Abstract
Background
Atrial fibrillation (AF) is a well‐established risk factor for ischemic stroke (IS). Emerging evidence also indicates an association between AF and pulmonary embolism (PE). Because IS may potentially mediate the observed risk of PE in AF, we aimed to assess the impact of AF on the cause‐specific risks of PE and IS in a large cohort recruited from the general population.
Methods and Results
We observed 29 842 participants from 3 surveys of the Tromsø study (inclusion in 1994–1995, 2001–2002, and 2007–2008) to the end of 2012. Incident events of AF, IS, and PE during follow‐up were recorded, and information on potential confounders was obtained at baseline. Cox regression models, with AF as a time‐dependent variable, were used to calculate cause‐specific hazard ratios (HRs) with 95% confidence intervals (CIs) for PE and IS. There were 2067 participants diagnosed as having AF, 296 with PE and 1164 with IS, during a median of 17.6 years of follow‐up. The risks of PE (HR, 10.88; 95% CI, 6.23–18.89) and IS (HR, 6.16; 95% CI, 4.47–8.48) were substantially increased during the first 6 months after AF diagnosis, with crude incidence rates of 18.5 per 1000 person‐years for PE and 52.8 per 1000 person‐years for IS. The risk estimates remained elevated for both PE (HR, 1.72; 95% CI, 1.10–2.71) and IS (HR, 2.45; 95% CI, 2.05–2.92) throughout the study period.
Conclusions
AF was associated with increased cause‐specific risks of both PE and IS. Our findings infer that the risk of PE in AF is not explained by intermediate IS.
Keywords: atrial fibrillation, epidemiology, ischemic stroke, pulmonary embolism, risk factor
Subject Categories: Atrial Fibrillation, Epidemiology, Ischemic Stroke, Embolism, Thrombosis
Clinical Perspective
What Is New?
In the present prospective study, atrial fibrillation conferred a significantly increased risk of pulmonary embolism in cause‐specific analysis that did not appear to be explained by intermediate ischemic stroke.
What Are the Clinical Implications?
Our findings suggest that underlying atrial fibrillation should be actively sought in patients presenting with isolated pulmonary embolism.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia, affecting >33 million individuals worldwide, and both the incidence and prevalence of AF are increasing.1, 2 AF contributes substantially to morbidity and mortality, with ischemic stroke (IS) being its most detrimental complication.2 Strokes occur in patients with AF when thrombi formed in the fibrillating left atrium embolize to the cerebral circulation.3 Thrombus formation in the right atrium has also been reported in patients with AF,4, 5 suggesting that pulmonary embolism (PE) may arise from intracardiac thrombi. Although traditionally perceived as a complication to deep vein thrombosis (DVT), recent data indicate that 50% of the PE events occur in the absence of detectable DVTs.6, 7
Findings from recent observational studies support the concept that AF is a risk factor for PE. Several studies in selected hospital‐based cohorts have demonstrated increased prevalence of AF in patients with acute PE compared with the general population.8, 9, 10 In a previous study, we found that patients with AF had an increased risk of subsequent venous thromboembolism (VTE). The risk was especially high during the first 6 months after the diagnosis of AF, particularly for PE, and 15% to 20% of the PE events in the population could be attributed to AF.11 A similar association between AF and PE was shown in a large population‐based registry study from Taiwan.12
The apparent association between AF and PE may be attributable to shared risk factors, induced by factors related to AF itself (eg, intracardiac thrombi), or mediated by stroke or stroke‐related complications secondary to AF. Both clinical trials and population‐based studies have convincingly shown that patients with stroke are at increased VTE risk, especially during the first months after diagnosis.13, 14, 15 Strokes caused by AF are more severe16 and frequently result in hospitalization and comorbid conditions, such as dehydration, immobility, and infections, that may additionally contribute to increase the risk of VTE.17 Therefore, we aimed to assess the impact of AF on PE risk in the absence of IS.
Methods
Study Population
Study participants were recruited from the fourth (1994–1995), fifth (2001–2002), and sixth (2007–2008) surveys of the Tromsø study, an ongoing prospective health study of the inhabitants in Tromsø, Norway. For these surveys, the entire population (Tromsø 4) or parts of the population (Tromsø 5 and 6) aged ≥25 years living in the Tromsø municipality were invited to participate. The attendance rates were high, ranging from 77% in Tromsø 4 to 66% in Tromsø 6. A total of 30 586 participants aged 25 to 97 years participated in at least 1 of the surveys. Detailed descriptions of the Tromsø study inclusion criteria and participation have been published previously.18, 19 Participants who did not give their written consent to medical research (n=181), those not officially registered as inhabitants of the municipality of Tromsø at study enrollment (n=23), and participants with VTE (n=78), IS (n=216), or AF (n=246) before the inclusion date were excluded. In total, 29 842 participants were included in the study and observed from the date of enrollment until the end of follow‐up, December 31, 2012 (Figure 1).
Figure 1.
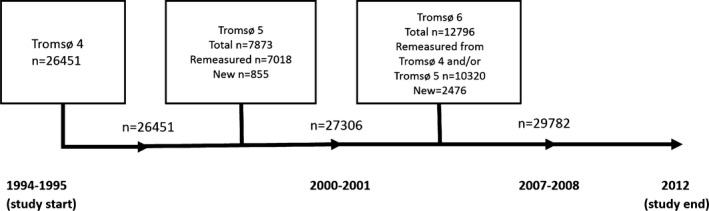
Inclusion of study participants from the fourth (1994–1995), fifth (2001–2002), and sixth (2007–2008) surveys of the Tromsø study.
Baseline Measurements
Baseline information was collected by physical examination, nonfasting blood samples, and self‐administered questionnaires. Blood pressure was measured after 2 minutes of rest using an automatic device (Dinamap Vital Signs Monitor, 1846; Critikon Inc, Tampa, FL). Three readings were taken on the upper right arm at 1‐minute intervals, and the average of the 2 last readings was used in the analysis. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or current use of antihypertensive drugs. Nonfasting blood samples were obtained from all study participants, and serum was prepared and analyzed at the Department of Clinical Biochemistry, University Hospital of North Norway. Serum total cholesterol, serum high‐density lipoprotein cholesterol, and serum triglycerides were measured, as previously described.20 Height and weight were measured with participants wearing light clothing and no shoes. Body mass index (BMI) was calculated as weight in kilograms per height in meters squared (kg/m2). History of myocardial infarction (MI), diabetes mellitus, and current smoking was obtained from a self‐administered questionnaire. Physical activity was defined as ≥1 hour of moderate or hard physical activity (vigorous enough to work up a sweat and cause shortness of breath) per week (yes/no).
Exposure: AF
Incident AF during follow‐up was identified by searching the discharge diagnosis registry at the University Hospital of North Norway (diagnoses from both hospitalizations and outpatient clinic visits), the only hospital serving the entire area of Tromsø, and the National Causes of Death registry at Statistics Norway. Because Norway has a unique personal identification system that allows exact matching of population register data, the identification number of the Tromsø study participants was linked to the diagnosis registries, using the following diagnosis codes: International Classification of Diseases, Ninth Revision (ICD‐9) codes 427.0 to 427.99 and ICD‐10 codes I47 and I48. For participants with a diagnosis of cerebrovascular or cardiovascular events without a diagnosis of arrhythmia, paper versions of hospital records (used until 2001) for notes on AF were manually searched, and text searches with the term “atrial fibrillation” were performed in the electronic records. The medical record of each potential patient with AF was reviewed by trained personnel. The diagnosis of AF had to be documented by an ECG, and an independent end point committee adjudicated all events. Classification of AF into paroxysmal and persistent versus permanent forms was performed when possible. People having paroxysmal AF initially, but who later developed a permanent form, were classified as having permanent AF. Participants in whom the AF could not be classified as paroxysmal or persistent and participants with transient AF occurring only during an acute MI or in relation to cardiac surgery were defined as “other AF.”
Outcomes: PE and IS
Incident symptomatic PE during follow‐up was identified by searching the hospital discharge diagnosis registry, the autopsy registry, and the radiology procedure registry at the University Hospital of North Norway, as previously described.21 Medical records of each potential PE case were retrieved for case validation by trained personnel. A PE event was considered verified and recorded when the presence of clinical signs and symptoms of PE was combined with objective confirmation tests (spiral computed tomography, perfusion‐ventilation scan, pulmonary angiography, or autopsy) and resulted in a PE diagnosis that required treatment. PE cases from the autopsy registry were recorded when the death certificate indicated PE as the cause of death or a significant condition associated with death.
Incident IS was defined according to the World Health Organization definition as rapidly developing clinical signs of focal or global disturbance of cerebral function, with symptoms lasting ≥24 hours or leading to death with no apparent cause other than vascular origin, and only when computed tomography, magnetic resonance imaging, or autopsy had ruled out intracerebral or subarachnoid hemorrhage.22 The diagnosis registry at the University Hospital of North Norway (the outpatient clinic included) and the National Causes of Death registry at Statistics Norway were searched for cases of possible nonfatal and fatal IS identified by a broad search for the ICD‐8 and ICD‐9 codes 430 to 438 and ICD‐10 codes I60 to I69 (cerebrovascular diseases). To ensure case completeness, additional systematic manual and electronic text searches were performed in the medical records for patients with ICD‐8 and ICD‐9 diagnosis codes 410 to 414 and 798 to 799 and ICD‐10 codes I20 to I25, R96, R98, and R99. Event validation was performed by an independent end point committee on the basis of retrieved data from hospital and out‐of‐hospital medical records, autopsy records, and death certificates. Event validation followed a detailed protocol, according to established diagnostic criteria.
Statistical Analyses
Participants who developed AF during the study period contributed with nonexposed person‐time from the date of enrollment to the date of a diagnosis of AF and with exposed person‐time from the date of AF onwards. Participants with incident AF and VTE on the same day (n=9) or AF and IS on the same day (n=51) were excluded from the analyses because the temporal sequence of events could not be determined in these participants. For each participant, nonexposed and exposed person‐years were counted from the date of enrollment to the date of a diagnosis of IS or PE, the date the participant died or moved from the municipality of Tromsø, or the end of the study period (December 31, 2012), whichever came first. Participants who died (n=4441) or moved (n=4457) during follow‐up were censored at the date of migration or death.
Statistical analyses were performed with STATA, version 14 (Stata Corporation, College Station, TX). Cause‐specific models were used, in which attained age was used as time scale, with participants’ age at study enrollment defined as entry time; exit time was defined as age at the censoring event (PE, IS, death, migration, or study end). All subjects had, at most, 1 of the 2 outcomes (ie, PE or IS) on the date of first occurrence in the cause‐specific model. Participants who experienced a DVT during follow‐up without confirmed concurrent PE were censored at the date of DVT diagnosis. The exposure variable AF was included as a time‐dependent variable using multiple observation periods per study participant. None of the participants had AF at study entry, and the variable was updated in subjects who experienced AF during follow‐up. Cause‐specific hazard ratios (HRs) for PE and IS, according to time since AF diagnosis (any time or <6 and ≥6 months), were calculated. These HRs were further adjusted for potential confounding factors (ie, sex, BMI, smoking status, hypertension, cholesterol levels, and self‐reported history of MI and diabetes mellitus). The proportional hazards assumption was tested using Schoenfeld residuals, and no violation was found. Statistical interactions between AF and sex were tested by including cross‐product terms in the proportional hazards model. A significant interaction between sex and AF on IS was present, and we consequently performed analyses stratified by sex for both outcomes. We also performed sensitivity analyses in which participants who experienced AF only within 28 days after cardiac surgery or MI or in the last 7 days of life were excluded.
To show the change in risk of PE and IS over time, HRs of PE and IS were plotted against time (0.5, 1, 3, 5, and 10 years) since AF diagnosis, using GraphPad Prism, version 5.0 (GraphPad Software, San Diego, CA).
Attributable risk, the proportion of events among the exposed participants that can be explained by the exposure, was calculated from incidence rates of PE and IS in the population with AF (Ie) and without AF (I0) [100%×(Ie−I0)/Ie]. Population attributable risk, the proportion of events in the study population attributable to the exposure, was calculated by use of the incidence rates of PE and IS in the entire population (Ip) and in I0 [100%×(Ip−I0)/Ip].
Results
Among 29 782 study participants, 2067 (6.9%) developed AF, 1164 (3.9%) had an incident IS, and 700 (2.4%) had a VTE (405 with DVT and 295 with PE) during a median of 17.6 years of follow‐up (range, 2 days to 18.3 years). Sixty‐eight participants experienced both IS and VTE (PE and/or DVT) during follow‐up, and follow‐up was terminated at the date of their first event. In those with AF, 198 (9.6%) subsequently developed an IS and 36 (1.7%) developed a PE.
Baseline characteristics of the study participants are shown in Table 1. Participants with AF during follow‐up were considerably older than participants without AF, with an average age difference of 16 years (Table 1). Compared with those without AF, participants with AF had a less favorable cardiovascular risk profile, with higher mean cholesterol and triglyceride levels, higher BMI, and a larger proportion of hypertension, diabetes mellitus, smoking, physical inactivity, and self‐reported cardiovascular disease (Table 1). Among the 2067 participants with AF during follow‐up, 680 had an MI before or after AF diagnosis. Twenty‐five people had both PE and MI, and the median time to event for PE in relation to MI was 9.4 months (mean, 4.6 years). One‐hundred forty‐four people had both IS and MI, and the median time to event for IS in relation to MI was 4.4 years (mean, 5.3 years).
Table 1.
Baseline Characteristics of Participants With or Without AF During Follow‐Up
| Characteristics | Participants Without AF (n=27 715) | Participants With AF (n=2067) | P Value |
|---|---|---|---|
| Type of AF | |||
| Paroxysmal/persistent | ··· | 41.6 (861) | ··· |
| Permanent | ··· | 36.4 (752) | ··· |
| Other | ··· | 22.0 (454) | ··· |
| Male sex | 46.7 (12 949) | 55.5 (1148) | <0.001 |
| Age, y | 45.0 (14.0) | 62.4 (11.8) | <0.001 |
| BMI, kg/m2 | 25.2 (3.9) | 26.9 (4.2) | <0.001 |
| Total cholesterol, mmol/L | 5.91 (1.29) | 6.68 (1.22) | <0.001 |
| Triglycerides, mmol/L | 1.53 (1.04) | 1.75 (1.06) | <0.001 |
| HDL cholesterol, mmol/L | 1.49 (0.41) | 1.50 (0.43) | 0.41 |
| Systolic blood pressure, mm Hg | 132 (19) | 150 (24) | <0.001 |
| Diastolic blood pressure, mm Hg | 77 (12) | 85 (13) | <0.001 |
| Hypertensiona | 31.5 (8730) | 69.6 (1439) | <0.001 |
| Smoking | 36.6 (10 103) | 27.9 (575) | <0.001 |
| Physical activityb | 33.3 (9222) | 21.0 (433) | <0.001 |
| Self‐reported MI | 3.8 (1044) | 17.6 (364) | <0.001 |
| Self‐reported diabetes mellitus | 1.5 (424) | 4.8 (99) | <0.001 |
Values are given as percentages (absolute numbers) or as means (SDs). AF indicates atrial fibrillation; BMI, body mass index; HDL, high‐density lipoprotein; and MI, myocardial infarction.
Systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or current use of antihypertensive drugs.
One or more hours of moderate or hard physical activity per week.
Incidence rates and cause‐specific HRs for PE and IS during follow‐up are presented in Table 2. Participants with AF had higher relative and absolute risks of both PE and stroke compared with those without AF. For both outcomes, the incidence rates were highest during the first 6 months after AF diagnosis (18 PEs/1000 person‐years and 53 ISs/1000 person‐years). In this time period, the relative risk of PE was 11‐fold higher in those with AF than in those without AF (HR, 10.88; 95% confidence interval [CI], 6.23–18.89). Furthermore, the risk of PE remained 72% increased in the period ≥6 months up to 17 years after AF diagnosis (HR, 1.72; 95% CI, 1.10–2.71) (Table 2). When examining PE risk at different time points after AF diagnosis, the risk decreased over time and disappeared 3 years after onset of AF (Figure 2A). The risk of stroke was 6‐fold increased in the first 6 months after AF diagnosis (HR, 6.16; 95% CI, 4.47–8.48) and 2.5‐fold increased during the remaining follow‐up period (HR, 2.45; 95% CI, 2.05–2.92) (Table 2). The risk diminished over time but was still 2‐fold increased >10 years after onset of AF (Figure 2B). Further adjustments for BMI, smoking, total cholesterol, hypertension, self‐reported cardiovascular disease, and diabetes mellitus slightly attenuated the risk estimates for both outcomes (Table 2). Although patients with AF appeared to have a more sedentary lifestyle (Table 1), the impact of AF on PE and IS risk was not altered by adjustment for self‐reported physical activity (data not shown). The attributable risks of PE and stroke by AF were 86.9% and 90.6%, respectively, and 11.6% of the PE events and 15.7% of the ISs in the population were attributable to AF.
Table 2.
Crude IRs and HRs for PE and IS in Participants Developing AF During Follow‐Up Compared With Subjects Without AF
| Variable | Person‐Years | Events | Crude IR (95% CI)a | HR (95% CI) | |
|---|---|---|---|---|---|
| Model 1b | Model 2c | ||||
| PE | |||||
| No AF | 397 384 | 239 | 0.60 (0.53–0.69) | Reference | Reference |
| At any time after AF diagnosis | 7852 | 36 | 4.58 (3.30–6.35) | 2.57 (1.78–3.71) | 2.45 (1.69–3.56) |
| <6 mo after AF diagnosis | 758 | 14 | 18.46 (10.93–31.17) | 10.88 (6.23–18.89) | 10.57 (6.09–18.37) |
| ≥6 mo after AF diagnosis | 7094 | 22 | 3.10 (2.04–4.71) | 1.72 (1.10–2.71) | 1.64 (1.05–2.59) |
| IS | |||||
| No AF | 397 384 | 942 | 2.37 (2.22–2.52) | Reference | Reference |
| At any time after AF diagnosis | 7852 | 198 | 25.22 (21.94–28.99) | 2.79 (2.38–3.27) | 2.63 (2.24–3.10) |
| <6 mo after AF diagnosis | 758 | 40 | 52.75 (38.69–71.91) | 6.16 (4.47–8.48) | 5.86 (4.25–8.07) |
| ≥6 mo after AF diagnosis | 7094 | 158 | 22.27 (19.06–26.03) | 2.45 (2.05–2.92) | 2.30 (1.93–2.75) |
AF indicates atrial fibrillation; CI, confidence interval; HR, hazard ratio; IR, incidence rate; IS, ischemic stroke; and PE, pulmonary embolism.
Per 1000 person‐years.
Using age as time scale and adjusted for sex.
Using age as time scale and adjusted for sex, body mass index, smoking, total cholesterol, hypertension, and history of myocardial infarction and diabetes mellitus.
Figure 2.
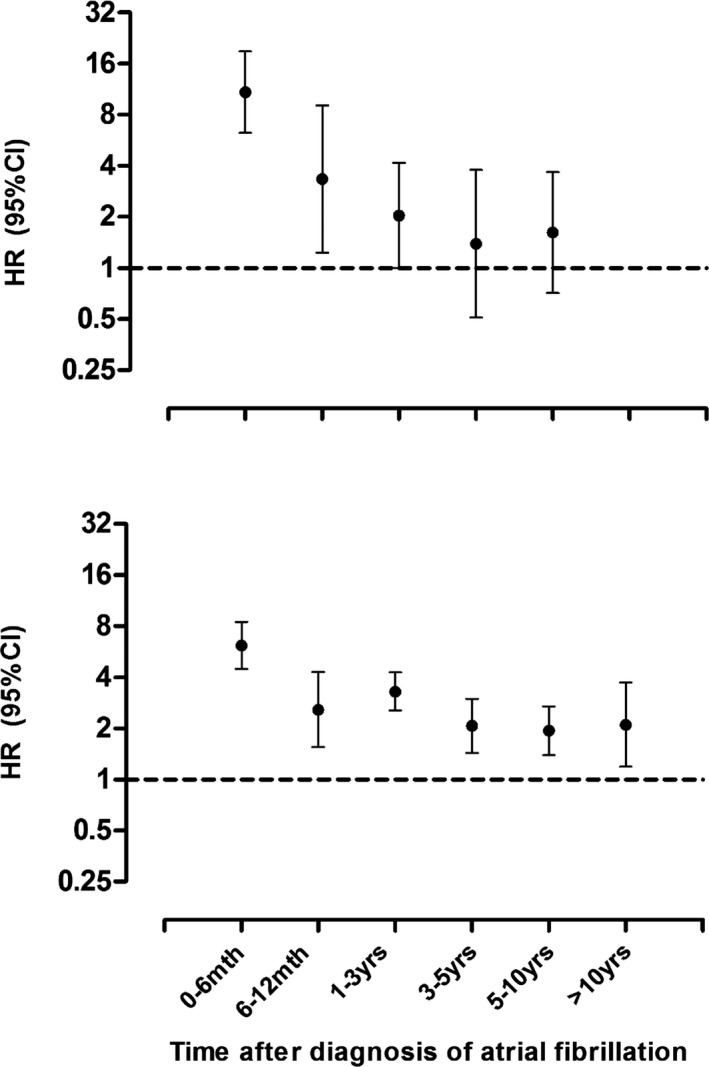
Hazard ratios (HRs) with 95% confidence intervals (CIs) for pulmonary embolism (A) and ischemic stroke (B) by time periods after a diagnosis of atrial fibrillation.
In analyses stratified by sex, crude incidence rates for IS were higher in women than in men (Table 3). Similarly, AF also conferred a higher relative risk of stroke in women (multivariable HR, 3.65; 95% CI, 2.91–4.58) than in men (multivariable HR, 1.97; 95% CI, 1.55–2.49). A similar pattern was seen for the association between AF and PE, with an overall HR for PE after AF diagnosis of 3.26 (95% CI, 1.97–5.42) in women and 1.91 (95% CI, 1.11–3.31) in men (Table 3). When stratified by type of AF (paroxysmal/persistent versus permanent forms), permanent AF was associated with a slightly higher risk of both PE (multivariable HR, 2.69; 95% CI, 1.68–4.32) and IS (multivariable HR, 3.14; 95% CI, 2.54–3.89) than paroxysmal/persistent AF (multivariable HR for PE, 1.92 [95% CI, 1.09–3.40]; multivariable HR for IS, 2.31 [95% CI, 1.80–2.96]) (data not shown).
Table 3.
Crude IRs and HRs for PE and IS in Men and Women Developing AF During Follow‐Up Compared With Subjects Without AF
| Variable | Person‐Years | Events | Crude IR (95% CI)a | HR (95% CI) | |
|---|---|---|---|---|---|
| Model 1b | Model 2c | ||||
| PE | |||||
| Men | |||||
| No AF | 184 172 | 118 | 0.64 (0.53–0.77) | Reference | Reference |
| 4541 | 16 | 3.52 (2.16–5.75) | 1.98 (1.15–3.41) | 1.91 (1.11–3.31) | |
| Women | |||||
| No AF | 213 212 | 121 | 0.57 (0.47–0.68) | Reference | Reference |
| 3310 | 20 | 6.04 (3.90–9.36) | 3.33 (2.02–5.52) | 3.26 (1.97–5.42) | |
| IS | |||||
| Men | |||||
| No AF | 184 172 | 545 | 2.96 (2.72–3.22) | Reference | Reference |
| 4541 | 91 | 20.04 (16.32–24.61) | 2.10 (1.67–2.64) | 1.96 (1.55–2.48) | |
| Women | |||||
| No AF | 213 212 | 397 | 1.86 (1.69–2.05) | Reference | Reference |
| 3310 | 107 | 32.32 (26.74–39.07) | 3.89 (3.11–4.87) | 3.65 (2.90–4.58) | |
AF indicates atrial fibrillation; CI, confidence interval; HR, hazard ratio; IR, incidence rate; IS, ischemic stroke; and PE, pulmonary embolism.
Per 1000 person‐years.
Using age as time scale.
Using age as time scale and adjusted for body mass index, smoking, total cholesterol, hypertension, and history of myocardial infarction and diabetes mellitus.
In total, 381 participants experienced AF only within 28 days after cardiac surgery or MI or in the last 7 days of life. In sensitivity analyses in which these cases were excluded, the overall risk estimates were barely altered (multivariable HRs, 11.14 [95% CI, 6.28–19.77] for PE and 5.57 [95% CI, 3.92–7.92] for IS in the first 6 months after AF diagnosis) (data not shown).
Discussion
In cause‐specific analyses, we found that subjects with AF had increased risk for both PE and IS. For PE, the incidence rate and relative risk were especially high during the first 6 months after onset of AF and remained elevated throughout the entire follow‐up. The risk estimates for PE by AF were essentially unchanged after adjustment for potential confounders, such as age, sex, BMI, atherosclerotic risk factors, and cardiovascular disease. A similar risk pattern was observed for the association between AF and IS. In sex‐stratified analyses, women had a higher risk of thromboembolic complications than men. The population attributable risk of PE and IS by incident AF was 12% and 16%, respectively.
Apart from our previous publication from the Tromsø study,11 only a few population‐based studies have investigated the temporal relationship between AF and PE. In accordance with our findings, Sørensen and coworkers found a substantially higher prevalence of AF in subjects with PE compared with population controls in a registry‐based study from Denmark.23 Similarly, an increased incidence and relative risk of PE by AF after multivariable adjustments were reported from a large registry‐based cohort study from Taiwan.12 The explanations for the observed association between AF and future risk of PE may include shared risk factors, indirect conditions, or a direct relationship.
Current evidence argues against shared risk factors as major contributors to the association between AF and PE. First, shared risk factors are expected to induce a permanent, and not a short‐term, high risk of PE, as observed in our study. Second, previous studies have shown that cardiovascular risk factors, except for age and BMI, are not associated with VTE.20, 24 Adjustments for potentially shared cardiovascular risk factors did not affect the PE risk by AF in our study.
Compelling evidence infers that the apparent risk of PE by AF could be explained by intermediate development of IS. Clinical and observational studies, including this study, have shown that AF is associated with risk of IS2, 25, 26 and that patients with IS are at a high risk for venous thrombosis.13, 14, 27 In a recent publication from our research group, we showed that subjects who developed IS had a transient increased risk of VTE, and DVT in particular, compared with those without IS, with a preponderance of immobility and concurrent medical conditions as predisposing factors for VTE in patients with stroke.13 In the present study, participants were censored at their first thromboembolic event (PE or IS), thereby eliminating stroke as a possible mediator of PE risk. Furthermore, the difference in phenotypic presentation of venous thrombosis by IS (predominance of DVT27) and AF (predominance of PE11, 23) supports the notion that the PE risk is not mediated by IS in patients with AF. Therefore, our finding of a cause‐specific association between AF and PE risk supports the hypothesis that the association is related to the AF itself (eg, that right‐sided intracardiac thrombi may embolize to the pulmonary circulation).
In accordance with previous findings,28, 29 we found women with AF to be at a higher overall risk of stroke than men. AF was also a stronger risk factor for PE in women than in men. Similar results were recently reported in a large registry‐based study, in which the excess PE risk conferred by AF was significantly higher in women.12 Several explanatory mechanisms have been proposed for the apparent increased thromboembolic risk in women with AF. A recent review article proposed that hormone replacement therapy, postmenopausal changes in endogenous estrogen levels, or sex differences in cardiac remodeling, hemodynamics, and procoagulant activity could be possible explanations.29 In addition, there are studies suggesting that women with AF receive suboptimal anticoagulation and poorer preventive treatment of cardiovascular risk factors compared with men.30 In clinical practice, the increased risk of thromboembolism in women with AF has been acknowledged by the inclusion of female sex as an independent risk factor in the CHA2DS2‐VASc score,31 the preferred stroke risk‐stratification scheme in patients with AF.2 To date, the clinical utility of the CHA2DS2‐VASc score for PE prediction has only been assessed in one registry‐based study with limited follow‐up.32 In this study, the PE risk was directly associated with the severity of the CHA2DS2‐VASc score, and the scoring scheme had similar prediction for PE and IS.32
The main strengths of our study include the prospective design, the large number of participants recruited from a general population, and a thorough validation scheme for both exposure and outcomes. In addition, the cause‐specific hazards model eliminates the effect of IS on PE risk and vice versa. Some limitations also warrant attention. In the multivariable models in the present study, some subgroup analyses have few events per number of independent predictor variables, rendering less certain estimates, as echoed by the wide CIs. We may further underestimate the true incidence of AF in our study population, because many episodes of AF are asymptomatic.33 Also, potential AF cases were derived from a discharge diagnosis registry and the Norwegian Cause of Death Registry; thus, patients with AT solely treated in general practice would have been missed. It is also possible that the observed association between AF and PE is confounded by concurrent development of other conditions during follow‐up, such as heart failure and chronic kidney disease. In the present study, we found PE risk to be particularly high during the first 6 months after AF, and it disappeared 3 years after AF onset. Concomitant conditions, such as hospitalizations and/or other comorbidities, may contribute to the excessive PE risk observed during this time period. Obstructive sleep apnea may trigger intravascular clot formation and is associated with both AF34 and VTE.35 Unfortunately, obstructive sleep apnea data were not collected in the Tromsø study. Other potential confounders, such as BMI, were measured at baseline only and may have changed over time. Nevertheless, previous estimates for VTE by cardiovascular risk factors based on baseline measures and time‐fixed analysis corresponded well with risk estimates based on repeated measurements and time‐varying analyses.36 Furthermore, comparison within the same population ensures that the degree of confounding is similar for both outcomes. Regrettably, we did not have individual information on the use of anticoagulants in participants with AF. In a previous study from our hospital, 70% of patients discharged with a diagnosis of chronic AF were treated with oral anticoagulants and 20% were treated with platelet inhibitors.37 Similar figures were recently reported from western European countries, including Norway, in a recently published registry‐based study.38 Because anticoagulant treatment efficiently reduces the risk of VTE,39 it is likely that our findings underestimate the true risk of thromboembolic complications in participants with AF.
In conclusion, the association between AF and future risk of PE could not be explained by intermediate development of IS. Our findings suggest that mechanisms and conditions related to AF itself may partly explain the increased risk of PE.
Sources of Funding
K. G. Jebsen Thrombosis Research and Expertise Center is supported by an independent grant from the K. G. Jebsen Foundation. The publication charges for this article have been funded by a grant from the publication fund of UiT The Arctic University of Norway.
Disclosures
None.
(J Am Heart Assoc. 2018;7:e006502 DOI: 10.1161/JAHA.117.006502.)29378729
References
- 1. Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, Agewall S, Camm J, Baron Esquivias G, Budts W, Carerj S, Casselman F, Coca A, De Caterina R, Deftereos S, Dobrev D, Ferro JM, Filippatos G, Fitzsimons D, Gorenek B, Guenoun M, Hohnloser SH, Kolh P, Lip GY, Manolis A, McMurray J, Ponikowski P, Rosenhek R, Ruschitzka F, Savelieva I, Sharma S, Suwalski P, Tamargo JL, Taylor CJ, Van Gelder IC, Voors AA, Windecker S, Zamorano JL, Zeppenfeld K. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016;18:1609–1678. [DOI] [PubMed] [Google Scholar]
- 3. Savelieva I, Bajpai A, Camm AJ. Stroke in atrial fibrillation: update on pathophysiology, new antithrombotic therapies, and evolution of procedures and devices. Ann Med. 2007;39:371–391. [DOI] [PubMed] [Google Scholar]
- 4. Carmichael AJ, Martin AM. Pulmonary embolism: a complication of right atrial thrombi due to atrial fibrillation. J R Soc Med. 1991;84:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aberg H. Atrial fibrillation, I: a study of atrial thrombosis and systemic embolism in a necropsy material. Acta Med Scand. 1969;185:373–379. [PubMed] [Google Scholar]
- 6. van Langevelde K, Sramek A, Vincken PW, van Rooden JK, Rosendaal FR, Cannegieter SC. Finding the origin of pulmonary emboli with a total‐body magnetic resonance direct thrombus imaging technique. Haematologica. 2013;98:309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Girard P, Sanchez O, Leroyer C, Musset D, Meyer G, Stern JB, Parent F; Evaulation du Scanner Spiralé dans l'Embolie Pulmonaire Study Group . Deep venous thrombosis in patients with acute pulmonary embolism: prevalence, risk factors, and clinical significance. Chest. 2005;128:1593–1600. [DOI] [PubMed] [Google Scholar]
- 8. Koracevic G, Atanaskovic V. Is atrial fibrillation a prognosticator in acute pulmonary thromboembolism? Med Princ Pract. 2010;19:166. [DOI] [PubMed] [Google Scholar]
- 9. Barra SN, Paiva LV, Providencia R, Fernandes A, Leitao Marques A. Atrial fibrillation in acute pulmonary embolism: prognostic considerations. Emerg Med J. 2014;31:308–312. [DOI] [PubMed] [Google Scholar]
- 10. Kukla P, Dlugopolski R, Krupa E, Furtak R, Szelemej R, Mirek‐Bryniarska E, Jastrzebski M, Nowak J, Wanczura P, Bryniarski L. Electrocardiography and prognosis of patients with acute pulmonary embolism. Cardiol J. 2011;18:648–653. [DOI] [PubMed] [Google Scholar]
- 11. Enga KF, Rye‐Holmboe I, Hald EM, Lochen ML, Mathiesen EB, Njolstad I, Wilsgaard T, Braekkan SK, Hansen JB. Atrial fibrillation and future risk of venous thromboembolism: the Tromso Study. J Thromb Haemost. 2015;13:10–16. [DOI] [PubMed] [Google Scholar]
- 12. Wang CC, Lin CL, Wang GJ, Chang CT, Sung FC, Kao CH. Atrial fibrillation associated with increased risk of venous thromboembolism: a population‐based cohort study. Thromb Haemost. 2015;113:185–192. [DOI] [PubMed] [Google Scholar]
- 13. Rinde LB, Smabrekke B, Mathiesen EB, Lochen ML, Njolstad I, Hald EM, Wilsgaard T, Braekkan SK, Hansen JB. Ischemic stroke and risk of venous thromboembolism in the general population: the Tromso Study. J Am Heart Assoc. 2016;5:e004311 DOI: 10.1161/JAHA.116.004311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kelly J, Rudd A, Lewis R, Hunt BJ. Venous thromboembolism after acute stroke. Stroke. 2001;32:262–267. [DOI] [PubMed] [Google Scholar]
- 15. Sorensen HT, Horvath‐Puho E, Sogaard KK, Christensen S, Johnsen SP, Thomsen RW, Prandoni P, Baron JA. Arterial cardiovascular events, statins, low‐dose aspirin and subsequent risk of venous thromboembolism: a population‐based case‐control study. J Thromb Haemost. 2009;7:521–528. [DOI] [PubMed] [Google Scholar]
- 16. Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, Carolei A. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population‐based study. Stroke. 2005;36:1115–1119. [DOI] [PubMed] [Google Scholar]
- 17. Davenport RJ, Dennis MS, Wellwood I, Warlow CP. Complications after acute stroke. Stroke. 1996;27:415–420. [DOI] [PubMed] [Google Scholar]
- 18. Eggen AE, Mathiesen EB, Wilsgaard T, Jacobsen BK, Njolstad I. The sixth survey of the Tromso Study (Tromso 6) in 2007–08: collaborative research in the interface between clinical medicine and epidemiology: study objectives, design, data collection procedures, and attendance in a multipurpose population‐based health survey. Scand J Public Health. 2013;41:65–80. [DOI] [PubMed] [Google Scholar]
- 19. Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njolstad I. Cohort profile: the Tromso Study. Int J Epidemiol. 2012;41:961–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Braekkan SK, Hald EM, Mathiesen EB, Njolstad I, Wilsgaard T, Rosendaal FR, Hansen JB. Competing risk of atherosclerotic risk factors for arterial and venous thrombosis in a general population: the Tromso Study. Arterioscler Thromb Vasc Biol. 2012;32:487–491. [DOI] [PubMed] [Google Scholar]
- 21. Braekkan SK, Borch KH, Mathiesen EB, Njolstad I, Wilsgaard T, Hansen JB. Body height and risk of venous thromboembolism: the Tromso Study. Am J Epidemiol. 2010;171:1109–1115. [DOI] [PubMed] [Google Scholar]
- 22. WHO MONICA Project Principal Investigators. The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. J Clin Epidemiol. 1988;41:105–114. [DOI] [PubMed] [Google Scholar]
- 23. Sørensen HT, Horvath‐Puho E, Lash TL, Christiansen CF, Pesavento R, Pedersen L, Baron JA, Prandoni P. Heart disease may be a risk factor for pulmonary embolism without peripheral deep venous thrombosis. Circulation. 2011;124:1435–1441. [DOI] [PubMed] [Google Scholar]
- 24. Mahmoodi BK, Cushman M, Anne Naess I, Allison MA, Jan Bos W, Braekkan SK, Cannegieter SC, Gansevoort RT, Gona PN, Hammerstrom J, Hansen JB, Heckbert S, Holst AG, Lakoski SG, Lutsey PL, Manson JE, Martin LW, Matsushita K, Meijer K, Overvad K, Prescott E, Puurunen M, Rossouw JE, Sang Y, Severinsen MT, Ten Berg J, Folsom AR, Zakai NA. Association of traditional cardiovascular risk factors with venous thromboembolism: an individual participant data meta‐analysis of prospective studies. Circulation. 2017;135:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Christiansen CB, Gerds TA, Olesen JB, Kristensen SL, Lamberts M, Lip GY, Gislason GH, Kober L, Torp‐Pedersen C. Atrial fibrillation and risk of stroke: a nationwide cohort study. Europace. 2016;18:1689–1697. [DOI] [PubMed] [Google Scholar]
- 26. Bjorck S, Palaszewski B, Friberg L, Bergfeldt L. Atrial fibrillation, stroke risk, and warfarin therapy revisited: a population‐based study. Stroke. 2013;44:3103–3108. [DOI] [PubMed] [Google Scholar]
- 27. Kamphuisen PW, Agnelli G. What is the optimal pharmacological prophylaxis for the prevention of deep‐vein thrombosis and pulmonary embolism in patients with acute ischemic stroke? Thromb Res. 2007;119:265–274. [DOI] [PubMed] [Google Scholar]
- 28. Fang MC, Singer DE, Chang Y, Hylek EM, Henault LE, Jensvold NG, Go AS. Gender differences in the risk of ischemic stroke and peripheral embolism in atrial fibrillation: the AnTicoagulation and Risk factors In Atrial fibrillation (ATRIA) study. Circulation. 2005;112:1687–1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cove CL, Albert CM, Andreotti F, Badimon L, Van Gelder IC, Hylek EM. Female sex as an independent risk factor for stroke in atrial fibrillation: possible mechanisms. Thromb Haemost. 2014;111:385–391. [DOI] [PubMed] [Google Scholar]
- 30. Glader EL, Stegmayr B, Norrving B, Terent A, Hulter‐Asberg K, Wester PO, Asplund K, Riks‐Stroke C. Sex differences in management and outcome after stroke: a Swedish national perspective. Stroke. 2003;34:1970–1975. [DOI] [PubMed] [Google Scholar]
- 31. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor‐based approach: the Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–272. [DOI] [PubMed] [Google Scholar]
- 32. Saliba W, Rennert G. CHA2DS2‐VASc score is directly associated with the risk of pulmonary embolism in patients with atrial fibrillation. Am J Med. 2014;127:45–52. [DOI] [PubMed] [Google Scholar]
- 33. Savelieva I, Camm AJ. Clinical relevance of silent atrial fibrillation: prevalence, prognosis, quality of life, and management. J Interv Card Electrophysiol. 2000;4:369–382. [DOI] [PubMed] [Google Scholar]
- 34. Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, Malouf JF, Ammash NM, Friedman PA, Somers VK. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–367. [DOI] [PubMed] [Google Scholar]
- 35. Arzt M, Luigart R, Schum C, Luthje L, Stein A, Koper I, Hecker C, Dumitrascu R, Schulz R; “Circulation and Sleep” working group of the German Society of Sleep Research and Sleep Medicine (DGSM) . Sleep‐disordered breathing in deep vein thrombosis and acute pulmonary embolism. Eur Respir J. 2012;40:919–924. [DOI] [PubMed] [Google Scholar]
- 36. Smabrekke B, Rinde LB, Hindberg K, Hald EM, Vik A, Wilsgaard T, Lochen ML, Njolstad I, Mathiesen EB, Hansen JB, Braekkan S. Atherosclerotic risk factors and risk of myocardial infarction and venous thromboembolism; time‐fixed versus time‐varying analyses: the Tromso Study. PLoS One. 2016;11:e0163242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Thomassen G, Hansen MS, Nordoy A, Hansen JB. Antithrombotic treatment of atrial fibrillation in hospital [in Norwegian]. Tidsskr Nor Laegeforen. 2001;121:2800–2804. [PubMed] [Google Scholar]
- 38. Lip GY, Laroche C, Boriani G, Dan GA, Santini M, Kalarus Z, Rasmussen LH, Oliveira MM, Mairesse G, Crijns HJ, Simantirakis E, Atar D, Maggioni AP, Tavazzi L. Regional differences in presentation and treatment of patients with atrial fibrillation in Europe: a report from the EURObservational Research Programme Atrial Fibrillation (EORP‐AF) Pilot General Registry. Europace. 2015;17:194–206. [DOI] [PubMed] [Google Scholar]
- 39. Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence‐Based Clinical Practice Guidelines. Chest. 2012;141:e419S–e494S. [DOI] [PMC free article] [PubMed] [Google Scholar]


