Summary
Most clinicians do not adhere to IDSA guidelines, fostering overutilization of unnecessary head computed tomography (CT) scans that delay diagnosis and therapy of adults with community-acquired meningitis. Only 8 of 549 (1.5%) head CT scan results had abnormalities that affected clinical management.
Keywords: head CT, lumbar puncture, meningitis.
Abstract
Background.
The Infectious Diseases Society of America (IDSA) guidelines delineate criteria for the use of computed tomography (CT) scan of the head before lumbar puncture (LP) in adults with community-acquired meningitis (CAM). There are limited data to document adherence to these guidelines and assess the clinical utility of brain imaging.
Methods.
This was a retrospective analysis from January 2005 to January 2010 in Houston, Texas.
Results.
Among 614 adults with CAM, 407 patients (66.3%) did not have an indication for a head CT scan and 207 (33.7%) did. Patients with a CT scan indication were older, had more comorbidities, were sicker, and had more urgent treatable etiologies and adverse clinical outcomes (P < .001). A CT scan was ordered before the LP in 549 patients (89%). Overall, clinicians did not adhere to clinical guidelines in 368 of 614 (60%) subjects. A CT of the head was ordered when not indicated in 355 of 549 patients (64%), and not done when indicated in 13 of 207 patients (0.6%). CT of the head revealed intracranial abnormalities in 35 of 193 patients (18.1%) with an indication for brain imaging, compared with only 2 of 356 (0.05%) with no indication (P < .05). Major intracranial findings were seen in only 15 of 549 (2.7%) patients, all with an indication for brain imaging. Furthermore, only 8 patients had abnormalities that affected clinical management.
Conclusions.
Most clinicians do not adhere to IDSA guidelines, delaying diagnostic LP and increasing costs. Usefulness of head CT in patients with CAM without an indication for imaging is limited and has no impact in clinical management.
Community-acquired meningitis (CAM) is caused by a variety of pathogens and the associated mortality varies accordingly [1]. Rapid diagnosis and prompt initiation of therapy can reduce morbidity and mortality [1, 2]. A computed tomography (CT) scan of the head is frequently ordered by clinicians prior to performing a lumbar puncture (LP) to rule out an intracranial abnormality with elevated intracranial pressure that could potentially place the patient at risk for brain herniation, a rare, yet fatal complication [1–5]. To avoid unnecessary delays in diagnosis and treatment, the Infectious Diseases Society of America (IDSA) recommends the following criteria for ordering a head CT prior to LP: immunocompromised state (eg, human immunodeficiency virus [HIV]/AIDS, receiving immunosuppressive therapy, or after transplantation), history of central nervous system (CNS) disease (eg, mass lesion, stroke, or focal infection), new-onset seizure (eg, within 1 week of presentation), papilledema, abnormal level of consciousness, and focal neurological deficit [3]. In 2009, the Swedish guidelines removed altered mental status as an indication for cranial imaging and recently reported that this practice has been associated with earlier treatment and improved outcomes [6]. In this study, patients who received a CT scan had worse outcomes, but this difference was not statistically significant after adjusting for confounders. United Kingdom guidelines recommend a CT scan if there are focal neurological findings and a Glasgow Coma Scale (GCS) score ≤12, but suggest that an LP can be done safely at lower levels [7]. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines state that CT should precede LP if the GCS score is <10 and if there is focal neurologic deficit excluding cranial nerve palsies [8]. According to Swedish guidelines, CT should precede LP if there is suspicion of cerebral mass/abscess (>4 days of cerebral symptoms or neurologic deficit except cranial nerve palsy) and if there are signs of herniation including coma with dilated nonreactive pupils. Otherwise, prompt LP is recommended [6, 9].
Despite available guidelines to improve the utilization of cranial imaging in suspected meningitis, compliance has been low in the United States [10]. Additionally, a recent study from the Netherlands has also demonstrated that physicians continue to order cranial imaging in the majority of patients despite guideline recommendations [11]. The main objectives of this study were to identify the adherence of clinicians to IDSA guidelines regarding cranial imaging in patients with CAM, to evaluate the clinical and prognostic differences between those patients with and without an indication for cranial imaging, and to assess the clinical impact in management in those with abnormal intracranial findings with or without altered mental status as their sole indication for imaging.
METHODS
Case Definition
A case was defined as an adult patient (aged >16 years) with community-acquired symptoms of meningitis (fever, headache, stiff neck, altered mental status, or focal neurological symptoms) and cerebrospinal fluid (CSF) white blood cell (WBC) count > 5 cells/µL, who presented to an emergency department between January 2005 and January 2010 at 8 hospitals in Houston and its surrounding areas. The study was approved by the University of Texas Health Center at Houston Committee for the Protection of Human Subjects and by the Memorial Hermann Hospital Research Review Committee.
Data Collection, Laboratory Testing, and Definition of Diagnostic Outcomes
Baseline characteristics were recorded at as the time when the patient presented to the emergency department. Sociodemographic data, comorbidity as measured by the Charlson comorbidity index [12], immunocompetence, presenting symptoms and signs including neurological exam and GCS [13], laboratory results, and management decisions were recorded. Head CT scans and magnetic resonance imaging (MRI) of the brain were read by a board-certified neuroradiologist and classified as abnormal if anything other than cerebral atrophy or sinusitis were noted. The CT scan findings were further classified as major if they had intracranial hemorrhage, mass lesion, stroke other than lacunar, or cerebral edema and classified as minor if they had chronic ischemic changes, white matter abnormalities, and/or lacunar strokes.
The etiologies of the meningitis syndromes were divided into 4 categories as previously described: (1) unknown cause; (2) untreatable cause; (3) treatable but not urgent cause; (4) urgent treatable cause [14]. Patients’ outcomes were assessed at the time of discharge from the hospital using the Glasgow Outcome Scale [14, 15]. The main objectives of the study were to describe clinicians’ adherence to the indications for brain imaging, to assess the clinical and prognostic differences in those patients with and without an indication, and to describe the major and minor intracranial findings in those with and without an indication for scanning. Furthermore, we examined the impact of the intracranial findings on management decisions in those with and without altered mental status as their sole indication.
Statistical Analysis
Baseline clinical characteristics, etiologies, and abnormalities on cranial imaging were compared between those patients with an indication for cranial imaging and those without an indication by bivariate analysis by using the Fisher exact test, χ2 test, and Student t test. Continuous data were examined by analysis of variance. All P values <.05 were considered to be statistically significant. Data were analyzed using IBM SPSS software version 21.
RESULTS
Cohort Assembly
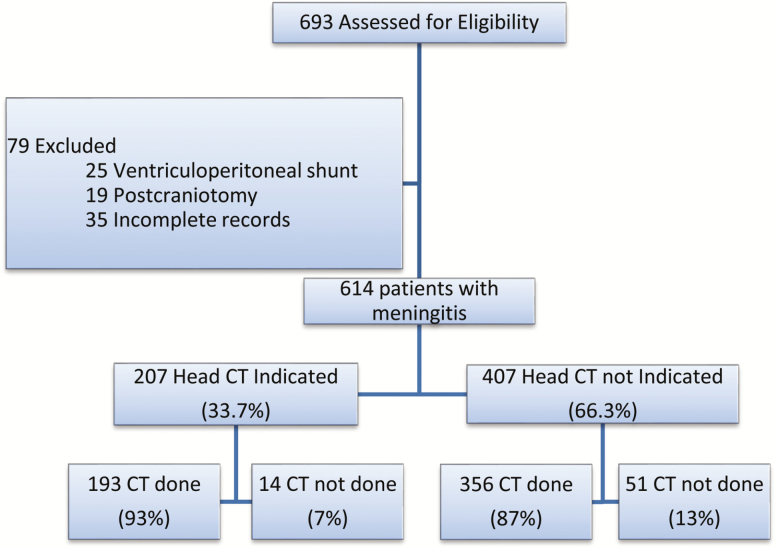
Once we screened 693 patients with meningitis, 79 patients were excluded for the following reasons: presence of a ventricular peritoneal shunt (n = 25) or postcraniotomy meningitis (n = 19), and incomplete medical records (n = 35). Consequently, a total of 614 patients were enrolled and distributed based on whether a head CT was not indicated before LP (n = 407 [66.3%]) or indicated before LP (n = 207 [33.7%]) (Figure 1).
Figure 1.
Cohort assembly and proportions of patients with indications for head computed tomography (CT) scan before lumbar puncture.
Baseline Features and Clinical Findings of Adults With and Without a CT Indication
Baseline characteristic and clinical data are summarized in (Table 1). The cohort consisted of mainly young adults (median age, 37 years [range, 18–92 years]), with older and male patients having more indications for a CT scan. Racial minorities (African Americans, Hispanics, and other) had also more indications for CT scans than did white patients. Patients with an indication for CT had more comorbidities (Charlson score >1), HIV/AIDS, history of injection drug use, sinusitis, otitis, and history of a CNS lesion. The patients without an indication for a CT scan reported more of the following symptoms: headache (97.8%, P < .001), nausea (75.2%, P < .001), photophobia (47.9%, P < .001), and stiff neck (52%, P < .01). There were no patients in those without an indication for a CT scan with abnormal mental status, seizures, focal neurological deficits, or papilledema (P < .01). Subjective fever did not significantly differ between groups, but those with an indication for CT scan had fever more frequently documented (temperature >38.4°C, P < .001).
Table 1.
Baseline Characteristics of 614 Adults With Community-Acquired Meningitis
| Clinical Features | CT Indicated (n = 207) | CT Not Indicated (n = 407) | P Value |
|---|---|---|---|
| Age, y, median (range) | 46 (18–92) | 34 (18–89) | <.001 |
| Female sex | 89 (42.4) | 238 (58.2) | <.001 |
| Race | |||
| White | 80 (38.1) | 207 (50.6) | <.001 |
| African American | 71 (33.8) | 97 (23.7) | <.001 |
| Hispanic | 53 (25.2) | 93 (22.7) | .49 |
| Other | 6 (2.9) | 12 (2.9) | .96 |
| Coexisting medical conditions | |||
| Charlson comorbidity index score ≥1 | 131 (62.4) | 36 (8.8) | <.001 |
| HIV/AIDS* | 63/207 (30.4) | 1 (0.2) | <.001 |
| History of injection drug use | 11/203 (5.4) | 1 (0.2) | <.001 |
| Sinusitis or otitis | 27 (12.9) | 14 (3.4) | <.001 |
| History of CNS lesion* | 18 (8.6) | 0 (0.0) | <.001 |
| Presenting history | |||
| Headache | 147/190 (77.4) | 400 (97.8) | <.001 |
| Nausea | 97/186 (52.2) | 306/407 (75.2) | <.001 |
| Subjective fever | 128/203 (63.1) | 258/407 (63.3) | .97 |
| Stiff neck | 56/185 (30.3) | 209/402 (52.0) | <.001 |
| Photophobia | 34/157 (21.7) | 184/384 (47.9) | <.001 |
| Seizure* | 26/206 (12.6) | 0 (0.0) | <.001 |
| Presenting signs | |||
| Nuchal rigidity | 48/179 (26.8) | 131/395 (33.2) | .13 |
| Temperature >38.4°C | 99/205 (48.3) | 91/407 (22.3) | <.001 |
| Abnormal mental statusa,* | 118/207 (57.0) | 0/407 (0.0) | <.001 |
| GCS score <15 | 81/196 (41.3) | 0/407 (0.0) | <.001 |
| Focal neurologic deficitsb,* | 43/202 (21.3) | 0/407 (0.0) | <.001 |
| Vesicular or petechial rash | 6/200 (3.0) | 5 (1.2) | .12 |
| Papilledema | 1/2 (50.0) | 0/4 (0.0) | .12 |
| Blood and CSF analysis | |||
| CSF leukocyte, cells/μL, median (range) | 103.5 (6–53.600) | 175 (6–44040) | .009 |
| Serum leukocyte, × 103 cells/μL, median (range) | 9.4 (1.5–43.5) | 8.6 (0.9–42.0) | .006 |
| CSF protein, mg/dL, median (range) | 105.5 (21–659) | 74 (18–706) | <.001 |
| CSF glucose, mg/dL, median (range) | 52 (1–421) | 56 (1–366) | .782 |
| Management decision | |||
| Admission to hospital | 207 (99.5) | 392 (95.8) | .01 |
| Empiric antibiotic therapy | 149/205 (72.7) | 303/406 (74.6) | .60 |
| Empiric acyclovir therapy | 76/207 (36.7) | 81/407 (19.9) | <.001 |
| Head CT taken | 193 (93.2) | 356 (87.3) | .02 |
| Abnormalc | 35/193 (18.1) | 2/356 (0.05) | <.001 |
| Brain MRI taken | 146 (69.5) | 144 (35.2) | <.001 |
| Abnormald | 76/146 (52.1) | 33/144 (22.9) | <.001 |
| Clinical status at discharge | |||
| Adverse clinical outcomee | 59 (28.5) | 11 (2.7) | <.001 |
Data are presented as No. (%) unless otherwise indicated. Some denominators are presented to reflect missing data. Infectious Diseases Society of America criteria for undergoing CT prior to lumbar puncture are indicated by (*).
Abbreviations: CNS, central nervous system; CSF, cerebrospinal fluid; CT, computed tomography; GCS, Glasgow Coma Scale; HIV, human immunodeficiency virus; MRI, magnetic resonance imaging.
aDisorientation (n = 37) or Glasgow Coma Scale score <15 (n = 81).
bFocal motor deficit, cranial nerve abnormality, or aphasia.
cSee Table 4.
dMass lesions, strokes, hypoattenuations, meningeal enhancement, bleeds, white matter abnormalities.
eGlasgow Outcome Scale score of 1–4.
Patients with an indication for a CT scan had lower CSF pleocytosis, higher CSF protein, and higher serum WBC counts (P < .001), but had similar median CSF glucose levels (P = .782). Patients with an indication for a CT scan were more likely to undergo brain imaging with CT and MRI, had more abnormalities on imaging, and were more likely to be admitted and treated with empiric acyclovir therapy (P ≤ .01). Both groups had similar rates of empiric antibiotic use (P = .60). Finally, patients with an indication for a CT scan had more adverse clinical outcomes (28.5% vs 2.7%, P < .001).
An etiological agent was not identified in 406 patients (66%); patients with an indication for a CT scan were more likely to have a pathogen identified (unknown etiology, 41% vs 78.9%, P < .001) (Table 2). Patients with an indication for a CT scan had more urgent treatable causes (eg, bacterial meningitis, herpes simplex encephalitis, Cryptococcus neoformans, varicella zoster virus) (P < .001) and less likely to have nonurgent treatable etiologies (P = .01). Untreatable conditions (West Nile virus, enterovirus, St Louis encephalitis virus, and Epstein-Barr virus) were identified in 6.8% of cases, with no significant differences between those with or without a CT indication (P = .35).
Table 2.
Etiologies in 614 Patients With Community-Acquired Meningitis
| Etiology | CT Indicated (n = 207) | CT Not Indicated (n = 407) | P Valuea |
|---|---|---|---|
| Unknown | 85 (41.0) | 321 (78.9) | <.001 |
| Urgent treatableb | 100 (48.3) | 22 (5.4) | <.001 |
| Untreatablec | 17 (8.2) | 25 (6.1) | .35 |
| Nonurgent treatabled | 5 (2.4) | 38 (9.5) | .01 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviation: CT, computed tomography.
a P values comparing patients with an indication for CT before lumbar puncture vs those who lack indications.
bIncluding bacterial meningitis (n = 46), Cryptococcus neoformans (n = 51), herpes simplex virus encephalitis (n = 9), Mycobacterium tuberculosis (n = 3), varicella zoster virus (n = 3), central nervous system lymphoma (n = 1), systemic lupus erythematosus flare (n = 1), Toxoplasma gondii (n = 1), infective endocarditis (n = 1), histoplasmosis (n = 1), cerebral aneurysm (n = 1), epidural empyema (n = 1), Brucella (n = 1), and Escherichia coli urinary tract infection (n = 2).
cIncluding West Nile virus (n = 28), enterovirus (n = 12), St Louis encephalitis virus (n = 1), Epstein-Barr virus (n = 1).
dIncluding herpes simplex virus meningitis (n = 37), acute human immunodeficiency virus (n = 1), neurosyphilis (n = 1), multiple sclerosis (n = 1), influenza A virus (n = 1), and cytomegalovirus (n = 2).
A total of 207 patients (33.7%) had indication(s) for having a CT ordered; several patients had >1 criteria. The most common indications were abnormal consciousness (19.1%), immunocompromise (13.4%), focal neurological deficit (6.9%), and new-onset seizures (4.2%) (Table 3). A history of CNS disease was seen in 2.9%, and only 1 patient had papilledema. Only 36 of the 118 (30.5%) patients with altered mental status had no other indication for brain imaging.
Table 3.
Indications for Undergoing Head Computed Tomography Prior to Lumbar Puncture in 614 Patients With Community-Acquired Meningitis as per Infectious Diseases Society of America Criteria
| Indications | No. (%) of Patients With Indicationa |
|---|---|
| Abnormal consciousnessb | 118 (19.1) |
| Immunocompromisedc | 83 (13.4) |
| Focal neurologic deficitd | 43 (6.9) |
| New-onset seizures | 26 (4.2) |
| History of CNS disease | 18 (2.9) |
| Papilledema | 1 (0.2) |
Abbreviation: CNS, central nervous system.
aSome patients may have >1 indication.
bThirty-six of the 118 (30.5%) patients only had altered mental status without any other indication.
cIncluding patients with human immunodeficiency virus, AIDS, organ transplantation, steroid use, recent chemotherapy, and other conditions affecting immune status.
dFocal motor deficit (n = 40), cranial nerve abnormality (n = 1), or aphasia (n = 2).
A CT scan was ordered before the LP in 549 of 614 patients (89%). Overall, clinicians did not adhere to clinical guidelines in 370 of 614 (60%) subjects. A CT of the head was ordered when not indicated in 355 of 549 (64%), and not done when indicated in 13 of 207 (0.6%). There was no difference in the delay in antibiotic therapy in those patients who received a head CT scan vs those who did not (median delay, 8.25 hours [range, 0.25–94.6 hours] vs 5.5 hours [range, 0.8–29.5 hours], respectively, P = .460). CT of the head revealed intracranial abnormalities in 35 of 193 (18.1%) with an indication for brain imaging compared to only 2 of 356 (0.05%) with no indication (P < .05) (Table 4). In patients with an indication for a CT scan, major intracranial findings (eg, intracranial hemorrhage, mass, strokes, cerebral edema) were seen in 15 of 35 (42%) abnormal CT scans. In 4 of those 15 patients, the indication was solely altered mental status. A change in therapy occurred in only 8 of the 15 patients with major intracranial findings; all of them had more than altered mental status as their only indication. These 8 cases had repeat cranial imaging with either a CT and/or MRI: 5 underwent surgery (3 had a ventriculoperitoneal shunt placement [preoperative diagnoses: brain injury, worsening hydrocephalus, ventriculomegaly/vasculitis], 1 had an external ventricular device [preoperative diagnosis: skull-based defect with symptomatic pneumocephalus and CSF rhinorrhea], and 1 underwent resection of a pituitary mass [preoperative diagnosis: pituitary tumor]); the remaining 3 cases had a change in management, including a laryngoscopy of a clival lesion, treatment of suspected herpes simplex encephalitis, and a diagnosis of a pituitary adenoma. In the group without an indication for a CT scan, only 2 patients showed abnormal findings; both showed minor intracranial findings with no impact on clinical management.
Table 4.
Head Computed Tomography Findings in 549 Patients With Community-Acquired Meningitis
| Results of Head CT | No. (%) of Patients With Indication (n = 193) | No. (%) of Patients Without Indication (n = 356) | P Value |
|---|---|---|---|
| Normal | 158 (81.4) | 354 (99.4) | <.05 |
| Abnormal | 35 (18.5) | 2 (0.05) | <.05 |
| Major intracranial findingsa | 15 | 0 | |
| Only AMS | 4 | 0 | |
| Minor intracranial findingsb | 20 | 2 | |
| Only AMS | 4 | 1 | |
| Head CT scan findings changed therapy | (n = 8) | (n = 0) | |
| Major | 8/15c | NA | |
| Only AMS | 0 | NA | |
| Minor | 0/20 | 0/2 | |
| Only AMS | 0 | 0 |
Abbreviations: AMS, altered mental status; CT, computed tomography; NA, not applicable.
aMajor: intracranial hemorrhage (n = 6), mass (n = 5), stroke other than lacunar (n = 2), cerebral edema (n = 3).
bMinor: chronic ischemic changes (n = 11), white matter abnormalities (n = 6), lacunar stroke (n = 3).
cVentricular peritoneal shunt placement (n = 3), external ventricular device (n = 1), laryngoscopy of clival lesion (n = 1), resection of pituitary mass (n = 1), treatment for suspected herpes simplex virus encephalitis (n = 1) and for pituitary adenoma (n = 1).
DISCUSSION
Lumbar puncture is required to diagnose and to define the etiology of CAM, but clinicians fear the potential for complications in those with intracranial pressure [4–8]. The IDSA issued specific guidelines in 2004 to help guide clinicians in the selection of patients who should undergo a screening CT scan of the brain [3]. Obtaining a CT scan before the LP has also been shown to delay diagnosis and treatment in patients with bacterial meningitis and has been reported to have an associated increase in unfavorable outcomes [6, 16]. In the recent registry study from Sweden, the authors identified a significant reduction in mortality after their guidelines were revised to delete altered mental status as an indication for scanning [16]. The difference in mortality and neurological sequelae was not statistically different after adjusting for other confounders such as age, sex, mental status, antibiotic therapy, and adjunctive corticosteroids. In this study, we observed that having an indication for a CT scan has significant clinical and prognostic implications. Patients with an indication for CT scanning are older, are sicker, and have more comorbidities, urgent treatable etiologies, and adverse clinical outcomes (P < .001). Adjusting for these differences is important to clearly understand the true prognostic impact of receiving a CT scan in patients with CAM.
Data on compliance with the IDSA bacterial meningitis guidelines in the United States are scant. In a study of 160 adults with suspected meningitis, overall noncompliance with neuroimaging recommendations was 46% [9]. In our study, clinicians did not adhere to guidelines in 370 of 614 (60%) subjects. A CT of the head was ordered when not indicated in 355 of 549 (64%), and not done when indicated in 13 of 207 (0.6%). Approximately 50% of patients with an urgent treatable etiology such as bacterial meningitis had an indication for a CT scan. Altered mental status was the most common indication for brain imaging in 118 of 207 patients (57%), followed by immunocompromised host (40%) and focal neurological deficits (20.8%). It is important to note that several patients had >1 indication for a CT scan, with only 36 of 118 patients (30.5%) having altered mental status as their only indication. Removing altered mental status as the sole indication as per the Swedish guidelines would have only prevented a small subset of patients undergoing cranial imaging (36 of 207 [17%]) [6], but would have missed 4 major intracranial findings, although none with an impact on clinical management.
In our study, brain imaging was done in 356 patients without an indication with only 2 minor intracranial findings, with no impact on clinical management. Obtaining a CT scan without an indication is of no clinical benefit, is costly, delays diagnosis and therapy, and can impact outcomes in patients with meningitis [4, 6, 10, 11, 16]. Avoiding cranial imaging in those without an indication could aid in reducing the costs of taking care of patients with CAM [17]. In our study, though, obtaining a CT scan was not associated with a delay in antibiotic therapy (median delay, 8.25 hours in those with CT vs 5.5 hours without CT); this could possibly be explained by the low prevalence of bacterial meningitis (7.4%). The median delay in studies of bacterial meningitis ranges from 1 hour to 5.5 hours [18].
This study reinforces the lack of utility of brain imaging in those without indications and, for the first time, compares the clinical and prognostic differences between patients with and without an indication. An impact on clinical management was seen in only 8 of 549 (1.5%) patients undergoing cranial imaging. All 8 patients had major intracranial findings and had an indication for a CT scan, and none of them had altered mental status as their only indication. Thus, the importance of CT findings prior to LP should be weighed against the risk of delayed treatment in patients with bacterial meningitis. The probability of a significant cerebral mass is most likely very low in patients with acute symptoms consistent with meningitis and impaired mental status but without focal neurologic deficits. Furthermore, in this study, an LP was performed in 37 patients with abnormal CT findings with no complications, similar to another prospective study that showed no brain herniation in 52 patients with abnormal CT scans [4].
Our study had limitations. First, cases with major intracranial findings that precluded the performance of an LP would have been missed, as only patients with proven meningitis were included in our study. This would have most likely resulted in excluding only a few patients, as this is seen in about 1.3% of patients with suspected meningitis [4]. Second, this was a retrospective study, resulting in some of the variables having missing data. Third, this study had a small proportion of bacterial meningitis cases, so the results are not optimal to influence bacterial meningitis guidelines. Fourth, funduscopic examination was only documented in 6 (1%) of all patients, representing the reality of the adherence to this IDSA recommendation. Last, the results of the CT scans were based on the reading by a board-certified neuroradiologist and not confirmed by an independent radiologist.
Despite the limitations, our study had several strengths and advantages over previous work. First, this is the largest study evaluating compliance with IDSA guidelines regarding cranial imaging in CAM and the first one evaluating the clinical and prognostic impact of having a CT scan indication. Second, this is the only study that describes the frequency of the different indications for a CT scan and evaluates the impact of altered mental status as the sole indication on intracranial findings. Last, this study is the first one to classify intracranial findings as minor and major in CAM to evaluate its impact on clinical management.
In conclusion, most clinicians do not adhere to guidelines for head imaging in suspected CAM, thus delaying diagnostic LP and increasing costs. Usefulness of head CT in patients with CAM without an indication for imaging is limited and does not change the management of these patients.
Notes
Acknowledgments. We thank Mr and Mrs Starr from the Grant-A-Starr Foundation for their support.
Financial support. This study was supported by the Grant-A-Starr Foundation and the National Center for Research Resources (grant number NIH-1 K23 RR018929-01A2; R. H., Principal Investigator).
Potential conflicts of interest. R. H. is a consultant to bioMérieux and is part of speaker’s bureaus for The Medicines Company, Pfizer, and Biofire Diagnostics. L. S. reports no potential conflicts. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Wang AY, Machicado JD, Khoury NT, Wootton SH, Salazar L, Hasbun R. Community-acquired meningitis in older adults: clinical features, etiology, and prognostic factors. J Am Geriatr Soc 2014; 62:2064–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Aronin SI, Peduzzi P, Quagliarello VJ. Adverse clinical outcome and effect of antibiotic timing. Ann Intern Med 1998; 129:862–9. [DOI] [PubMed] [Google Scholar]
- 3. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39:1267–84. [DOI] [PubMed] [Google Scholar]
- 4. Hasbun R, Abrahams J, Jekel J, Quagliarello VJ. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. N Engl J Med 2001; 345:1727–33. [DOI] [PubMed] [Google Scholar]
- 5. Korein J, Cravioto H, Leicach M. Reevaluation of lumbar puncture; a study of 129 patients with papilledema or intracranial hypertension. Neurology 1959; 9:290–7. [DOI] [PubMed] [Google Scholar]
- 6. Glimåker M, Johansson B, Grindborg Ö, Bottai M, Lindquist L, Sjölin J. Adult bacterial meningitis: earlier treatment and improved outcome following guideline revision promoting prompt lumbar puncture. Clin Infect Dis 2015; 60:1162–9. [DOI] [PubMed] [Google Scholar]
- 7. McGill F, Heyderman RS, Michael BD, et al. The UK Joint Specialist Societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults. J Infect 2016; 72:405–38. [DOI] [PubMed] [Google Scholar]
- 8. van de Beek D, Cabellos C, Dzupova O, Esposito S, Klein M, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microb Infect 2016; 22:S37–62. [DOI] [PubMed] [Google Scholar]
- 9. Glimåker M, Johansson B, Bell M, et al. Early lumbar puncture in adult bacterial meningitis—rationale for revised guidelines. Scand J Infect Dis 2013; 45:657–63. [DOI] [PubMed] [Google Scholar]
- 10. Chia D, Yavari Y, Kirsanov E, Aronin SI, Sadigh M. Adherence to standard of care in the diagnosis and treatment of suspected bacterial meningitis. Am J Med Qual 2015; 30:539–42. [DOI] [PubMed] [Google Scholar]
- 11. Costerus JM, Brouwer MC, Bijlsma MW, Tanck MW, van der Ende A, van de Beek D. Impact of an evidence-based guideline on the management of community-acquired bacterial meningitis: a prospective cohort study. Clin Microbiol Infect 2016; 22:928–33. [DOI] [PubMed] [Google Scholar]
- 12. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373–83. [DOI] [PubMed] [Google Scholar]
- 13. Plum F, Levy DE. Predicting prognosis in coma. Can one improve medical decisions? Am J Med 1978; 65:224–6. [DOI] [PubMed] [Google Scholar]
- 14. Khoury NT, Hossain MM, Wootton SH, Salazar L, Hasbun R. Meningitis with a negative cerebrospinal fluid Gram stain in adults: risk classification for an adverse clinical outcome. Mayo Clin Proc 2012; 87:1181–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Van De Beek D, De Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004; 351:1849–59. [DOI] [PubMed] [Google Scholar]
- 16. Proulx N, Fréchette D, Toye B, Chan J, Kravcik S. Delays in the administration of antibiotics are associated with mortality from adult acute bacterial meningitis. QJM 2005; 98:291–8. [DOI] [PubMed] [Google Scholar]
- 17. Castelblanco RL, Lee M, Hasbun R. Epidemiology of bacterial meningitis in the USA from 1997 to 2010: a population-based observational study. Lancet Infect Dis 2014; 14:813–9. [DOI] [PubMed] [Google Scholar]
- 18. Køster-Rasmussen R, Korshin A, Meyer CN. Antibiotic treatment delay and outcome in acute bacterial meningitis. J Infect 2008; 57:449–54. [DOI] [PubMed] [Google Scholar]