ABSTRACT
Introduction:
The Royal Victoria Hospital, Belfast provides the regional neuroendovascular service for Northern Ireland and was an enrolling centre for the ESCAPE endovascular stroke trial. Our aim was to assess outcomes for patients presenting with acute stroke following discontinuation of trial enrolment at our centre.
Methods
We collected data on all patients presenting with acute stoke between Nov-1st-2014 and Oct-31st-2015 who received endovascular treatment or received IV thrombolysis (IV-tPA) alone. ESCAPE eligibility of each patient was assessed. Primary outcome was modified Rankin Score (mRS) at 3 months.
Results
129 patients presented with acute stoke symptoms during the time period; 56/129 (43.4%) patients in the intervention group and 73/129 (56.5%) patients in the control group. In the interventional group, 42/56 (75%) were considered ESCAPE eligible and 14/56 (25%) were considered ESCAPE ineligible. 30/42 (71.4%) ESCAPE eligible patients had a positive functional outcome at 3 months compared to 9/14 (64.2%) ESCAPE ineligible patients. In the control group, 37 (50.7%) had identifiable thrombotic occlusion and 13/37 (35.1%) were considered eligible for intervention. 4/13 (30.8%) achieved functional independence (mRS<3) at 3 months.
There was a statistically significant difference in functional independence in those who underwent endovascular therapy compared to the control group (p= 0.04).
Conclusion
ESCAPE eligible patients in our centre had favourable outcome rates superior to the published trial data. ESCAPE ineligible patients tended to do slightly less well, but still better than the favourable outcome rates achieved with IVtPA alone. There is potentially a wide discordance between the threshold for futility and trial eligibility criteria when considering endovascular treatment for acute ischaemic stroke.
INTRODUCTION
Endovascular therapy for acute ischemic stroke is now accepted as the standard of care for selected patients with anterior circulation occlusion following publication of five positive randomized trials; MR CLEAN, ESCAPE, EXTEND-IA, SWIFT-PRIME and REVASCAT.1-6 The Royal Victoria Hospital, Belfast, UK was one of 22 international centres to enrol patients into the Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) trial.3 Enrollment into the ESCAPE trial was stopped in October 2014 following unplanned interim analysis triggered by release of the MR CLEAN trial results which showed superior efficacy of endovascular therapy. The safety monitoring board advised stopping the study as the prespecified boundary for efficacy had been crossed.3
It is estimated that 5-10% of patients with ischaemic stroke may benefit from endovascular therapy.7 The RVH serves a population of approximately 400000 people and treats an estimated 120-150 acute strokes per year with IV-tPA and/or thrombectomy. At our centre, routine imaging work-up when endovascular therapy is available includes unenhanced CT brain, CT angiogram from the aortic arch and CT perfusion. Patients who are transferred from other units for endovascular therapy will have been initially triaged by the stroke team and interventional neuroradiologist following imaging review via the regional NIPACS (Northern Ireland Picture Archiving and Communication System) service. Imaging will then be repeated upon arrival (CT brain and CT angiogram) to assess continued eligibility for thrombectomy. We prospectively evaluate the ASPECTS score in all patients, which is a 10-point scoring system to determine the extent of early ischaemic changes in the middle cerebral artery territory.8 A maximum of 10 reflects normal and 1 point is deducted for every abnormal region. ASPECTS ≤ 5 is considered to be the threshold for futility. Clot location and perfusion mismatch is also documented. We regard the ESCAPE trial eligibility criteria as a guide, but not prescriptive when considering endovascular therapy and it does not define our boundary for endovascular treatment.3 For patients receiving endovascular therapy we prospectively document procedural times and recanalization success. Baseline and discharge NIHSS is also recorded routinely in all admitted stroke patients. Our stroke research nurse evaluates 3-month mRS via clinic appointment or telephone assessment.
The purpose of this study was threefold; first to ensure that patients meeting eligibility criteria for the ESCAPE trial continued to have outcomes comparable with the published data. Second, to evaluate outcomes in patients receiving endovascular treatment who would not have been eligible for ESCAPE as per the trial inclusion criteria. Lastly; to evaluate the outcomes in all patients who underwent medical treatment for acute ischemic strokes. Considering the service for endovascular treatment remains time limited, we were particularly interested in the outcomes of patients who were potentially eligible for endovascular treatment according to the ESCAPE trial eligibility criteria but received thrombolysis only.
MATERIALS AND METHODS
This retrospective case-control study was conducted on clinical records of all patients admitted to the Royal Victoria Hospital, Belfast from 1st November 2014 to 31st October 2015 who were treated for acute ischaemic stroke (n=129). The clinical records of 56 patients who underwent endovascular treatment with or without IV-tPA were “intervention cases”. The remaining clinical records of 73 patients who received IV-tPA only served as “controls” for the study. Within each of the intervention and control groups patients were stratified by those considered ESCAPE eligible and those considered ESCAPE ineligible. The major ESCAPE trial eligibility criteria are presented in Table 1. For all patients treated via endovascular therapy we collected demographics including baseline NIHSS, baseline mRS, ASPECTS on initial unenhanced CT, clot location, administration of IV-tPA, CT to groin puncture time, groin puncture to recanalization time, TICI score, procedural complications, discharge NIHSS and 3-month mRS.
Table 1.
ESCAPE trial eligibility
| Criteria | Description |
|---|---|
| 1. | NIHSS score >5 |
| 2. | <12 hours onset of symptoms |
| 3. | Adult (>18 years). No age limit |
| 4. | Good pre-morbid status (baseline mRS ≤2) |
| 5. | CT brain: ASPECTS Score >5 |
| 6. | CT angiogram showed occluded proximal artery in the anterior circulation. |
| 7. | CT angiogram showed good collateral circulation |
For patients treated via IV-tPA alone we collected demographics including baseline mRS, ASPECTS on initial unenhanced CT, clot location, discharge NIHSS and 3-month mRS. Patients were grouped into those considered ESCAPE eligible and those considered ESCAPE ineligible if an occluding thrombus was identified. Patients without an identifiable thrombus were evaluated separately
As this was a service evaluation study informed consent was not obtained.
Outcome measures. The functional outcome in each patient at 3 months after treatment was evaluated by the mRS score.
Statistical analysis. Descriptive statistics were computed and compared between the intervention and control groups. A chi squared test was applied to determine whether there was any statistical significance in functional outcomes between the control and intervention groups, between ESCAPE eligible and ineligible in the intervention group and between ESCAPE eligible patients in the control and intervention groups. The following assumptions were made for the analysis; a positive outcome1 resulting in functional independence was defined as an mRS of <3 at 3 months and a negative outcome2 defined as an mRS of ≥3 at 3 months. We hypothesise that for the intention to treat population (ITT), endovascular treatment has more positive outcomes than medical therapy alone. We also hypothesise that for the endovascular treatment population (ETP), ESCAPE eligible patients would also have more positive outcomes than non-eligible patients. Statistical significance was set at the p = 0.05 level.
RESULTS
Demographic and clinical characteristics for both the ITT and ETP are reported in Figure 1 and Tables 2 & 3. Overall 129 patient clinical records were identified that met the inclusion criteria of the study. There were 56 intervention and 73 control cases. Patients who had intervention and no intervention appear to be relatively homogeneous with regards to age, sex, baseline NHISS Score and basline ASPECTS on CT. All subjects in the control group were treated with IV alteplase.
Fig 1.
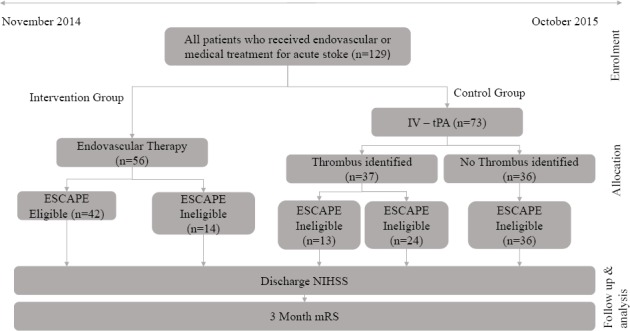
Disposition of subjects
Table 2.
Baseline Characteristics and Process Measures
| Variable | Intervention (n=56) | Control (n=73) |
|---|---|---|
| Demographics | ||
| Age -yr | ||
| Median | 71 | 72 |
| IQR | 61-78 | 67-84 |
| Female – no. (%) | 28 (50%) | 37 (50.7%) |
| Clinical characteristics | ||
| NIHSS Score* | ||
| Median | 16 | 11 |
| IQR | 11-20 | 6-18 |
| Treatment with IV alteplase no. (%) | 27 (48.2%) | 73 (100%) |
| Imaging Characteristics | ||
| ASPECTS on CT | 9(7-10) | 10(8-10) |
Scores on National Institutes of Health Stroke Scale (NIHSS) range from 0 to 42, with higher scores indicating more severe neurologic deficits
Table 3.
Baseline Characteristics and Process Measures within Intervention Group
| Variable | ESCAPE eligible (n=42) | ESCAPE ineligible (N=14) |
|---|---|---|
| Demographics | ||
| Age -yr | ||
| Median | 71 | 67 |
| IQR | 62-78 | 40-77 |
| Female sex – no. (%) | 24 (57.1%) | 4 (28.6%) |
| Clinical characteristics | ||
| NIHSS Score* | ||
| Median | 16 | 14 |
| IQR | (11-20) | (5-18) |
| Treatment with IV alteplase no. (%) | 21 (50%) | 6 (43%) |
| Imaging Characteristics | ||
| ASPECTS on CT | 8 (7-9) | 10 (8-10) |
Scores on National Institutes of Health Stroke Scale (NIHSS) range from 0 to 42, with higher scores indicating more severe neurologic deficits
Intervention group. Of the 56 cases treated via endovascular therapy, 42 (75%) were considered eligible for intervention using the ESCAPE trial eligibility criteria and 14 patients (25%) were considered ineligible. These patients appear to be homogenous with regards to age, NHISS Score, treatment with IV alteplase and ASPECTS on CT. There were more females in the eligible group 24 (57.1%) compared to the ineligible group 4 (28.6%). The reasons for ineligibility included 6 (43%) patients with basilar artery occlusion and 8 (57%) patients with solitary M2 level occlusions. Twenty-one (37.5%) cases underwent endovascular therapy following transfer from another stroke centre in Northern Ireland. Median time from CT to groin puncture was 26 minutes (IQR: 21-32) and median groin puncture to recanalization was 35 minutes (IQR: 25-65) in the ESCAPE eligible group. For the ESCAPE ineligible group, median time from CT to groin puncture was 18 minutes (IQR: 15-34) and for groin puncture to recanalization was 43 minutes (IQR: 24-85). Recanalization success as defined by TICI 2b/3 was 33/42 (78.5%) in the ESCAPE eligible group and 12/14 (85.6%) in the ESCAPE ineligible group. Median discharge NIHSS score was 9 (IQR:2-15) in the ESCAPE eligible group and 9 in the ESCAPE ineligible group (IQR: 3-15). Functional independence as defined as mRS 0-2 was 30 (71.4%) in the ESCAPE eligible group and 9 (64.2%) in the ESCAPE ineligible group. The following post procedural complications occurred; 3 (5.4%) patients developed intracranial haemorrhage and 1 patient developed a common femoral artery pseudoaneurysm.
Control group. 73 cases were treated with IV-tPA, 37 (50.7%) had identifiable thrombotic occlusion (via CT angiography or the presence of a hyperdense vessel on unenhanced CT). Of these 23 (62%) patients had proximal anterior circulation occlusion (ICA/M1), 11 (30%) had M2/A2 occlusion and 3 (8%) had posterior circulation occlusion. 13/23 proximal anterior circulation occlusion cases would have be considered eligible for endovascular intervention based on the ESCAPE eligibility criteria. 12 (92.3%) of these patients who were considered ESCAPE eligible presented out of hours when the clot retrieval service was not available. Overall, median door to needle time was 48 minutes (IQR: 33-65) among IV tPA patients. Median discharge NIHSS score for ESCAPE eligible patients treated with IV tPA was 19 (IQR: 14-22). For ESCAPE ineligible patients with thrombotic occlusion median discharge NIHSS was 8 (IQR: 3-15) and for patients without thrombotic occlusion median discharge NIHSS was 3 (IQR:0-5). In patients with thrombotic occlusion, functional independence as defined by mRS 0-2 at 3 months was 4 (30.8%) among ESCAPE eligible patients compared to 9 (37.5%) among ESCAPE ineligible patients. Table 4 summarises the outcomes of the intervention and control groups.
Table 4.
Clinical Characteristics in Intervention and Control Groups
| Endovascular Therapy n=56 | IV-tPA Thrombus Identified N=37 | IV-tPA No Thrombus Identified | |||
|---|---|---|---|---|---|
| Clinical characteristics | ESCAPE Eligible (N=42) | ESCAPE Ineligible (N=14) | ESCAPE Eligible (N=13) | ESCAPE Ineligible (N=24) | ESCAPE Ineligible (N=36) |
| 3 Month mRS 0-2 – n (%) | 30(71.4%) | 9(64.2%) | 4(30.8%) | 9(37.5%) | 25(69.4%) |
| Discharge NIHSS Score* - Median (IQR) | 9 (2-15) | 9 (3-15) | 19 (14-22) | 8 (3-15) | 3 (0-5) |
Scores on National Institutes of Health Stroke Scale (NIHSS) range from 0 to 42, with higher scores indicating more severe neurologic deficits
n: Number of patients with outcome. N: Total number of patients within group.
Analysis. The chi squared analysis showed a statistically significant difference in functional independence (mRS<3) in those who underwent endovascular therapy compared to the control group, χ2 (1, n=129) = 4.0742 p= 0.04. Eligibility criteria was also considered as a factor that could influence functional outcomes within the intervention group but was not statistical significant. An additional analysis showed a statistically significant difference in functional outcomes in patients who were ESCAPE eligible and underwent intervention and those who were ESCAPE eligible and received IV-tPA only, χ2 (1, n=55) = 6.9531 p = 0.008.
DISCUSSION
Our study showed that patients with acute ischemic stroke and proximal anterior circulation occlusion with a small core infarct who were treated with endovascular therapy had improved functional outcomes at 3 months compared to those treated with IV-tPA only (p=0.04). Good outcome rates were superior to ESCAPE results (71.4% versus 53.0%) and support the benefit of endovascular therapy in the treatment of acute stroke.3 Our higher good outcome rates may be accounted for via our faster documented procedural times (median CT to recanalization of 68 minutes versus 84 minutes) and slightly better documented recanalization rates (TICI 2b/3 78.5% versus 72.4%) An example of successful recanalisation is shown in Figure 2. The rate of post procedural haemorrhage was slightly higher in our centre compared to the trial (5.1% versus 4.2%).
Fig 2.
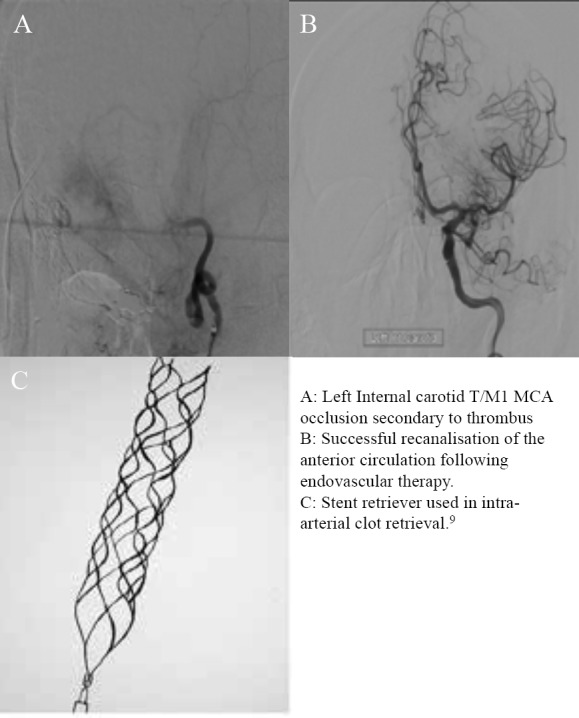
An example of successful recanalisation
Despite high level evidence supporting endovascular therapy in acute stroke, there is heterogeneity among the intention to treat population.2-6 For example, two trials enforced age limits on potentially eligible patients (SWIFT PRIME and EXTEND IA) and the onset of treatment of endovascular therapy varied among studies (within 6, 8 or 12 hours).4,5 Baseline imaging to evaluate vessel occlusion and salvageable brain tissue, presenting ASPECTS, baseline NIHSS score, and contraindications to thrombectomy varied between trials. Consensus regarding the inclusion of solitary M2 occlusions also differed. Although MR CLEAN and REVASCAT included solitary M2 occlusions, the overall numbers were small and a recent meta-analysis of the five trials published in the Lancet did not demonstrate significant benefit for intervention for these distal occlusions.2,6,10 Firm evidence for thrombectomy in this location may remain elusive given the difficulty in distinguishing (and inconsistency in classification) between the M1 and M2 segments and the greater anatomical variability with the M2 segment.11 The limits for intervening in basilar artery occlusion may also be difficult to define, given the otherwise high rate of death and dependence among survivors with conservative management.12
In our centre, the ESCAPE eligibility criteria do not strictly define our boundary for treatment, with approximately one quarter (14/56, 25%) of our endovascular cases being outside eligibility criteria. The overall outcome at 3 months for these patients was slightly worse compared to the ESCAPE eligible group (64.2% compared to 71.4%). However, these results were not statistically significant (p=0.61) accepting the null hypothesis that there is no difference in functional outcomes when selecting patients for endovascular treatment using the ESCAPE eligible criteria. Although patients deemed ESCAPE ineligible represent a very heterogeneous patient group, as the interventional cases in this study had solitary M2 (8/14) or basilar artery clots (6/14).
As this is a relatively new and evolving service, our endovascular stroke service continues to be time limited to ‘office hours’ with only ad hoc out of hours availability. In our study, there was a statistically significant difference in functional outcomes in ESCAPE eligible patients within the intervention group compared to ESCAPE eligible patients within the control group who presented outside office hours (p=0.008). These patients treated solely via IV-tPA but deemed ESCAPE eligible had very similar 3-month outcomes to the control group (30.8% versus 29.3%). There is a clear imperative to deliver an effective and accessible 24/7 thrombectomy service. Indeed, given the effective outcomes with thrombectomy it is not surprising that this treatment is cost effective within the NHS.14 It should also be noted that 21/56 (37.5%) patients treated with thrombectomy were transferred in from other units which cover 78% of the Northern Ireland population (NI population – Belfast Trust population/NI Population x 10). Equity of access to this service must also be addressed.
There are limitations to this study. The overall numbers are small, data presented has not been independently verified and assessment of 3-month mRS was not carried out by a blinded assessor. It will be useful to collect additional data to assess outcomes between those presenting directly to the RVH compared to those who are transferred from other units. 32.4% (35/108) of actively treated acute ischaemic strokes within the Royal Victoria Hospital received thrombectomy during this period. It would be useful to compare with other units that rely on transferring patients to access the endovascular service for the purposes of future planning.
Further research addressing thrombectomy in basilar clots and single M2 occlusions is needed. Research to compare intravenous lysis plus endovascular treatment versus endovascular thrombectomy alone is also limited.
CONCLUSIONS
The primary purpose of this study was to demonstrate outcomes in our centre following discontinuation of patient enrolment into the ESCAPE trial. In real world practice, outside of trial participation, our centre has demonstrated outcomes better than the published data from ESCAPE. Patients treated via endovascular therapy but considered ESCAPE ineligible also had overall outcomes better than those treated via IV-tPA alone. However, given the extent of heterogeneity in this group, defining the absolute boundary of futility will likely prove difficult and in practice the decision to intervene will remain a judgment call.
Footnotes
Provenance: externally peer-reviewed
ABBREVIATIONS
| IV-tPA | Intravenous tissue plasminogen activator | MCA | Middle cerebral artery |
| ASPECTS | Alberta Stroke Program Early CT Score | mRS | modified Rankin Scale |
| NIHSS | National Institutes of Health Stroke Scale | IQR | Interquartile range |
| ICA | Internal carotid artery | TICI | Thrombolysis in cerebral infarction |
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 guidelines for early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46(10):3020-35. [DOI] [PubMed] [Google Scholar]
- 2.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372(1):11-20. [DOI] [PubMed] [Google Scholar]
- 3.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thorneton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372(11):1019-30. [DOI] [PubMed] [Google Scholar]
- 4.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372(1):1009-18. [DOI] [PubMed] [Google Scholar]
- 5.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372(24):2285-95. [DOI] [PubMed] [Google Scholar]
- 6.Jovin TG, Chamorro A, Cobo E, de Miguel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372(24):2296-306. [DOI] [PubMed] [Google Scholar]
- 7.Ganesalingam J, Pizzo E, Morris S, Sunderland T, Ames D, Lobotesis K. Cost-utility analysis of mechanical thrombectomy using stent retrievers in acute ischemic stroke. Stroke. 2015; 46(9):2591–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000; 355(9216):1670-4. [DOI] [PubMed] [Google Scholar]
- 9.Sussman E, Kellner C, McDowell M, Yang P, Nelson E, Greenberg S, et al. Endovascular thrombectomy following acute ischemic stroke: a single-center case series and critical review of the literature. Brain Sci. 2013; 3(2): 521-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomized trials. Lancet. 2016;387(10029):1723-31. [DOI] [PubMed] [Google Scholar]
- 11.Rai AT, Hogg JP, Cline B, Hobbs G. Cerebrovascular geometry in the anterior circulation: an analysis of diameter, length and the vessel taper. J Neurointerv Surg. 2013; 5(4):371-5. [DOI] [PubMed] [Google Scholar]
- 12.Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005; 76(9):1238-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furlan AJ. Endovascular therapy for stroke. It’s about time. New Eng J Med. 2015; 372(24):2347-9. [DOI] [PubMed] [Google Scholar]


