymphoplasmacytic infiltration, fibrosis, obliterative phlebitis, and eosinophilic infiltration in the involved organs (7,8). Many reports indicate that coronary artery involvement is related to a poor prognosis (6,9-15).
We herein report a case of IgG4-RD with coronary artery involvement that was detected incidentally with echocardiography as a screening test of the cardiac function and treated successfully with corticosteroid before any associated clinical events occurred.
Case Report
A 59-year-old man developed painless enlargement of the submandibular glands bilaterally in 2009 and lost 10 kg in body weight over 6 months. Abdominal discomfort and pain accompanied this weight loss. Computed tomography (CT) revealed an abdominal aortic aneurysm (AAA) that required aortic prosthesis implantation in 2010. A histological assessment of the affected blood vessel confirmed an inflammatory aortic aneurysm. Incidentally, echocardiography to assess the cardiac function before surgery revealed masses surrounding the left and right coronary arteries. In 2012, follow-up echocardiography showed that the masses had increased in size. Laboratory tests revealed hypergammaglobulinemia and high serum IgG4 levels. The patient was referred to our institution for a further evaluation and treatment in August 2012.
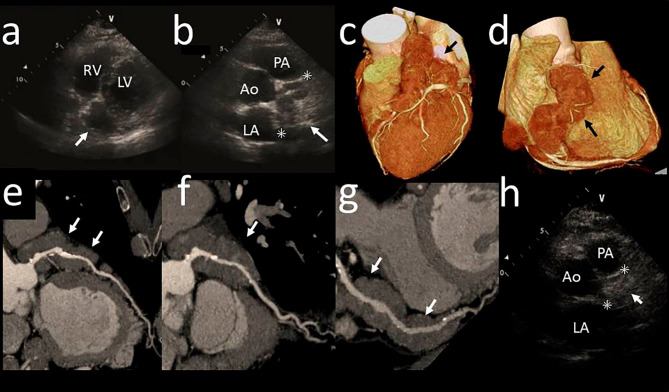
Upon transfer to our institution, non-tender, elastic and mobile bilateral enlargement of the submandibular glands and cervical and axillary lymph nodes was observed. He had no sicca symptoms. Laboratory investigation indicated an accelerated erythrocyte sedimentation rate (90 mm/h) along with high IgG (4,125 mg/dL), IgG4 (2,920 mg/dL), and creatinine (1.49 mg/dL) levels (Table 1). The patient was negative for antinuclear antibodies and autoantibodies to SS-A and SS-B. Echocardiography confirmed the masses surrounding the left and right coronary arteries (Fig. 1a and b). The maximum diameter of the larger mass, located on the right coronary artery, was 32.5 mm (Fig. 1b). Coronary CT angiography revealed no significant stenotic lesions (<50%) or aneurysms in the lumen but did show diffuse thick perivascular masses around the coronary arteries with low density (Fig. 1c-g). The average value of the mass was 60 Hounsfield units on CT.
Table 1.
Laboratory Findings on Admission.
| Property | Value | |
|---|---|---|
| ESR | 90 | mm/h |
| WBC | 6,000 | /μL |
| Neu | 57.5 | % |
| Lym | 29.5 | % |
| Mon | 5.3 | % |
| Eos | 7.0 | % |
| Bas | 0.7 | % |
| RBC | 398×104 | /μL |
| Hb | 12.2 | g/dL |
| Ht | 37.2 | % |
| Plt | 25.5×104 | /μL |
| TP | 9.3 | g/dL |
| γ-globulin | 43.1 | % |
| Alb | 3.5 | g/dL |
| BUN | 28 | mg/dL |
| Cre | 1.49 | mg/dL |
| Na | 134 | mEq/L |
| K | 4.7 | mEq/L |
| Cl | 105 | mEq/L |
| LDH | 175 | IU/L |
| AST | 19 | IU/L |
| ALT | 15 | U/L |
| CRP | 0.18 | mg/dL |
| C3 | 101 | mg/dL |
| C4 | 21 | mg/dL |
| CH50 | 66 | U/mL |
| IgG | 4,125 | mg/dL |
| IgG4 | 2,920 | mg/dL |
| IgM | 16 | mg/dL |
| IgA | 113 | mg/dL |
| sIL-2R | 844 | U/mL |
| ANA | - | |
| anti SS-A Ab | - | |
| anti SS-B Ab | - | |
ESR: erythrocyte sedimentation rate, TP: total protein, Alb: albumin, LDH: lactate dehydrogenase, AST: aspartate aminotransferase, AST: alanine aminotransferase, CRP: C-reactive protein, sIL-2R: soluble interleukin 2 receptor, ANA: antinuclear antibody, Ab: antibody
Figure 1.
Transthoracic echocardiography and computed tomography (CT) of the masses surrounding the coronary arteries. Transthoracic echocardiography depicted hypoechoic areas surrounding the left (a; parasternal short-axis view) and right (b; apex long-axis view) coronary arteries before treatment. Coronary CT angiography depicted diffuse masses surrounding the left (c) and right coronary arteries (d). No stenotic lesions or aneurysms were found in the left anterior descending (e), left circumflex coronary (f), or right (g) coronary arteries. Echocardiography showed that the hypoechoic areas were reduced in the right coronary artery (h) after treatment. Arrows denote the masses surrounding coronary arteries. Asterisks denote the maximum diameter. Ao: aorta, PA: pulmonary artery, LA: left atrium, LV: left ventricle, RA: right atrium
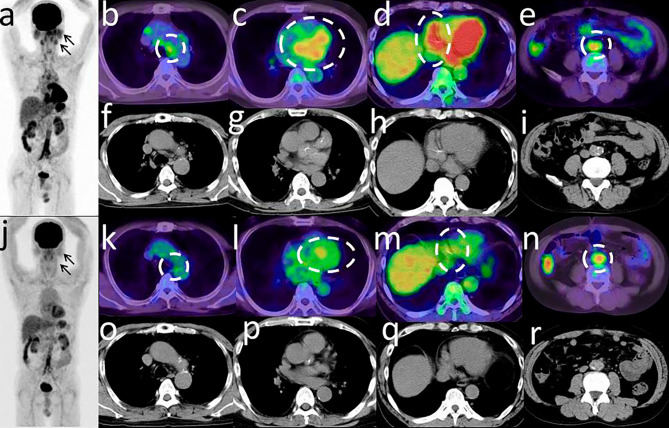
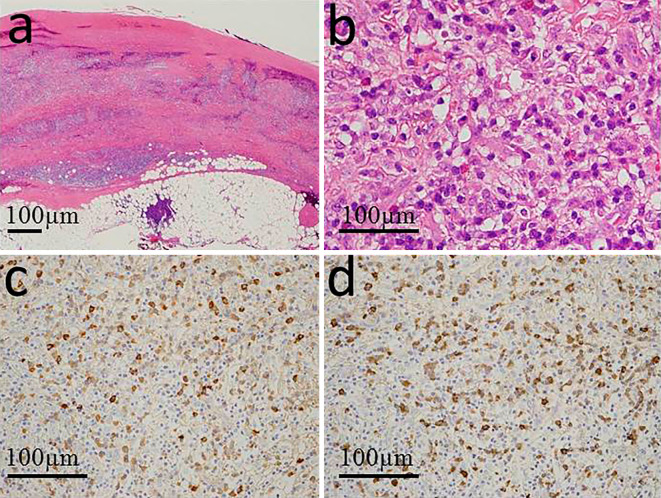
Fluorine-18 (18F) fluorodeoxyglucose positron emission tomography-CT (FDG-PET/CT) showed an abnormal FDG uptake in the area corresponding to the coronary arteries as well as in the bilateral parotid and submandibular glands, mediastinal lymph nodes, and abdominal aorta (Fig. 2a-i). The FDG uptake was higher than normal, with a maximum standardized uptake value (SUVmax) of 4.9 in the masses, 3.4 in salivary glands, 3.8 in mediastinal lymph nodes, and 5.8 in abdominal aorta. These findings were compatible with the presence of coronary arteritis. Serial sections of the abdominal aortic segment resected during the prosthesis implantation were immunostained with anti-IgG, or anti-IgG4 antibodies (Fig. 3). The IgG4-positive and IgG-positive cells were counted in the same microscopic field. The field was selected in the areas of intense IgG4 focus (16). The ratio of IgG4/IgG-positive plasma cells was >80% (Fig. 3). According to the diagnostic criteria for IgG4-RD (17), IgG4-RD was diagnosed.
Figure 2.
Fluorine-18 fluorodeoxyglucose-positron emission tomography-computed tomography (FDG-PET/CT) of the masses. A maximum intensity projection image revealed the foci of the uptake in the bilateral parotid and submandibular glands, mediastinal lymph nodes, the masses, and abdominal aorta before the treatment (a). FDG-PET/CT showed the FDG accumulation in the area corresponding to the mediastinal lymph nodes (b), the masses (c, d), and abdominal aorta (e) before treatment. CT depicted lymph nodes (f), the mass (g, h), and abdominal aorta (i) in same cross sections. The FDG accumulation decreased after treatment (j-m). The FDG accumulation in the descending aorta decreased to only a modest value after treatment (n). CT showed that the lymph nodes and the mass were reduced in the same cross section (o-q). CT depicted the abdominal aorta in the same section (r). Arrows denote the parotid glands and submandibular glands. Circles surround the abnormal FDG uptake. We performed FDG-PET/CT for the target lesion of the coronary arterial wall with a fasting time of 6 hours.
Figure 3.
A histological examination of an abdominal aorta section resected during prosthesis implantation. Hematoxylin and Eosin staining revealed fibrosis in the vascular media (a) and infiltration of mononuclear cells without atypical cells in the vascular media and adventitia (b). The upper side is luminal (a). IgG4 immunostaining (c) and IgG immunostaining (d) revealed infiltrating IgG4-positive plasma cells and IgG-positive plasma cells.
The patient was treated with 40 mg/day (0.6 mg/kg/day) of prednisolone. The dosage was tapered gradually after confirming the size reduction of the coronary lesions with monthly echocardiography. After 28 days, the value of serum IgG4 was 280 mg/dL. The serum IgG4/IgG ratio decreased to 0.2. The submandibular glands also shrank in size. After 150 days, the maximum diameter of the larger mass was 21.0 mm (Fig. 1h). The abnormal FDG uptake disappeared in the salivary grands, mediastinal lymph nodes, and masses (Fig. 2j-m, o-q). After treatment with prednisolone, a maximum intensity projection image showed that the abnormal FDG uptake in the area corresponding to the abdominal aorta had decreased to only a modest value (Fig. 2j). The SUVmax was reduced to 5.2 from 5.8 (Fig. 2n and r). No relapse of IgG4-RD has been observed under continuous treatment of 10 mg/day of prednisolone for 3 years.
Discussion
We herein report a case of IgG4-RD involving the coronary arteries that was identified using echocardiography before any associated cardiovascular events occurred. This case emphasizes the utility of echocardiography for screening asymptomatic coronary artery involvement of IgG4-RD.
Generally, corticosteroid is effective for the treatment of IgG4-RD (17). However, corticosteroid was found to be ineffective in 8 out of 10 IgG4-RD patients with coronary artery involvement (6, 9-15, 18, Table 2). Regarding the eight patients in whom corticosteroid was ineffective, seven had coronary stenosis and/or aneurysm, five had stenosis, one had aneurysm, and two had both. Cardiac surgery was necessary in three of the eight cases (6, 9-15, Table 2). All patients who had coronary stenosis or aneurysms were resistant to corticosteroid (6,9-15). In contrast, the patients without coronary stenosis or aneurysms responded to corticosteroid (18, the present case). These findings suggest that the efficacy of corticosteroid therapy might depend on the presence of coronary stenosis and/or aneurysm. Indeed, in one patient in whom whom corticosteroid was ineffective, fibrosis of the coronary artery lesion was observed (19). In IgG4-related sialadenitis, treatment responsiveness was related to the degree of fibrosis in the salivary gland (20). Similarly to sialadenitis, treatment responsiveness of IgG4-RD with coronary stenosis may be related to the presence of fibrosis. In one patient in whom corticosteroid was effective, 0.6 mg/kg/day of prednisolone was sufficient for treating coronary involvement (18). That dose (0.6 mg/kg/day) was consistent with the dose administered in the present case. Corticosteroid-responsive patients had no coronary stenosis or aneurysms. Some of the patients in whom corticosteroid was ineffective underwent surgical intervention (6,9,12,14).
Table 2.
Clinical Characteristics in Patients with IgG4-RD Involving Coronary Artery.
| Reference | Age/Sex | Symptom | Coronary Stenosis | Coronary Aneurysm | IgG4 (mg/dL) | Treatment | Outcome | Other lesions |
|---|---|---|---|---|---|---|---|---|
| 6 | 63/F | Dyspnea | + | - | 456 | Bypass | - | AAA |
| 9 | 75/M | Chest pain | + | - | 2,510 | PSL 15 mg/day Bypass | - | AAA, Pancreatitis, Parotitis |
| 10 | 64/M | Dyspnea | - | + | - | PSL | - | Interstitial nephritis |
| 11 | 71/M | - | + | + | 2,720 | PSL, CV | - | AAA, Pancreatitis Sialadenitis, Cholangitis, |
| 12 | 66/M | Chest pain | + | - | 564 | Bypass | - | - |
| 13 | 75/M | - | + | - | 625 | PSL 20 mg/day | - | Aortitis |
| 14 | 72/M | Dyspnea | + | - | - | PSL 50 mg/day, Rituximab Bypass | - | Uveitis, Lung |
| 15 | 60/M | - | + | + | 1,350 | PSL 20 mg/day | - | Aortitis, Sialadenitis, Pancreatitis |
| 18 | 62/M | - | - | - | 2,170 | PSL 40 mg/day (0.6 mg/kg/day) | Improved | AAA |
| The present case | 59/M | - | - | - | 2,920 | PSL 40 mg/day (0.6 mg/kg/day) | Improved | AAA |
PSL: prednisolone, CY: Cyclophosphamide, Bypass: coronary artery bypass, AAA: abdominal aortic aneurysm
In patients with chest pain or shortness of breath related to IgG4-RD, a coronary artery lesion was diagnosed based on high levels of IgG4 and the findings of echocardiogram and coronary CT (6,9,10,12,14). In patients without chest pain or shortness of breath, IgG4-RD with a coronary artery lesion was diagnosed by screening of systemic organ involvements (11, 13, 15, 18, the present case). Patients without coronary stenosis or aneurysms were asymptomatic (18, the present case). In one patient who died of a heart attack, autopsy revealed multiorgan involvement with IgG4-RD, including coronary artery involvement (19). Screening for coronary involvement is important, even if patients are asymptomatic.
Electrocardiography, echocardiography, and coronary CT were performed to assess myocardial ischemia. Coronary CT revealed moderate stenosis (25-50%) and calcification. Significant stenosis (>50%) was not detected. In the present case, the uptake of FDG was noted in the left ventricular myocardium. FDG-PET was performed to detect inflammatory lesions of the coronary arterial wall in the patient with a fasting time of 6 hours. To assess the myocardial inflammation, the sufficient suppression of the physiological FDG uptake is necessary with longer fasting periods (>12 hours) (21). Fortunately for the present case, FDG-PET with a fasting time of 6 hours allowed us to assess the lesions of the coronary arterial wall.
The IgG4 levels are reported to be significantly higher in IgG4-RD patients with the involvement of multiple organs (mean: 699 mg/dL) than in those with only single organ involvement (mean: 233 mg/dL) (22). In the present case, the high serum IgG4 level (2,920 mg/dL) was consistent with multiple organ involvement, including swollen submandibular and parotid glands and masses surrounding the coronary arteries. Patients presenting with high serum levels of IgG4 should be investigated for multiple organ involvement. Of note, among the 10 cases including the present case, 7 had an AAA or aortitis (6, 9, 11, 13, 15, 18, the present case). The incidence of IgG4-RD associated inflammatory abdominal aortic aneurysm (IAAA) was 57% among the patients with surgically treated IAAA (23). If IAAA is detected, the possibility of IgG4-RD should be considered.
A prospective cohort study revealed that FDG-PET was a useful tool for assessing multiple organ involvement and monitoring the therapeutic effects in IgG4-RD (24). In the present case, FDG-PET was useful for diagnosing multiple organ involvement. Although the abnormal FDG uptake disappeared after treatment with prednisolone, only a modest decrease in the FDG uptake was observed in the area corresponding to the abdominal aorta. The reasons for only a modest decrease in the FDG uptake are considered to be as follows: (1) Only modest inflammation remained in the abdominal aorta after surgery, and treatment with 0.6 mg/kg/day of prednisolone was sufficient for IgG4-RD-associated peri-aortitis; and (2) This modest decrease in the FDG uptake indicated the effect of the implantation of the aortic prosthesis (25).
In conclusion, echocardiography should be used as a screening tool for the early detection of coronary artery involvement in IgG4-RD patients.
Author's disclosure of potential Conflicts of Interest (COI).
Hitoshi Kohsaka: Honoraria, Ono Pharmaceutical; Research funding, Chugai Pharmaceutical, Mitsubishi Tanabe Pharma Corporation, Ono Pharmaceutical, Astellas Pharma and Eisai.
References
- 1. Cheuk W, Yuen HK, Chu SY, Chiu EK, Lam LK, Chan JK. Lymphadenopathy of IgG4-related sclerosing disease. Am J Surg Pathol 32: 671-681, 2008. [DOI] [PubMed] [Google Scholar]
- 2. Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol 38: 982-984, 2003. [DOI] [PubMed] [Google Scholar]
- 3. Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med 344: 732-738, 2001. [DOI] [PubMed] [Google Scholar]
- 4. Hamano H, Kawa S, Ochi Y, et al. Hydronephrosis associated with retroperitoneal fibrosis and sclerosing pancreatitis. Lancet 359: 1403-1404, 2002. [DOI] [PubMed] [Google Scholar]
- 5. Stone JH, Khosroshahi A, Deshpande V, Stone JR. IgG4-related systemic disease accounts for a significant proportion of thoracic lymphoplasmacytic aortitis cases. Arthritis Care Res 62: 316-322, 2010. [DOI] [PubMed] [Google Scholar]
- 6. Matsumoto Y, Kasashima S, Kawashima A, et al. A case of multiple immunoglobulin G4-related periarteritis: a tumorous lesion of the coronary artery and abdominal aortic aneurysm. Hum Pathol 39: 975-980, 2008. [DOI] [PubMed] [Google Scholar]
- 7. Kamisawa T, Funata N, Hayashi Y, et al. Close relationship between autoimmune pancreatitis and multifocal fibrosclerosis. Gut 52: 683-687, 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kitagawa S, Zen Y, Harada K, et al. Abundant IgG4-positive plasma cell infiltration characterizes chronic sclerosing sialadenitis (Küttner's tumor). Am J Surg Pathol 29: 783-791, 2005. [DOI] [PubMed] [Google Scholar]
- 9. Ikutomi M, Matsumura T, Iwata H, et al. Giant tumorous lesions (correction of legions) surrounding the right coronary artery associated with immunoglobulin-G4-related systemic disease. Cardiology 120: 22-26, 2011. [DOI] [PubMed] [Google Scholar]
- 10. Debonnaire P, Bammens B, Blockmans D, Herregods MC, Dubois C, Voigt JU. Multimodality imaging of giant coronary artery aneurysms in immunoglobulin G4-related sclerosing disease. J Am Coll Cardiol 3: 59, 2012. [DOI] [PubMed] [Google Scholar]
- 11. Takei H, Nagasawa H, Sakai R, et al. A case of multiple giant coronary aneurysms and abdominal aortic aneurysm coexisting with IgG4-related disease. Intern Med 51: 963-967, 2012. [DOI] [PubMed] [Google Scholar]
- 12. Tanigawa J, Daimon M, Murai M, Katsumata T, Tsuji M, Ishizaka N. Immunoglobulin G4-related coronary periarteritis in a patient presenting with myocardial ischemia. Hum Pathol 43: 1131-1134, 2012. [DOI] [PubMed] [Google Scholar]
- 13. Hourai R, Miyamura M, Tasaki R, et al. A case of IgG4-related lymphadenopathy, pericarditis, coronary artery periarteritis and luminal stenosis. Heart Vessels 31: 1709-1713, 2016. [DOI] [PubMed] [Google Scholar]
- 14. Tran MN, Langguth D, Hart G, et al. IgG4-related systemic disease with coronary arteritis and aortitis, causing recurring critical coronary ischemia. Int J Cardiol 15: 33-34, 2015. [DOI] [PubMed] [Google Scholar]
- 15. Nishimura S, Amano M, Izumi C, et al. Multiple coronary artery aneurysms and thoracic aortitis associated with IgG4-related disease. Intern Med 55: 1605-1609, 2016. [DOI] [PubMed] [Google Scholar]
- 16. Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol 25: 1181-1192, 2012. [DOI] [PubMed] [Google Scholar]
- 17. Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD). Mod Rheumatol 22: 21-30, 2011. [DOI] [PubMed] [Google Scholar]
- 18. Kusumoto S, Kawano H, Takeno M, et al. Mass lesions surrounding coronary artery associated with immunoglobulin G4-related disease. JC Cases 5: e150-e154, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Patel NR, Anzalone ML, Buja LM, Elghetany MT. Sudden cardiac death due to coronary artery involvement by IgG4-related disease: a rare, serious complication of a rare disease. Arch Pathol Lab Med 138: 833-836, 2014. [DOI] [PubMed] [Google Scholar]
- 20. Shimizu Y, Yamamoto M, Naishiro Y, et al. Necessity of early intervention for IgG4-related disease-delayed treatment induces fibrosis progression. Rheumatology (Oxford) 52: 679-683, 2013. [DOI] [PubMed] [Google Scholar]
- 21. Ohira H, Tsujino I, Yoshinaga K. 18F-Fluoro-2-deoxyglucose positron emission tomography in cardiac sarcoidosis. Eur J Nucl Med Mol Imaging 38: 1773-1783, 2011. [DOI] [PubMed] [Google Scholar]
- 22. Carruthers MN, Khosroshahi A, Augustin T, et al. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann Rheum Dis 74: 14-18, 2015. [DOI] [PubMed] [Google Scholar]
- 23. Zen Y, Kasashima S, Inoue D. Retroperitoneal and aortic manifestations of immunoglobulin G4-related disease. Semin Diagn Pathol 29: 212-218, 2012. [DOI] [PubMed] [Google Scholar]
- 24. Zhang J, Chen H, Ma Y, et al. Characterizing IgG4-related disease with 18F-FDG PET/CT: a prospective cohort study. Eur J Nucl Med Mol Imaging 41: 1624-1634, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wassélius J, Malmstedt J, Kalin B, et al. High 18F-FDG Uptake in synthetic aortic vascular grafts on PET/CT in symptomatic and asymptomatic patients. J Nucl Med 49: 1601-1605, 2008. [DOI] [PubMed] [Google Scholar]