Abstract
Antimicrobial resistance in gram-positive bacteria remains a challenge in infectious diseases. The mission of the Gram-Positive Committee of the Antibacterial Resistance Leadership Group (ARLG) is to advance knowledge in the prevention, management, and treatment of these challenging infections to improve patient outcomes. Our committee has prioritized projects involving methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) due to the scope of the medical threat posed by these pathogens. Approved ARLG projects involving gram-positive pathogens include (1) a pharmacokinetics/pharmacodynamics study to evaluate the impact of vancomycin dosing on patient outcome in MRSA bloodstream infection (BSI); (2) defining, testing, and validating innovative assessments of patient outcomes for clinical trials of MRSA-BSI; (3) testing new strategies for “step-down” antibiotic therapy for MRSA-BSI; (4) management of staphylococcal BSIs in neonatal intensive care units; and (5) defining the impact of VRE bacteremia and daptomycin susceptibility on patient outcomes. This article outlines accomplishments, priorities, and challenges for research of infections caused by gram-positive organisms.
Keywords: gram-positive bacteria, bloodstream infection, Staphylococcus aureus, vancomycin-resistant enterococci, Clostridium difficile infection.
Infections caused by gram-positive bacteria such as methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), and Clostridium difficile are among the most common multidrug-resistant infections in the United States [1]. Despite their frequency, few data exist to inform best management practices for these infections. For example, there has been only one high-quality randomized controlled trial comparing S. aureus bloodstream infection (SA-BSI) treatment strategies [2], and there are only 2 US Food and Drug Administration (FDA)–approved antibiotics for the treatment of MRSA bacteremia and endocarditis [3]. Similarly, VRE infections are increasingly common, particularly in cancer and organ transplant patients; however, treatment options are limited. There is only one FDA-approved antibiotic for VRE infections, and the optimal management strategy is unknown [4]. In addition, C. difficile now accounts for almost half a million infections and tens of thousands of deaths annually, mostly in elderly and hospitalized individuals [5]. Since the Antibacterial Resistance Leadership Group’s (ARLG) inception, addressing unmet needs in gram-positive infections has been one of 4 main areas of major emphasis [6]. This article summarizes accomplishments to date, research priorities and unmet needs, ongoing studies, and planned studies related to gram-positive infections conducted by the ARLG.
COMPLETED AND ACTIVE STUDIES
Study of Vancomycin Pharmacodynamics
Vancomycin has been used for more than half a century for the treatment of serious staphylococcal infections, but the optimal dosing strategy is unknown [7]. The relationship between vancomycin exposure and outcomes has been evaluated in several retrospective cohort studies of adults with MRSA bacteremia [8–10]. While these evaluations suggest that the vancomycin area under the curve (AUC)/minimum inhibitory concentration (MIC) ratio is the best pharmacokinetic/pharmacodynamic (PK/PD) predictor for outcome, these studies have relied on calculations derived from a simple formula for daily vancomycin dose and predicted renal function to estimate AUC values. Projections of exposure variables in a given individual based on glomerular filtration estimation formulas alone have inherent inaccuracies [11]. The ARLG Pharmacokinetic Special Emphasis Panel Chair, in collaboration with the ARLG Gram-Positive Committee and the Statistical and Data Management Center (SDMC) [12] and Leadership and Operations Center (LOC) [13], has therefore designed and undertaken PROVIDE (Prospective Validation of the Vancomycin Exposure Profile Associated With Optimal Outcomes Among Patients With MRSA Bloodstream Infections) to determine whether vancomycin AUC/MIC is related to patient outcome in MRSA bacteremia. A validated Bayesian method will be used to estimate the vancomycin exposure profile with limited vancomycin plasma concentration data to identify the pharmacodynamic index that is most closely linked to clinical outcomes early in therapy. Determination of the vancomycin exposure effect link has the potential to transform clinical practice by altering dosing standards. Enrollment of 310 subjects is complete, and results will be available in 2017.
Staphylococcus aureus Bloodstream Infection
Current treatment approaches for SA-BSI, particularly related to MRSA, are mainly based on expert opinion and small, observational or nonrandomized studies [3]. Existing guidelines call for prolonged courses of intravenous antibiotics and little evidence exists to support alternative treatment strategies or shorter duration of therapy [14–18]. This lack of data stems in part from the difficulty in designing and executing high-quality trials for SA-BSI and is constrained by often impractically large sample sizes required to answer therapeutic questions [19, 20]. Historically, noninferiority designs have been used to support new treatment approaches, but this trial design cannot fully answer the question of which treatment strategy is better in a global sense.
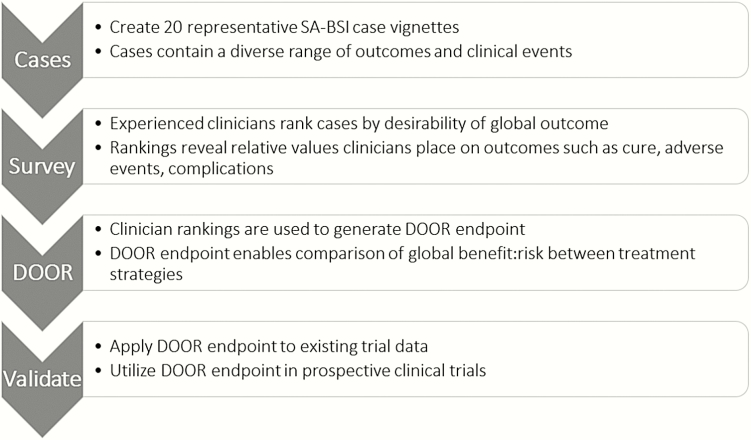
In a recent ARLG study, the ARLG SDMC and colleagues described an approach to outcome determination that aims to better achieve systematic benefit-risk assessment of the complete patient experience rather than one specific endpoint [21]. Termed desirability of outcome ranking (DOOR), this approach uses expert opinions to help prioritize and weigh specific outcomes and can be tailored for the disease and the treatment, taking into account factors such as mortality, cure, side effects, complications, and quality of life (QOL). DOOR-associated outcomes are ordinal, rather than dichotomous, which allows smaller samples for clinical trials.
Another project, STAMP (Staphylococcus aureus Management Approaches), in collaboration with the ARLG SDMC and LOC, aims to develop, design, and execute trials of treatment strategies, particularly for SA-BSI. The goals of STAMP are to (1) develop a DOOR endpoint for treatment trials for SA-BSI; (2) validate the DOOR endpoint using prior trial data; (3) generate a QOL scale to be incorporated into a future DOOR endpoint; and (4) design and execute a trial of step-down therapy for SA-BSI. To develop a DOOR endpoint for use in future trials, SA-BSI case vignettes were presented to a group of 43 infectious diseases physicians from the ARLG committees, who ranked the cases for global outcome. Results from this ranking exercise were used to generate a DOOR endpoint (Figure 1) [22]. This DOOR endpoint will be validated with data from completed trials in SA-BSI. Additionally, the STAMP group is prospectively developing and validating a QOL tool that can be used in future trials of SA-BSI treatment approaches to better evaluate patient-centered outcomes. The goal for all of the studies described above is to develop novel approaches to assess complex outcomes, which will be ultimately used in a future strategy trial for SA-BSI.
Figure 1.
Process to generate and implement a desirability of outcome ranking (DOOR) endpoint for Staphylococcus aureus bloodstream infection (SA-BSI) studies.
To determine whether it is safe and effective to shorten the duration of daily intravenous therapy for SA-BSI, the ARLG Gram-Positive Committee and SDMC are designing a randomized clinical trial comparing traditional treatment approaches vs initial traditional therapy followed by step-down therapy for patients with SA-BSI. Potential step-down comparator approaches include newer long-acting intravenous MRSA agents as well as oral agents active against S. aureus. Possible advantages of early step-down therapy include decreasing duration of peripherally inserted central catheter line placement with attendant complications, reducing need for prolonged hospitalization or home health services, improving patient convenience and QOL, and reducing antibiotic-associated adverse events [23]. This proposed study will contribute significantly to the limited literature on SA-BSI management and will set a precedent for use of DOOR to gain a more nuanced view of the global benefits and risks of novel treatment approaches.
Staphylococcal Bacteremia in Neonates
Gram-positive BSIs cause significant morbidity and mortality among infants in neonatal intensive care units (NICUs) [24–26]. Little is known about the impact of early adequate empiric antibiotic therapy in this patient population. To address this unmet need, the ARLG collaborated with the Pediatric Trials Network to utilize information from a large cohort of infants with S. aureus [27] or coagulase-negative staphylococcal [28] BSI discharged from 348 NICUs from 1997 to 2012. Thaden et al identified 3339 infants with SA-BSI, one-quarter of which were MRSA BSI [27]; 78% received early adequate empiric antibiotic therapy. In multivariable analysis, 30-day mortality was higher for infants with MRSA BSI who received inadequate empiric antibiotic therapy (odds ratio [OR], 2.03 [95% confidence interval {CI}, 1.08–3.82]). Among infants with methicillin-susceptible S. aureus BSI, there was no association between inadequate antibiotic therapy and 30-day mortality (OR, 0.52 [95% CI, .26–1.06]). In the other analysis, Ericson et al identified 4364 infants with coagulase-negative Staphylococcus BSI, 65% of which were treated with empiric vancomycin [28]. In multivariable analysis, empiric vancomycin therapy was not associated with 30-day mortality (OR, 1.14 [95% CI, .84–1.56]). However, the median (interquartile range) duration of bacteremia was a day longer for infants with delayed vancomycin therapy (4 days [2–6 days] vs 3 days [2–5 days]; P < .0001). Together, these studies help to elucidate the role for empiric vancomycin in the neonatal population.
Defining Optimal Treatment for VRE BSIs
Invasive VRE infection is a potentially life-threatening complication in severely ill and immunocompromised patients, particularly those with hematological malignancies [29]. Therapy for these infections is challenging due to the paucity of reliable therapeutic options and because optimal treatment strategies are not defined [30–33]. One area of uncertainty is the use of daptomycin to treat patients with VRE BSI who have daptomycin MICs close to the established susceptibility breakpoint (4 μg/mL), as these organisms frequently harbor mutations associated with daptomycin resistance and tolerance and are most likely to fail daptomycin therapy [34, 35].
To evaluate clinical outcomes of cancer patients with vancomycin-resistant Enterococcus faecium (VREF) BSI treated with daptomycin, ARLG investigators are assembling a multicenter prospective cohort of patients with hematologic malignancies and/or stem-cell transplants who have VREF BSI and are treated with daptomycin from 2 large academic cancer centers in the United States. The main objective of this study is to evaluate the impact of daptomycin MIC of the baseline infecting pathogen on clinical outcomes. This initial effort, funded via an ARLG early stage investigator seed grant (designed to allow researchers to generate preliminary data leading to additional external funding), and supported by the ARLG Mentoring Committee, will serve as a platform for future interventional trials to test novel therapeutic strategies that provide valuable clinical data to define the best approach to treat deep-seated VRE infections. The study is expected to begin in late 2016 or early 2017.
Unmet Needs and Opportunities
Gram-positive organisms comprise 7 of the 18 urgent, serious, or concerning drug-resistance threats outlined by the US Centers for Disease Control and Prevention in 2013 [36]. Together, these organisms—including C. difficile, MRSA, and VRE—are estimated to cause more than 1.3 million infections and 34000 deaths in the United States every year at a cost of billions of dollars annually. There remain many unanswered questions regarding each of these critical gram-positive threats, and the ARLG Gram-Positive Committee has identified multiple areas of research that are of particular urgency and are priorities for future investigations (Table 1). Despite consensus about priorities, significant barriers to trial feasibility have hampered progress to date. Thus, investigations of these and related questions will leverage the ARLG’s existing structure of clinical trial expertise, innovative approaches to trial design, and engagement with both public and private sectors to advance knowledge of how best to identify, prevent, and treat these threats. To date, our studies in the gram-positive realm have focused on staphylococcal and enterococcal infections, but C. difficile remains a major gram-positive priority for the ARLG to investigate in upcoming studies.
Table 1.
Antibacterial Resistance Leadership Group Studies Addressing Unmet Needs in Gram-Positive Bacterial Infections
| Study | Description | Status |
|---|---|---|
| PROVIDE (Prospective Validation of the Vancomycin Exposure Profile Associated With Optimal Outcomes Among Patients With MRSA Bloodstream Infections) |
Prospective observational study to assess the impact of vancomycin exposure profile on outcomes of patients with MRSA BSI | Completed |
| STAMP (Staphylococcus aureus Management Approaches), others |
Clinician ranking exercise to develop a DOOR endpoint for use in SA-BSI treatment trials | Completed |
| Analysis of previous SA-BSI trials using DOOR endpoint | Ongoing | |
| Development and validation of a quality-of-life tool for SA-BSI trials | Ongoing | |
| Randomized trial comparing step-down therapy strategy to standard of care for SA-BSI | Planning | |
| Neonatal ICU cohort | Analysis of impact of adequate empiric antibiotic therapy on outcomes in neonatal staphylococcal BSI | Completed |
| VRE BSI (seed grant) |
Multicenter prospective cohort of hematological malignancy and/ or stem-cell transplant patients with VRE BSI treated with daptomycin | Planning |
Abbreviations: BSI, bloodstream infection; DOOR, desirability of outcome ranking; ICU, intensive care unit; MRSA, methicillin-resistant Staphylococcus aureus; SA, Staphylococcus aureus; VRE, vancomycin-resistant enterococci.
For example, 2 previous industry-funded phase 3 studies of VRE BSI were aborted due to poor enrollment [37, 38]. Optimal treatment strategies for this infection remain uncertain, and an interventional trial comparing treatments for VRE BSI would help shed light on best treatment. Such a trial would build upon knowledge gained from the study described above. Potential innovative strategies that could be applied to this hypothetical trial include adaptive design to identify the best therapy for VRE infection (eg, daptomycin, linezolid, combination therapy), the best dosage of daptomycin for groups with various MICs, and use of ordinal ranking methods to enable use of superiority design with the potential for smaller sample size than traditional trials. With multiple public–private partnerships, it would be possible to pair studies of VRE BSI using master protocols to address multiple questions simultaneously. In addition, the ARLG has developed a rich network of hospitals and medical centers that can be leveraged to maximize enrollment. Similar approaches could be used to address many of the questions outlined in Table 2.
Table 2.
Priorities and Opportunities for Gram-Positive Infections
| Unmet Need | Category |
|---|---|
| Topic: Staphylococci | |
| Prospective evaluation of strategies to diagnose MRSA colonization as a way to risk-stratify need for MRSA antibiotic therapy for common infectious syndromes | Diagnosis |
| Comparative efficacy, safety, and tolerability of oral antibiotics for invasive Staphylococcus aureus infections | Treatment |
| Defining the role of combination therapy with β-lactams for MRSA and methicillin-resistant CoNS BSIs | Treatment |
| Defining optimal management of persistent MRSA BSI | Treatment |
| Defining comparative efficacy and safety of intravenous agents other than vancomycin for MRSA and methicillin-resistant CoNS BSIs | Treatment |
| Defining the efficacy and safety of adjunctive therapies such as immunotherapeutics | Treatment |
| Adequacy of oral vs parenteral therapy for osteomyelitis | Treatment |
| Safety and efficacy of step-down therapy for osteomyelitis | Treatment |
| Comparative efficacy and safety of regimens with and without adjunctive rifampin for vertebral osteomyelitis | Treatment |
| Topic: Enterococci | |
| Approaches to prevention of VRE colonization and infection | Prevention |
| Defining subgroups of patients who are at high risk of failing a particular therapy | Diagnosis |
| Comparative efficacy and safety of linezolid vs daptomycin for VRE BSI | Treatment |
| Role of combination therapy with β-lactams for enterococcal BSI and osteomyelitis | Treatment |
| Role of combination therapy with β-lactams against VRE | Treatment |
| Defining the optimal length of therapy for VRE BSI | Treatment |
| Optimal therapy for VRE endocarditis | Treatment |
| Optimal therapy for VRE with high daptomycin MIC | Treatment |
| Topic: Clostridium difficile infection | |
| Impact of testing approaches on rates of infection and individual outcomes | Diagnosis |
| Development and impact of ultra-sensitive toxin-detection tests | Diagnosis |
| Better elucidation of complex relationships in the inpatient and outpatient setting contributing to CDI | Prevention |
| Microbiome-related strategies for secondary prevention of CDI | Prevention |
| Vaccine development | Prevention |
| Microbiome-related strategies for secondary prevention of CDI | Prevention |
| Microbiome-related strategies for treatment of mild, moderate, and severe CDI | Treatment |
| Colon-sparing surgical approaches for management of severe/complicated CDI | Treatment |
| Topic: New gram-positive antibiotics | |
| Dosing, efficacy, safety, and impact on resistance of oritavancin and dalbavancin for follow-on therapy for resistant infections | Treatment |
| Safety and efficacy of tedizolid for longer-term use | Treatment |
| Topic: Group A Streptococcus | |
| Efficacy of intravenous immunoglobulin for treatment of severe, invasive infections | Treatment |
Abbreviations: BSI, bloodstream infection; CDI, Clostridium difficile infection; CoNS, coagulase-negative staphylococci; MIC, minimum inhibitory concentration; MRSA, methicillin-resistant Staphylococcus aureus; VRE, vancomycin-resistant enterococci.
In conclusion, since its establishment, the ARLG Gram-Positive Committee has addressed certain key questions related to MRSA and VRE infections, and we will continue to evaluate and execute studies related to gram-positive priorities with the goals of improving individual and population outcomes.
Notes
ARLG Gram-Positive Committee. Cesar Arias, MD, PhD; Helen Boucher, MD; Ralph Corey, MD; Sara Cosgrove, MD, MS; Sarah Doernberg, MD, MAS; George Eliopoulos, MD*; Scott Evans, PhD; Thomas L. Holland, MD; Frank Lowy, MD; Loren Miller, MD, MPH; Barbara Murray, MD; David Snydman, MD [*former member].
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health (NIH).
Financial support. This article was supported by the National Institute of Allergy and Infectious Diseases of the NIH (award number UM1AI104681).
Supplement sponsorship. This article appears as part of the supplement "Antibacterial Resistance Leadership Group (ARLG): Productivity and Innovation," sponsored by the Antibacterial Resistance Leadership Group.
Potential conflicts of interest. S. B. D. has received research funding from Merck, Genentech, Cerexa, and Cubist Pharmaceuticals and has served as a consultant for Genentech. T. P. L. has received grant support from ARLG, which funded the PROVIDE study; has been a consultant for Allergen, The Medicines Company, Merck, and Theravance; has received payment for lectures, including speakers bureaus, for Allergen and The Medicines Company; and has received contracts from Merck. S. E. C. has consulted for Novartis and Theravance and has received grants from Pfizer Grants for Learning and Change/The Joint Commission. C. A. A. has served on the speaker bureau for Allergan, Pfizer, Merck, and the Medicines Company; has received grants from Allergan, Pfizer, Theravance, Merck, and The Medicines Company, and has served on the advisory board for Theravance, Merck, The Medicines Company, and Bayer Global. H. W. B. has served on the data monitoring committee for Actelion and Cardeas and the Adjudication Committee for the NIH. G. R. C. serves on the scientific advisory boards for Nabriva, Medtronic, Cerexa/Forest/Actavis, Merck, Achaogen, Melinta, Tetraphase, Arsanis, Contrafect, Paratek, and SCPharma; has participated in study design for Medtronic; has served as a consultant for The Medicines Company, Theravance, Melinta, Motif, Arsanis, Contrafect, Cowen Group, Paratek, Bayer, SCPharma, Basilea, and Cempra; and has served on a mortality board for Pfizer and adjudication committees for Bio2 Medical and Quintiles/Novella. F. D. L. has received royalties from UpToDate and has performed research for Theravance. B. M. has served on pharmaceutical advisory boards for Cempra and Paratek and as co-investigator on institutional grants for Merck, Theravance, and Actavis. L. G. M. has served as a consultant for Tetraphase and has received grants from Gilead Sciences, Achaogen, Merck, Abbott, and Cepheid. T. L. H. has served as a consultant for The Medicines Company and Basilea Pharmaceutica and has received royalties from UpToDate. J. T. T. reports no potential conflicts. The authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. Available at: http://www.cdc.gov/drugresistance/threat-report-2013/. Accessed 10 August 2016.
- 2. Fowler VG, Jr, Boucher HW, Corey GR, et al. ; Staphylococcus aureus Endocarditis and Bacteremia Study Group Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med 2006; 355:653–65. [DOI] [PubMed] [Google Scholar]
- 3. Holland TL, Arnold C, Fowler VG., Jr Clinical management of Staphylococcus aureus bacteremia: a review. JAMA 2014; 312:1330–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McKinnell JA, Arias CA. Editorial commentary: linezolid vs daptomycin for vancomycin-resistant enterococci: the evidence gap between trials and clinical experience. Clin Infect Dis 2015; 61:879–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lessa FC, Mu Y, Bamberg WM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med 2015; 372:825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chambers HF, Bartlett JG, Bonomo RA, et al. Antibacterial resistance leadership group: open for business. Clin Infect Dis 2014; 58:1571–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lodise TP, Drusano GL, Zasowski E, et al. Vancomycin exposure in patients with methicillin-resistant Staphylococcus aureus bloodstream infections: how much is enough? Clin Infect Dis 2014; 59:666–75. [DOI] [PubMed] [Google Scholar]
- 8. Moise-Broder PA, Forrest A, Birmingham MC, Schentag JJ. Pharmacodynamics of vancomycin and other antimicrobials in patients with Staphylococcus aureus lower respiratory tract infections. Clin Pharmacokinet 2004; 43:925–42. [DOI] [PubMed] [Google Scholar]
- 9. Kullar R, Leonard SN, Davis SL, et al. Validation of the effectiveness of a vancomycin nomogram in achieving target trough concentrations of 15–20 mg/L suggested by the vancomycin consensus guidelines. Pharmacotherapy 2011; 31:441–8. [DOI] [PubMed] [Google Scholar]
- 10. Holmes NE, Turnidge JD, Munckhof WJ, et al. Vancomycin AUC/MIC ratio and 30-day mortality in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 2013; 57:1654–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Patel N, Pai MP, Rodvold KA, Lomaestro B, Drusano GL, Lodise TP. Vancomycin: we can’t get there from here. Clin Infect Dis 2011; 52:969–74. [DOI] [PubMed] [Google Scholar]
- 12. Huvane J, Komarow L, Hill C, et al. Fundamentals and catalytic innovation: the Statistical and Data Management Center of the Antibacterial Resistance Leadership Group. Clin Infect Dis 2017; 64(Suppl 1):S18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cross HR, Harris A, Arias RM, et al. Transforming concepts into clinical trials and creating a multisite network: the Leadership and Operations Center of the Antibacterial Resistance Leadership Group. Clin Infect Dis 2017; 64(Suppl 1):S8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu C, Bayer A, Cosgrove SE, et al. ; Infectious Diseases Society of America Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011; 52:e18–55. [DOI] [PubMed] [Google Scholar]
- 15. Paul M, Bishara J, Yahav D, et al. Trimethoprim-sulfamethoxazole versus vancomycin for severe infections caused by meticillin resistant Staphylococcus aureus: randomised controlled trial. BMJ 2015; 350:h2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shorr AF, Kunkel MJ, Kollef M. Linezolid versus vancomycin for Staphylococcus aureus bacteraemia: pooled analysis of randomized studies. J Antimicrob Chemother 2005; 56:923–9. [DOI] [PubMed] [Google Scholar]
- 17. Heldman AW, Hartert TV, Ray SC, et al. Oral antibiotic treatment of right-sided staphylococcal endocarditis in injection drug users: prospective randomized comparison with parenteral therapy. Am J Med 1996; 101:68–76. [DOI] [PubMed] [Google Scholar]
- 18. Jernigan JA, Farr BM. Short-course therapy of catheter-related Staphylococcus aureus bacteremia: a meta-analysis. Ann Intern Med 1993; 119:304–11. [DOI] [PubMed] [Google Scholar]
- 19. DiNubile MJ. Noninferior antibiotics: when is “not bad” “good enough”? Open Forum Infect Dis 2016; 3:ofw110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Evans SR, Follmann D. Comment: fundamentals and innovation in antibiotic trials. Stat Biopharm Res 2015; 7:331–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Evans SR, Rubin D, Follmann D, et al. Desirability of outcome ranking (DOOR) and response adjusted for duration of antibiotic risk (RADAR). Clin Infect Dis 2015; 61:800–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Doernberg S, Gouskova N, Evans S, et al. BAC DOOR: a clinician ranking exercise for better S. aureus bacteremia trial design. In: IDWeek 2016. New Orleans, LA, 26–30 October 2016. [Google Scholar]
- 23. Chopra V, Anand S, Krein SL, Chenoweth C, Saint S. Bloodstream infection, venous thrombosis, and peripherally inserted central catheters: reappraising the evidence. Am J Med 2012; 125:733–41. [DOI] [PubMed] [Google Scholar]
- 24. Burke RE, Halpern MS, Baron EJ, Gutierrez K. Pediatric and neonatal Staphylococcus aureus bacteremia: epidemiology, risk factors, and outcome. Infect Control Hosp Epidemiol 2009; 30:636–44. [DOI] [PubMed] [Google Scholar]
- 25. Carey AJ, Duchon J, Della-Latta P, Saiman L. The epidemiology of methicillin-susceptible and methicillin-resistant Staphylococcus aureus in a neonatal intensive care unit, 2000–2007. J Perinatol 2010; 30:135–9. [DOI] [PubMed] [Google Scholar]
- 26. Marchant EA, Boyce GK, Sadarangani M, Lavoie PM. Neonatal sepsis due to coagulase-negative staphylococci. Clin Dev Immunol 2013; 2013:586076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thaden JT, Ericson JE, Cross H, et al. ; Antibacterial Resistance Leadership Group Survival benefit of empirical therapy for Staphylococcus aureus bloodstream infections in infants. Pediatr Infect Dis J 2015; 34:1175–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ericson JE, Thaden J, Cross HR, et al. ; Antibacterial Resistance Leadership Group No survival benefit with empirical vancomycin therapy for coagulase-negative staphylococcal bloodstream infections in infants. Pediatr Infect Dis J 2015; 34:371–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zirakzadeh A, Patel R. Vancomycin-resistant enterococci: colonization, infection, detection, and treatment. Mayo Clin Proc 2006; 81:529–36. [DOI] [PubMed] [Google Scholar]
- 30. Balli EP, Venetis CA, Miyakis S. Systematic review and meta-analysis of linezolid versus daptomycin for treatment of vancomycin-resistant enterococcal bacteremia. Antimicrob Agents Chemother 2014; 58:734–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Whang DW, Miller LG, Partain NM, McKinnell JA. Systematic review and meta-analysis of linezolid and daptomycin for treatment of vancomycin-resistant enterococcal bloodstream infections. Antimicrob Agents Chemother 2013; 57:5013–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chuang YC, Wang JT, Lin HY, Chang SC. Daptomycin versus linezolid for treatment of vancomycin-resistant enterococcal bacteremia: systematic review and meta-analysis. BMC Infect Dis 2014; 14:687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shukla BS, Shelburne S, Reyes K, et al. Influence of minimum inhibitory concentration in clinical outcomes of Enterococcus faecium bacteremia treated with daptomycin: is it time to change the breakpoint? Clin Infect Dis 2016; 62:1514–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Munita JM, Panesso D, Diaz L, et al. Correlation between mutations in liaFSR of Enterococcus faecium and MIC of daptomycin: revisiting daptomycin breakpoints. Antimicrob Agents Chemother 2012; 56:4354–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Munita JM, Mishra NN, Alvarez D, et al. Failure of high-dose daptomycin for bacteremia caused by daptomycin-susceptible Enterococcus faecium harboring LiaSR substitutions. Clin Infect Dis 2014; 59:1277–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Centers for Disease Control and Prevention. Antibiotic/antimicrobial resistance: biggest threats Available at: http://www.cdc.gov/drugresistance/biggest_threats.html. Accessed 10 August 2016.
- 37. Carpenter CF, Chambers HF. Daptomycin: another novel agent for treating infections due to drug-resistant gram-positive pathogens. Clin Infect Dis 2004; 38:994–1000. [DOI] [PubMed] [Google Scholar]
- 38. Florescu I, Beuran M, Dimov R, et al. ; 307 Study Group Efficacy and safety of tigecycline compared with vancomycin or linezolid for treatment of serious infections with methicillin-resistant Staphylococcus aureus or vancomycin-resistant enterococci: a phase 3, multicentre, double-blind, randomized study. J Antimicrob Chemother 2008; 62:i17–28. [DOI] [PubMed] [Google Scholar]