Abstract
Liposarcoma of the spermatic cord is a rare disease and often mistakenly diagnosed as inguinal hernia, hydrocele, and lipoma. We report the case of a 58-year-old man who presented with persistent discomfort and swelling on the left inguinal region. He was diagnosed with left scrotum lipoma when he was 12 years old. He underwent high orchiectomy and wide resection of the inguinal tumor. Histopathological examination revealed a well-differentiated liposarcoma of the spermatic cord with negative resection margin and scrotum lipoma. To our knowledge, this is the first report of liposarcoma of the spermatic cord with scrotum lipoma in English literature.
Keywords: Liposarcoma, Spermatic cord, Lipoma
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography; AFP, α-fetoprotein; β-HCG, β-human chorionic gonadotrophin; LDH, lactate dehydrogenase
1. Introduction
Diagnosing liposarcomas of the spermatic cord preoperatively may be challenging because of their rarity and disease with similar characteristics, including inguinal hernia, lipoma, hydrocele epididymal cyst, and testicular tumor.1 We report a rare case of liposarcoma of the spermatic cord with scrotum lipoma along with a review of the literature.
2. Case presentation
On July 2017, a 58-year-old man presented with persistent discomfort and swelling on the left inguinal region, not in the scrotum, during the past 3 months. He was diagnosed with left scrotum lipoma when he was 12 years old, and the size of the lipoma had been the same when he was examined, but physical examination revealed left inguinal tenderness.
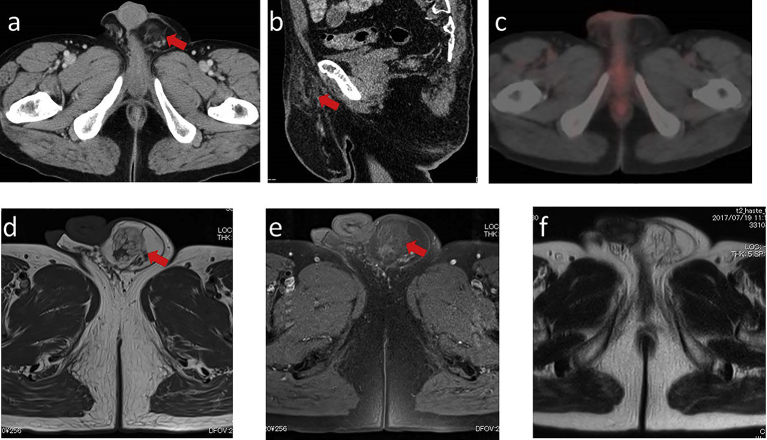
Chest and abdominal enhanced computed tomography (CT), abdominal magnetic resonance imaging (MRI), and positron emission tomography CT (PET-CT) revealed left scrotal lipoma, measuring 14 cm; left inguinal liposarcoma, measuring 5 cm; and an atrophic left testis (Fig. 1). Testicular tumor markers, such as AFP (α-fetoprotein), β-HCG (β-human chorionic gonadotrophin) and LDH (lactate dehydrogenase), were normal and there were no metastatic tumor.
Fig. 1.
Abdominal enhanced CT, MRI, and PET-CT scans. a, axial CT image. b, sagittal CT image: scrotum lipoma is not enhanced, and an uneven mass close to the left spermatic cord is weakly enhanced (arrow). c, axial PET-CT image: a soft-tissue mass on the left inguinal region had fluorodeoxyglucose accumulation (SUVmax = 1.5). d, axial MRI at T1WI. e, axial MRI at T1WI fat suppression. f, axial MRI at T2WI: Scrotum lipoma, which has a low signal only at T1WI fat suppression, and left inguinal tumor, which has a high signal at T1WI and T2WI (arrow).
We performed surgery with the diagnosis of the combination of left scrotal lipoma and left inguinal liposarcoma. High orchiectomy and radical en bloc resection of the tumor were performed through inguinal incision. Intraoperatively, we found an inguinal capsule tumor reaching the outer inguinal ring, so the tumor can be macroscopically resected completely. The specimen weighed 250 g, and he was discharged on the third postoperative day. The macroscopic cut surface of the specimen revealed a white firm mass, sized 6 cm × 5 cm, adjoining the spermatic cord, and a yellow soft large tissue, sized 14 cm × 6 cm (Fig. 2). Histopathological examination revealed a well-differentiated liposarcoma close to the spermatic cord with negative resection margin, scrotum lipoma, and normal testis (Fig. 3). No adjuvant treatment was done, and CT and MRI scans at 6 months after operation found no signs of recurrence and metastasis.
Fig. 2.
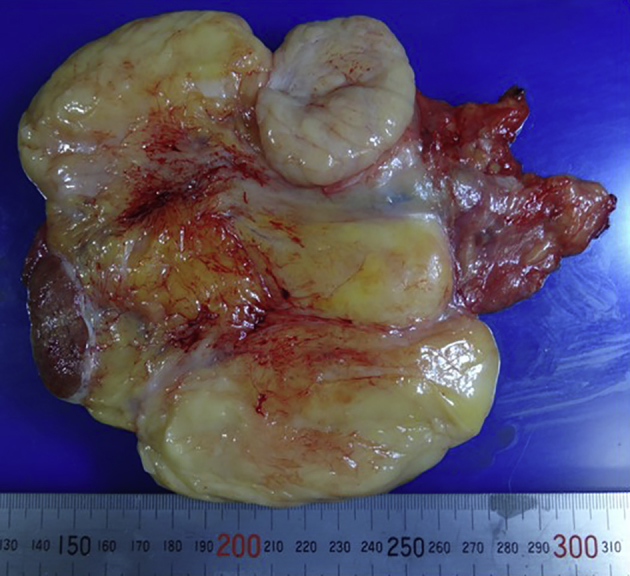
Macroscopic findings of the left inguinal and scrotum tumor resection.
Fig. 3.
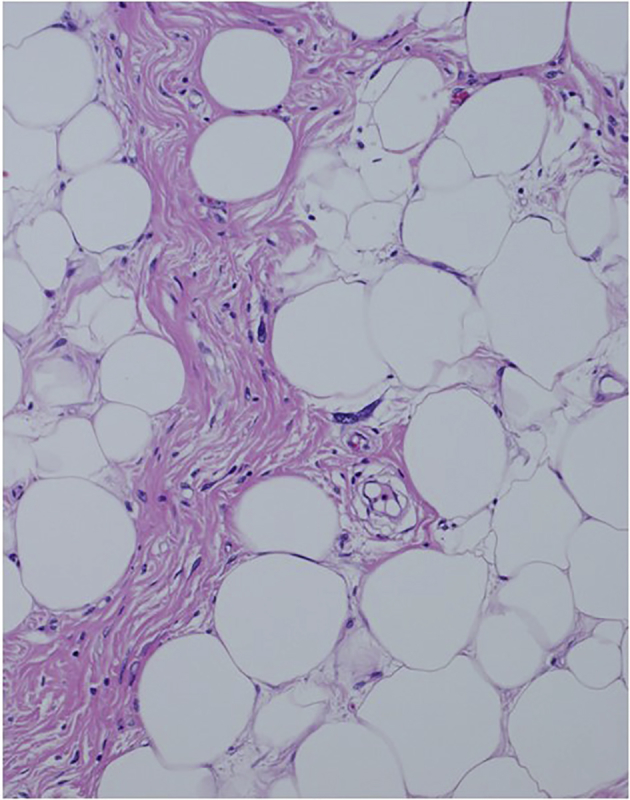
Histological findings of the spermatic cord tumor. The specimen reveals mature adipocytes and well-differentiated liposarcoma with negative margins.
3. Discussion
There are no protocols for liposarcoma of the spermatic cord due to its rarity. The common histological types of the spermatic cord tumor are liposarcoma (46%), leiomyosarcoma (20%), histiocytoma (13%), and rhabdomyosarcoma (9%).2 The median age of diagnosis for spermatic cord tumor except for rhabdomyosarcomas was 64.7 years.2 The World Health Organization classification of soft tissue tumors recognizes five categories of liposarcomas: well differentiated type, including adipocytic, sclerosing, and inflammatory subtypes; dedifferentiated type; myxoid type; pleomorphic type; and round-cell type. As in our case, a well-differentiated liposarcoma has a minimal tendency to metastasize.1 Based on our extensive search on PubMed, this is the first report of liposarcoma of the spermatic cord with scrotum lipoma, especially diagnosed more than 45 years ago. It is unlikely that lipomas differentiate into liposarcoma, and we consider that they are merely merged into the close site by chance.
Liposarcomas of the spermatic cord commonly present as painless, slowly growing tumors and are challenging to diagnose and are often mistaken as inguinal hernia, lipoma, hydrocele, epididymal cyst, or testicular tumors.1 If there are any little suspicions about the diagnosis, we should prompt imaging studies.1 CT is more useful for the diagnosis of liposarcoma than ultrasound examination.1 MRI provides good information for the precise localization of the tumor, but it cannot provide the complete type of the tumor.4 PET-CT scans are also useful in case of recurrence. In our case, since he appealed of a new discomfort and swelling on left inguinal region beside the scrotum lipoma, we performed CT, MRI, and PET-CT scans early, so it was easily diagnosed as not inguinal hernia but liposarcoma of the spermatic cord with scrotum lipoma.
Because many patients with paratesticular liposarcoma are surgically treated with presumed inguinal hernia, unusual intraoperative findings should be verified through biopsies to determine the diagnosis.3 Like other sarcoma treatments, at present, it is believed that complete resection of the tumor is the best treatment for liposarcoma of the spermatic cord. High orchiectomy and resection of the tumor and spermatic cord are standard surgeries for liposarcoma of the spermatic cord.3 Because of unclear benefits, rarity of lymph node metastasis of spermatic cord liposarcoma, and postoperative complications, lymph node dissection or adjuvant radiotherapy of the inguinal area in addition to high orchiectomy should not be performed in general.3 However, a previous study reported that adjuvant radiotherapy for liposarcoma of the spermatic cord is recommended only for high-grade tumors, lymphatic invasion, inadequate margins, or relapses.4 Another study reported that postoperative intensity-modulated radiotherapy for spermatic cord sarcoma is safe and efficient in local cancer control.5 However, this report has only five cases, and leiomyosarcoma is also included in addition to liposarcoma, so it is unlikely to be decisive.
Tumor grade, distant disease, positive lymph nodes, and leiomyosarcoma or histiocytoma cell histology are independent predictors of prognosis of the spermatic cord tumors.2 In the literature, the local recurrence rate of liposarcoma of the spermatic cord after radical resection is reported to be 17%.1 Since liposarcoma often recurs in the late period, it is important to exclude completely the tumor with no positive surgical margins and conduct long-term imaging examinations.
4. Conclusion
Liposarcoma of the spermatic cord is a rare disease especially with long-term scrotum lipoma. The diagnosis is difficult but important. Imaging examinations should be necessary, if there is any possibility of malignancy. Radical surgery of high orchiectomy with wide resection of the tumor is necessary for long-term disease free survival.
Conflicts of interest
None.
Consent for publication
Informed consent was obtained from the patient for this publication.
Acknowledgments
We thank the patient for allowing us to publish this case report. We would like to thank Editage (https://www.editage.jp/) for the English language review. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Chalouhy C., Ruck J.M., Moukarzel M. Current management of the spermatic cord: a case report and review of the literature. Mol Clin Oncol. 2017;6:438–440. doi: 10.3892/mco.2017.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez D., Barrisford G.W., Sanchez A. Primary spermatic cord tumors: disease characteristics, prognostic factors, and treatment outcomes. Urol Oncol. 2014;32:e19–25. doi: 10.1016/j.urolonc.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Bachmann R., Rolinger J., Girotti P. Liposarcoma of the spermatic cord: impact of final surgical intervention-An institutional experience. Int J Surg Oncol. 2016;2016 doi: 10.1155/2016/4785394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gregorio M.D., D'Hondt L., Nollevaux M.C. Liposarcoma of the spermatic cord: an infrequent pathology. Case Rep Oncol. 2017;10:136–142. doi: 10.1159/000455900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cerda T., Martin E., Truc G. Safety and efficacy of intensity-modulated radiotherapy in the management of spermatic cord sarcoma. Cancer Radiother. 2017;21:16–20. doi: 10.1016/j.canrad.2016.07.102. [DOI] [PubMed] [Google Scholar]