Abstract
Background
No longitudinal study compared associations of echocardiographic indexes of diastolic left ventricular function studies with conventional (CBP) and daytime ambulatory (ABP) blood pressure in the general population.
Methods and Results
In 780 Flemish (mean age, 50.2 years; 51.7% women), we measured left atrial volume index (LAVI), peak velocities of the transmitral blood flow (E) and mitral annular movement (e′) in early diastole and E/e′ 9.6 years (median) after CBP and ABP. In adjusted models including CBP and ABP, we expressed associations per 10/5‐mm Hg systolic/diastolic blood pressure increments. LAVI and E/e′ were 0.65/0.40 mL/m2 and 0.17/0.09 greater with higher systolic/diastolic ABP (P≤0.028), but not with higher baseline CBP (P≥0.086). e′ was lower (P≤0.032) with higher diastolic CBP (−0.09 cm/s) and ABP (−0.19 cm/s). When we substituted baseline CBP by CBP recorded concurrently with echocardiography, LAVI and E/e′ remained 0.45/0.38 mL/m2 and 0.15/0.08 greater with baseline ABP (P≤0.036), while LAVI (+0.53 mL/m2) and E/e′ (+0.19) were also greater (P<0.001) in relation to concurrent systolic CBP. In categorized analyses of baseline data, sustained hypertension or masked hypertension compared with normotension or white‐coat hypertension was associated with greater LAVI (24.0 versus 22.6 mL/m2) and E/e′ (7.35 versus 6.91) and lower e′ (10.7 versus 11.6 cm/s; P≤0.006 for all) with no differences (P≥0.092) between normotension and white‐coat hypertension or between masked hypertension and sustained hypertension.
Conclusions
ABP is a long‐term predictor of diastolic left ventricular function, statistically outperforming distant but not concurrent CBP. Masked hypertension and sustained hypertension carry equal risk for deterioration of diastolic left ventricular function.
Keywords: blood pressure, blood pressure measurement/monitoring, hypertension, left ventricular diastolic dysfunction, population science
Subject Categories: Congenital Heart Disease, Hypertension, Echocardiography
Clinical Perspective
What Is New?
Data obtained in a general population are less prone to bias than studies performed in hypertensive populations.
Our literature search did not identify any longitudinal study comparing associations of multiple indexes of diastolic left ventricular function with conventional versus daytime ambulatory blood pressure and linking blood pressure categories at baseline with diastolic left ventricular function at follow‐up.
What Are the Clinical Implications?
The take‐home message of our current study is that multiple measurements of blood pressure outside the medical environment are superior to fewer measurements by observers to screen for diastolic left ventricular dysfunction and that ambulatory monitoring, as already proposed more than a decade ago by Thomas Pickering and as reiterated in contemporary guidelines, is the state‐of‐the‐art technique for assessing blood pressure in clinical practice and research.
In view of the epidemiological transition, heart failure (HF) is a major public health problem.1 Diastolic HF, also referred to as HF with preserved ejection fraction, accounts for 50% of cases.2 Mortality of diastolic HF is 30% within 1 year of the first hospital admission.3 Subclinical diastolic left ventricular (LV) dysfunction has a prevalence of 25% in the general population,4, 5 predisposes to further deterioration of LV function,6 and finally evolves to overt HF.2 Raised blood pressure is the major risk factor associated cross‐sectionally4, 5, 7 and prospectively6, 8, 9, 10 with diastolic LV dysfunction in the general population. Most studies making this point relied on conventional office blood pressure. However, all current hypertension guidelines11, 12, 13, 14 endorse the use of ambulatory monitoring as the state‐of‐the‐art method for monitoring blood pressure, because the greater number of readings obtained over the whole day outside the medical environment enhance risk stratification.
The single prospective population study of diastolic LV dysfunction10 that applied ambulatory monitoring covered a narrow age range (40–59 years), only reported on the echocardiographically assessed LV filling pressure, did not compare the predictive value of ambulatory versus office blood pressure, and did not report on diastolic LV function in truly normotensive people versus patients with white‐coat, masked, or sustained hypertension. To address these knowledge gaps, we analyzed the database of the FLEMENGHO (Flemish Study on Environment, Genes and Health Outcomes).4, 6, 15 We assessed to what extent office compared with ambulatory blood pressure predicted over a 10‐year span multiple echocardiographic indexes capturing diastolic LV function, first in all people combined, and next in participants categorized according to the guideline‐endorsed operational thresholds of their baseline office and ambulatory blood pressure.
Methods
Study Population
FLEMENGHO complies with the Helsinki declaration for research in human subjects.16 The Ethics Committee of the University of Leuven approved the study. At each contact, participants renewed informed written consent. The data, analytic methods, and study materials will not be made available to other researchers for purposes of reproducing the results or replicating the procedure, because informed consent did not cover this option. Recruitment started in 1985 and continued until 2004.4, 6, 15 The initial participation rate was 78.0%. Of 3343 participants enrolled from 1985 until 2004, 2904 had their daytime ambulatory blood pressure measured (1989–2008) and afterwards 828 underwent echocardiography (2005–2010). The participation rate for ambulatory blood pressure monitoring and echocardiography amounted to 94.7% and 76.0%, respectively. In the context of this article, baseline and follow‐up, respectively, refer to the timing of blood pressure monitoring and echocardiography (Figure 1).
Figure 1.
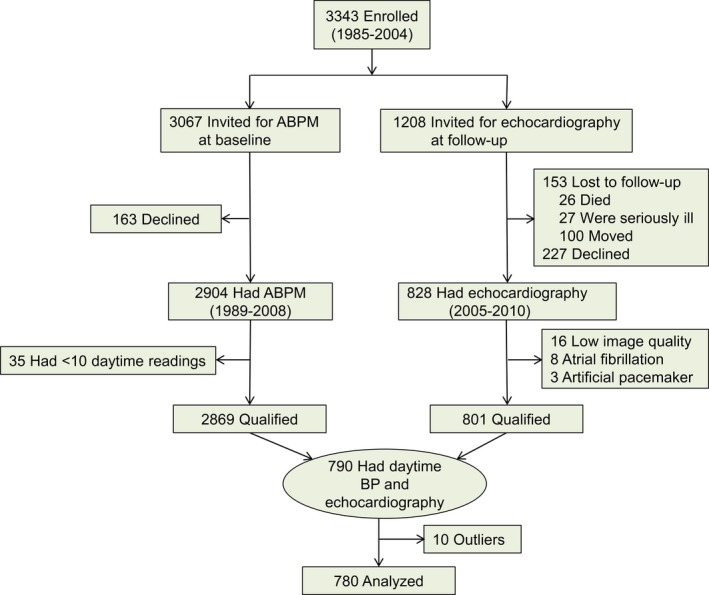
Flowchart summarizing inclusion of participants in the study. ABPM refers to ambulatory blood pressure (BP) measurement.
We excluded participants from analysis if the daytime ambulatory blood pressure was the mean of <10 readings (n=35), if diastolic LV function could not be reliably graded, because of image quality (n=16), atrial fibrillation (n=8), or paced heart rhythm (n=3). This left 790 participants with both conventional and ambulatory blood pressure measured and with gradable echocardiographic images. Finally, we excluded 10 participants because their blood pressure levels were >3 SDs higher than the population mean. Thus, the number of participants statistically analyzed totaled 780.
Clinical Measurements
Nurses measured blood pressure at baseline17 and follow‐up by auscultation of the Korotkoff sounds. After the participants had rested for 5 minutes in the sitting position, the observers obtained 5 consecutive blood pressure readings (phase V diastolic pressure) to the nearest 2 mm Hg, using mercury sphygmomanometers. Standard cuffs had a 12×24‐cm inflatable portion, but if upper arm girth exceeded 31 cm, larger cuffs with 15×35‐cm bladders were used. For analysis, the 5 blood pressure readings obtained at baseline or at follow‐up were averaged. From baseline to follow‐up, we implemented a stringent quality control program described elsewhere.18, 19 Hypertension on conventional blood pressure measurement was a blood pressure ≥140 mm Hg systolic or 90 mm Hg diastolic.
At baseline, participants wore validated20 SpaceLabs 90204 or 90207 portable monitors (Spacelabs Healthcare, Snoqualmie, WA) to record their daytime ambulatory blood pressure from 8 am until 10 pm at 20‐minute intervals. As an alternative, they could also opt having their blood pressure monitored over 24 hours, but for the current study only the daytime part of these recordings was analyzed. The recordings were sparsely edited, removing only readings labeled with an error code or with lower systolic than diastolic blood pressure level. For continuous analyses,21 we computed the daytime blood pressure as the within‐individual mean of the readings between 10 am and 8 pm weighted for the interval between readings. This short definition of daytime eliminates the transition periods in the morning and evening during which blood pressure changes rapidly in most people and approximates within 1 to 2 mm Hg to the wakeful blood pressure recorded by the diary method.22 In categorical analyses, ambulatory hypertension was a daytime blood pressure of 135 mm Hg systolic or 85 mm Hg diastolic or higher.13 Normotension and sustained hypertension were a consistently normal or elevated blood pressure on conventional and ambulatory measurement. White‐coat hypertension was a raised conventional blood pressure in the presence of a normal daytime blood pressure. Masked hypertension was an elevated ambulatory blood pressure with normal conventional blood pressure. Participants were categorized based on blood pressure levels only, irrespective of treatment with antihypertensive drugs.23
Echocardiography
The acquisition and off‐line analysis of the echocardiographic images were done according to current guidelines.24, 25 Previous publications describe the procedures applied for acquisition and the off‐line analysis of the echocardiographic measurements in detail.4, 6 In short, digitally stored echocardiographic images, obtained with a Vivid7 Pro (GE Vingmed, Horten, Norway) interfaced with a 2.5‐ to 3.5‐MHz phased‐array probe, were averaged over 3 heart cycles. End‐diastolic LV dimensions were used to calculate LV mass by an anatomically validated formula according to the recommendations of the American Society of Echocardiography.24, 25 Left atrial (LA) volume was calculated using the prolate‐elipsoid method. Diastolic LV function was assessed by EchoPac software, version 4.0.4 (GE Vingmed). We determined early (E) and late (A) diastolic peak velocities of the transmitral blood flow from the pulsed Doppler signal and early (e′) and late (a′) peak velocities of the mitral annular movement by tissue Doppler imaging. The tissue Doppler imaging measurements were averaged over 4 acquisition sites (septal, lateral, inferior, and posterior). The intraobserver reproducibility of the single observer in the study (T.K.), defined as the 2‐SD interval about the mean of the relative differences between duplicate readings, across the 4 tissue Doppler imaging sampling sites, ranged from 4.5% to 5.3% for e′ and from 4.0% to 4.5% for a′.6
Other Measurements
The study nurses counted heart rate for 1 minute and measured the participants’ anthropometric characteristics. Body mass index was weight in kilograms divided by height in meters squared. They also administered a standardized questionnaire inquiring into each participant's medical history, smoking and drinking habits, and intake of medications. Consumption of alcohol was a daily intake of at least 5 g of ethanol per day.26 Plasma glucose and total serum cholesterol were measured using automated methods in a single certified laboratory. Diabetes mellitus was a fasting or random glucose level exceeding 126 or 200 mg/dL (7.0 or 11.1 mmol/L), or use of antidiabetic agents.27
Statistical Analysis
For database management and statistical analysis, we used SAS software, version 9.4. We compared means and proportions between groups by ANOVA and the χ2 statistic, respectively. We applied a paired t test and McNemar test to assess changes over time in means and proportions. Statistical significance was a 2‐sided significance level of 0.05.
In exploratory analyses, we plotted the sex‐ and age‐adjusted indexes of diastolic LV function by fifths of the distributions of conventional and daytime blood pressure at baseline. As described before,4, 6 covariables in the multivariable‐adjusted analyses included sex, the baseline characteristics age, body mass index, heart rate, serum total cholesterol, plasma glucose, γ‐glutamyltransferase (index of alcohol intake)28 and smoking, use of lipid‐lowering treatment at follow‐up, 3 indicator variables coding for starting, stopping, or continuing antihypertensive drug treatment from baseline to follow‐up, and duration of follow‐up. We computed the variance inflation factor from regression models that included both conventional and daytime blood pressure.29 The final multivariable‐adjusted estimates were derived from mixed models that accounted for family clusters modeled as a random effect with the other covariables entered as fixed effects. In sensitivity analyses, we modeled diastolic LV function indexes in relation to the daytime blood pressure at baseline and the conventional blood pressure at follow‐up.
Results
Characteristics of Participants
All 780 participants were white Europeans, of whom 403 (51.7%) were women. The study population consisted of 116 singletons and 664 related subjects, belonging to 131 one‐generation families and to 61 complex pedigrees. Table 1 shows the clinical characteristics at baseline and follow‐up. In all participants (Table 1), mean baseline values were 40.2 years for age, 121.8/75.4 and 123.0/76.0 mm Hg for systolic/diastolic blood pressure on conventional and daytime ambulatory measurement, and 25.0 kg/m2 for body mass index. Median follow‐up was 9.6 years (5th–95th percentile interval, 5.5–16.1 years). From baseline to follow‐up (Table 1), the prevalence of smoking decreased from 26.5% to 21.2%, whereas the proportion of people drinking 5 g alcohol or more daily increased from 23.6% to 40.6%. Body mass index, the prevalence of overweight and obesity, conventional blood pressure, and treatment rates for hypertension and dyslipidemia increased from baseline to follow‐up. Serum total cholesterol and plasma glucose decreased over time.
Table 1.
Characteristics of 780 Participants at Baseline and Follow‐Up
| Characteristic | Baseline | Follow‐Up | P Value |
|---|---|---|---|
| Number with characteristics (%) | |||
| Current smoker | 207 (26.5) | 165 (21.2) | <0.001 |
| Drinking alcohol ≥5 g/d | 184 (23.6) | 317 (40.6) | <0.001 |
| Overweight | 296 (38.0) | 344 (44.1) | <0.001 |
| Obesity | 77 (9.9) | 137 (17.6) | <0.001 |
| Diabetes mellitus | 8 (1.0) | 29 (3.7) | <0.001 |
| Conventional hypertension | 143 (18.3) | 312 (40.0) | <0.001 |
| Daytime hypertension | 122 (15.6) | ··· | |
| On antihypertensive drugs | 61 (7.8) | 185 (23.7) | <0.001 |
| Lipid‐lowering treatment | 16 (2.0) | 112 (14.4) | <0.001 |
| Mean of characteristic (±SD) | |||
| Age, y | 40.2±14.4 | 50.6±15.4 | <0.001 |
| Body mass index, kg/m2 | 25.0±4.1 | 26.4±4.2 | <0.001 |
| Conventional blood pressure | |||
| Systolic, mm Hg | 121.8±13.8 | 128.7±17.1 | <0.001 |
| Diastolic, mm Hg | 75.4±10.2 | 79.5±9.4 | <0.001 |
| Daytime blood pressure | |||
| Systolic, mm Hg | 123.0±9.9 | ··· | |
| Diastolic, mm Hg | 76.0±7.8 | ··· | |
| Heart rate, bpm | 69.1±10.0 | 63.5±9.5 | <0.001 |
| Total cholesterol, mmol/L | 5.33±1.11 | 5.24±0.96 | 0.013 |
| Plasma glucose, mmol/L | 4.98±1.28 | 4.94±0.81 | 0.38 |
| Geometric mean (IQR) of characteristic | |||
| γ‐Glutamyltransferase (U/L) | 21.4 (12.9–31.6) | 22.9 (15.1–32.4) | <0.001 |
Body mass index was body weight in kilogram divided by height in meters squared. Overweight and obesity refer to a body mass index of 25 to 29.9 and ≥30 kg/m2, respectively. Conventional hypertension was a blood pressure of ≥140 mm Hg systolic or ≥90 mm Hg diastolic. Daytime hypertension was a blood pressure of ≥135 mm Hg systolic or ≥85 mm Hg diastolic. P values indicate the significance of the difference between baseline and follow‐up. IQR indicates interquartile range.
Associations With Blood Pressure
The median number of readings averaged to estimate the daytime ambulatory blood pressure was 32 (5th–95th percentile interval, 20–40; range, 11–43). Mean values (±SD) of the echocardiographic measurements at follow‐up were the following: 22.8±6.30 mL/m2 and 91.3±21.4 g/m2 for the LA volume and LV mass indexes; 75.4±16.0 cm/s, 64.5±16.7 cm/s, and 1.26±0.48 for transmitral E, A, and E/A; 11.5±3.6 cm/s, 10.1±2.1 cm/s, and 1.26±0.64 for the tissue Doppler imaging indexes e′, a′, and e′/a′; and 6.98±1.91 for E/e′. In exploratory analyses, only adjusted for sex and age (Figure 2), the LA volume index and E/e′ increased (P≤0.007) and e′ decreased (P=0.001) with higher daytime systolic blood pressure, whereas the corresponding associations were directionally similar for systolic blood pressure on conventional measurement (P≤0.002), but not significant for the LA volume index (P=0.12).
Figure 2.
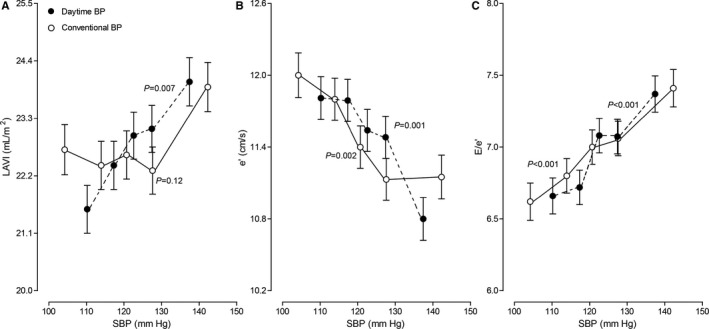
Sex‐ and age‐adjusted left atrial volume index (A), e′ (B), and E/e′ (C) at follow‐up by quintiles of the distribution of baseline systolic blood pressure on conventional (open circles) or daytime ambulatory (closed dots) blood pressure measurement. Vertical bars denote the SE. P values are for linear trend.
In multivariable‐adjusted mixed models that accounted for family clusters (Table 2), the LV mass and LA volume indexes increased with higher systolic and diastolic daytime pressure (P≤0.004), but not with higher conventional pressure (P≥0.14). The association sizes per 10/5‐mm Hg increment in systolic/diastolic daytime blood pressure were 2.20/1.26 g/m2 and 0.62/0.31 mL/m2. The e′ peak velocity decreased with higher conventional (−0.16 cm/s; P<0.001) and daytime (−0.24 cm/s; P<0.001) diastolic blood pressure. E/e′ increased with higher conventional (+0.15; P=0.001) and daytime (+0.23; P<0.001) systolic blood pressure.
Table 2.
Echocardiographic Indexes at Follow‐Up in Relation to Baseline Blood Pressure
| Model Echocardiographic Index | Systolic Blood Pressure | Diastolic Blood Pressure | ||
|---|---|---|---|---|
| Conventional | Daytime | Conventional | Daytime | |
| Single blood pressure | ||||
| LV mass index, g/m2 | 0.82 (−0.26 to 1.90) | 2.20 (0.80–3.60)† | −0.01 (−0.72 to 0.69) | 1.26 (0.39–2.13)† |
| LA volume index, mL/m2 | 0.18 (−0.14 to 0.51) | 0.62 (0.20–1.04)† | −0.06 (−0.27 to 0.16) | 0.31 (0.05–0.57)* |
| e′ peak, cm/s | −0.10 (−0.23 to 0.02) | −0.15 (−0.31 to 0.009) | −0.16 (−0.24 to −0.08)‡ | −0.24 (−0.34 to −0.14)‡ |
| E/e′ ratio | 0.15 (0.06–0.24)† | 0.23 (0.11–0.34)‡ | −0.004 (−0.06 to 0.06) | 0.07 (0.0004–0.15)* |
| Twin blood pressure | ||||
| LV mass index, g/m2 | 0.01 (−1.21 to 1.24) | 2.20 (0.60–3.79)† | −0.52 (−1.29 to 0.24) | 1.53 (0.58–2.48)† |
| LA volume index, mL/m2 | −0.05 (−0.42 to 0.32) | 0.65 (0.17–1.12)† | −0.19 (−0.42 to 0.05) | 0.40 (0.12–0.69)† |
| e′ peak, cm/s | −0.06 (−0.02 to 0.08) | −0.11 (−0.29 to 0.07) | −0.09 (−0.18 to −0.008)* | −0.19 (−0.30 to −0.09)‡ |
| E/e′ ratio | 0.09 (−0.01 to 0.20) | 0.17 (0.04–0.30)* | −0.03 (−0.10 to 0.03) | 0.09 (0.01–0.17)* |
Association sizes (95% confidence interval) express the differences in the echocardiographic indexes associated with a 10‐mm Hg higher baseline systolic blood pressure or a 5‐mm Hg higher diastolic blood pressure. All models account for clustering within families and were adjusted for sex, the baseline characteristics age, body mass index, heart rate, serum total cholesterol, plasma glucose, γ‐glutamyltransferase (index of alcohol intake) and smoking, use of lipid‐lowering treatment at follow‐up, 3 indicator variables coding for starting, stopping, or continuing antihypertensive drug treatment from baseline to follow‐up, and duration of follow‐up. Single blood pressure models include the conventional or daytime blood pressure and twin models both. LV mass index was available in 750 participants, LA volume index in 763 and e′ and E/e′ in 780. E indicates early diastolic peak velocities; e′, early peak velocities of mitral annular movement; LA, left atrial; LV, left ventricular.
Significance of the associations: *P≤0.05; † P≤0.01; and ‡ P≤0.001.
In regression models that related the echocardiographic indexes to both conventional and daytime ambulatory blood pressure and included the fixed‐effect covariables, variance inflation factor was consistently lower than 2.0. In mixed models that included both blood pressure components, findings were confirmatory (Table 2). LV mass and LA volume indexes and E/e′ increased with higher systolic and diastolic daytime pressure (P≤0.028), but not with higher conventional pressure (P≥0.086). The association sizes per 10/5‐mm Hg increment in systolic/diastolic daytime blood pressure were 2.20/1.53 g/m2, 0.65/0.40 mL/m2, and 0.17/0.09. The e′ peak velocity decreased with higher conventional (−0.09 cm/s; P=0.032) and daytime (−0.19 cm/s; P<0.001) diastolic blood pressure. In multivariable‐adjusted analyses additionally accounting for baseline conventional pulse pressure, a 10‐mm Hg higher daytime ambulatory pulse pressure was associated with a 0.20 greater E/e′ ratio (P=0.044).
Last, we replaced the conventional blood pressure measured at baseline by the office blood pressure measured concurrently with echocardiography (Table 3). Variance inflation factor for all of these models was lower than 1.6. LV mass and LA volume indexes and E/e′ increased with higher systolic and diastolic daytime pressure (P≤0.036). The association sizes per 10/5‐mm Hg increment in systolic/diastolic daytime blood pressure were 1.60/0.96 g/m2, 0.45/0.38 mL/m2, and 0.15/0.08. LV mass and LA volume indexes and E/e′ increased with higher conventional systolic pressure (P≤0.002). The association sizes per 10‐mm Hg increment in systolic conventional blood pressure were 1.44 g/m2, 0.53 mL/m2, and 0.19. The e′ peak velocity decreased with higher conventional (−0.20 cm/s; P<0.001) and daytime (−0.17 cm/s; P<0.001) diastolic blood pressure (Table 3).
Table 3.
Echocardiographic Indexes at Follow‐Up in Relation to Baseline Daytime and Follow‐Up Conventional Blood Pressure
| Model Echocardiographic Index | Systolic Blood Pressure | Diastolic Blood Pressure | ||
|---|---|---|---|---|
| Follow‐Up Conventional | Baseline Daytime | Follow‐Up Conventional | Baseline Daytime | |
| LV mass index, g/m2 | 1.44 (0.54–2.33)† | 1.60 (0.17–3.04)* | 0.55 (−0.24 to 1.33) | 0.96 (0.06–1.86)* |
| LA volume index, mL/m2 | 0.53 (0.26–0.79)‡ | 0.45 (0.03–0.88)* | −0.17 (−0.41 to 0.06) | 0.38 (0.12–0.65)† |
| e′ peak, cm/s | −0.04 (−0.14 to 0.05) | −0.11 (−0.26 to 0.04) | −0.20 (−0.28 to −0.12)‡ | −0.17 (−0.27 to −0.08)‡ |
| E/e′ ratio | 0.19 (0.12–0.26)‡ | 0.15 (0.03–0.26)* | 0.01 (−0.05 to 0.08) | 0.08 (0.01–0.16)* |
Association sizes (95% confidence interval) express the differences in the echocardiographic indexes associated with a 10‐mm Hg higher systolic blood pressure or a 5‐mm Hg higher diastolic blood pressure. All models included both blood pressure components, account for clustering within families, and were adjusted for sex, the follow‐up characteristics age, body mass index, heart rate, serum total cholesterol, plasma glucose, γ‐glutamyltransferase (index of alcohol intake) and smoking, and use of lipid‐lowering treatment, 3 indicator variables coding for starting, stopping, or continuing antihypertensive drug treatment from baseline to follow‐up, and duration of follow‐up. LV mass index was available in 750 participants, LA volume index in 763, and e′ and E/e′ in 780. E indicates early diastolic peak velocities; e′, early peak velocities of mitral annular movement; LA, left atrial; LV, left ventricular.
Significance of the associations: *P≤0.05; † P≤0.01; and ‡ P≤0.001.
Associations With Blood Pressure Category
Of the 780 participants, at baseline, 604 (77.4%) were truly normotensive based on their conventional and daytime blood pressure and 54 (6.9%), 74 (9.5%), and 48 (6.2%) had white‐coat, masked, or sustained hypertension. Among 54 white‐coat hypertensive patients, the conventional blood pressure thresholds were met by 28 participants (51.8%) for systolic pressure, by 17 (31.5%) for diastolic pressure, and by 9 (16.7%) for systolic and diastolic blood pressure. Among the 74 participants with masked hypertension, 9 (12.2%) satisfied the daytime threshold for systolic pressure, 13 (17.6%) the diastolic threshold, and 52 (70.3%) both.
Table 4 shows the echocardiographic traits by cross‐classification based on the baseline conventional and daytime blood pressure. Compared with participants with true normotension, patients with ambulatory hypertension at baseline (15.6%) had larger LV mass index (102.7 versus 89.3 g/m2; P<0.001), LA volume index (25.4 versus 22.3 mL/m2; P<0.001) and E/e′ ratio (7.64 versus 6.86; P<0.001), and smaller e′ (9.6 versus 11.8 cm/s; P<0.001) at follow‐up. Sustained or masked hypertension at baseline compared with normotension or white‐coat hypertension (Figure 3) were associated with greater LA volume index (24.0 versus 22.6 mL/m2; P=0.006) and E/e′ (7.35 versus 6.91; P=0.005) and lower e′ (10.7 versus 11.6 cm/s; P<0.001) with no differences between normotension and white‐coat hypertension (P≥0.16) or between masked and sustained hypertension (P≥0.092). A sensitivity analysis from which we excluded 61 participants on antihypertensive drug treatment at baseline produced confirmatory results (Table 4).
Table 4.
Echocardiographic Indexes by Hypertension Category at Baseline
| Echocardiographic Indexes | Normotension | White‐Coat Hypertension | Masked Hypertension | Sustained Hypertension | P NT | P WT | P MT |
|---|---|---|---|---|---|---|---|
| All (n=780) | 604 | 54 | 74 | 48 | |||
| LV mass index, g/m2 | 90.1±0.70 | 90.3±2.4 | 97.2±2.0 | 99.3±2.7 | 0.002 | 0.011 | 0.52 |
| Ejection fraction, % | 68.2±0.31 | 70.6±1.0 | 70.2±0.88 | 69.7±1.2 | 0.23 | 0.58 | 0.74 |
| LA volume index, mL/m2 | 22.6±0.22 | 21.7±0.73 | 23.4±0.61 | 25.1±0.82 | 0.004 | 0.001 | 0.092 |
| e′ peak, cm/s | 11.6±0.08 | 11.4±0.27 | 10.5±0.23 | 11.0±0.30 | 0.033 | 0.23 | 0.20 |
| E/e′ ratio | 6.89±0.06 | 7.13±0.21 | 7.34±0.17 | 7.39±0.23 | 0.038 | 0.39 | 0.86 |
| Baseline Untreated (n=719) | 569 | 42 | 69 | 39 | |||
| LV mass index, g/m2 | 89.2±0.70 | 93.0±2.6 | 96.2±2.0 | 97.3±3.0 | 0.034 | 0.29 | 0.98 |
| Ejection fraction, % | 68.1±0.32 | 71.3±1.2 | 70.1±0.91 | 69.1±1.3 | 0.50 | 0.20 | 0.53 |
| LA volume index, mL/m2 | 22.3±0.23 | 21.9±0.84 | 23.3±0.65 | 25.1±0.94 | 0.008 | 0.004 | 0.14 |
| e′ peak, cm/s | 11.9±0.08 | 11.5±0.31 | 10.8±0.24 | 11.3±0.34 | 0.069 | 0.62 | 0.24 |
| E/e′ ratio | 6.79±0.06 | 7.04±0.22 | 7.20±0.17 | 7.04±0.24 | 0.33 | 0.99 | 0.60 |
Values are mean±SE. All estimates account for clustering within families. Estimates were adjusted for sex, the baseline characteristics age, body mass index, heart rate, serum total cholesterol, plasma glucose, γ‐glutamyltransferase (index of alcohol intake) and smoking, for use of lipid‐lowering treatment at follow‐up, for 3 indicator variables coding for starting, stopping, or continuing antihypertensive drug treatment from baseline to follow‐up, and for duration of follow‐up. LV mass index (untreated at baseline) was available in 750 (694) participants, ejection fraction in 708 (655), LA volume index in 763 (703), and e′ and E/e′ in 780 (719). E indicates early diastolic peak velocities; e′, early peak velocities of mitral annular movement; LA, left atrial; LV, left ventricular; P MT, the significance of the difference between masked hypertension and sustained hypertension; P NT , the significance of the difference between normotension and sustained hypertension; P WT , the significance of the difference between white‐coat hypertension and sustained hypertension.
Figure 3.
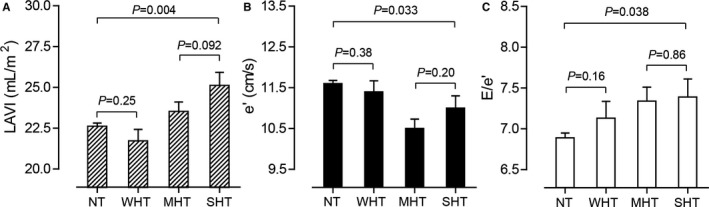
Multivariable‐adjusted means of left atrial volume index (A), e′ (B), and E/e′ (C) at follow‐up by hypertension category at baseline. NT, WHT, MHT, and SHT indicate true normotension and white‐coat, masked, and sustained hypertension, respectively. Estimates given with SE account for clustering within families and were adjusted for sex, the baseline characteristics age, body mass index, heart rate, serum total cholesterol, plasma glucose, γ‐glutamyltransferase (index of alcohol intake) and smoking, for use of lipid‐lowering treatment at follow‐up, for 3 indicator variables coding for starting, stopping, or continuing antihypertensive drug treatment from baseline to follow‐up, and for duration of follow‐up. Left atrial volume index was available in 763 participants and e′ and E/e′ in 780. P values are for the between‐group comparisons. LAVI indicates left atrial volume index.
Discussion
The key finding of our study was that ambulatory blood pressure is a long‐term predictor of diastolic LV function statistically outperforming distant but not concurrent conventional blood pressure, and that masked and sustained hypertension are equal predictors of worse diastolic LV function over a 10‐year horizon. Concurrent conventional blood pressure might directly influence the LV loading conditions and LV filling. This might explain why conventional concurrent compared with distant baseline blood pressure performed better in the associations with the indexes of LV diastolic function. The clinical implication is that ambulatory blood pressure monitoring is a prerequisite for the long‐term risk stratification for impaired diastolic LV function in relation to blood pressure. Only out‐of‐the office blood pressure monitoring allows differentiation between true normotension and risk‐carrying masked hypertension23 among individuals with normal office blood pressure or between low‐risk white‐coat hypertension30 and sustained hypertension.
To our surprise, a thorough literature search of the PubMed database, using as search terms “blood pressure” OR “ambulatory blood pressure” OR “hypertension” AND “heart” OR “left ventricular diastolic function” revealed only 1 other longitudinal population study relating E/e′ at follow‐up to the ambulatory blood pressure measured 20 years earlier.10 This Finnish study included 414 individuals enrolled in the OPERA (Oulu Project Elucidating Risk of Atherosclerosis) study.10 Age ranged from 40 to 59 years. E/e′ was the only echocardiographic index of diastolic LV function reported and analyzed as a categorical variable using a threshold of 15 to discriminate between normal (n=381) and impaired (n=33) diastolic LV performance. With adjustments applied for sex, age, stature, body mass index, prevalence of diabetes mellitus, office systolic and pulse pressure, N‐terminal pro‐atrial natriuretic peptide, and the use of antihypertensive therapy, there was no association between diastolic LV dysfunction and the 24‐hour, daytime or nighttime systolic or diastolic blood pressure. However, with additional adjustment for ambulatory diastolic blood pressure, diastolic LV dysfunction at follow‐up was associated with higher baseline pulse pressure on 24‐hour (53.4 versus 46.4 mm Hg; P=0.001), daytime (54.3 versus 47.0 mm Hg; P=0.016), and nighttime blood pressure measurements (51.2 versus 44.2 mm Hg; P=0.015).10 This Finnish study did not compare the predictive performance of the office and ambulatory blood pressure and, in view of the low number of cases and the complex adjustments for highly intercorrelated covariables, remains difficult to interpret.
The Finnish OPERA study8 and the United Kingdom Medical Research Council National Survey of Health and Development9 reported on the longitudinal associations between diastolic LV function and the conventional blood pressure. Using the same approach as in their article on ambulatory blood pressure,10 the OPERA investigators demonstrated that greater in‐office systolic blood pressure, shorter height, and lower estimated glomerular filtration rate in middle‐aged people were forerunners of diastolic dysfunction 20 years later.8 In 1653 singletons enrolled in the Medical Research Council National Survey of Health and Development birth cohort, investigators measured the participants’ conventional blood pressure, using the Hawskley random‐zero sphygmomanometer or an oscillometric device at ages 36, 43, 53, and 60 to 64 years.9 At the last follow‐up visit, diastolic LV function was also assessed. Increased systolic blood pressure at 36, 43, and 53 years was predictive of increased E/e′ and increased LA volume index. These effects were only partially explained by systolic blood pressure at 60 to 64 years or increased LV mass. Antihypertensive drug treatment was also associated with poorer diastolic function after adjustment for systolic blood pressure at age 60 to 64 years. The authors concluded that faster rates of increase in systolic blood pressure in midlife were associated with poorer diastolic function.9
In categorized analyses of baseline data, we demonstrated that sustained or masked hypertension compared with normotension or white‐coat hypertension was associated with greater LA volume index and E/e′ and lower e′ with no differences between normotension and white‐coat hypertension30 or between masked and sustained hypertension. Data obtained in a general population are less prone to bias than studies performed in hypertensive populations. Our literature search did not identify any longitudinal study linking blood pressure categories at baseline with diastolic LV function at follow‐up. In a cross‐sectional study of 52 111 Korean adults who had their office blood pressure measured oscillometrically and who were examined echocardiographically, the adjusted mean E/e′ ratio was 7.56 in normotensive people, 7.89 and 8.17 in prehypertensive and controlled hypertensive patients, and 8.28 and 8.54 in newly diagnosed and uncontrolled patients.31 The LV mass and LA volume indexes showed similar trends.31 The International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcome includes randomly enrolled population samples who had office and ambulatory blood pressure and cardiovascular risk factors measured at baseline with a longitudinal follow‐up of fatal and nonfatal cardiovascular outcomes.23 Using a daytime threshold of 135/85 mm Hg,13 the prevalence of normotension and white‐coat, masked, and sustained hypertension was 49.4%, 10.6%, 14.6%, and 25.4%, respectively.23 The multivariable‐adjusted risk associated with white‐coat hypertension did not differ from normotension, whereas masked hypertension conferred a risk not different from that of sustained hypertension.23 Our current study extends the International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcome findings to a trait reflecting intermediate target organ damage (ie, diastolic LV dysfunction).
The clinical implications of our current findings can be gauged against the prognosis associated with asymptomatic diastolic LV dysfunction, which in the general population has a prevalence of around 25%4, 5 and over time evolves to symptomatic LV dysfunction6 and heart failure2 and predicts the incidence of adverse health outcomes. Guideline‐driven echocardiographic criteria24, 25 to stage patients with advanced diastolic LV dysfunction leave a large proportion of people unclassified in population studies. As we reported previously,32 the threshold of 7 cm/s for e′ corresponds with the 10th percentile of the distribution in the current study population and the thresholds 14 for E/e′ and 34 mL/m2 for LAVI are equivalent to the 95th percentiles of their distribution. Among 793 Flemish followed up for 5 years, the multivariable‐adjusted hazard ratios per 1‐SD decrease (P=0.001) in e′ amounted to 2.50 and 3.66 for cardiovascular and cardiac complications, respectively.33 Furthermore, in 2042 participants enrolled in the Olmsted County Study34 and followed up for 3.5 years, mild (20.8%) and moderate‐to‐severe (7.3%) diastolic LV dysfunction at baseline predicted all‐cause mortality with hazard ratios of 8.3 and 10.2 (P<0.001). In the Framingham Heart Study, remote blood pressure (average of all reading 11–20 years before current) and recent blood pressure (average of all reading 1–10 years before current) predicted the risk of cardiovascular disease incrementally over current blood pressure.35 This observation was consistent irrespective of sex and age.35 Explanations offered by the Framingham investigators were that antecedent blood pressure is a forerunner of cardiovascular target organ damage, which is on the path to hard cardiovascular complications, and that the relation between cardiovascular risk and blood pressure weakens over time by the initiation of antihypertensive drug treatment.35 What our current study adds is that ambulatory blood pressure is a long‐term predictor of diastolic LV function, statistically outperforming distant but not concurrent conventional blood pressure.
Our current study must be interpreted within the context of some potential limitations. First, in line with current practice,13 we used daytime not 24‐hour ambulatory or nighttime blood pressure to categorize our participants. Our study participants could opt to have their 24‐hour blood pressure monitored. However, in view of the discomfort caused by nighttime blood pressure readings, only 290 had whole‐day recordings. Participants opting for 24‐hour instead of daytime‐only monitoring had similar sex distribution and prevalence of smoking and plasma glucose (P≥0.36), but were on average 6.0 years older and therefore had a slightly but significantly (P≤0.038) higher body mass index, blood pressure, serum cholesterol, and plasma glucose. Previous studies demonstrated that using daytime or 24‐hour blood pressure yields similar proportions of patients with white‐coat and masked hypertension36 as well as similar estimates of cardiovascular risk.37 Second, the prevalence of white‐coat hypertension in our study was about two thirds less as compared with other studies of populations23, 37 and patients.36 However, our participants were repeatedly followed up by the same team of study nurses living in the catchment area of the study. Familiarization of participants with the study team is a likely explanation of the low prevalence of white‐coat hypertension and the 5.6‐beat/min decrease in heart rate from baseline to follow‐up.38 Finally, our study included only white Europeans. However, in the international multiethnic International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcome study, there were no differences in the risks associated with blood pressure among Europeans, Asians, and South Americans.37
In conclusion, ambulatory blood pressure is a long‐term predictor of diastolic LV function outperforming distant but not concurrent conventional blood pressure. Masked and sustained hypertension carry equal risk for deterioration of diastolic LV function. The take‐home message of our current study is that multiple measurements of blood pressure outside the medical environment are superior to fewer measurements by observers to screen for diastolic LV dysfunction and that ambulatory monitoring, as already proposed more than a decade ago by Thomas Pickering39 and as reiterated in contemporary guidelines,11, 12, 13, 14 is the state‐of‐the‐art technique for assessing blood pressure in clinical practice and research.
Sources of Funding
The European Union (HEALTH‐F7‐305507 HOMAGE) and the European Research Council (Advanced Researcher Grant 2011‐294713‐EPLORE and Proof‐of‐Concept Grant 713601‐uPROPHET), the European Research Area Net for Cardiovascular Diseases (JTC2017‐046‐PROACT), and the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0881.13, G.088013, and 11Z0916N) currently support the Studies Coordinating Centre in Leuven.
Disclosures
None.
Acknowledgments
The authors gratefully acknowledge the contribution of the nurses working at the examination center (Linda Custers, Marie‐Jeanne Jehoul, Daisy Thijs, and Hanne Truyens) and the clerical staff at the Studies Coordinating Centre (Vera De Leebeeck, Yvette Piccart, and Renilde Wolfs).
(J Am Heart Assoc. 2018;7:e007868 DOI: 10.1161/JAHA.117.007868.)29437597
References
- 1. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction. J Am Coll Cardiol. 2013;62:263–271. [DOI] [PubMed] [Google Scholar]
- 3. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. [DOI] [PubMed] [Google Scholar]
- 4. Kuznetsova T, Herbots L, López B, Jin Y, Richart T, Thijs L, González A, Herregods MC, Fagard RH, Díez J, Staessen JA. Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail. 2009;2:105–112. [DOI] [PubMed] [Google Scholar]
- 5. Kloch‐Badelek M, Kuznetsova T, Sakiewicz W, Tikhonoff V, Ryabikov A, González A, Loster M, Thijs L, Jin Y, Malyutina S, Stolarz‐Skrzypek K, Casiglia E, Díez J, Narkiewicz K, Kawecka‐Jaszcz K, Staessen JA; on behalf of the European Project on Genes in Hypertension (EPOGH) Investigators . Prevalence of diastolic left ventricular dysfunction in European populations based on cross‐validated diagnostic thresholds. Cardiovasc Ultrasound. 2012;10:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kuznetsova T, Thijs L, Knez J, Cauwenberghs N, Petit T, Gu YM, Zhang Z, Staessen JA. Longitudinal changes in left ventricular diastolic dysfunction in a general population. Circ Cardiovasc Imaging. 2015;8:e002882. [DOI] [PubMed] [Google Scholar]
- 7. Zhang Y, Li Y, Ding FH, Sheng CS, Huang QF, Wang JG. Cardiac structure and function in relation to central blood pressure components in Chinese. J Hypertens. 2011;29:2462–2468. [DOI] [PubMed] [Google Scholar]
- 8. Perkiömäki JS, Möttönen M, Lumme J, Kesäniemi YA, Ukkola O, Huikuri HV. Predictors of development of echocardiographic left ventricular diastolic dysfunction in the subjects aged 40 to 59 years (from the Oulu Project Elucidating Risk of Atherosclerosis Study). Am J Cardiol. 2015;116:1374–1378. [DOI] [PubMed] [Google Scholar]
- 9. Ghosh AK, Hughes AD, Francis D, Chaturvedi N, Pellerin D, Deanfield J, Kuh D, Mayet J, Hardy R; on behalf of the MRC NSHD Scientific and Data Collection Team . Midlife blood pressure predicts future diastolic dysfunction independently of blood pressure. Heart. 2016;102:1380–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pääkkõ TJW, Renko RJ, Perkiõmäki JS, Kesäniemi YA, Ylitalo AS, Lumme JA, Huikuri HV, Ruskoaho H, Vuolteenaho O, Ukkola OH. Ambulatory pulse pressure predicts the development of left ventricular diastolic dysfunction in over 20 years of follow‐up. Am J Hypertens. 2017;30:985–992. [DOI] [PubMed] [Google Scholar]
- 11. Siu AL; on behalf of the U.S. Preventive Services Task Force . Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–786. [DOI] [PubMed] [Google Scholar]
- 12. National Institute for Health and Clinical Excellence (NICE) . The Clinical Management of Primary Hypertension in Adults. London, UK: National Institute for Health and Clinical Excellence; 2011. [Google Scholar]
- 13. O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head G, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope L, Shennan A, Staessen JA, van Montfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y; on behalf of the European Society of Hypertension Working Group on Blood Pressure Monitoring . European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1767. [DOI] [PubMed] [Google Scholar]
- 14. Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, Cloutier L, Gelfer M, Lamarre‐Cliche M, Milot A, Bolli P, Tremblay G, McLean D, Tobe SW, Ruzicka M, Burns KD, Vallée M, Prasad GVR, Lebel M, Feldman RD, Selby P, Pipe A, Schiffrin EL, McFarlane PA, Oh P, Hegele RA, Khara M, Wilson TW, Penner SB, Burgess E, Herman RJ, Bacon SL, Rabkin SW, Gilbert RE, Campbell TS, Grover S, Honos G, Lindsay P, Hill MD, Coutts SB, Gubitz G, Campbell NRC, Moe GW, Howlett JG, Boulanger JM, Prebtani A, Larochelle P, Leiter LA, Jones C, Ogilvie RI, Woo V, Kaczorowski J, Trudeau L, Petrella RJ, Hiremath S, Drouin D, Lavoie KL, Hamet P, Fodor G, Grégoire JC, Lewanczuk R, Dresser GK, Sharma M, Reid D, Lear SA, Moullec G, Gupta M, Magee LA, Logan AG, Harris KC, Dionne J, Fournier A, Benoit G, Feber J, Poirier L, Padwal RS, Rabi DM; for the CHEP Guidelines Task Force . Hypertension Canada's 2016 Canadian Hypertension Education Program guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2016;32:569–588. [DOI] [PubMed] [Google Scholar]
- 15. Wei FF, Zhang ZY, Thijs L, Yang WY, Jacobs L, Cauwenberghs N, Gu YM, Kuznetsova T, Allegaert K, Verhamme P, Li Y, Struijker‐Boudier HAJ, Staessen JA. Conventional and ambulatory blood pressure as predictors of retinal arteriolar narrowing. Hypertension. 2016;68:511–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Medical Association . Declaration of Helsinki. J Am Med Assoc. 2013;227:184–189. [Google Scholar]
- 17. Li Y, Zagato L, Kuznetsova T, Tripodi G, Zerbini G, Richart T, Thijs L, Manunta P, Wang JG, Bianchi G. Angiotensin‐converting enzyme I/D and α‐adducin Gly460Trp polymorphisms. From angiotensin‐converting enzyme activity to cardiovascular outcome. Hypertension. 2007;49:1291–1297. [DOI] [PubMed] [Google Scholar]
- 18. Staessen J, Bulpitt CJ, Fagard R, Jossens JV, Lijnen P, Amery A. Familial aggregation of blood pressure, anthropometric characteristics and urinary excretion of sodium and potassium—a population study in two Belgian towns. J Chronic Dis. 1985;38:397–407. [DOI] [PubMed] [Google Scholar]
- 19. Kuznetsova T, Staessen JA, Kawecka‐Jaszcz K, Babeanu S, Casiglia E, Filipovský J, Nachev C, Nikitin Y, Peleská J, O'Brien E; on behalf of the EPOGH Investigators . Quality control of the blood pressure phenotype in the European Project on Genes in Hypertension. Blood Press Monit. 2002;7:215–224. [DOI] [PubMed] [Google Scholar]
- 20. Groppelli A, Omboni S, Parati G, Mancia G. Evaluation of noninvasive blood pressure monitoring devices Spacelabs 90202 and 90207 versus resting and ambulatory 24‐hour intra‐arterial blood pressure. Hypertension. 1992;20:227–232. [DOI] [PubMed] [Google Scholar]
- 21. Thijs L, Staessen J, Fagard R, Zachariah P, Amery A. Number of measurements required for the analysis of diurnal blood pressure profile. J Hum Hypertens. 1994;8:239–244. [PubMed] [Google Scholar]
- 22. Fagard R, Brguljan J, Thijs L, Staessen J. Prediction of the actual awake and asleep blood pressures by various methods of 24 h pressure analysis. J Hypertens. 1996;14:557–563. [DOI] [PubMed] [Google Scholar]
- 23. Hansen TW, Kikuya M, Thijs L, Björklund‐Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp‐Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA; on behalf of the IDACO Investigators . Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta‐analysis of 7030 individuals. J Hypertens. 2007;25:1554–1564. [DOI] [PubMed] [Google Scholar]
- 24. Gottdiener JS, Bednarz J, Devereux R, Gardin J, Klein A, Manning WJ, Morehead A, Kitzman D, Oh J, Quinones M, Schiller NB, Stein JH, Weissman NJ; American Society of Echocardiography recommendations for use of echocardiography in clinical trials . A report from the American Society of Echocardiography's Guidelines and Standard Committee and the Task Force on Echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17:1086–1119. [DOI] [PubMed] [Google Scholar]
- 25. Nagueh SF. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314. [DOI] [PubMed] [Google Scholar]
- 26. McFadden CB, Brensinger CM, Berlin JA, Townsend RR. Systematic review of the effect of daily alcohol intake on blood pressure. Am J Hypertens. 2005;18:276–286. [DOI] [PubMed] [Google Scholar]
- 27. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus . Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(suppl 1):S5–S20. [DOI] [PubMed] [Google Scholar]
- 28. Whitehead TP, Clarke CA, Whitfield AGW; Medical Service Study Group of the Royal College of Physicians of London . Biochemical and haematological markers of alcohol intake. Lancet. 1978;311:978–981. [DOI] [PubMed] [Google Scholar]
- 29. Kleinbaum DG, Kupper LL, Muller KE. Regression diagnostics In: Kleinbaum DG, Kupper LL, Muller KE, ed. Applied Regression Analysis and Other Multivariate Methods. Boston, MA: PWS‐Kent Publishing Company; 1988:181–227. [Google Scholar]
- 30. Asayama K, Li Y, Franklin SS, Thijs L, O'Brien E, Staessen JA. Cardiovascular risk associated with white‐coat hypertension. Con side of the argument. Hypertension. 2017;70:676–682. [DOI] [PubMed] [Google Scholar]
- 31. Jung JY, Park SK, Oh CM, Kang JG, Choi JM, Ryoo JH, Lee JH. The influence of prehypertension, controlled and uncontrolled hypertension on left ventricular diastolic function and structure in the general Korean population. Hypertens Res. 2017;40:606–612. [DOI] [PubMed] [Google Scholar]
- 32. Zhang ZY, Ravassa S, Yang WY, Petit T, Pejchinovski M, Zürbig P, López B, Wei FF, Pontillo C, Thijs L, Jacobs L, González A, Koeck T, Delles C, Voigt JU, Verhamme P, Kuznetsova T, Díez J, Mischak H, Staessen JA. Diastolic left ventricular function in relation to urinary and serum collagen biomarkers in a general population. PLoS One. 2016;11:e0167582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kuznetsova T, Thijs L, Knez J, Herbots L, Zhang Z, Staessen JA. Prognostic value of left ventricular diastolic dysfunction in a general population. J Am Heart Assoc. 2014;3:e000789 DOI: 10.1161/JAHA.114.000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community. Appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. [DOI] [PubMed] [Google Scholar]
- 35. Vasan RS, Massaro JM, Wilson PWF, Seshadri S, Wolf PA, Levy D, D'Agostino RB. Antecedent blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2002;105:48–53. [DOI] [PubMed] [Google Scholar]
- 36. Zhang L, Li Y, Wei FF, Thijs L, Kang YY, Wang S, Xu TY, Wang JG, Staessen JA. Strategies for classifying patients based on office, home and ambulatory blood pressure measurement. Hypertension. 2015;65:1258–1265. [DOI] [PubMed] [Google Scholar]
- 37. Brguljan‐Hitij J, Thijs L, Li Y, Hansen TW, Boggia J, Liu YP, Asayama K, Wei FF, Björklund‐Bodegård K, Gu YM, Ohkubo T, Jeppesen J, Torp‐Pedersen C, Dolan E, Kuznetsova T, Stolarz‐Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka‐Jaszcz K, Filipovský J, Imai Y, Wang JG, O'Brien E, Staessen JA; on behalf of the Ambulatory blood pressure monitoring in relation to Cardiovascular Outcome (IDACO) Investigators . Risk stratification by ambulatory blood pressure monitoring across JNC classes of conventional blood pressure. Am J Hypertens. 2014;27:956–965. [DOI] [PubMed] [Google Scholar]
- 38. Schouten F, Twisk JW, de Boer MR, Stehouwer CD, Serné EH, Smulders YM, Ferreira I. Increases in central fat mass and decreases in peripheral fat mass are associated with accelerated arterial stiffening in healthy adults: the Amsterdam Growth and Health Longitudinal Study. Am J Clin Nutr. 2011;94:40–48. [DOI] [PubMed] [Google Scholar]
- 39. Pickering TG, Shimbo D, Haas D. Ambulatory blood‐pressure monitoring. N Engl J Med. 2006;354:2368–2374. [DOI] [PubMed] [Google Scholar]


