Abstract
Several MRI contrast agent clinical formulations are now known to leave deposits of the heavy metal gadolinium in the brain, bones, and other organs of patients. This persistent biological accumulation of gadolinium has been recently recognized as a deleterious outcome in patients administered Gd-based contrast agents (GBCAs) for MRI, prompting the European Medicines Agency to recommend discontinuing the use of over half of the GBCAs currently approved for clinical applications. To address this problem, we find that the orally-available metal decorporation agent 3,4,3-LI(1,2-HOPO) demonstrates superior efficacy at chelating and removing Gd from the body compared to diethylenetriaminepentaacetic acid, a ligand commonly used in the United States in the GBCA Gadopentetate (Magnevist). Using the radiotracer 153Gd to obtain precise biodistribution data, the results herein, supported by speciation simulations, suggest that the prophylactic or post-hoc therapeutic use of 3,4,3-LI(1,2-HOPO) may provide a means to mitigate Gd retention in patients requiring contrast-enhanced MRI.
Introduction
The use of gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) has been ubiquitous in radiology for nearly three decades1. Recently however, it has come to light that the suboptimal biological stability of GBCAs can lead to accumulation of Gd in patients’ bone and brain tissue, as well as to kidney damage and associated systemic conditions due to compromised renal function2–4. These findings have prompted a substantial volume of new reports on the identification of residual Gd accumulation in contrast MRI patients, with the emerging consensus that GBCAs of the so-called “linear” type deposit more Gd into the body than their macrocyclic counterparts (Fig. 1). In one study, the linear contrast agent Gadodiamide (Omniscan), a derivative of the diethylenetriaminepentaacetic acid (DTPA) chelator currently in use as a metal decorporation agent5, was found to release 24% of its Gd3+ payload after only a single day in human serum; a number that increases to 64% in the presence of elevated phosphate levels4. In July 2017 the European Medicines Agency recommended suspending the intravenous use of Gadodiamide and Gadopentetate ([Gd(DTPA)]2−, Magnevist) in light of the available data, and in September 2017, the U.S. Food and Drug Administration’s Medical Imaging Drugs Advisory Committee recommended that prescribing information should include “a warning for retention for all GBCAs, with greater retention of all or some of the linear GBCAs compared to the macrocyclics in certain organs including the brain”.
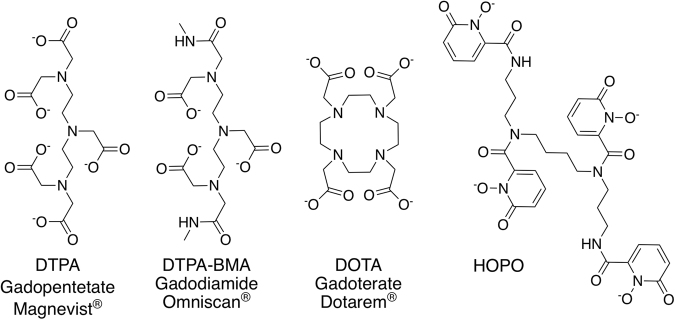
Figure 1.
Structures of exemplary linear (DTPA, DTPA-BMA) or macrocyclic (DOTA) ligands used as GBCAs (generic and trade names are given for the corresponding Gd3+ complexes) and of the experimental chelator used in this study (HOPO).
While much of the literature has addressed both the cause and nature of metal accumulation in vivo6, little emphasis is placed on the prevention or remediation of Gd deposition. In this study, the chelating agent 3,4,3-LI(1,2-HOPO), or HOPO, is evaluated relative to DTPA as a preventive treatment for Gd accumulation (Fig. 1).
HOPO is an octadentate hydroxypyridinone ligand that is among the most competent chelating agents for heavy f-block metals (log KML at pH 7.4 for Gd of 20.5(1))7. It is orally available, non-toxic at therapeutic dosages, and is extremely selective for actinide and lanthanide ions over biologically-relevant metal ions such as iron, potassium, and calcium8. These are highly advantageous properties for a therapeutic chelator, and thus HOPO has been approved for a first-in-human Phase 1 safety trial as an actinide decorporation agent9. This led us to surmise that HOPO could provide an effective treatment for preventing and remediating the biological accumulation of Gd that has been observed in numerous recent studies. To evaluate this hypothesis, the respective efficacies of HOPO and DTPA as decorporation agents for the radiotracer 153Gd were probed in a murine model8,10.
Results
Bodily 153Gd Accumulation
Intraperitoneal (ip) administration of both HOPO and DTPA was found to promote the clearance of 153Gd, and for both chelators, the extent of clearance varies with administration time relative to 153Gd contamination. Figure 2 shows the total percentage of the Gd dose recovered from the subject animals for each treatment group (%RD), as well as the distribution of 153Gd found in selected organ systems. In the absence of treatment nearly 60% of 153Gd was retained in the body after 4 days; primarily from the skeleton (41% RD), soft and abdominal tissues (4% RD), and excretory organs (liver 11% RD, kidneys 1% RD). These data reflect the established propensity of heavy metals to accumulate in the skeleton, and it is noted that this biodistribution, particularly the elevated liver accumulation of Gd compared to other non-skeletal organ systems, is consistent with previous reports11,12. While all treatment groups in the present study show an increase in cleared 153Gd, three are notable in their ability to reduce the amount of retained metal to under 10% RD. Treatment with DTPA 1 h prior to contamination lowered the amount of bodily153 Gd to 9.4 ± 1.3% RD, while administration of HOPO either 24 h or 1 h prior to contamination reduced the amount of retained metal to 6.3 ± 1.6% RD and 1.04 ± 0.18% RD, respectively. The latter treatment regimen corresponds to more than a 50-fold decrease in bodily 153Gd content compared to the control group, but more importantly a roughly 9-fold decrease relative to DTPA, one of the linear GBCAs currently approved for clinical use in the United States.
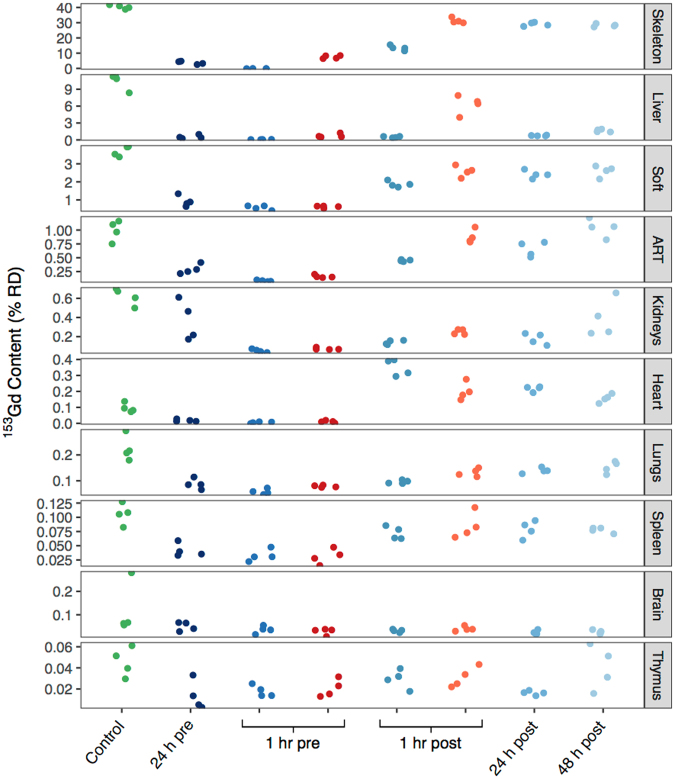
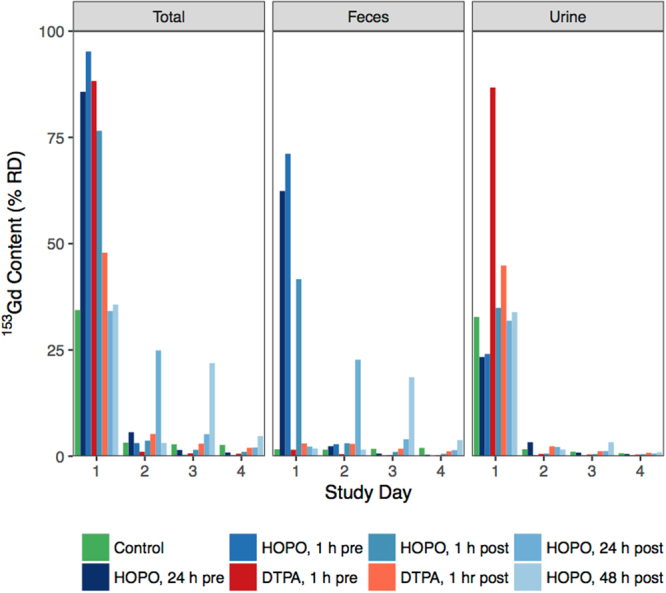
Figure 2.
Total murine body content and distribution of 153Gd four days following contamination via intravenous injection into a warmed lateral tail vein, reported as % RD. Treatments were administered at a dose of 100 μmol/kg via ip injection at times varying from 24 h pre- to 48 h post-Gd injection. Analyzed organ systems that comprise at least 1% RD are shown. Unless otherwise indicated, the results of one-way ANOVA (Dunnett’s method) yielded p-values < 0.001 (n.s., not significant, **p < 0.01).
Of particular interest are the organs that exhibit substantial levels of Gd in this model, as well as those that show lasting Gd accumulation in human patients with potentially negative health outcomes: skeleton, liver, kidneys, and brain. Figures 2 and 3 show that for all treatment groups except a 1 h pre-treatment with HOPO, skeletal 153Gd makes up the majority of the recovered bodily content. For that particular treatment however, there is complete prevention of Gd accumulation in the skeleton. As previously mentioned approximately 11% RD was recovered from the liver in the control group (Tables S1, 2, Fig. 3). Interestingly, all of the treatments succeeded in reducing this burden to <2% RD except 1 h post-contamination DTPA, where 6.3 ± 1.6% RD was found in the liver (2). The substantially lower liver content of the 1 h pre-contamination DTPA treatment (0.78 ± 0.33% RD) suggests that while DTPA can effectively chelate Gd in other organ systems and prevent its accumulation in liver tissue, either it cannot effectively compete for Gd binding with hepatic proteins or small molecules, or it simply does not reach appreciable concentrations in liver tissue. In contrast, administration of HOPO even 48 h following contamination reduces the 153Gd liver content to 1.68 ± 0.24% RD, suggesting that HOPO is capable of diffusing to the highly vascularized liver tissue and also exhibits a higher affinity for Gd than do endogenous biomolecules.
Figure 3.
Murine organ content of 153Gd four days following contamination, reported as %RD. Data points correspond to the values obtained for each mouse in a group (n = 4). The data points on the right side of the 1 hr pre and 1 hr post groups (red and orange) received treatment with DTPA, and all other non-control groups received HOPO. Organs are ranked in order of contribution to the total RD.
There is now a substantial body of literature implicating Gd from GBCAs in the onset of nephrogenic systemic fibrosis (NSF) in patients with suppressed renal function13,14. Thus, the accumulation of Gd in kidneys is of importance. Nephrogenic 153Gd accumulation in the control group accounts for 0.62 ± 0.09% RD, and all treatment regimens were able to promote a reduction in 153Gd content. A 1 h pre-contamination treatment of either HOPO or DTPA showed the most substantial effect, resulting in statistically-equivalent burdens of 0.06 ± 0.02% and 0.08 ± 0.01% RD, respectively. For both chelators, delayed administration increases the 153Gd kidney concentration, suggesting that their ability to recover 153Gd is impaired over time. Given that the chelators’ pharmacokinetic profiles should not be impacted by the administration time relative to contamination, the data may indicate that progressively, kidney physiology could promote formation of Gd species that are more resistant to chelation by DTPA or HOPO.
Recent studies have also highlighted the accumulation of Gd in the brain tissue of otherwise healthy patients, and the degree to which linear and macrocyclic GBCAs lead to such deposition remains an area of active debate3,15–18. Accordingly, the accumulation of 153Gd in the brain tissue was examined in greater detail. In the control group, an outlying data point (Fig. 3) was detected and removed (Q-value >0.95), to give a corrected concentration of 0.063 ± 0.003% RD. This value is second only to the thymus for the least amount of accumulated 153Gd, and there is no statistical difference between groups, seemingly contrary to many of the studies referenced previously. However we note that as the timescale of intra-cranial Gd deposition is unclear, the experiment duration (4 d) was possibly too short to observe appreciable accumulation in the brain. Additionally, the physiological Gd concentration in the present study is at radiotracer levels; roughly 100 million times lower than therapeutic concentrations for contrast MRI. This may simply be too low to observe intracranial accumulation if there is a threshold concentration for Gd transiting the blood-brain barrier.
153Gd in Excreta
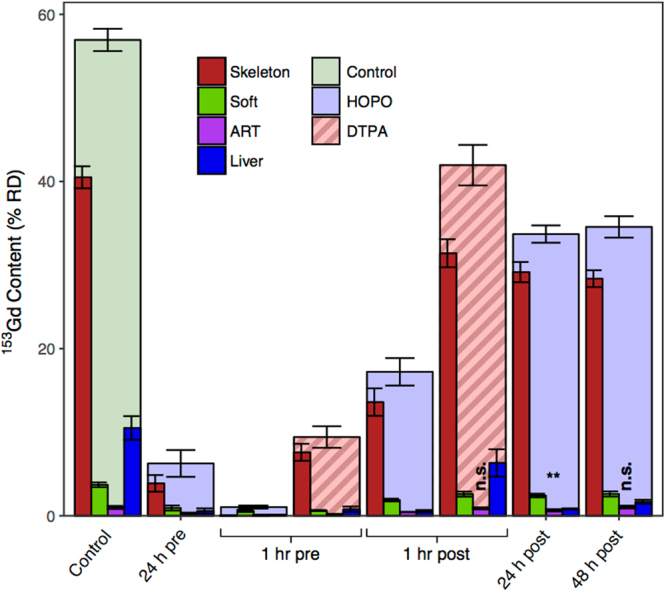
In addition to bodily accumulation, the excreta were collected daily and assayed for 153Gd content. Figure 4 shows the 153Gd recovered from the excreta of all study groups, as well as the relative amounts found in the urine and feces. The excreta of the control group contained 34.4% RD on day 1, with a roughly 95% urine and 5% feces ratio. On all subsequent days an additional ≈3% was found in the total excreta. Interestingly, while on day 2 an equal amount of 153Gd was found in the urine and feces, on days 3 and 4 the ratio of excreted Gd shifted towards increased concentration in the feces, indicating that while the urinary metabolism is responsible for the initial clearance of Gd, over time the remaining metal is cleared through solid waste. For the treatment groups, the cumulative total excreta on day 4 are, as expected, the inverse of the total bodily accumulations (Figure S1). The most dramatic difference between treatment groups is that upon treatment with HOPO, a substantial increase in fecal clearance is observed, whereas DTPA promotes clearance through the urinary pathway only. This is most clearly observed in the groups receiving HOPO 24 and 48 h post-contamination; those treatment groups are statistically identical to the control until treatment, whereupon a significant increase in fecal excretion is found. It is noted that this is consistent with the observed capacity of HOPO to reduce liver concentrations of 153Gd when administered 48 h post-contamination. In contrast, DTPA is cleared via the renal pathway, and even a 1 h post-contamination administration leaves substantial Gd accumulation in the liver tissue.
Figure 4.
Excreted 153Gd by study day and excretion route, reported as %RD. Treatments were administered at a dose of 100 μmol/kg via ip injection at times varying from 24 h pre- to 48 h post-Gd injection. Treatment groups administered HOPO show significant enhancement of fecal excretion relative to both control and groups receiving DTPA.
Discussion
Biodistribution and Decorporation
The data presented here illustrate the fundamental propensity of Gd3+ to accumulate in various organ systems, and provide insight into the strengths and weaknesses of DTPA as a prototypical linear GBCA ligand. The primary purpose of this study was to determine the biodistribution of Gd and understand the changes engendered by two different chelating agents, and to ultimately inform the design or selection of chelators that are more ideally compatible with the biochemistry of Gd. While it is clearly of interest to consider the implications of these findings in light of present concerns regarding the widespread use of GBCAs, we caution that a few key differences preclude direct comparison of these data to post-hoc studies of clinical subjects. First, the concentration of the 153Gd radiotracer (≈0.67 pmol/kg) was tailored to provide accurate dosimetry without unnecessary radiation exposure to either the subject animals or the researchers, and as mentioned previously the concentrations of Gd are lower than clinical doses (0.1 mmol/kg) by roughly seven orders of magnitude, adjusting for the human-equivalent dose19,20. Additionally, clinical formulations of Gd-DTPA only contain a 0.1% excess of DTPA4, however in the present study the chelator concentrations were 100 μmol/kg, a >10 million-fold excess. A higher level of Gd deposition can therefore be expected in the case of an actual Gd-DTPA MRI formulation20.
Despite these deviations from clinically-relevant conditions, the varying effects of the chelation treatments on 153Gd biodistribution give rise to important conclusions regarding the biochemistry of Gd in various organ systems. Deposition in the skeleton is the ultimate fate of a substantial fraction of the retained contaminant. However, consistent with previous studies on the decorporation of other f-elements such as 238Pu4+ 21,22, 241Am3+ 19, or 152Eu3+ 7, HOPO is more effective than DTPA at reducing the overall skeletal content of the heavy metal, even when administered up to 48 h post-contamination. In comparison, administration of DTPA only 1 h post-contamination cannot prevent Gd accumulation in the skeleton as efficiently. It is noted that our previous studies examining the chelation of 238Pu by HOPO determined that administration even 7 d post-contamination was as efficacious as administration 1 d post-contamination; were the present study extended further, we posit that similar behavior could be anticipated. It is also probable that repeated administration of HOPO could further improve the clearance of Gd from the body.
Synthesis of the concentration data from the liver, kidneys, and excreta derives a more comprehensive picture of the differences in pharmacokinetics between DTPA and HOPO. The inability of DTPA to retroactively clear Gd from the liver, even at 1 h post-contamination, suggests that either the biochemistry of liver tissue suppresses complexation of Gd, or that DTPA is rapidly metabolized via the kidneys and has negligible circulation through the liver. The almost exclusive elimination of Gd in the urine following treatment with DTPA indicates that the latter is, in our opinion, more likely. In contrast, HOPO effectively removes 153Gd from the liver even if administered 48 h post-contamination. Coupled with the sizable increase in fecal excretion upon treatment with HOPO, as well as the negligible fecal clearance of the control group, the data present a compelling case that the Gd-HOPO complex is metabolized through the liver and cleared as solid waste. While the use of linear GBCAs in patients with advanced kidney disease has been largely discontinued, the genesis of Gd-induced nephrotoxicity and the potential implications for otherwise healthy patients have not been established. Thus, it would seem that a decorporation strategy that does not utilize the renal excretion pathway could be advantageous.
Finally, in the present study, treatment with a chelating agent had statistically no influence on the extent of 153Gd recovered from the brain tissue; however as discussed previously it is highly possible that either the timescale or the concentration regime of this experiment precluded the observation of any treatment group-dependent trends. Intra-cranial Gd deposition has received substantial attention in the recent literature, with mounting evidence that even in patients with uncompromised renal function, Gd will accumulate in various regions of the brain1,16,18,23. Additionally, efforts to characterize the speciation of Gd in both brain and other tissues have identified insoluble Gd-containing deposits high in phosphate and calcium, strongly suggesting that Gd is no longer associated with the intended chelating agent6,24. As such, it would seem imperative that more effective chelators be employed. While the present data reveal no specific trends regarding Gd deposition in brain tissue, the overall decorporation efficacies indicate that HOPO is a far better chelator of Gd compared to DTPA, particularly if the present data are indicative of delayed intracranial Gd accumulation; in this case HOPO would be expected to substantially mitigate this problem.
Gd Speciation in Physiological Conditions
In the present context, the effectiveness of a chelator is determined by its ability to maintain coordination in vivo, which is of importance for preventing the precipitation of Gd deposits in the body. To properly address this question the speciation of Gd must be considered in the presence of not only the chelator, but also additional biological anions capable of coordinating the metal. The in vivo chemistry of exogenous metals such as Gd is far too complex to be modeled completely, as it would require knowledge of the thermodynamic and kinetic properties of all potential ligands (small inorganic and organic molecules, transport proteins, etc.). Ideally, the effect of the ionic strength, temperature, viscosity, local concentration and interference with essential cations such as Fe3+, Ca2+, and Zn2+ would also be taken into account, but these necessary data are not known for many of the chelators utilized in GBCAs. We have therefore performed speciation simulations for the most common Gd3+-MRI chelator systems, utilizing published thermodynamic parameters and accounting for the presence of the most abundant and relevant natural chelators: phosphates, carbonates, hydroxides, oxalates, lactates, and citrates, as well as the synthetic chelators themselves (Table S3).
Parameterization of metal complex stability to account for chelators of different nature, acidity, and denticity in a biological environment is a nontrivial problem. To enable a direct comparison of common exogenous chelators utilized for Gd and other metals in vivo, the simulations performed here consisted of lowering the concentration of Gd and the synthetic chelator at constant pH and concentration of endogenous ligands. This aims to mimic the progressive dilution or clearance of the GBCA from the blood stream, and as the concentrations decrease at static conditions of the other ligands, ultimately the chelator is unable to compete with the biological molecules and Gd is released. The concentration at which this is predicted to occur allows for the evaluation of the relative stability of the synthetic chelators post-treatment. Figure 5 shows the results of the simulations for the Gd-chelator complexes of ethylenediaminetetraacetate (EDTA), DTPA-BMA, DTPA, DOTA, and HOPO (Fig. 1), in the presence of competing biological ligands and at physiological pH. We chose DTPA-BMA, DTPA, and DOTA as models for speciation calculations in part due to the availability of thermodynamic parameters for these particular ligands, but mostly because all other currently used GBCAs are derived from these molecular structures.
Figure 5.
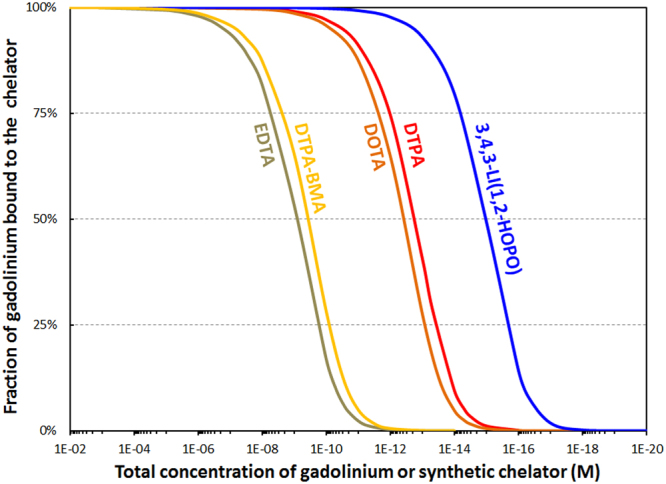
Calculated percentage of gadolinium bound to various chelators relevant for MRI as a function of dilution and under biological conditions. Total concentrations of phosphates (1.1 mM), carbonates (25 mM), oxalates (9.2 μM), lactates (1.5 mM), and citrates (160 μM) held constant to match physiological conditions. Ratio Gd/synthetic chelator = 1.0 mol/mol. pH = 7.4. See Table S3 for stability constants used in these speciation simulations.
EDTA has been included because it is available and commonly used for chelation therapy of lead, another heavy metal. Figure 5 suggests that HOPO outperforms all challenge chelators by at least two orders of magnitude. In line with the in vivo studies with Gd ions, the binding ability of the synthetic chelators extrapolated from the speciation simulation is as follows: EDTA = DTPA-BMA < DTPA = DOTA < HOPO. The simulation does not however account for differences in kinetic inertness between chelators; while the macrocyclic DOTA chelator for example has a lower stability constant than DTPA, the activation energy for demetallation is substantially greater, and DOTA has thus emerged as a more stable chelator than DTPA in vivo4,25,26. A few additional points from this simulation should be noted. First, while numerical values are provided on the x-axis, they should be taken as relative stabilities rather than absolute: Other endogenous challengers (such as metal-binding proteins and other metal ions)27 are present in actual biological media in addition to those taken into account in the present speciation studies. Therefore the thresholds at which the synthetic chelators release Gd are expected to be higher in actuality, but this offset due to other natural ligands is expected to be very similar.
Once the Gd is released, an equilibrium is predicted between citrate, carbonate, and phosphate (Figs S3–4), however precipitation of Gd phosphate, the least soluble species, depletes that term of the equilibrium expression. In an abundance of phosphate, the equilibrium is expected to shift, inducing continued precipitation and formation of Gd phosphate deposits, as has been reported in the tissues of patients receiving GBCAs6,24. Further, speciation was also calculated for the Gd-DTPA and Gd-DTPA-BMA complexes in the presence of Ca2+ and Zn2+ ions, since the stability constants of the Ca-DTPA, Ca-DTPA-BMA, Zn-DTPA, Zn-DTPA-BMA, and the Ca2+ and Zn2+ complexes of the relevant endogenous ligands are known (Table S3). The in vivo exchange of metal ions, commonly referred to in the literature as transmetallation, is a compelling theory that rationalizes the release of Gd3+ in the body, and our results show an important Gd3+-Zn2+ transmetallation effect for both linear chelators. Ca2+ is a weaker competitor for GBCAs than Zn2+ but both endogenous metals can displace Gd3+ from the pharmaceutical complexes below a certain concentration (Fig. 6, Figure S5).
Figure 6.
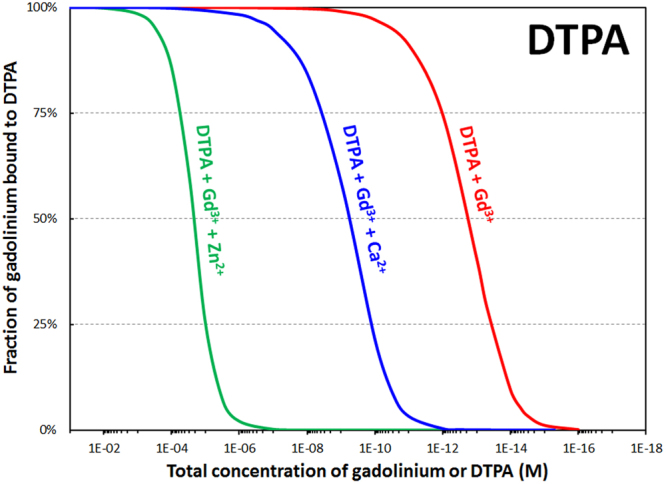
Calculated percentage of gadolinium bound to DTPA as a function of dilution in the presence of biological chelators, and with inclusion of physiological concentrations of calcium (1.1 mM) or zinc (15 μM). Total concentrations of phosphates (1.1 mM), carbonates (25 mM), oxalates (9.2 μM), lactates (1.5 mM), and citrates (160 μM) held constant to match physiological conditions. Ratio Gd/synthetic chelator = 1.0 mol/mol. pH = 7.4. See Table S3 for stability constants used in these speciation simulations.
These simulations provide excellent rationale for the elevated levels of urinary Zn (zincuria) that have been observed in both human and animal studies13, given that our findings indicate urinary clearance of the Mn+-DTPA complexes7,19,21,22. It then seems likely that Zn transmetallation of GBCAs in the kidneys could be implicated as an underlying cause of NSF.
These speciation simulations were based on published thermodynamic parameters, and are to the best of our knowledge wholly supported by the available clinical data. In theory, the observed in vivo behavior of these linear GBCAs, both in terms of phosphate precipitation and Zn transmetallation, could have been predicted from such simulations prior to their clinical use. Consideration of biologically-relevant metals as coordination complexes, both exogenous and otherwise, can provide rational solutions to problems such as release of Gd in vivo, utilizing existing knowledge of the coordination preferences of alkali earth, transition, and heavy metals. DTPA and most other GBCA chelators are promiscuous in their chelation of metal ions, and the adverse chelation of Zn2+ and other vital biological cations such as Ca2+, Mg2+, and Fe3+ is a key reason for the inherent toxicity of DTPA and other chelators28.
In stark contrast, the HOPO chelator is, by design, highly selective for lanthanide and actinide ions. This octadentate ligand binds metal ions through the eight oxygen donor atoms of its four bidentate binding units, and is ideally suited to the larger f-block cations, while disfavoring complexation of transition metals and Group I or II ions ubiquitous in biology. In fact, the maximum tolerated dose of HOPO in rats was determined to be in excess of 100 μmol kg−1 d−1 over 28 days of daily oral administration9,19,22. The higher acidity of HOPO (highest p Ka = 6.6) compared to DTPA (10.4) or DOTA (11.2) makes it more resistant to intrinsic competition between ligand protonation and metal binding at low concentrations. Due to its high denticity and steric bulk, we anticipate Gd-HOPO to be an ineffective MRI contrast agent, since all coordination sites of Gd3+ should be occupied and no water molecules are expected within the first coordination sphere, consistent with findings from time-resolved fluorescence measurements on the corresponding Eu3+ complex7. However, this same property makes it an excellent Gd-decorporation molecule compared to the GBCA chelators examined herein. Thus, one could envision a scenario where a currently-approved GBCA is administered, the MRI is performed, and a subsequent regimen of HOPO is prescribed to chelate and remove any Gd3+ that dissociates from the GBCA29,30.
In light of current data, the oral availability, safety, and selectivity for f-block elements make the metallobiochemistry of HOPO ideally suited to address the issue of Gd accumulation in patients receiving GBCAs. Subsequent experiments will address key outstanding questions; namely, how do the differences in chelator and Gd3+ concentration and stoichimetry impact biodistribution, and does the co- or pre-administration of HOPO adversely impact the ability of GBCAs to provide the t1 relaxation enhancement needed for contrast MRI. Finally, we plan to investigate if HOPO can provide improved clearance of Gd3+ from mice following dosing with clinically-relevant concentrations of linear and macrocyclic GBCAs. These studies will employ a wider range of GBCAs and treatment conditions, as well as therapeutic levels of Gd spiked with the 153Gd radiotracer for concurrent dosimetry. Considering the many patients who have undergone contrast MRIs and may have bodily Gd accumulation, the present data suggest that the HOPO chelator could provide improved retroactive chelation treatment compared to other ligands currently used for such applications. Previous work has shown that HOPO will circulate to the brain and bones31, and also that delayed treatment with HOPO is effective at removing 238Pu4+ from mice21. We note that the timescale of contamination relative to treatment, as well as the chemical speciation of deposited Gd, are additional factors to be explored when evaluating HOPO as a post-hoc Gd remediation therapy.
Conclusions
From the perspective of coordination chemistry, the design of a successful agent for contrast MRI is somewhat paradoxical. The ligand must have sufficient affinity and selectivity for Gd so as to be stable in vivo, either from competition for Gd by endogenous ligands or transmetallation of the chelator by bioavailable metals; however, without at least one open coordination site for water to bind, t1 relaxation enhancement is quenched and the complex ceases to perform as a contrast agent. Thus, many of the best ligands for chelating Gd, including HOPO, may be unsuitable as contrast agents because the chelator occupies all available coordination sites. Recognizing the value of the clinical data afforded by contrast-enhanced MRI, such insight inspires a critical evaluation of the current strategies employed for GBCAs, and in particular raises the question of whether a single-chelator approach is in fact the safest and most effective means to provide MRI contrast. We eagerly anticipate the creative consideration of the points raised herein, as well as the properties of f-block-specific chelators such as HOPO, in the rapidly-expanding body of literature in this field.
Methods
Metal and Ligand Solutions
A stock solution of 153Gd-chloride in 1 M HCl was purchased from Eckert and Ziegler Isotope Products (Valencia, CA, USA). Contamination doses consisted of 0.2 mL aliquots of solutions containing 0.925 kBq (6.94 pg) of 153Gd in 0.008 M sodium citrate and 0.14 M NaCl, pH 4. 3,4,3-LI(1,2-HOPO) was prepared by Ash Stevens, Inc. (Detroit MI, USA), as described previously9. DTPA was obtained from Sigma-Aldrich (St. Louis, MO, USA) and was formulated as Ca-DTPA using CaCO3 and NaOH, similar to the formerly available drug product commercialized by Hameln Pharmaceuticals GmbH (Hameln, Germany). Ligand solutions were prepared such that the dosage of 100 μmol/kg was contained in 0.5 mL of 0.14 M NaCl, with the pH adjusted to 7.4–8.4 with 1 N NaOH. All solutions were filter-sterilized (0.22 μm) prior to administration.
Animals and General Procedures
All procedures and protocols used in the described in vivo studies were reviewed and approved by the Institutional Animal Care and Use Committee of Lawrence Berkeley National Laboratory, and were performed in AAALAC-accredited facilities according to prescribed guidelines and regulations. The animals were young adult (102 days old) female (31.7 ± 2.1 g) Swiss-Webster mice (Simonsen Laboratories, Gilroy, CA, USA). Gross body and tissue compositions, plasma, extracellular fluid, and red cell volumes of the whole body, major tissues and organs of these mice have been determined previously32. Mice were kept under a 12 h light cycle with controlled temperature (18–22 °C) and relative humidity (30–70%), and were given water and food ad libitum. Each group was housed together in a plastic stock cage lined with a 0.5 cm layer of highly absorbent low-ash pelleted cellulose bedding (ALPHA-dri) for separation of urine and feces. Intravenous (iv) injections into a warmed lateral tail vein, ip injections, and euthanasia were performed under isoflurane anesthesia. Treatment dose volumes were adjusted based on the weight of the mouse, with a 0.5 mL volume corresponding to a 35-g mouse. To probe the effect of delayed treatment, groups of four mice were injected iv with a single dose of 153Gd-citrate, and ligand or control saline solutions were administered ip once at the following post-contamination treatment times: 1 h, 24 h, 48 h. To probe the effect of prophylactic treatment, groups of four mice were first administered ligand or control saline solutions ip once at the following pre-contamination treatment times: −1 h and −24 h. Mice were then injected iv with a single dose of 153Gd-citrate. Excreta were collected daily for 4 days until scheduled necropsy (4 days after metal challenge). Mice were euthanized by cervical dislocation over their respective cage to collect the excreta expelled at death, and immediately frozen for later dissection.
Tissue Sampling and Processing
Brains, thymuses, hearts, lungs, livers, spleens, and kidneys were dissected, and the abdominal remainder tissue (ART, which includes intact gastrointestinal (GI) tract, reproductive organs, urinary bladder, and abdominal fat) was removed. The organ samples and partially eviscerated carcasses were managed as individual samples. Feces samples were separated manually from urine-stained cellulose bedding and treated as group samples (one group per cage). All samples were dried at 100 °C and dry-ashed at 575 °C. The ashed samples were treated with concentrated HNO3. These acidified solutions were then homogenized in dilute HNO3 and mixed with Ultima Gold (Perkin Elmer, Shelton, CT, USA) for detection by liquid scintillation counting (Packard Tri-Carb model B4430, Perkin Elmer). Additional details of autopsy procedures, tissue and excreta collection and processing, as well as radioactivity measurements and methods of data reduction have been previously reported for similar experiments with several other long-lived radiotracers10,33.
Data management and analysis
All experiments used radioactive 153Gd as a contaminant and were managed as metabolic balance studies, in which all tissues and excreta were radioanalyzed; average radiochemical recoveries were all greater than 90% injected dose. All manipulation of the raw data was performed using the R program. The experimental data are reported as radionuclide fractions, expressed as percent of recovered 153Gd (%RD), and both graphical and tabulated values are reported as arithmetic means ± SD. The statistical significance of changes in 153Gd concentration was determined using one-way analysis of variance (ANOVA), and changes both pairwise and relative to the control group were assessed using Tukey’s and Dunnett’s tests respectively, as implemented in the Multcomp package for R. Unless otherwise noted, changes were considered significant for P < 0.001. Tests for statistical outliers were performed using Dixon’s Q test at a 95% confidence level as implemented in the Outliers package for R, where . The R script used to perform the analysis, as well as a complete ANOVA analysis, can be found at http://github.com/julianrees/2017_GdDecorporation.
Speciation calculations
All speciation calculations were performed using Hyperquad Simulation and Speciation software (HySS) in its high precision mode. HySS software was implemented with the published stability constants for the soluble species of Gd3+, Zn2+, and Ca2+ with the synthetic chelators of interest (DOTA, DTPA, DTPA-BMA, EDTA, and HOPO) and the endogenous chelators (hydroxides, phosphates, carbonates, citrates, lactates, and oxalates). The protonation constants of the chelators were also implemented in HySS software. Each speciation simulation contained between 40 and 74 equilibria. The stability constants used in this study are summarized in Table S3.
Electronic supplementary material
Acknowledgements
This work was supported by an Innovation Grant from the Lawrence Berkeley National Laboratory, operating under U.S. Department of Energy Contract No. DE-AC02-05CH11231.
Author Contributions
J.A.R., G.J.P.D., D.D.A. and R.J.A. designed research; G.J.P.D., D.D.A., C.A., S.S.G. and R.J.A. performed experimental work; J.A.R., G.J.P.D., D.D.A. and R.J.A. analyzed data; J.A.R., G.J.P.D. and R.J.A. wrote the manuscript.
Competing Interests
R.J.A. and G.J.P.D are listed as inventors on two separate patent applications filed by the Lawrence Berkeley National Laboratory and describing inventions related to the research results presented here.
Footnotes
Julian A. Rees, Gauthier J.-P. Deblonde and Dahlia D. An contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-22511-6.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kanal E. Gadolinium based contrast agents (GBCA): Safety overview after 3 decades of clinical experience. Magnetic Resonance Imaging. 2016;34:1341–1345. doi: 10.1016/j.mri.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Broome DR, et al. Gadodiamide-associated nephrogenic systemic fibrosis: Why radiologists should be concerned. American Journal of Roentgenology. 2007;188:586–592. doi: 10.2214/AJR.06.1094. [DOI] [PubMed] [Google Scholar]
- 3.Kanda T, et al. Gadolinium-based Contrast Agent Accumulates in the Brain Even in Subjects without Severe Renal Dysfunction: Evaluation of Autopsy Brain Specimens with Inductively Coupled Plasma Mass Spectroscopy. Radiology. 2015;276:228–32. doi: 10.1148/radiol.2015142690. [DOI] [PubMed] [Google Scholar]
- 4.Frenzel T, Lengsfeld P, Schirmer H, Hütter J, Weinmann HJ. Stability of gadolinium-based magnetic resonance imaging contrast agents in human serum at 37 degrees C. Investigative radiology. 2008;43:817–828. doi: 10.1097/RLI.0b013e3181852171. [DOI] [PubMed] [Google Scholar]
- 5.Durbin PW, Lauriston S. Taylor Lecture: the quest for therapeutic actinide chelators. Health physics. 2008;95:465–92. doi: 10.1097/01.HP.0000326345.41816.c2. [DOI] [PubMed] [Google Scholar]
- 6.Xia D, Davis RL, Crawford JA, Abraham JL. Gadolinium released from MR contrast agents is deposited in brain tumors: in situ demonstration using scanning electron microscopy with energy dispersive X-ray spectroscopy. Acta radiologica (Stockholm, Sweden: 1987) 2010;51:1126–36. doi: 10.3109/02841851.2010.515614. [DOI] [PubMed] [Google Scholar]
- 7.Sturzbecher-Hoehne M, et al. 3,4,3-LI(1,2-HOPO): In vitro formation of highly stable lanthanide complexes translates into efficacious in vivo europium decorporation. Dalton Transactions. 2011;40:8340. doi: 10.1039/c1dt10840a. [DOI] [PubMed] [Google Scholar]
- 8.White DL, Durbin PW, Jeung N, Raymond KN. Specific sequestering agents for the actinides. 16. Synthesis and initial biological testing of polydentate oxohydroxypyridinecarboxylate ligands. Journal of Medicinal Chemistry. 1988;31:11–18. doi: 10.1021/jm00396a005. [DOI] [PubMed] [Google Scholar]
- 9.Abergel RJ, et al. Biomimetic Actinide Chelators: An Update on the Preclinical Development of the Orally Active Hydroxypyridonate Decorporation Agents 3,4,3-LI(1,2-HOPO) and 5-LIO(Me-3,2-HOPO) Health Physics. 2010;99:401–407. doi: 10.1097/HP.0b013e3181c21273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Durbin PW, Kullgren B, Xu J, Raymond KN. Multidentate hydroxypyridinonate ligands for Pu(IV) chelation in vivo: comparative efficacy and toxicity in mouse of ligands containing 1,2-HOPO or Me-3,2-HOPO. International journal of radiation biology. 2000;76:199–214. doi: 10.1080/095530000138853. [DOI] [PubMed] [Google Scholar]
- 11.Rogosnitzky M, Branch S. Gadolinium-based contrast agent toxicity: a review of known and proposed mechanisms. BioMetals. 2016;29:365–376. doi: 10.1007/s10534-016-9931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White GW, Gibby WA, Tweedle MF. Comparison of Gd(DTPA-BMA) (Omniscan) Versus Gd(HP-DO3A) (ProHance) Relative to Gadolinium Retention in Human Bone Tissue by Inductively Coupled Plasma Mass Spectroscopy. Invest Radiol. 2006;41:272–278. doi: 10.1097/01.rli.0000186569.32408.95. [DOI] [PubMed] [Google Scholar]
- 13.Swaminathan S. Gadolinium toxicity: Iron and ferroportin as central targets. Magnetic Resonance Imaging. 2016;34:1373–1376. doi: 10.1016/j.mri.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Marckmann P. Nephrogenic Systemic Fibrosis: Suspected Causative Role of Gadodiamide Used for Contrast-Enhanced Magnetic Resonance Imaging. Journal of the American Society of Nephrology. 2006;17:2359–2362. doi: 10.1681/ASN.2006060601. [DOI] [PubMed] [Google Scholar]
- 15.Lancelot E. Revisiting the Pharmacokinetic Profiles of Gadolinium-Based Contrast Agents. Investigative Radiology. 2016;51:691–700. doi: 10.1097/RLI.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 16.Murata N, et al. Macrocyclic and Other Non-Group 1 Gadolinium Contrast Agents Deposit Low Levels of Gadolinium in Brain and Bone Tissue. Investigative Radiology. 2016;00:1. doi: 10.1097/RLI.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 17.McDonald RJ, et al. Intracranial Gadolinium Deposition after Contrast-enhanced MR Imaging. Radiology. 2015;000:150025. doi: 10.1148/radiol.15150025. [DOI] [PubMed] [Google Scholar]
- 18.Radbruch A, et al. Gadolinium Retention in the Dentate Nucleus and Globus Pallidus Is Dependent on the Class of Contrast Agent. Radiology. 2015;275:150337. doi: 10.1148/radiol.2015150337. [DOI] [PubMed] [Google Scholar]
- 19.Bunin DI, et al. Dose-dependent efficacy and safety toxicology of hydroxypyridinonate actinide decorporation agents in rodents: towards a safe and effective human dosing regimen. Radiation research. 2013;179:171–82. doi: 10.1667/RR3115.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Administration, U. F. & Drug. FDA Guidance. Tech. Rep., USFDA, Rockville, MD (2005).
- 21.An DD, et al. 238Pu elimination profiles after delayed treatment with 3,4,3-LI (1,2-HOPO) in female and male Swiss-Webster mice. International Journal of Radiation Biology. 2014;90:1055–1061. doi: 10.3109/09553002.2014.925150. [DOI] [PubMed] [Google Scholar]
- 22.An DD, Kullgren B, Jarvis EE, Abergel RJ. From early prophylaxis to delayed treatment: Establishing the plutonium decorporation activity window of hydroxypyridinonate chelating agents. Chemico-Biological Interactions. 2017;267:80–88. doi: 10.1016/j.cbi.2016.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prybylski JP, Maxwell E, Coste Sanchez C, Jay M. Gadolinium deposition in the brain: Lessons learned from other metals known to cross the blood–brain barrier. Magnetic Resonance Imaging. 2016;34:1366–1372. doi: 10.1016/j.mri.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 24.Sanyal S, Marckmann P, Scherer S, Abraham JL. Multiorgan gadolinium (Gd) deposition and fibrosis in a patient with nephrogenic systemic fibrosis - An autopsy-based review. Nephrology Dialysis Transplantation. 2011;26:3616–3626. doi: 10.1093/ndt/gfr085. [DOI] [PubMed] [Google Scholar]
- 25.Sherry AD, Caravan P, Lenkinski RE. Primer on gadolinium chemistry. Journal of Magnetic Resonance Imaging. 2009;30:1240–1248. doi: 10.1002/jmri.21966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, et al. A Kinetic Investigation of the Lanthanide DOTA Chelates. Stability and Rates of Formation and of Dissociation of a Macrocyclic Gadolinium(III) Polyaza Polycarboxylic MRI Contrast Agent. Inorganic Chemistry. 1992;31:1095–1099. doi: 10.1021/ic00032a034. [DOI] [Google Scholar]
- 27.Deblonde GJ-P, Sturzbecher-Hoehne M, Mason AB, Abergel RJ. Receptor recognition of transferrin bound to lanthanides and actinides: a discriminating step in cellular acquisition of f-block metals. Metallomics. 2013;5:619. doi: 10.1039/c3mt20237b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sillanpaa, M. Environmental Fate of EDTA and DTPA. 85–111 (Springer, New York, NY, 1997). [DOI] [PubMed]
- 29.Abergel RJ, D’Aleo A, Ng Pak Leung C, Shuh DK, Raymond KN. Using the Antenna Effect as a Spectroscopic Tool: Photophysics and Solution Thermodynamics of the Model Luminescent Hydroxypyridonate Complex [Eu III (3,4,3-LI(1,2-HOPO))] Inorganic Chemistry. 2009;48:10868–10870. doi: 10.1021/ic9013703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abergel, R. & Deblonde, G. Formulations and treatments employing hydroxypyridonate actinide/lanthanide decorporation agents (2017).
- 31.Choi TA, et al. Biodistribution of the Multidentate Hydroxypyridinonate Ligand [14 C]-3,4,3-LI(1,2-HOPO), a Potent Actinide Decorporation Agent. Drug Development Research. 2015;76:107–122. doi: 10.1002/ddr.21246. [DOI] [PubMed] [Google Scholar]
- 32.Durbin PW, Jeung N, Kullgren B, Clemons GK. Gross composition and plasma and extracellular water volumes of tissues of a reference mouse. Health physics. 1992;63:427–42. doi: 10.1097/00004032-199210000-00007. [DOI] [PubMed] [Google Scholar]
- 33.Durbin P, Kullgren B, Xu J, Raymond K. In Vivo Chelation of Am(III), Pu(IV), Np(V), and U(VI) in Mice by TREN-(Me-3,2-HOPO) Radiation Protection Dosimetry. 1994;53:305–309. doi: 10.1093/rpd/53.1-4.305. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.