Men and women in South Africa and men who have sex with men remain at increased risk of Kaposi sarcoma compared with other human immunodeficiency virus–positive persons receiving antiretroviral therapy, probably owing to high human herpesvirus 8 coinfection rates.
Keywords: Kaposi sarcoma, HIV, antiretroviral therapy, cohort study
Abstract
Background
We compared Kaposi sarcoma (KS) risk in adults who started antiretroviral therapy (ART) across the Asia-Pacific, South Africa, Europe, Latin, and North America.
Methods
We included cohort data of human immunodeficiency virus (HIV)–positive adults who started ART after 1995 within the framework of 2 large collaborations of observational HIV cohorts. We present incidence rates and adjusted hazard ratios (aHRs).
Results
We included 208140 patients from 57 countries. Over a period of 1066572 person-years, 2046 KS cases were diagnosed. KS incidence rates per 100000 person-years were 52 in the Asia-Pacific and ranged between 180 and 280 in the other regions. KS risk was 5 times higher in South African women (aHR, 4.56; 95% confidence intervals [CI], 2.73–7.62) than in their European counterparts, and 2 times higher in South African men (2.21; 1.34–3.63). In Europe, Latin, and North America KS risk was 6 times higher in men who have sex with men (aHR, 5.95; 95% CI, 5.09–6.96) than in women. Comparing patients with current CD4 cell counts ≥700 cells/µL with those whose counts were <50 cells/µL, the KS risk was halved in South Africa (aHR, 0.53; 95% CI, .17–1.63) but reduced by ≥95% in other regions.
Conclusions
Despite important ART-related declines in KS incidence, men and women in South Africa and men who have sex with men remain at increased KS risk, likely due to high human herpesvirus 8 coinfection rates. Early ART initiation and maintenance of high CD4 cell counts are essential to further reducing KS incidence worldwide, but additional measures might be needed, especially in Southern Africa.
Persons infected with human immunodeficiency virus (HIV) are at high risk of developing Kaposi sarcoma (KS) [1], and this risk seems to vary geographically. KS incidence rates seem to be higher in adults who started antiretroviral therapy (ART) in sub-Saharan Africa [2, 3] and the US [4] than in Europe [5]. However, direct comparisons of KS incidence rates across studies are complicated by differences in study populations and designs.
Several factors could contribute to regional differences in KS risk, including differences in the HIV epidemic, the adequacy of local healthcare, and the prevalence of human herpesvirus 8 (HHV-8). HHV-8 is a necessary but not sufficient cause of KS [6], and its distribution varies by geographic region and population group [7]. HIV-related immunosuppression is a strong risk factor for KS in HHV-8–coinfected persons [5, 8–10]. Access to healthcare varies across regions, and patients in high-income countries start ART at higher CD4 cell counts than those in low- and middle-income settings [11]. We compared KS incidence rates in HIV-positive adults who started ART across different continents, and we assessed factors associated with regional differences in KS risk.
METHODS
Databases
We analyzed longitudinal routine clinical care data of HIV-positive patients within the framework of the International Epidemiology Databases to Evaluate AIDS (IeDEA) and the Collaboration of Observational HIV Epidemiological Research in Europe (COHERE) in the European Coordinating Committee for the integration of ongoing coordination actions related to clinical and epidemiological HIV research (EuroCoord). IeDEA is a global research consortium of observational HIV cohorts with data centers in the Asia-Pacific, Australia, Africa, North, and Latin America. Four IeDEA regions contributed data to this study: the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) [12], the Caribbean, Central and South America network for HIV epidemiology (CCASAnet) [13], IeDEA Southern Africa [14], and IeDEA Asia-Pacific [15]; the latter includes data from 2 geographic regions: the Asia-Pacific and Australia. COHERE in EuroCoord is a collaboration of observational HIV cohorts across Europe [16]. For details on how data were collected and combined, see Supplementary Box S1. All cohorts obtained ethical approval from local ethics committees or institutional review boards.
Inclusion Criteria and Definitions
We restricted the analysis to cohorts that systematically collected cancer data or had improved their data through record linkages with cancer registries. We included HIV-positive adults (aged ≥16 years) who started ART after enrollment into the cohort from 1996 onward. We excluded patients without follow-up after ART initiation and patients with no CD4 cell counts during follow-up. We excluded regions with <500 eligible patients and cohorts with <100 eligible patients. We excluded the region Asia-Pacific from statistical models owing to few KS cases (post hoc decision). Incident KS cases were defined as histologically or clinically diagnosed KS at any time after ART initiation. ART was defined as a regimen of ≥3 antiretroviral drugs from any class, including protease inhibitors (PIs), nucleoside reverse-transcriptase inhibitors, and nonnucleoside reverse-transcriptase inhibitors (NNRTIs). Patients were assumed to remain on ART once initiated. CD4 cell counts at ART initiation were defined as the measurement nearest ART initiation, within 180 days before to 7 days after initiation. The HIV/AIDS stage at ART initiation was defined according to the US Centers for Disease Control and Prevention [17].
Statistical Analyses
We calculated raw KS incidence rates by dividing the number of incident KS cases by person-years at risk. Time at risk was measured from ART initiation to the first occurrence of KS diagnosis, last follow-up visit, death, or database closure. We anticipated that the KS hazard would vary by follow-up time and geographic region and used proportional hazard flexible parametric survival models [18] to compare the risk of developing KS after ART initiation across regions and to identify KS risk factors. We modeled the baseline hazard using restricted cubic splines with 4 degrees of freedom and allowed for time-dependent region-effects with 2 degrees of freedom. Likelihood ratio tests were used to test for interactions between risk factors and regions. We assessed sex, exposure group (women, heterosexual men, men who have sex with men [MSM]), age at ART initiation (16–25, 26–35, 36–45, 46–55, or ≥56 years), first-line ART regimen (NNRTI-based, PI-based, other), calendar period of ART initiation (1996–1998, 1999–2003, 2004–2007, or 2008–2014), and current (time-updated) CD4 cell count (<50, 50–99, 100–199, 200–349, 350–499, 500–699, or ≥700 cells/µL). Mode of infection, HIV/AIDS stage, and HIV RNA level at ART initiation were assessed in descriptive analyses.
We fit “crude” models with 1 risk factor and its interaction with region (where applicable) to compare the actual KS burden across regions. Adjusted models with relevant risk factors and their interaction with region (if necessary) were then fit to assess remaining differences in KS incidence rates across regions. The main adjusted model included region, sex and its interaction with region, age at ART initiation and its interaction with region, current CD4 cell count and its interaction with region, first-line ART regimen, and calendar period of ART initiation. The second adjusted model was restricted to the 3 regions with data on sexual orientation (Europe, Latin, and North America), and included exposure group, age at ART initiation, current CD4 cell count, first-line ART regimen, and calendar period of ART initiation. In sensitivity analyses, we excluded the first 3 months of follow-up. KS incidence rates were predicted from adjusted models for patients with a standardized risk factor set: initiation of NNRTI-based regimens between 2008 and 2014 at age 40 years and current CD4 cell count 350–499 cells/µL. Results are presented as medians with interquartile ranges (IQRs), number and percentage of patients, incidence rates per 100000 person-years, and hazard ratios (HRs) with 95% confidence intervals (CIs). Analyses were performed using Stata 14 (StataCorp) and R (R Foundation) software.
RESULTS
Descriptive Analyses
The merged multiregional data set included data on 408395 HIV-positive adults. We excluded 200255 patients for reasons detailed in Supplementary Figure S1. Excluded and included patients were similar with regard to sex (male, 70% vs 69%), risk group (MSM, 33% vs 36%), age (median, 35 years vs 37 years), and CD4 cell count at ART initiation (median, 240 cells/µL vs 222 cells/µL).
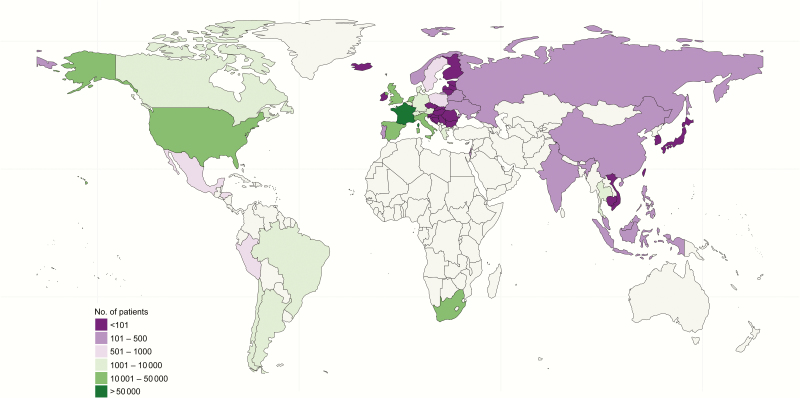
We included data on 208140 patients from 42 cohorts in 57 countries across the Asia-Pacific, South Africa, Europe, Latin, and North America (Figure 1). The median age at ART initiation was 37.3 years (IQR, 31.4–44.4 years) and similar across regions (Table 1). The percentage of men ranged from 37% in South Africa to 75% in North America. More men were MSM in Europe (54%), Latin America (57%), and North America (67%) but not in the Asia-Pacific (34%); data were not available for South Africa. The median CD4 cell count at ART initiation was <200 cells/µL in the Asia-Pacific, South Africa, and Latin America and >200 cells/µL in North America and Europe (Table 1). In South Africa and the Asia-Pacific, <5% of patients started ART before 2004, but 39% in Europe and 63% in North America started ART between 1996 and 2003. Approximately half of North American and European patients started PI-based regimens, compared with just 22% in Latin America, and <10% in South Africa and the Asia-Pacific. The median follow-up after ART initiation was >4 years in Europe, North, and Latin America but shorter in the Asia-Pacific (2.7 years) and South Africa (2.0 years).
Figure 1.
Map of countries contributing patient data to the descriptive analyses.
Table 1.
Characteristics of Included Adults at Antiretroviral Therapy Initiation
| Characteristic | Patients, No. (%)a | ||||
|---|---|---|---|---|---|
| Asia-Pacific (n = 2641) | South Africa (n = 21421) | Latin America (n = 8454) | North America (n = 16742) | Europe (n = 158882) | |
| Follow-up time, median (IQR), y | 2.7 (1.7–3.9) | 2.0 (0.8–4.0) | 4.6 (1.9–8.1) | 4.2 (1.7–8.5) | 4.4 (1.8–8.4) |
| Sex | |||||
| Female | 816 (31) | 13554 (63) | 2264 (27) | 4218 (25) | 44198 (28) |
| Male | 1825 (69) | 7867 (37) | 6190 (73) | 12524 (75) | 114684 (72) |
| Age at ART initiation, median (IQR), y | 36.3 (30.5–43.1) | 36.4 (31.0–42.7) | 35.6 (29.7–42.9) | 39.6 (33.8–46.1) | 37.3 (31.4–44.5) |
| Age at ART initiation, y | |||||
| 16–25 | 233 (9) | 1719 (8) | 993 (12) | 923 (6) | 13186 (8) |
| 26–35 | 1053 (40) | 8549 (40) | 3372 (40) | 4770 (28) | 57333 (36) |
| 36–45 | 871 (33) | 7689 (36) | 2568 (30) | 6825 (41) | 54749 (34) |
| 46–55 | 355 (13) | 2851 (13) | 1111 (13) | 3305 (20) | 23460 (15) |
| ≥56 | 129 (5) | 613 (3) | 410 (5) | 919 (5) | 10154 (6) |
| Mode of infection | |||||
| MSM | 616 (23) | NR | 3543 (42) | 8419 (50) | 62314 (39) |
| PWID | 164 (6) | NR | 169 (2) | 1794 (11) | 17241 (11) |
| Heterosexual | 1678 (64) | 17965 (84) | 3671 (43) | 4965 (30) | 65445 (41) |
| Other | 175 (7) | 9 (<1) | 91 (1) | 258 (2) | 3520 (2) |
| Missing | 8 (<1) | 3447 (16) | 980 (12) | 1306 (8) | 10362 (7) |
| First-line ART regimen | |||||
| NNRTI-based | 2375 (90) | 20267 (95) | 6361 (75) | 6167 (37) | 66569 (42) |
| PI-based | 229 (9) | 1107 (5) | 1891 (22) | 9044 (54) | 80995 (51) |
| Other ART | 37 (1) | 47 (<1) | 202 (2) | 1531 (9) | 11318 (7) |
| Year of ART initiation | |||||
| 1996–1998 | 0 (0) | 0 (0) | 107 (1) | 5332 (32) | 18771 (12) |
| 1999–2003 | 100 (4) | 99 (<1) | 1926 (23) | 5167 (31) | 43004 (27) |
| 2004–2007 | 510 (19) | 10365 (48) | 2786 (33) | 4055 (24) | 39388 (25) |
| 2008–2014 | 2031 (77) | 10957 (51) | 3635 (43) | 2188 (13) | 57719 (36) |
| CDC stage at ART initiation | |||||
| A/B | 1225 (46) | 16561 (77) | 3850 (46) | 11920 (71) | 122365 (77) |
| C | 921 (35) | 746 (3) | 1183 (14) | 2536 (15) | 19708 (12) |
| Missing | 495 (19) | 4114 (19) | 3421 (40) | 2286 (14) | 16809 (11) |
| CD4 cell count at ART initiation, median (IQR), cells/µL | 137 (43–234) | 107 (43–176) | 165 (61–273) | 233 (93–378) | 250 (128–369) |
| CD4 cell count at ART initiation, cells/µL | |||||
| <50 | 680 (26) | 5461 (25) | 1509 (18) | 2620 (16) | 17691 (11) |
| 50–99 | 327 (12) | 3915 (18) | 1031 (12) | 1318 (8) | 11749 (7) |
| 100–199 | 604 (23) | 7178 (34) | 1649 (20) | 2620 (16) | 25890 (16) |
| 200–349 | 736 (28) | 2589 (12) | 2145 (25) | 4205 (25) | 48185 (30) |
| 350–499 | 95 (4) | 395 (2) | 584 (7) | 2340 (14) | 23895 (15) |
| 500–699 | 16 (1) | 188 (1) | 204 (2) | 1343 (8) | 11225 (7) |
| ≥700 | 6 (<1) | 81 (<1) | 81 (1) | 694 (4) | 5498 (3) |
| Missing | 177 (7) | 1614 (8) | 1251 (15) | 1602 (10) | 14749 (9) |
| HIV RNA at ART initiation, median (IQR), log10 copies/mL | 5.0 (4.5–5.4) | 4.5 (2.7–5.3) | 4.9 (4.3–5.4) | 4.5 (3.5–5.2) | 4.8 (4.1–5.3) |
| HIV RNA at ART initiation, log10 copies/mL | |||||
| <2.7 | 43 (2) | 1192 (6) | 278 (3) | 2485 (15) | 13057 (8) |
| 2.7–3.9 | 201 (8) | 589 (3) | 699 (8) | 2392 (14) | 18352 (12) |
| 4.0–4.9 | 760 (29) | 1306 (6) | 2273 (27) | 5132 (31) | 50850 (32) |
| ≥5.0 | 1044 (40) | 1633 (8) | 2673 (32) | 4499 (27) | 54417 (34) |
| Missing | 593 (22) | 16701 (78) | 2531 (30) | 2234 (13) | 22206 (14) |
Abbreviations: ART, antiretroviral therapy; CDC, Centers for Disease Control and Prevention; HIV, human immunodeficiency virus; IQR, interquartile range; MSM, men who have sex with men; NNRTI, nonnucleoside reverse-transcriptase inhibitor; NR, not reported; PI, protease inhibitor; PWID, persons who inject drugs.
aData represent No. (%) of patients unless otherwise specified.
Over the course of 1066572 person-years, 2046 KS cases were diagnosed (1572 in Europe, 211 in North America, 150 in South Africa, 109 in Latin America, and 4 in the Asia-Pacific; Supplementary Table S1). The median time between ART initiation and KS diagnosis was 0.5 year (IQR, 0.1–2.5 years). The median age at KS diagnosis ranged from 35 years in the Asia-Pacific to 43 years in North America. The median CD4 cell count at KS diagnosis was <100 cells/µL in the Asia-Pacific, Latin, and North America and 180 cells/µL in South Africa and Europe.
The raw KS incidence rate per 100000 person-years was highest in South Africa (280; 95% CI, 238–328), followed by Latin America (244; 203–295), North America (237; 207–271), Europe (180; 172–190), and the Asia-Pacific (52; 19–137; Supplementary Table S2). The raw KS incidence rates were especially high in patients with current CD4 cell counts <50 cells/µL (ranging from 1368 in South Africa to 2950 in Latin America; Supplementary Table S3), MSM in Europe, Latin, and North America (all >300), and South African men (371; 95% CI, 293–470; Supplementary Table S4).
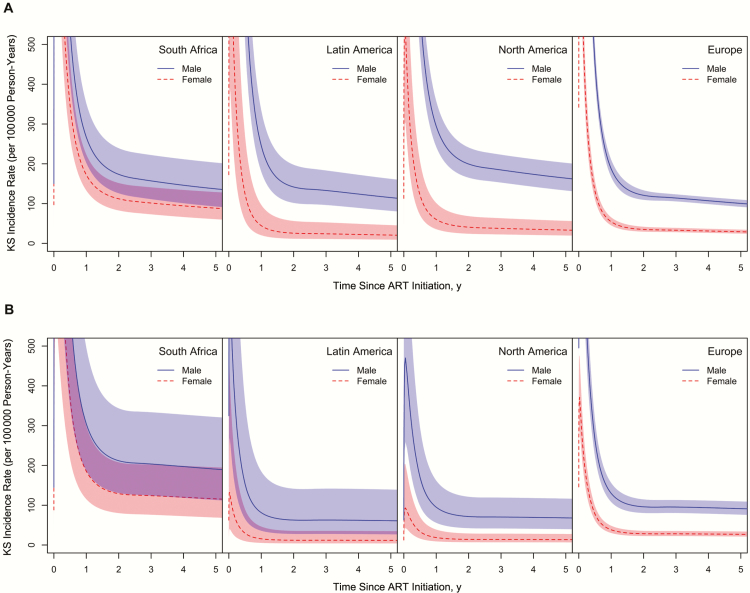
Risk Factors for Incident Kaposi Sarcoma
The following statistical models include the regions Europe, South Africa, Latin, and North America. Crude KS incidence rates were highest immediately after ART initiation and declined steeply thereafter in all population groups (Supplementary Figures S2, S3). The effect of sex, age at ART initiation, and current CD4 cell count on KS risk varied across regions. In all regions, women had a lower risk of developing KS than men in crude and adjusted analyses, but the sex difference was less pronounced in South Africa (P for interaction < .001; Table 2 and Figure 2). In Europe, North, and Latin America, KS incidence rates were highest in MSM, followed by heterosexual men, and women in crude and adjusted analyses (Supplementary Figure S4). After adjustment for current CD4 cell count, age at ART initiation, first-line regimen, and calendar year of ART initiation, the KS risk was 53% higher in heterosexual men than women (adjusted HR [aHR] 1.53; 95% CI, 1.28–1.83), and 6 times higher in MSM (aHR 5.95; 5.09–6.96). There was no evidence that the effect of exposure group on KS risk differed across regions (P for interaction = .19).
Table 2.
Regional Risk Factors for Incident Kaposi Sarcoma in Adults Who Started ART
| Risk Factor | HR (95% CI)a | P Value for Interactionb | |||
|---|---|---|---|---|---|
| South Africa | Latin America | North America | Europe | ||
| Sex | |||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | <.001 |
| Female | 0.61 (.44–.85) | 0.19 (.09–.41) | 0.20 (.12–.34) | 0.29 (.25–.35) | |
| Age at ART initiation (per decade increase) | 0.76 (.62–.93) | 0.88 (.72–1.09) | 1.17 (1.01–1.36) | 1.04 (.99–1.09) | .003 |
Abbreviations: ART, antiretroviral therapy; CI, confidence interval; HR, hazard ratio.
aHRs adjusted for current CD4 cell count and its interaction with region, sex and its interaction with region, age and its interaction with region, calendar year of ART initiation, and first-line ART regimen.
b P values derived from likelihood ratio test comparing the main adjusted model with the model without interaction of a specific variable with region.
Figure 2.
Kaposi sarcoma (KS) incidence rates by time since antiretroviral therapy (ART) initiation in men and women predicted from the crude model with sex and its interaction with region (A), and predicted from the main adjusted model for men and women with a current CD4 cell count of 350–499 cells/µL who started a nonnucleoside reverse-transcriptase inhibitor–based first-line ART regimen between 2008 and 2014 at age 40 years (B).
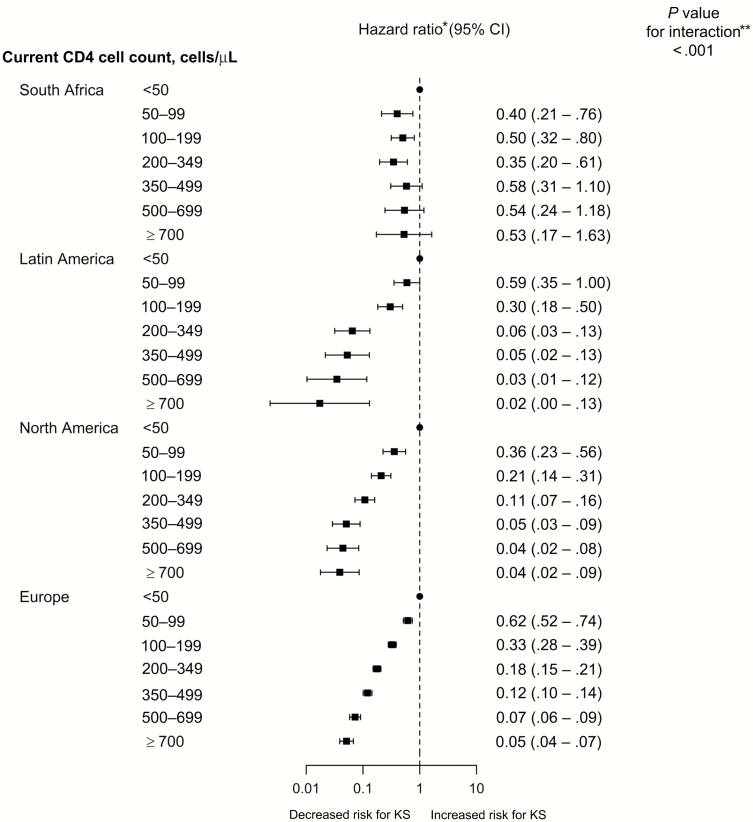
In all regions, KS risk was highest in persons with current CD4 cell counts <50 cells/µL. However, comparing patients with current CD4 cell counts ≥700 cells/µL to those with cell counts <50 cells/µL, KS risk was halved in South Africa (aHR, 0.53; 95% CI, .17–1.63), but reduced by ≥95% in the other regions (P for interaction < .001; Figure 3). In Europe and North America, KS risk tended to increase with older age, whereas it decreased in Latin America and South Africa (P for interaction = .003; Table 2). There was no strong evidence that the effect of first-line regimen or calendar period of ART initiation varied across regions (Supplementary Table S5). Patients who received PI-based first-line regimens had a slightly higher risk of developing KS than those who received NNRTI-based regimens (aHR, 1.12; 95% CI, 1.01–1.24).
Figure 3.
Regional effects of current CD4 cell counts on the risk of Kaposi sarcoma (KS) in adults who started antiretroviral therapy (ART). The blocks and horizontal lines represent hazard ratios and 95% confidence intervals (CIs). Points represent the reference categories. *Adjusted for sex and its interaction with region, age and its interaction with region, calendar year of ART start, and first-line ART regimen. **Derived from likelihood ratio test comparing the main adjusted model with the model without interaction of a specific variable with region.
Comparison of Kaposi Sarcoma Risk Between Regions
In women, KS risk at 2 years after ART initiation was >3 times higher in South Africa than in Europe in crude analyses (HR, 3.19; 95% CI, 2.26–4.52) and almost 5 times higher in analyses adjusted for current CD4 cell count, age at ART initiation, first-line regimen, and calendar period of ART initiation (aHR 4.56; 2.73–7.62; Table 3). The adjusted KS risk tended to be lower in North and Latin American women than in European women, but the effect was not statistically significant. In men, the crude risk of developing KS was highest in North America compared with Europe (HR, 1.65; 95% CI, 1.35–2.01), followed by South Africa (1.44; 1.03–2.00). In adjusted analyses, the HR for men declined to 0.75 (95% CI, 0.44–1.27) in North America, but it increased to 2.21 (1.34–3.63) in South Africa. Both changes were mainly due to adjustment for current CD4 cell count. KS risk did not differ significantly between Latin American and European men in crude or adjusted analyses.
Table 3.
Comparison of Kaposi Sarcoma Risk Between Different Regions and Europe: Crude and Adjusted HRs for Development of KS 2 Years After Antiretroviral Therapy Initiation in Women and Men
| Region | Women | Men | ||
|---|---|---|---|---|
| Crude HR (95% CI) | Adjusted HRa (95% CI) | Crude HR (95% CI) | Adjusted HRa (95% CI) | |
| Europe | 1.00 | 1.00 | 1.00 | 1.00 |
| North America | 1.16 (.68–2.00) | 0.50 (.24–1.04) | 1.65 (1.35–2.01) | 0.75 (.44–1.27) |
| Latin America | 0.73 (.33–1.63) | 0.43 (.14–1.27) | 1.17 (.84–1.64) | 0.65 (.29–1.48) |
| South Africa | 3.19 (2.26–4.52) | 4.56 (2.73–7.62) | 1.44 (1.03–2.00) | 2.21 (1.34–3.63) |
Abbreviations: CI, confidence interval; HR, hazard ratio; KS, Kaposi sarcoma.
aFor human immunodeficiency virus–positive patients with a current CD4 cell count of 350–499 cells/µL who started a nonnucleoside reverse-transcriptase inhibitor–based regimen between 2008 and 2014 at age 40 years.
We predicted KS incidence rates per 100000 person-years at 2 years after ART initiation for patients with current CD4 cell counts of 350–499 cells/µL who started NNRTI-based regimens between 2008 and 2014 at age 40 years. Predicted KS incidence rates in women were 12 (95% CI, 4–36) in Latin America, 14 (7–29) in North America, and 28 (22–36) in Europe. In heterosexual men, KS incidence rates were 29 (95% CI, 20–42) in Latin America, 35 (27–47) in North America, and 34 (27–41) in Europe. In South Africa, KS incidence rates remained at 212 (95% CI, 131–344) in men and 129 (80–208) in women. Predicted KS incidence rates in MSM were 114 (95% CI, 81–160) in Latin America, 131 (109–157) in Europe, and 138 (107–178) in North America (Supplementary Table S6).
Sensitivity Analysis
Excluding the first 3 months of follow-up resulted in lower raw KS incidence rates (Supplementary Table S7); other results remained similar (Supplementary Tables S8–S10).
DISCUSSION
After adjustment for HIV-related risk factors, HIV-positive men and women in South Africa had a higher risk of developing KS than their counterparts in Europe. In Europe, Latin, and North America, MSM had a higher KS risk than heterosexual men and women. In all regions, current CD4 cell count <50 cells/µL was a strong risk factor for incident KS. However, the clear trend toward lower KS risk with higher current CD4 cell counts seen in Europe, North, and Latin America was not observed in South Africa.
This is the first study to directly compare KS risk across several continents in adults who started ART. We used the same inclusion criteria, definitions, and statistical methods across regions. However, comparability of incidence estimates might be impaired by regional and cohort-level differences in mode and completeness of KS ascertainment. We assumed that patients within regions were independent, which might have led us to overestimate the precision of regional KS risk comparisons. To reduce underreporting of KS, data from South Africa were restricted to 2 urban cohorts that obtained additional KS data through record linkages with a cancer registry [2]. However, these South African data are not necessarily representative of the whole of South Africa, and it is unclear to what extent these results can be extrapolated to Southern Africa as a region.
We did not consider ART interruptions; therefore, KS risk in patients continuously receiving ART might be lower than what we found in our analysis for patients after ART initiation. Most patients from North America started ART before 2004 with NNRTI- or PI-based regimens, whereas almost all patients in South Africa started NNRTI-based ART from 2004 onward. Temporal changes in ART effectiveness and HIV care in general might contribute to the observed regional differences in KS risk. HIV RNA measurements at ART initiation were missing for 30% of patients in Latin America and 78% in South Africa. Therefore, it was not possible to use HIV RNA measurements to assess ART response and treatment failure. Patient-level data on HHV-8 serostatus, immune reconstitution inflammatory syndrome (IRIS)–KS, and mode of KS ascertainment were generally not available.
In our analyses, KS incidence rates were highest immediately after ART initiation, which is consistent with findings in previous studies [4, 5, 10, 19]. These peaks are partly explained by immunodeficiency that persisted after ART initiation, unmasking IRIS-KS [9, 20], and possible misclassification of some prevalent KS as incident KS. However, when we excluded KS cases occurring within 3 months after ART initiation in sensitivity analyses, our results remained similar. The effect of age at ART initiation differed across regions, with KS risk increasing with older age in North America and Europe but decreasing in Latin America and South Africa. Most previous studies have shown no or only a weakly positive association between older age and KS risk in patients receiving ART [3–5, 8, 9, 19, 21]. The slightly increased KS risk in patients who received PI-based first-line regimens might be due to confounding by indication.
Our study is one of the first to report KS incidence rates in HIV-positive adults in the Asia-Pacific, a region where HHV-8 prevalence is generally low [22]. Compared with the other regions, we found KS risk to be much lower in the Asia-Pacific. KS incidence rates were higher in South African than in European men and women. Previous studies also tended to show higher KS incidence rates in HIV-positive persons in sub-Saharan Africa [23, 24], where HHV-8 is endemic, than in Europe [9, 21]. As in other studies, our analyses showed higher KS incidence rates in MSM than in heterosexual men [5, 8, 25], and higher KS risk in men than in women [19, 25]. In South Africa, the sex difference in KS risk was smaller than in other regions. This pattern may reflect different HHV-8 risk profiles in HIV-positive men and women. In Europe, Latin, and North America, >50% of included men were MSM and, therefore, at high risk of HHV-8 coinfection, whereas women in these regions generally have lower HHV-8 seroprevalence [7]. In sub-Saharan Africa where HHV-8 is endemic, both men and women are at high risk of HHV-8 coinfection [26]. Indirect effects of sex hormones on KS tumorigenesis [27] and sex differences in immune response might also contribute to the male predominance in KS risk.
The high KS risk in South African compared with European women might be mainly explained by the higher HHV-8 prevalence in South African compared with European women. However, South African men also had a higher risk of KS than European men after adjustment for HIV-related factors. Besides differences in HHV-8 prevalence, other factors such as environmental exposures and malaria might play a role [28–30]. However, such cofactors for KS pathogenesis remain controversial. Our analyses also suggest that differences in access to HIV treatment and patient monitoring contribute to the regional differences in KS risk. For example, North American men had a higher risk of KS than European men, but after adjustment for current CD4 cell counts, the KS risk was similar.
We and others found that high CD4 cell counts had a weaker protective effect in South Africa [3, 19] than in other regions [5, 8–10]. In line with other studies [24, 31, 32], this indicates that KS diagnosis and treatment will remain a relevant aspect of HIV care in Southern Africa, also as access to ART is improving. Further research is needed to understand why KS still develops in patients with high current CD4 cell counts, especially in Southern Africa but also in other regions of the world [33, 34].
In conclusion, despite ART-related declines in KS incidence, men and women in South Africa and MSM remain at higher risk of KS than other HIV-positive persons, probably owing to higher HHV-8 coinfection rates. While a vaccine against HHV-8 remains unavailable, early ART initiation and maintenance of high CD4 cell counts are essential to reducing the incidence of KS in populations at high risk for HHV-8 coinfection.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Notes
Writing group. Eliane Rohner1, Lukas Bütikofer2, Kurt Schmidlin1, Mazvita Sengayi3, Mhairi Maskew4, Janet Giddy5, Daniela Garone6, Richard D. Moore7, Gypsyamber D’Souza8, James J. Goedert9, Chad Achenbach10, M. John Gill11, Mari M. Kitahata12, Pragna Patel13, Michael J. Silverberg14, Jessica Castilho15, Catherine McGowan15, Yi-Ming Arthur Chen16, Matthew Law17, Ninon Taylor18, Vassilios Paparizos19, Fabrice Bonnet20,21, Annelies Verbon22, Gerd Fätkenheuer23, Frank A. Post24, Caroline Sabin25, Amanda Mocroft25, Vincent Le Moing26, Fernando Dronda27, Niels Obel28, Sophie Grabar29-31, Vincenzo Spagnuolo32, Andrea Antinori33, Eugenia Quiros-Roldan34, Cristina Mussini35, José M. Miro36, Laurence Meyer37,38, Barbara Hasse39, Deborah Konopnicki40, Bernardino Roca41, Diana Barger21,42, Dorthe Raben43, Gary M. Clifford44, Silvia Franceschi44, Norbert Brockmeyr45, Rana Chakraborty46, Matthias Egger1,47, Julia Bohlius1.
Affiliations. 1Institute of Social and Preventive Medicine, University of Bern, Switzerland; 2CTU Bern, University of Bern, Switzerland; 3National Cancer Registry, National Health Laboratory Service, Johannesburg, South Africa; 4Health Economics and Epidemiology Research Office, Department of Internal Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; 5Department of Medicine, McCord Hospital, Durban, South Africa; 6Médecins Sans Frontières Belgium; 7Johns Hopkins University, School of Medicine, Baltimore, Maryland; 8Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland; 9Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland; 10Center for Global Health, Feinberg School of Medicine, Northwestern University, Chicago; 11University of Calgary, Alberta, Canada; 12University of Washington, School of Medicine, Seattle, Washington; 13Divisions of HIV/AIDS Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia; 14Division of Research, Kaiser Permanente Northern California, Oakland, USA; 15Vanderbilt University Medical Center, Nashville, TN, USA; 16Kaohsiung Medical University, Taiwan; 17Kirby Institute, UNSW Sydney, NSW Australia; 18IIIrd Medical Department with Haematology, Medical Oncology, Haemostaseology, Infectious Diseases and Rheumathology, Oncologic Center, Paracelsus Medical University, Salzburg, Austria; 19AIDS Unit, Clinic of Venereologic and Dermatologic Diseases, Athens Medical School, “Syngros” Hospital, Athens, Greece; 20CHU de Bordeaux, Service de Médecine Interne et Maladies Infectieuses, Hôpital Saint-André, Bordeaux, France; 21INSERM, ISPED, Centre INSERM U1219-Bordeaux Population Health, F-33000 Bordeaux, France; 22Department Medical Microbiology and Infectious Diseases, Erasmus Medical Center, Rotterdam, The Netherlands; 23Department I of Internal Medicine, University Hospital of Cologne, Cologne, Germany; 24King’s College Hospital NHS Foundation Trust, London, UK; 25Research Department of Infection & Population Health, UCL, London, United Kingdom; 26Montpellier University, Montpellier, France; 27Department of Infectious Diseases, Hospital Ramón y Cajal, Madrid, Spain; 28Department of Infectious Diseases, Copenhagen University Hospital, Copenhagen, Denmark; 29Sorbonne Universités, UPMC Univ Paris 06, UMR_S 1136, Institut Pierre Louis d’Epidémiologie et de Santé Publique, F-75013, Paris, France; 30INSERM, UMR_S 1136, Institut Pierre Louis d’Epidémiologie et de Santé Publique, F-75013, Paris, France; 31Université Paris Descartes et Assistance Publique-Hôpitaux de Paris, Groupe hospitalier Cochin Hôtel-Dieu, Paris, France; 32Department of Infectious Diseases, San Raffaele Scientific Institute, Milan, Italy; 33INMI ‘L. Spallanzani’, Rome, Italy; 34Infectious and Tropical Diseases Institute, University of Brescia, Brescia, Italy; 35Infectious Diseases Clinics, University Hospital, Modena, Italy; 36Infectious Diseases Service, Hospital Clinic – IDIBAPS, University of Barcelona, Barcelona, Spain; 37INSERM, U1018, Epidemiology of HIV, Reproduction, Paediatrics, CESP, University Paris-Sud, Paris, France; 38Department of Public Health and Epidemiology, Bicêtre Hospital, AP-HP, Le Kremlin Bicêtre, Paris, France; 39Division of Infectious Diseases and Hospital Epidemiology, University Hospital Zurich, University of Zurich, Switzerland; 40Department of Infectious Diseases, St Pierre University Hospital, Université Libre de Bruxelles, Brussels, Belgium; 41Hospital General Universitario, Castellón, Spain; 42Univ. Bordeaux, ISPED, Centre INSERM U1219-Bordeaux Population Health, F-33000 Bordeaux, France; 43CHIP, Department of Infectious Diseases, Rigshospitalet, Copenhagen, Denmark; 44International Agency for Research on Cancer, Lyon, France; 45Department of Dermatology, Venerology and Allergology, Center for Sexual Health and Medicine, St. Josef Hospital, Ruhr-Universität Bochum, Bochum, Germany; 46Division of Infectious Diseases, Department of Pediatrics, Emory University School of Medicine, Atlanta, USA; 47Centre for Infectious Disease Epidemiology and Research, University of Cape Town, Cape Town, South Africa
Acknowledgements. We thank Christopher Ritter for editorial suggestions.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Financial support. Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases, National Institute of Child Health and Human Development, and the National Cancer Institute of the US National Institutes of Health (grants U01AI069924 [Southern Africa], U01AI069907 [Asia-Pacific], U01AI069923 [Caribbean, Central and South America], U01-AI069918 [North America], and U01A1096186 [IeDEA Network Coordinating Center at Vanderbilt]). The North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) was also supported by the National Institutes of Health (grants F31DA037788, G12MD007583, K01AI093197, K23EY013707, K24AI065298, K24AI118591, K24DA000432, KL2TR000421, M01RR000052, N01CP01004, N02CP055504, N02CP91027, P30AI027757, P30AI027763, P30AI027767, P30AI036219, P30AI050410, P30AI094189, P30AI110527, P30MH62246, R01AA016893, R01CA165937, R01DA011602, R01DA012568, R24AI067039, U01AA013566, U01AA020790, U01AI031834, U01AI034989, U01AI034993, U01AI034994, U01AI035004, U01AI035039, U01AI035040, U01AI035041, U01AI035042, U01AI037613, U01AI037984, U01AI038855, U01AI038858, U01AI042590, U01AI068634, U01AI068636, U01AI069432, U01AI069434, U01AI103390, U01AI103397, U01AI103401, U01AI103408, U01DA03629, U01DA036935, U01HD032632, U10EY008057, U10EY008052, U10EY008067, U24AA020794,U54MD007587, UL1RR024131, UL1TR000004, UL1TR000083, UL1TR000454, UM1AI035043, Z01CP010214, and Z01CP010176), the US Centers for Disease Control and Prevention (contracts CDC-200-2006-18797 and CDC-200-2015-63931), the Agency for Healthcare Research and Quality (contract 90047713), the Health Resources and Services Administration (contract 90051652), the Canadian Institutes of Health Research (grants CBR-86906, CBR-94036, HCP-97105, and TGF-96118), the Ontario Ministry of Health and Long Term Care, and the Government of Alberta, Canada.
Additional support was provided by the National Cancer Institute, National Institute for Mental Health, and National Institute on Drug Abuse. The TREAT Asia HIV Observational Database (TAHOD) and the Australian HIV Observational Database (AHOD) are initiatives of TREAT Asia, a program of amfAR, the Foundation for AIDS Research; AHOD is also funded by unconditional grants from Merck Sharp & Dohme, Gilead Sciences, Bristol-Myers Squibb (BMS), Boehringer Ingelheim, Janssen-Cilag, ViiV Healthcare. The Kirby Institute is funded by the Australian Government Department of Health and Ageing and is affiliated with the Faculty of Medicine, University of New South Wales Australia. The COHERE study group has received unrestricted funding from ANRS, France; HIV Monitoring Foundation, the Netherlands; and the Augustinus Foundation, Denmark.
The research leading to these results has received funding from the European Union Seventh Framework Programme (FP7/2007–2013; EuroCoord grant 260694). A list of the funders of the participating cohorts can be found at www.COHERE.org. JMM received a personal 80:20 research grant from the Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona, Spain during 2017-19. This study was also made possible by the generous support of the American people through the United States Agency for International Development (INROADS USAID-674-A-12-00029) and by the Swiss National Science Foundation (grant Ambizione-PROSPER PZ00P3_160407 to J. B.).
Potential conflicts of interest. A. M. received honoraria, lecture fees, consultancy fees, and travel support from Gilead, BMS, BI, Pfizer, Merck, GSK and Wragge LLC. A. A. received support from Gilead Sciences, Bristol Myers Squibb, Janssen Cilag, Merck, ViiV Healthcare, and Abbvie. C. S. received support from MRC, Gilead Sciences, ViiV Healthcare, and Janssen-Cilag. C. A. is an ABIVAX DSMB member. C. M. received support from BMS, MSD, ViiV, Gilead, and Abbvie. D. B. received funding from Sidaction. F. B. received support from Gilead, Janssen, ViiV Healthcare, BMS, and MSD. G. F. received support from Janssen, BMS, MSD, and Gilead. J. C. is employed by the Vanderbilt University Medical Center, and received support from the NIH. M. J. G. is ad hoc member of HIV National Advisory Boards of Merck, Gilead, and ViiV. J. M. M. received support from Abbvie, BMS, Merck, Novartis, ViiV Healthcare, Genentech, Medtronic, and Pfizer. L. M. received funding from ANRS and FP7 through MRC. M. L. received support from Gilead Sciences, Boehringer Ingelheim, Merck, Sharp & Dohme, Bristol Myers Squibb, Janssen-Cilag, and ViiV Healthcare and DSMB sitting fees from Sirtex Pty Ltd. M. M. received support from the USAID. M. S. received funding from Pfizer and Merck. N. T. has been an advisory board member for GSK, Gilead, and MSD, and received travel support from Gilead and GSK. R. C. received funding from Gilead, the NICHD, and the NIAID. R. M. received payments for the development of educational presentations from Medscape. V. S. received payments for the development of educational presentations from ViiV Healthcare and Gilead Sciences. Y.-M. A. C. received support from the Kaohsiung Medical University and the Ministry of Science and Technology. All other authors report no potential conflicts. The authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
COHERE Steering Committee—contributing cohorts. Ali Judd (AALPHI), Robert Zangerle (AHIVCOS), Giota Touloumi (AMACS), Josiane Warszawski (Agence Nationale de Recherches sur le SIDA et les Hépatites Virales [ANRS] CO1 EPF/ANRS CO11 OBSERVATOIRE EPF), Laurence Meyer (ANRS CO2 SEROCO), François Dabis (ANRS CO3 AQUITAINE), Murielle Mary Krause (ANRS CO4 FHDH), Jade Ghosn (ANRS CO6 PRIMO), Catherine Leport (ANRS CO8 COPILOTE), Linda Wittkop (ANRS CO13 HEPAVIH), Peter Reiss (ATHENA), Ferdinand Wit (ATHENA), Maria Prins (CASCADE), Heiner Bucher (CASCADE), Diana Gibb (CHIPS), Gerd Fätkenheuer (Cologne-Bonn), Julia Del Amo (CoRIS), Niels Obel (Danish HIV Cohort), Claire Thorne (ECS), Amanda Mocroft (EuroSIDA), Ole Kirk (EuroSIDA), Christoph Stephan (Frankfurt), Santiago Pérez-Hoyos (GEMES-Haemo), Osamah Hamouda (German ClinSurv), Barbara Bartmeyer (German ClinSurv), Nikoloz Chkhartishvili (Georgian National HIV/AIDS), Antoni Noguera-Julian (CORISPE-cat), Andrea Antinori (ICC), Antonella d’Arminio Monforte (ICONA), Norbert Brockmeyer (KOMPNET), Luis Prieto (Madrid PMTCT Cohort), Pablo Rojo Conejo (CORISPES-Madrid), Antoni Soriano-Arandes (NENEXP), Manuel Battegay (SHCS), Roger Kouyos (SHCS), Cristina Mussini (Modena Cohort), Pat Tookey (NSHPC), Jordi Casabona (PISCIS), Jose M. Miró (PISCIS), Antonella Castagna (San Raffaele), Deborah Konopnick (St Pierre Cohort), Tessa Goetghebuer (St Pierre Paediatric Cohort), Anders Sönnerborg (Swedish InfCare), Eugenia Quiros-Roldan (Italian Master Cohort), Caroline Sabin (UK CHIC), Ramon Teira (VACH), Myriam Garrido (VACH), and David Haerry (European AIDS Treatment Group).
COHERE Executive Committee. Stéphane de Wit (chair; St Pierre University Hospital), Jose M. Miró (PISCIS), Dominique Costagliola (FHDH), Antonella d’Arminio-Monforte (ICONA), Antonella Castagna (San Raffaele), Julia del Amo (CoRIS), Amanda Mocroft (EuroSida), Dorthe Raben (Head, Copenhagen Regional Coordinating Centre), and Geneviève Chêne (head, Bordeaux Regional Coordinating Centre); pediatric cohort representatives: Ali Judd and Pablo Rojo Conejo.
COHERE regional coordinating centers. Bordeaux: Diana Barger, Christine Schwimmer, Monique Termote, and Linda Wittkop; Copenhagen: Maria Campbell, Casper M. Frederiksen, Nina Friis-Møller, Jesper Kjaer, Dorthe Raben, and Rikke Salbøl Brandt.
COHERE project leads and statisticians. Juan Berenguer, Julia Bohlius, Vincent Bouteloup, Heiner Bucher, Alessandro Cozzi-Lepri, François Dabis, Antonella d’Arminio Monforte, Mary-Anne Davies, Julia del Amo, Maria Dorrucci, David Dunn, Matthias Egger, Hansjakob Furrer, Sophie Grabar, Marguerite Guiguet, Ali Judd, Ole Kirk, Olivier Lambotte, Valériane Leroy, Sara Lodi, Sophie Matheron, Laurence Meyer, Jose M. Miro, Amanda Mocroft, Susana Monge, Fumiyo Nakagawa, Roger Paredes, Andrew Phillips, Massimo Puoti, Eliane Rohner, Michael Schomaker, Colette Smit, Jonathan Sterne, Rodolphe Thiebaut, Claire Thorne, Carlo Torti, Marc van der Valk, and Linda Wittkop.
IeDEA-SA Steering Group. Frank Tanser, Africa Centre for Health and Population Studies, University of Kwazulu-Natal, Somkhele, South Africa; Michael Vinikoor, Centre for Infectious Disease Research in Zambia, Lusaka; Eusebio Macete, Centro de Investigação em Saúde de Manhiça, Manhiça, Mozambique; Robin Wood, Desmond Tutu HIV Centre (Gugulethu and Masiphumelele clinics), Cape Town, South Africa; Kathryn Stinson, Khayelitsha ART Programme and Médecins Sans Frontières, Cape Town, South Africa; Daniela Garone, Khayelitsha ART Programme and Médecins Sans Frontières, Cape Town; Geoffrey Fatti, Kheth’Impilo Programme, South Africa; Sam Phiri, Lighthouse Trust Clinic, Lilongwe, Malawi; Janet Giddy, McCord Hospital, Durban, South Africa; Cleophas Chimbetete, Newlands Clinic, Harare, Zimbabwe; Kennedy Malisita, Queen Elizabeth Hospital, Blantyre, Malawi; Brian Eley, Red Cross War Memorial Children’s Hospital and Department of Paediatrics and Child Health, University of Cape Town; Christiane Fritz, SolidarMed SMART Programme, Lesotho; Michael Hobbins, SolidarMed SMART Programme, Pemba Region, Mozambique; Kamelia Kamenova, SolidarMed SMART Programme, Masvingo, Zimbabwe; Matthew Fox, Themba Lethu Clinic, Johannesburg, South Africa; Hans Prozesky, Tygerberg Academic Hospital, Stellenbosch, South Africa; Karl Technau, Empilweni Clinic, Rahima Moosa Mother and Child Hospital, Johannesburg, South Africa; and Shobna Sawry, Harriet Shezi Children’s Clinic, Chris Hani Baragwanath Hospital, Soweto, South Africa. We also acknowledge colleagues at the National Health Laboratory Service and the National Cancer Registry in South Africa.
NA-ACCORD collaborating cohorts and representatives. AIDS Clinical Trials Group Longitudinal Linked Randomized Trials: Constance A. Benson and Ronald J. Bosch; AIDS Link to the IntraVenous Experience: Gregory D. Kirk; Fenway Health HIV Cohort: Stephen Boswell, Kenneth H. Mayer, and Chris Grasso; HAART Observational Medical Evaluation and Research: Robert S. Hogg, P. Richard Harrigan, Julio S. G. Montaner, Benita Yip, Julia Zhu, Kate Salters, and Karyn Gabler; HIV Outpatient Study: Kate Buchacz, and John T. Brooks; HIV Research Network: Kelly A. Gebo and Richard D. Moore; Johns Hopkins HIV Clinical Cohort: Richard D. Moore; John T. Carey Special Immunology Unit Patient Care and Research Database, Case Western Reserve University: Benigno Rodriguez; Kaiser Permanente Mid-Atlantic States: Michael A. Horberg; Kaiser Permanente Northern California: Michael J. Silverberg; Longitudinal Study of Ocular Complications of AIDS: Jennifer E. Thorne; Multicenter Hemophilia Cohort Study–II: Charles Rabkin; Multicenter AIDS Cohort Study: Joseph B. Margolick, Lisa P. Jacobson, and Gypsyamber D’Souza; Montreal Chest Institute Immunodeficiency Service Cohort: Marina B. Klein; Ontario HIV Treatment Network Cohort Study: Sean B. Rourke, Anita R. Rachlis, and Patrick Cupido; Retrovirus Research Center, Bayamon Puerto Rico: Robert F. Hunter-Mellado and Angel M. Mayor; Southern Alberta Clinic Cohort: M. John Gill; Study of the Consequences of the Protease Inhibitor Era: Steven G. Deeks and Jeffrey N. Martin; Study to Understand the Natural History of HIV/AIDS in the Era of Effective Therapy: Pragna Patel and John T. Brooks; University of Alabama at Birmingham 1917 Clinic Cohort: Michael S. Saag, Michael J. Mugavero and James Willig; University of North Carolina at Chapel Hill HIV Clinic Cohort: Joseph J. Eron and Sonia Napravnik; University of Washington HIV Cohort: Mari M. Kitahata, Heidi M. Crane, and Daniel R. Drozd; Vanderbilt Comprehensive Care Clinic HIV Cohort: Timothy R. Sterling, David Haas, Peter Rebeiro, Megan Turner, Sally Bebawy, and Ben Rogers; Veterans Aging Cohort Study: Amy C. Justice, Robert Dubrow, and David Fiellin; Women’s Interagency HIV Study: Stephen J. Gange and Kathryn Anastos.
NA-ACCORD study administration. Executive Committee: Richard D. Moore, Michael S. Saag, Stephen J. Gange, Mari M. Kitahata, Keri N. Althoff, Michael A. Horberg, Marina B. Klein, Rosemary G. McKaig, and Aimee M. Freeman; Administrative Core: Richard D. Moore, Aimee M. Freeman, and Carol Lent; Data Management Core: Mari M. Kitahata, Stephen E. Van Rompaey, Heidi M. Crane, Daniel R. Drozd, Liz Morton, Justin McReynolds, and William B. Lober; Epidemiology and Biostatistics Core: Stephen J. Gange, Keri N. Althoff, Alison G. Abraham, Bryan Lau, Jinbing Zhang, Jerry Jing, Sharada Modur, Cherise Wong, Brenna Hogan, Fidel Desir, Bin Liu, and Bin You.
IeDEA Caribbean, Central and South America (CCASAnet). Fundación Huésped, Argentina: Pedro Cahn, Carina Cesar, Valeria Fink, Omar Sued, Emanuel Dell’Isola, Hector Perez, Jose Valiente, and Cleyton Yamamoto; Instituto Nacional de Infectologia-Fiocruz, Brazil: Beatriz Grinsztejn, Valdilea Veloso, Paula Luz, Raquel de Boni, Sandra Cardoso Wagner, Ruth Friedman, and Ronaldo Moreira; Universidade Federal de Minas Gerais, Brazil: Jorge Pinto, Flavia Ferreira, Marcelle Maia; Universidade Federal de São Paulo, Brazil: Regina Célia de Menezes Succi, Daisy Maria Machado, and Aida de Fátima Barbosa Gouvêa; Fundación Arriarán, Chile: Marcelo Wolff, Claudia Cortes, Maria Fernanda Rodriguez, and Gladys Allendes; Les Centres GHESKIO, Haiti: Jean William Pape, Vanessa Rouzier, Adias Marcelin, and Christian Perodin; Hospital Escuela Universitario, Honduras: Marco Tulio Luque; Instituto Hondureño de Seguridad Social, Honduras: Denis Padgett; Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico: Juan Sierra Madero, Brenda Crabtree Ramirez, Paco Belaunzaran, and Yanink Caro Vega; Instituto de Medicina Tropical Alexander von Humboldt, Peru: Eduardo Gotuzzo, Fernando Mejia, and Gabriela Carriquiry; Vanderbilt University Medical Center: Catherine C. McGowan, Bryan E. Shepherd, Timothy Sterling, Karu Jayathilake, Anna K. Person, Peter F. Rebeiro, Mark Giganti, Jessica Castilho, Stephany N. Duda, Fernanda Maruri, and Hilary Vansell.
TREAT Asia HIV Observational Database (TAHOD) study members. P. S. Ly (TAHOD Steering Committee member [TSC]) and V. Khol, National Center for HIV/AIDS, Dermatology and STDs, Phnom Penh, Cambodia; F. J. Zhang (TSC and TAHOD Steering Committee cochair), H. X. Zhao and N. Han, Beijing Ditan Hospital, Capital Medical University, Beijing, China; M. P. Lee (TSC), P. C. K. Li, W. Lam, and Y. T. Chan, Queen Elizabeth Hospital, Hong Kong, China; N. Kumarasamy (TSC), S. Saghayam and C. Ezhilarasi, Chennai Antiviral Research and Treatment Clinical Research Site (CARTCRS), YRGCARE Medical Centre, VHS, Chennai, India; S. Pujari (TSC), K. Joshi, S. Gaikwad, and A. Chitalikar, Institute of Infectious Diseases, Pune, India; T. P. Merati (TSC), D. N. Wirawan, and F. Yuliana, Faculty of Medicine, Udayana University and Sanglah Hospital, Bali, Indonesia; E. Yunihastuti (TSC), D. Imran and A. Widhani, Faculty of Medicine Universitas Indonesia–Dr Cipto Mangunkusumo General Hospital, Jakarta, Indonesia; J. Tanuma (TSC), S. Oka and T. Nishijima, National Center for Global Health and Medicine, Tokyo, Japan; J. Y. Choi (TSC), S. Na, and J. M. Kim, Division of Infectious Diseases, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, South Korea; B. L. H. Sim (TSC), Y. M. Gani, and R. David, Hospital Sungai Buloh, Sungai Buloh, Malaysia; A. Kamarulzaman (TSC), S. F. Syed Omar, S. Ponnampalavanar, and I. Azwa, University Malaya Medical Centre, Kuala Lumpur, Malaysia; R. Ditangco (TSC), E. Uy, and R, Bantique, Research Institute for Tropical Medicine, Manila, Philippines; W. W. Wong (TSC and TAHOD Steering Committee chair), W. W. Ku, and P. C. Wu, Taipei Veterans General Hospital, Taipei, Taiwan; O. T. Ng (TSC), P. L. Lim, L. S. Lee, and P. S. Ohnmar, Tan Tock Seng Hospital, Singapore; A. Avihingsanon (TSC), S. Gatechompol, P. Phanuphak, and C. Phadungphon, HIV-NAT/Thai Red Cross AIDS Research Centre, Bangkok, Thailand; S. Kiertiburanakul (TSC), S. Sungkanuparph, L. Chumla, and N. Sanmeema, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; R. Chaiwarith (TSC), T. Sirisanthana, W. Kotarathititum, and J. Praparattanapan, Research Institute for Health Sciences, Chiang Mai, Thailand; P. Kantipong (TSC) and P. Kambua, Chiangrai Prachanukroh Hospital, Chiang Rai, Thailand; W. Ratanasuwan (TSC) and R. Sriondee, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand; K. V. Nguyen (TSC), H. V. Bui, D. T. H. Nguyen, and D. T. Nguyen, National Hospital for Tropical Diseases, Hanoi, Vietnam; D. D. Cuong (TSC), N. V. An and N. T. Luan, Bach Mai Hospital, Hanoi; A. H. Sohn (TSC), J. L. Ross (TSC), and B. Petersen, TREAT Asia, amfAR–Foundation for AIDS Research, Bangkok, Thailand; D. A. Cooper, M. G. Law (TSC), A. Jiamsakul (TSC), and D. C. Boettiger, Kirby Institute, University of New South Wales, Australia, Sydney, Australia.
Australian HIV Observational Database (AHOD) study members. New South Wales: D. Ellis, Coffs Harbour Medical Centre, Coffs Harbour; M. Bloch, S. Agrawal, and T. Vincent, Holdsworth House Medical Practice, Sydney; D. Allen, Holden Street Clinic, Gosford; D. Smith, A. Rankin, Lismore Sexual Health and AIDS Services, Lismore; D. Baker (AHOD Steering Committee member [ASC]), East Sydney Doctors, Surry Hills; D. J. Templeton (ASC), C. C. O’Connor, and O. Thackeray, RPA Sexual Health, Camperdown; E. Jackson and K. McCallum, Blue Mountains Sexual Health and HIV Clinic, Katoomba; N. Ryder and G. Sweeney, Clinic 468, HNE Sexual Health, Tamworth; D. Cooper, A. Carr, K. Macrae, and K. Hesse, St Vincent’s Hospital, Darlinghurst; R. Finlayson and S. Gupta, Taylor Square Private Clinic, Darlinghurst; J. Langton-Lockton and J. Shakeshaft, Nepean Sexual Health and HIV Clinic, Penrith; K. Brown, S. Idle, and N. Arvela, Illawarra Sexual Health Service, Warrawong; R. Varma and H. Lu, Sydney Sexual Health Centre, Sydney; D. Couldwell and S. Eswarappa, Western Sydney Sexual Health Clinic; D. E. Smith (ASC), V. Furner, D. Smith, and G. Cabrera, Albion Street Centre; S. Fernando, Clinic 16–Royal North Shore Hospital; A. Cogle (ASC), National Association of People living with HIV/AIDS; C. Lawrence (ASC), National Aboriginal Community Controlled Health Organisation; B. Mulhall (ASC), Department of Public Health and Community Medicine, University of Sydney; M. Boyd (ASC), University of Adelaide; M. Law (ASC), K. Petoumenos (ASC), R. Puhr (ASC), R. Huang (ASC), and A. Han (ASC), Kirby Institute, University of New South Wales. Northern Territory: M. Gunathilake, R. Payne, Communicable Disease Centre, Darwin. Queensland: M. O’Sullivan and A. Croydon, Gold Coast Sexual Health Clinic, Miami; D. Russell, C. Cashman, and C. Roberts, Cairns Sexual Health Service, Cairns; D. Sowden, K. Taing, and P. Marshall, Clinic 87, Sunshine Coast-Wide Bay Health Service District, Nambour; D. Orth and D. Youds, Gladstone Road Medical Centre, Highgate Hill; D. Rowling, N. Latch, and E. Warzywoda, Sexual Health and HIV Service in Metro North, Brisbane; B. Dickson (ASC), CaraData. South Australia: W. Donohue, O’Brien Street General Practice, Adelaide: Victoria: R. Moore, S. Edwards, and S. Boyd, Northside Clinic, North Fitzroy; N. J. Roth (ASC) and H. Lau, Prahran Market Clinic, South Yarra; T. Read and J. Silvers (ASC), W. Zeng, Melbourne Sexual Health Centre, Melbourne; J. Hoy (ASC), K. Watson (ASC), M. Bryant, and S. Price, The Alfred Hospital, Melbourne; I. Woolley, M. Giles (ASC), T. Korman, and J. Williams (ASC), Monash Medical Centre, Clayton. Western Australia: D. Nolan, A. Allen, and G. Guelfi, Department of Clinical Immunology, Royal Perth Hospital. New Zealand: G. Mills and C. Wharry, Waikato District Hospital Hamilton; N. Raymond, K. Bargh, Wellington Hospital. Cause of death reviewers: D. Templeton, M. Giles, K. Brown, and J. Hoy.
Contributor Information
The AIDS-defining Cancer Project Working Group for IeDEA and COHERE in EuroCoord:
Eliane Rohner, Lukas Bütikofer, Kurt Schmidlin, Mazvita Sengayi, Mhairi Maskew, Janet Giddy, Daniela Garone, Richard D Moore, Gypsyamber D’Souza, James J Goedert, Chad Achenbach, M John Gill, Mari M Kitahata, Pragna Patel, Michael J Silverberg, Jessica Castilho, Catherine McGowan, Yi-Ming Arthur Chen, Matthew Law, Ninon Taylor, Vassilios Paparizos, Fabrice Bonnet, Annelies Verbon, Gerd Fätkenheuer, Frank A Post, Caroline Sabin, Amanda Mocroft, Vincent Le Moing, Fernando Dronda, Niels Obel, Sophie Grabar, Vincenzo Spagnuolo, Andrea Antinori, Eugenia Quiros-Roldan, Cristina Mussini, José M Miro, Laurence Meyer, Barbara Hasse, Deborah Konopnicki, Bernardino Roca, Diana Barger, Dorthe Raben, Gary M Clifford, Silvia Franceschi, Norbert Brockmeyr, Rana Chakraborty, Matthias Egger, and Julia Bohlius
References
- 1. Semeere AS, Busakhala N, Martin JN. Impact of antiretroviral therapy on the incidence of Kaposi’s sarcoma in resource-rich and resource-limited settings. Curr Opin Oncol 2012; 24:522–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sengayi M, Spoerri A, Egger M et al. . Record linkage to correct under-ascertainment of cancers in HIV cohorts: the Sinikithemba HIV clinic linkage project. Int J Cancer 2016; 139:1209–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Semeere A, Wenger M, Busakhala N et al. . A prospective ascertainment of cancer incidence in sub-Saharan Africa: the case of Kaposi sarcoma. Cancer Med 2016; 5:914–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yanik EL, Napravnik S, Cole SR et al. . Incidence and timing of cancer in HIV-infected individuals following initiation of combination antiretroviral therapy. Clin Infect Dis 2013; 57:756–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cancer Project Working Group for the Collaboration of Observational HIV Epidemiological Research Europe (COHERE) study in EuroCoord. Changing incidence and risk factors for Kaposi sarcoma by time since starting antiretroviral therapy: collaborative analysis of 21 European cohort studies. Clin Infect Dis 2016; 63:1373–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Moore PS, Chang Y. Detection of herpesvirus-like DNA sequences in Kaposi’s sarcoma in patients with and those without HIV infection. N Engl J Med 1995; 332:1181–5. [DOI] [PubMed] [Google Scholar]
- 7. Bhutani M, Polizzotto MN, Uldrick TS, Yarchoan R. Kaposi sarcoma-associated herpesvirus-associated malignancies: epidemiology, pathogenesis, and advances in treatment. Semin Oncol 2015; 42:223–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guiguet M, Boué F, Cadranel J, Lang JM, Rosenthal E, Costagliola D; Clinical Epidemiology Group of the FHDH-ANRS CO4 cohort Effect of immunodeficiency, HIV viral load, and antiretroviral therapy on the risk of individual malignancies (FHDH-ANRS CO4): a prospective cohort study. Lancet Oncol 2009; 10:1152–9. [DOI] [PubMed] [Google Scholar]
- 9. Lacombe JM, Boue F, Grabar S et al. . Risk of Kaposi sarcoma during the first months on combination antiretroviral therapy. AIDS 2013; 27:635–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lodi S, Guiguet M, Costagliola D, Fisher M, de Luca A, Porter K; CASCADE Collaboration Kaposi sarcoma incidence and survival among HIV-infected homosexual men after HIV seroconversion. J Natl Cancer Inst 2010; 102:784–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. IeDEA and ART Cohort Collaborations ; Avila D, Althoff KN, Mugglin C et al. . Immunodeficiency at the start of combination antiretroviral therapy in low-, middle-, and high-income countries. J Acquir Immune Defic Syndr 2014; 65:e8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gange SJ, Kitahata MM, Saag MS et al. . Cohort profile: the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD). Int J Epidemiol 2007; 36:294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McGowan CC, Cahn P, Gotuzzo E et al. . Cohort profile: Caribbean, Central and South America Network for HIV research (CCASAnet) collaboration within the International Epidemiologic Databases to Evaluate AIDS (IeDEA) programme. Int J Epidemiol 2007; 36:969–76. [DOI] [PubMed] [Google Scholar]
- 14. Egger M, Ekouevi DK, Williams C et al. . Cohort profile: the international epidemiological databases to evaluate AIDS (IeDEA) in sub-Saharan Africa. Int J Epidemiol 2012; 41:1256–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. IeDEA (International Epidemiology Databases to Evaluate AIDS). Asia-Pacific. Available at: http://www.iedea.org/regions/asia-pacific. Accessed 24 February 2017.
- 16. Chêne G, Phillips A, Costagliola D et al. . Cohort profile: Collaboration of Observational HIV Epidemiological Research Europe (COHERE) in EuroCoord [Epub ahead of print]. Int J Epidemiol 2016. doi:10.1093/ije/dyw211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. 1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep 1992; 41:1–19. [PubMed] [Google Scholar]
- 18. Royston P, Lambert P.. Flexible parametric survival analysis using Stata: beyond the Cox model (ed 1). College Station, TX: StataCorp, 2011. [Google Scholar]
- 19. Rohner E, Valeri F, Maskew M et al. . Incidence rate of Kaposi sarcoma in HIV-infected patients on antiretroviral therapy in Southern Africa: a prospective multicohort study. J Acquir Immune Defic Syndr 2014; 67:547–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Letang E, Almeida JM, Miró JM et al. . Predictors of immune reconstitution inflammatory syndrome-associated with Kaposi sarcoma in Mozambique: a prospective study. J Acquir Immune Defic Syndr 2010; 53:589–97. [DOI] [PubMed] [Google Scholar]
- 21. Franceschi S, Maso LD, Rickenbach M et al. . Kaposi sarcoma incidence in the Swiss HIV Cohort Study before and after highly active antiretroviral therapy. Br J Cancer 2008; 99:800–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ablashi D, Chatlynne L, Cooper H et al. . Seroprevalence of human herpesvirus-8 (HHV-8) in countries of Southeast Asia compared to the USA, the Caribbean and Africa. Br J Cancer 1999; 81:893–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Asiimwe F, Moore D, Were W et al. . Clinical outcomes of HIV-infected patients with Kaposi’s sarcoma receiving nonnucleoside reverse transcriptase inhibitor-based antiretroviral therapy in Uganda. HIV Med 2012; 13:166–71. [DOI] [PubMed] [Google Scholar]
- 24. Martin J, Wenger M, Busakhala N et al. . Prospective evaluation of the impact of potent antiretroviral therapy on the incidence of Kaposi’s Sarcoma in East Africa: findings from the International Epidemiologic Databases to Evaluate AIDS (IeDEA) Consortium. Infect Agent Cancer 2012; 7:O19. [Google Scholar]
- 25. Suárez-García I, Jarrín I, Iribarren JA et al. . Incidence and risk factors of AIDS-defining cancers in a cohort of HIV-positive adults: importance of the definition of incident cases. Enferm Infecc Microbiol Clin 2013; 31:304–12. [DOI] [PubMed] [Google Scholar]
- 26. Maskew M, MacPhail AP, Whitby D, Egger M, Fox MP. Kaposi sarcoma-associated herpes virus and response to antiretroviral therapy: a prospective study of HIV-infected adults. J Acquir Immune Defic Syndr 2013; 63:442–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ziegler JL, Katongole-Mbidde E, Wabinga H, Dollbaum CM. Absence of sex-hormone receptors in Kaposi’s sarcoma. Lancet 1995; 345:925. [DOI] [PubMed] [Google Scholar]
- 28. Ruocco E, Ruocco V, Tornesello ML, Gambardella A, Wolf R, Buonaguro FM. Kaposi’s sarcoma: etiology and pathogenesis, inducing factors, causal associations, and treatments: facts and controversies. Clin Dermatol 2013; 31: 413–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Simonart T. Role of environmental factors in the pathogenesis of classic and African-endemic Kaposi sarcoma. Cancer Lett 2006; 244:1–7. [DOI] [PubMed] [Google Scholar]
- 30. Dukers NH, Rezza G. Human herpesvirus 8 epidemiology: what we do and do not know. AIDS 2003; 17:1717–30. [DOI] [PubMed] [Google Scholar]
- 31. Mutyaba I, Phipps W, Krantz EM et al. . A population-level evaluation of the effect of antiretroviral therapy on cancer incidence in Kyadondo County, Uganda, 1999–2008. J Acquir Immune Defic Syndr 2015; 69:481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dryden-Peterson S, Medhin H, Kebabonye-Pusoentsi M et al. . Cancer incidence following expansion of HIV treatment in Botswana. PLoS One 2015; 10:e0135602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Krown SE, Lee JY, Dittmer DP; AIDS Malignancy Consortium. More on HIV-associated Kaposi’s sarcoma. N Engl J Med 2008; 358:535–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Yanik EL, Achenbach CJ, Gopal S et al. . Changes in clinical context for Kaposi’s sarcoma and non-Hodgkin lymphoma among people with HIV infection in the United States. J Clin Oncol 2016; 34:3276–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.