Abstract
In this study, ticks from pastoral communities in Kenya were tested for Rickettsia spp. infections in geographical regions where the presence of tick-borne arboviruses had previously been reported. Rickettsial and arbovirus infections have similar clinical features which makes differential diagnosis challenging when both diseases occur. The tick samples were tested for Rickettsia spp. by conventional PCR using three primer sets targeting the gltA, ompA, and ompB genes followed by amplicon sequencing. Of the tick pools screened, 25% (95/380) were positive for Rickettsia spp. DNA using the gltA primer set. Of the tick-positive pools, 60% were ticks collected from camels. Rickettsia aeschlimannii and R. africae were the main Rickettsia spp. detected in the tick pools sequenced. The findings of this study indicate that multiple Rickettsia species are circulating in ticks from pastoral communities in Kenya and could contribute to the etiology of febrile illness in these areas. Diagnosis and treatment of rickettsial infections should be a public health priority in these regions.
Keywords: Rickettsia, pastoral, tick, gltA, diagnosis
Rickettsioses are caused by bacteria in the order Rickettsiales and the genus Rickettsia. The Rickettsia genus is divided into four groups: spotted fever group (SFG), the transitional group (TRG), typhus group (TG), and the ancestral group (AG; Gillespie et al. 2008). Rickettsioses mainly cause fever, malaise, arthralgia, lymphadenopathy, myalgia, and headaches in humans (La Scola and Raoult 1997). An inoculation eschar may be absent or present and clinical manifestations vary between species of Rickettsia (Faccini-Martínez et al. 2014). The same spectrum of clinical symptoms are observed in other diseases such as malaria, influenza, and typhoid fever (Richards et al. 2010), making empirical diagnosis of Rickettsia infection difficult. Rickettsial infections are easily and affordably treated with antibiotics such as doxycycline or chloramphenicol (Huntzinger 2007), so accurate diagnosis can lead to significant reduction in the associated morbidity. Ticks are the main vectors and reservoirs of the SFG Rickettsiae, and they transmit the infection to domestic animals, wildlife, and humans (Raoult and Roux 1997). There is a growing body of evidence indicating the widespread presence of Rickettsia spp. in ticks, vertebrate hosts, and humans in Kenya. Antibodies against R. conorii were detected in rodents from Machakos, Kerugoya, Kisumu, Nairobi and the Rift Valley (Heisch et al. 1962). In addition, several Rickettsia spp. have been detected in ticks and whole blood collected from domestic animals at two major slaughter houses in Kenya (Mutai et al. 2013). Rickettsiaafricae was detected in ticks collected from domestic animals and wildlife in Kenya at the Maasai Mara and the Shimba hill reserves (Macaluso et al. 2003, Mwamuye et al. 2016) and R. africae variants detected in ticks from rural Western Kenya. In a recent study, the heterogeneity of R. africae was confirmed and a new Rickettsia species identified that had been collected from the northern part of Kenya where communities are mainly nomads (Kimita et al. 2016). Nomadic communities in Kenya live in arid and semiarid zones and practice pastoralism with herds predominantly consisting of sheep, goats, and camels. Ticks found on these livestock potentially play a role in the transmission dynamics of tick-borne diseases (Pfaffle et al. 2013). Since these nomadic communities in Kenya interact closely with their livestock and are at risk of exposure to ticks, they could also be at high risk of acquiring tick-borne infections. This is consistent with reports that have identified zoonotic diseases such as Crimean Congo hemorrhagic fever virus and Rift Valley fever virus in these pastoral communities (LaBeaud et al. 2008, Lwande et al. 2012, Lwande et al. 2013). Few studies in Kenya have examined the burden of rickettsial infections in these nomadic communities in spite of the presence of these risk indicators. Unfortunately, many rickettsial diseases would be difficult to recognize in these communities because of the generalized clinical presentation and lack of routine or robust diagnostics for febrile illnesses in the local hospitals (Richards et al. 2010). Consequently, a study nested within the arbovirus surveillance program run by the US Army Medical Research Directorate-Kenya and the Arbovirus Incidence and Diversity project in KEMRI was undertaken to determine the prevalence of Rickettsia in tick population in nomadic communities and to identify associated animal reservoirs and tick species that could be vectors for human transmission. Several sites in Kenya were studied to examine geographic differences in Rickettsia species distribution and to identify the potential risk of tick-borne rickettsial infections.
Materials and Methods
Study Sites
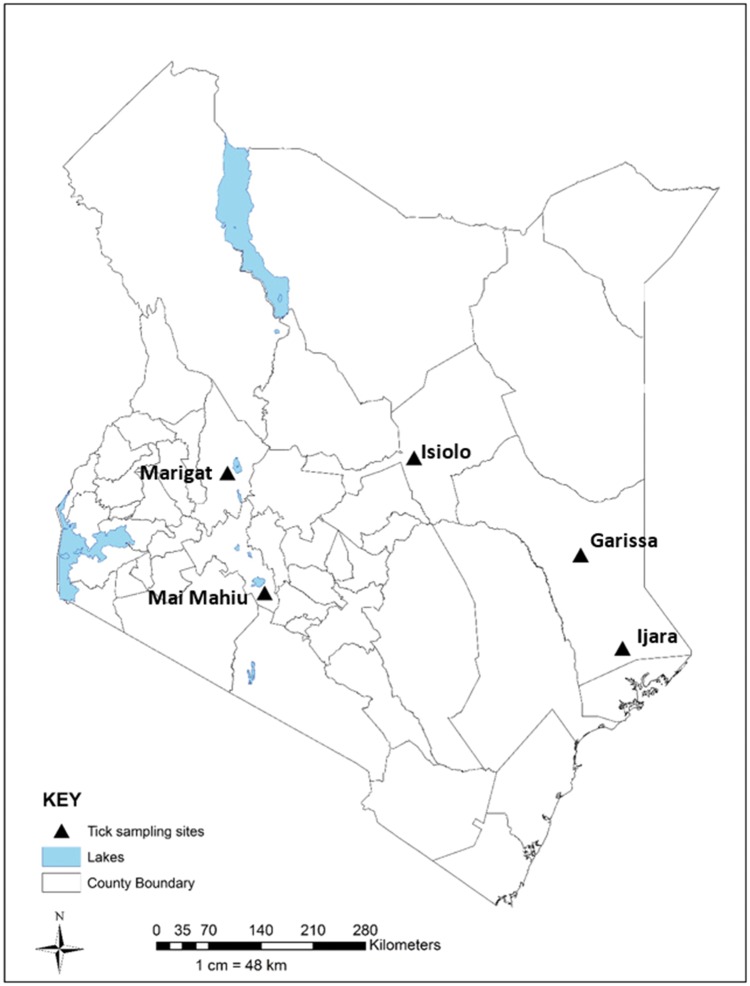
The study sites were selected because they fall within the arid and semiarid zones where most communities practice pastoral farming (Lwande et al. 2013), and where tick-borne zoonotic diseases have been previously reported (Sang et al. 2011, Lwande et al. 2012). The five sites were Garissa and Ijara, both located in Garissa County, Mai Mahiu located in Nakuru County, Marigat located in Baringo County, and Isiolo in Isiolo County (Fig. 1).
Fig. 1.
Map of Kenya showing the sites where tick samples were collected.
Tick Pool Samples
All the 380 tick pools tested in this study were collected in 2006–2011, from livestock in the five study sites. Whole adult ticks had been identified to the species level using two tick identification keys (Matthysse and Colbo 1987, Okello-Onen et al.1999). The ticks were then pooled in groups of 1 to 8 according to sex, developmental stage, species, area, site, collection date, and host. Each tick pool was placed in a prechilled sterile mortar and homogenized in 90-mesh alundum (Thermo Fisher Scientific, Fair Lawn, NJ) with a pestle. The homogenization media contained 2 ml minimum essential medium, constituting 15% fetal bovine serum, 2% l-glutamine, and 2% antibiotic and antimycotic (100 U/ml penicillin, 100 µg/ml streptomycin, and 1 µl/ml fungizone; Sigma-Aldrich, St. Louis, MO; Lutomiah et al. 2014). Homogenates were clarified by low speed centrifugation (5590 × g) and the supernatants stored at −70 to −80 °C until tested.
DNA Extraction and Polymerase Chain Reaction Amplification
DNA was extracted from the tick homogenates using the Qiagen DNeasy Blood and Tissue kit (Qiagen Inc., Valencia, CA). The DNA was quantified using a Nanodrop 2000 spectrophotometer (Thermo Fisher scientific) and stored at −70 to −80°C. The SFG Rickettsia was detected by a single-step PCR assay using the primers CS78 and CS323 targeting a 401 bp fragment of the citrate synthase gene (gltA). The following PCR cycling condition were used, 95°C for 3 min followed by 40 cycles of 95°C for 15 s, 55°C for 30 s, 72°C for 30 s and a final extension at 72°C for 7 min (Labruna et al. 2004, Ndip et al. 2004). The DNA of Rickettsia africae was used as a positive control and water was used as a negative control. Fetal bovine serum was also tested to determine that it was free of rickettsial DNA. Further analysis of the positive samples was performed by PCR amplification of the Rickettsia outer membrane protein genes using primer ompA (532bp) and a nested primer set for the ompB gene (≈420bp-SFG) and (≈230bp-TG). For the ompA primer, the following conditions were used, 94°C for 5 min followed by 94°C for 30 s, 58°C for 1 min, 72°C for 2 min, for 35 cycles, and a final extension at 72°C for 5 min (Regnery et al. 1991). The following conditions were used in the outer ompB PCR reaction. An initial denaturation step at 95 °C for 5 min, followed by 35 cycles of 95 °C for 15 s, 54 °C for 15 s, and 72 °C for 30 s, and a final extension at 72 °C for 3 min. The nested PCR cycle was 95 °C for 5 min, followed by 35 cycles of 95 °C for 15 s, 56 °C for 15 s, and 72 °C for 30 s, and a final extension at 72 °C for 3 min (Choi et al. 2005).
The PCR assays were performed in a Gene Amp PCR system 9700 thermal cycler (Applied Biosystems) using Taq PCR master mix (Qiagen Inc.,Valencia, CA), 1 ng of template DNA, and 1 μl each of 20 μM of the gltA, ompA, and outer ompB primers pairs in a total volume of 25 μl. The nested PCR reaction mix contained 1 μl of 10 μM of the inner ompB primers in a 25μl reaction volume. PCR products were separated on a 2% agarose gel along with a reference 100bp DNA ladder (Thermo Fisher scientific) and visualized with ethidium bromide on a UV transilluminator.
Sequencing and Phylogenetic Analysis
The PCR products were purified using the QIAquick PCR Purification Kit (Qiagen Inc., Valencia, CA) according to the manufacturer’s instructions and sequenced directly using the Sanger chain termination method.
The resulting sequence fragments were assembled into contigs using DNA base version 3.2 by Heracle Biosoft (Stucky 2012). Preliminary identification of the specific Rickettsia species was performed using the online Basic Local Alignment Search Tool (BLASTn) (Madden 2013). Subsequently, the gltA, ompA, and ompB gene sequences were aligned separately using the Muscle v3.8 software (Edgar 2004) and compared to reference strain sequences from GenBank. Nucleotide sequences of gltA, OmpA, and OmpB genes reported in this study are available in GenBank under accession numbers: KX227772 to KX227792.
Statistical Analysis
Statistical analysis was performed using the R statistical software-R version 3.1.0 (RCoreTeam 2014). Chi-square test was used to detect any differences between the distributions of outcomes in different groups. A P value of < 0.05 was considered significant.
Results
Prevalence of Rickettsia spp. in Ticks
Of the 380 tick pools tested, 25% (95% CI 20.72–29.67%) were positive for Rickettsia using the gltA primer set. The prevalence of Rickettsia varied significantly across the sites (Chi Sq = 42.25, df =4, P < 0.0001), with Garissa recording the highest prevalence (52.63%), followed by Isiolo (25%), Marigat (19.7%), Ijara (14.5%), and Mai Mahiu (13.16%). The number of tick pools positive for Rickettsia also varied significantly with animal host (Chi Sq = 34.21, df =3, P < 0.0001). The highest number of tick pools positive for Rickettsia were collected from camels (60%), followed by cattle (31.37%), sheep (16.67%), and goats (13.74%).
All gltA-positive tick pool samples were subsequently tested using the outer membrane protein primers (ompA and ompB). A total of 21 (22.1%) tick pools were positive for the ompA gene and 27 (28.4%) were positive for the ompB gene while 16.8% of these tick pools were both ompA and ompB positive.
Distribution of Tick Species and Rickettsia spp.-Positive Ticks
There were 12 tick species identified from the total tick collection from the five sites. Ijara had the greatest diversity of tick species (8) followed by Garissa (7), Isiolo (4), Mai Mahiu (5), and Marigat (5) (Table 1). Only two species (Rhipicephalus pulchellus and Amblyomma gemma) were found across all five sites. The most abundant tick species was Rh. pulchellus which constituted more than half (53%, n = 201) of all the ticks sampled. Some of the tick species could not be fully identified to species level, as some body parts were missing. Rickettsiae-positive ticks were predominantly from three genera—Hyalomma (76.9%), Amblyomma (44.8%), and Rhipicephalus (14%).
Table 1.
Distribution of tick species for each collection site
| Species | Garissa |
Ijara |
Isiolo |
Mai mahiu |
Marigat |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. ticks | %ticks | No. ticks | %ticks | No. ticks | %ticks | No. ticks | %ticks | No. ticks | %ticks | |
| Rh. pulchellus | 34 | 44.7 | 55 | 72.4 | 68 | 89.5 | 1 | 1.3 | 43 | 56.6 |
| Rh.evertsi evertsi | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 65 | 85.5 | 3 | 3.9 |
| H. truncatum | 21 | 27.6 | 4 | 5.3 | 3 | 3.9 | 0 | 0.0 | 1 | 1.3 |
| Rh. appendiculatus | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 | 28 | 36.8 |
| A.gemma | 6 | 7.9 | 5 | 6.6 | 4 | 5.3 | 1 | 1.3 | 1 | 1.3 |
| H. marginatum | 5 | 6.6 | 2 | 2.6 | 0 | 0.0 | 8 | 10.5 | 0 | 0.0 |
| Hyalomma spp. | 7 | 9.2 | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| A.lepidum | 0 | 0.0 | 7 | 9.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| A.variegatum | 2 | 2.6 | 0 | 0.0 | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 |
| A.hebraeum | 0 | 0.0 | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 |
| Amblyomma spp. | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Rh. annulatus | 0 | 0.0 | 1 | 1.3 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
A: Amblyomma, H: Hyalomma, Rh: Rhipicephalus.
Rickettsia spp. Identified From the PCR-Positive Tick Pool Samples
The 23 gltA, 21 OmpA, and 27 OmpB amplicons from tick pools were successfully sequenced and compared to those available in GenBank database using BLASTn analyses. The Rickettsia spp. detected in the gltA-positive tick pools were predominantly R. aeschlimannii or R. africae.Rickettsiaraoultii (n = 4) was also detected, with a single pool each positive for R. sibirica and R. conorii subsp. israelensis. A BLASTn search showed that the OmpA nucleotide sequences of the tick pools exhibited homology to those of R. aeschlimannii (n = 14), R. africae (n = 6), and R. monglotimonae (n = 1) species. Likewise, OmpB sequences of the tick pools showed homology to R. aeschlimannii (n = 14), R. raoultii (n = 1), R. montanensis (n = 1), R. africae (n = 7), and R. parkeri (n = 4). (Sequence homologies ranged from 97–100%). Only seven tick pools were successfully amplified using the three primers (gltA, ompA, and ompB). For five of the tick pools sequences, a consensus identity was obtained with sequence homology to R. aeschlimannii. However, consensus sequence identity was not obtained for two of the seven tick pool samples; different species were detected with each of the three primer sets (Table 2).
Table 2.
Rickettsial species detected in tick pools by PCR and sequencing of gltA, OmpA, and OmpB genes of rickettsial species
| Sample tested | Site | Host | gltA | OmpA | OmpB |
|---|---|---|---|---|---|
| H. truncatum | Garissa | Camel | ns | R. africae | R. parkeri |
| H. truncatum | Garissa | Camel | ns | R. aeschlimannii | R. aeschlimannii |
| H. truncatum | Garissa | Cattle | R. aeschlimannii | R. aeschlimannii | R. aeschlimannii |
| H. truncatum | Garissa | Cattle | ns | R. aeschlimannii | R. aeschlimannii |
| H. truncatum | Garissa | Camel | ns | R. aeschlimannii | R. aeschlimannii |
| H. truncatum | Garissa | Camel | R. aeschlimannii | R. aeschlimannii | R. aeschlimannii |
| H. truncatum | Garissa | Cattle | ns | R. aeschlimannii | R. aeschlimannii |
| Hyalomma spp. | Garissa | Camel | ns | R. aeschlimannii | R. aeschlimannii |
| Hyalomma spp. | Garissa | Camel | ns | R. monglotimonae | R. parkeri |
| H. truncatum | Garissa | Cattle | ns | R. aeschlimannii | R. aeschlimannii |
| Hyalomma spp. | Garissa | Camel | R. aeschlimannii | R. aeschlimannii | na |
| A. gemma | Garissa | Camel | R. africae | R. africae | R. africae |
| H. truncatum | Garissa | Camel | ns | na | R. africae |
| H. truncatum | Garissa | Sheep | ns | na | R. parkeri |
| H. truncatum | Garissa | Cattle | ns | na | R. africae |
| H. truncatum | Garissa | Cattle | ns | na | R. aeschlimannii |
| H. truncatum | Garissa | Cattle | ns | na | R. aeschlimannii |
| H. marginatum | Garissa | Cattle | ns | na | R. aeschlimannii |
| Rh. appendiculatus | Garissa | Cattle | ns | na | R. montanensis |
| H. truncatum | Garissa | Camel | R. aeschlimannii | na | R. aeschlimannii |
| Rh. pulchellus | Garissa | Cattle | R. aeschlimannii | na | na |
| H. truncatum | Garissa | Camel | R. aeschlimannii | na | na |
| Rh. pulchellus | Garissa | Cattle | R. raoultii | na | na |
| A. lepidum | Ijara | Goat | R. africae | R. africae | R. africae |
| Rh. pulchellus | Ijara | Camel | ns | R. africae | R. parkeri |
| Hyalomma spp. | Ijara | Camel | R. sibirica | R. africae | R. aeschlimannii |
| H. marginatum | Ijara | Cattle | R. aeschlimannii | R. aeschlimannii | R. aeschlimannii |
| H. marginatum | Ijara | Cattle | R. raoultii | R. aeschlimannii | na |
| A. lepidum | Ijara | Goat | R. africae | na | na |
| A. gemma | Isiolo | Camel | R. aeschlimannii | R. africae | R. africae |
| A. gemma | Isiolo | Cattle | R. africae | R. africae | na |
| A. gemma | Isiolo | Sheep | R. raoultii | na | R. africae |
| Rh. pulchellus | Isiolo | Goat | R. aeschlimannii | na | na |
| Rh. pulchellus | Isiolo | Goat | R. raoultii | na | na |
| H. marginatum | Mai Mahiu | Cattle | R. aeschlimannii | na | na |
| H. marginatum | Mai Mahiu | Cattle | R. aeschlimannii | R. aeschlimannii | na |
| A. variegatum | Mai Mahiu | Cattle | R. aeschlimannii | na | R. africae |
| H. marginatum | Mai Mahiu | Goat | ns | R. aeschlimannii | na |
| Rh. appendiculatus | Marigat | Sheep | ns | na | R. raoultii |
| Rh. appendiculatus | Marigat | Sheep | R. coronii subsp Israelensis | na | na |
| A. gemma | Marigat | Cattle | R. africae | na | na |
A: Amblyomma, H: Hyalomma, Rh: Rhipicephalus, R: Rickettsia, ns: not sequenced, na: no amplification.
Discussion
Rickettsia spp. Prevalence in Ticks
We were able to demonstrate a high prevalence (25%) of Rickettsia infection in tick pools obtained from livestock at five geographically dispersed sites in Kenya, with Rickettsiae-positive ticks being found at every site. The prevalence is similar to that found in a study that examined ticks from cattle, sheep, and goats originating from counties across Kenya at two major slaughter houses (Mutai et al. 2013). This confirms that Rickettsia will likely be present where cattle and other domestic animals which harbor ticks are found (Okabayashi et al. 1999, Brouqui et al. 2004). Ticks from Garissa and Isiolo had a significantly higher rickettsial infection rate compared to the other sites. This outcome could be related to the high population of domestic animals found in these two sites and in particular the presence of camels in these two sites which are not commonly herded in Ijara, Marigat, and Mai Mahiu. This is significant because ticks collected from camels had the highest Rickettsia infection rate, suggesting the importance of these animals as reservoirs of SFG Rickettsia spp. Camels and ticks infesting camels have also been found infected with SFG Rickettsia in Israel (Kleinerman et al. 2013) and in Egypt, respectively (Abdel-Shafy et al. 2012).
Hyalomma marginatum, H. truncatum, Rh.pulchellus, Rh. appendiculatus, Rh. evertsi, and A. gemma the main tick species infected with Rickettsia in this study, predominantly feed on cattle, sheep, goats, camels, and large wild ruminants such as giraffes, buffaloes, and rhinoceroses. The larvae and nymphs stages also feed on humans and small mammals such as hares, rabbits, hedgehogs, and birds (Walker et al. 2003). The wide host range of these ticks at each developmental stage increases their ability to acquire and transmit Rickettsia spp. infections to human populations living in Isiolo, Garissa, Marigat, Ijara, and Mai Mahiu.
In the tick positive pools confirmed by sequencing, R. aeschlimannii was predominant, followed by R. africae. We detected R. aeschlimannii in H. marginatum, H. truncatum, Rh. pulchellus, and Hyalomma spp. ticks. This Rickettsia species has been reported before in Kenya in H. truncatum ticks (Mutai et al. 2013) but not in H. marginatum and Rh. pulchellus ticks. Rickettsiaaeschlimannii was first described in Hyalomma marginatum tick species from Morrocco (Sarih et al. 2008) and has also been reported in Rhipicephalus appendiculatus ticks from South Africa (Pretorius and Birtles 2002). This is the first description of R. aeschlimannii being identified in H. marginatum and Rh. pulchellus ticks in Kenya, indicating a broader range of widely distributed ticks that could transmit this infection. In this study, R. africae was predominantly detected in Amblyomma tick species which correlates well with other studies which show a strong link between the distribution of R. africae and the geographical distribution of Amblyomma tick species (Raoult et al. 2001).
Of the two predominant rickettsial species identified in this study, both present as febrile illness in humans but neither has very distinct clinical features. Rickettsiaaeschlimannii causes a clinical syndrome that is similar to the Mediterranean spotted fever (MSF) that is caused by R. conorii. Patients may present with multiple eschars, fever, and a maculopapular rash (Parola et al. 2005). On the other hand, Rickettsia africae is known to cause African tick bite fever (ATBF), a milder disease with no rash (Kelly et al. 1996). We postulate that these two rickettsial species detected in our tick samples could be the cause of a significant portion of undiagnosed febrile illness in the human population in these pastoral sites. This is corroborated by the high sero prevalence of SFG Rickettsia antibodies found among pastoralists in Garissa and Marigat (Thiga et al. 2015). A high antibody titer to TG Rickettsia has also been reported in pastoralist from the northern part of the country (Omballa et al. 2016). In spite of this serological evidence, rickettsial diseases are not routinely diagnosed in Kenya. Diagnosed cases of acute rickettsiosis are mainly reported by travelers returning from sub-Saharan African countries (Raoult et al. 2001, Jensenius et al. 2003), who return to countries better able to detect these infections using the standard diagnostic tests—ELISA and PCR tests. For example, R. conorii infections contracted in Kenya have been reported in a missionary from the United States and a Japanese traveler (Rutherford et al. 2004, Yoshikawa et al. 2005). This disparity in diagnostic capabilities accounts for the very few acute clinical cases of Rickettsia infection that have been reported in the human population in Kenya (Wanzala and Ondiaka 2013) despite the evidence of Rickettsia spp. infections in ticks and humans.
One limitation of this study is that not all gltA-positive samples were sequenced and as a result only seven tick pools had sequences for all three gene targets. In two of the tick pools tested, different Rickettsia species were obtained with each of the primers used. Although we used three target genes to clarify the taxonomic classification of the species (Fournier and Raoult 2009), the lack of phylogenetic resolution in some of our nucleotide sequences could have been due to the genetic closeness of Rickettsia species or mixed infections in the tick pools.
In conclusion, the findings of this study indicate that multiple Rickettsia species are circulating in a wide range of ticks from pastoral communities in Kenya, and clinicians should be aware that these species may potentially be causing febrile disease in the human population. Better diagnostic capabilities such as rapid kits, which could be used in public health facilities in these pastoral communities, would lead to detection and treatment of these infections. It would also reduce the morbidity associated with febrile illness and the overtreatment with ineffective drugs used for syndrome treatment of febrile illness such as antimalarials.
Acknowledgments
We thank Silvanos Opanda, Benjamin Opot, John Gachoya, James Mutisya, Francis Mulwa, Dunstone Beti, Philip Tunge, and Faith Sigei for their technical assistance. We thank Caroline Tungwony for generating the map. We would also like to thank the US Army Medical Research Directorate—Kenya arbovirus surveillance program and the Arbovirus Incidence and Disease (AVID) program sponsored by Google.org for providing the samples that were used in this study. Materials and reagents were provided by the US Army Medical Research Directorate—Kenya.
This study was approved by the Institutional Review Boards at Kenya Medical Research Institute (KEMRI study 2454) and Walter Reed Army Institute of Research (WRAIR study 2099). Collection of tick samples had been previously approved by the KEMRI IRB (Study 1560 and 824) and WRAIR IRB study 1134.
References Cited
- Abdel-Shafy S., Allam N. A., Mediannikov O., Parola P., Raoult D.. 2012. Molecular detection of spotted fever group rickettsiae associated with ixodid ticks in Egypt. Vector Borne Zoonotic Dis. 12: 346–359. [DOI] [PubMed] [Google Scholar]
- Brouqui P., Bacellar F., Baranton G., Birtles R. J., Bjoersdorff A., Blanco J. R., Caruso G., Cinco M., Fournier P. E., Francavilla E., et al. 2004. Guidelines for the diagnosis of tick-borne bacterial diseases in Europe. Clin Microbiol. Infect. 10: 1108–1132. [DOI] [PubMed] [Google Scholar]
- Choi Y. J., Jang W. J., Ryu J. S., Lee S. H., Park K. H., Paik H. S., Koh Y. S., Choi M. S., Kim I. S.. 2005. Spotted fever group and typhus group rickettsioses in humans, South Korea. Emerg. Infect. Dis. 11: 237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar R. C. 2004. MUSCLE: multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res. 32: 1792–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faccini-Martínez Á. A., García-Álvarez L., Hidalgo M., Oteo J. A.. 2014. Syndromic classification of rickettsioses: An approach for clinical practice. Int. J. Infect. Dis. 28: 126–139. [DOI] [PubMed] [Google Scholar]
- Fournier P. E., Raoult D.. 2009. Current knowledge on phylogeny and taxonomy of Rickettsia spp. Ann N Y Acad Sci. 1166: 1–11. [DOI] [PubMed] [Google Scholar]
- Gillespie J. J., Williams K., Shukla M., Snyder E. E., Nordberg E. K., Ceraul S. M., Dharmanolla C., Rainey D., Soneja J., Shallom J. M., et al. 2008. Rickettsia phylogenomics: Unwinding the intricacies of obligate intracellular life. PLoS ONE 3: e2018.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huntzinger A. 2007. Guidelines for the diagnosis and treatment of tick-borne rickettsial diseases. Am. Fam. Physician 76: 137–139. [Google Scholar]
- Jensenius M., Fournier P. E., Vene S., Hoel T., Hasle G., Henriksen A. Z., Hellum K. B., Raoult D., Myrvang B., and N.A.T.B.F.S. Group. 2003. African tick bite fever in travelers to rural Sub-Equatorial Africa. Clin. Infect. Dis. 36: 1411–1417. [DOI] [PubMed] [Google Scholar]
- Kelly P. J., Beati L., Mason P. R., Matthewman L. A., Roux V., Raoult D.. 1996. Rickettsia africae sp. nov., the etiological agent of African tick bite fever. Int. J. Syst. Bacteriol. 46: 611–614. [DOI] [PubMed] [Google Scholar]
- Kimita G., Mutai B., Nyanjom S. G., Wamunyokoli F., Waitumbi J.. 2016. Phylogenetic variants of Rickettsia africae, and incidental identification of “Candidatus Rickettsia Moyalensis” in Kenya. PLoS Negl. Trop. Dis. 10: e0004788.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinerman G., Baneth G., Mumcuoglu K. Y., van Straten M., Berlin D., Apanaskevich D. A., Abdeen Z., Nasereddin A., Harrus S.. 2013. Molecular detection of Rickettsia africae, Rickettsia aeschlimannii, and Rickettsia sibirica mongolitimonae in camels and Hyalomma spp. ticks from Israel. Vector Borne Zoonotic Dis. 13: 851–856. [DOI] [PubMed] [Google Scholar]
- La Scola B., Raoult D.. 1997. Laboratory diagnosis of rickettsioses: Current approaches to diagnosis of old and new rickettsial diseases. J. Clin. Microbiol. 35: 2715–2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBeaud A. D., Muchiri E. M., Ndzovu M., Mwanje M. T., Muiruri S., Peters C. J., King C. H.. 2008. Interepidemic Rift Valley fever virus seropositivity, northeastern Kenya. Emerg. Infect. Dis. 14: 1240–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labruna M. B., Whitworth T., Horta M. C., Bouyer D. H., McBride J. W., Pinter A., Popov V., Gennari S. M., Walker D. H.. 2004. Rickettsia species infecting Amblyomma cooperi ticks from an area in the state of Sao Paulo, Brazil, where Brazilian spotted fever is endemic. J. Clin. Microbiol. 42: 90–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutomiah J., Musila L., Makio A., Ochieng C., Koka H., Chepkorir E., Mutisya J., Mulwa F., Khamadi S., Miller B. R., et al. 2014. Ticks and tick-borne viruses from livestock hosts in arid and semiarid regions of the eastern and northeastern parts of Kenya. J. Med. Entomol. 51: 269–277. [DOI] [PubMed] [Google Scholar]
- Lwande O. W., Irura Z., Tigoi C., Chepkorir E., Orindi B., Musila L., Venter M., Fischer A., Sang R.. 2012. Seroprevalence of Crimean Congo hemorrhagic fever virus in Ijara District, Kenya. Vector Borne Zoonotic Dis. 12: 727–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lwande O. W., Lutomiah J., Obanda V., Gakuya F., Mutisya J., Mulwa F., Michuki G., Chepkorir E., Fischer A., Venter M., et al. 2013. Isolation of tick and mosquito-borne arboviruses from ticks sampled from livestock and wild animal hosts in Ijara District, Kenya. Vector Borne Zoonotic Dis. 13: 637–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden T. 2013. The BLAST sequence analysis tool.
- Macaluso K. R., Davis J., Alam U., Korman A., Rutherford J. S., Rosenberg R., Azad A. F.. 2003. Spotted Fever Group Rickettsiae In Ticks From The Masai Mara Region Of Kenya. The American Journal of Tropical Medicine and Hygiene. 68: 551–553. [DOI] [PubMed] [Google Scholar]
- Matthysse J., Colbo M. H.. 1987. The Ixodid ticks of Uganda together with species pertinent to Uganda because of their present known distribution. Entomological Society of America, College Park, MD. [Google Scholar]
- Mutai B. K., Wainaina J. M., Magiri C. G., Nganga J. K., Ithondeka P. M., Njagi O. N., Jiang J., Richards A. L., Waitumbi J. N.. 2013. Zoonotic surveillance for rickettsiae in domestic animals in Kenya. Vector Borne Zoonotic Dis. 13: 360–366. [DOI] [PubMed] [Google Scholar]
- Mwamuye M. M., Kariuki E., Omondi D., Kabii J., Odongo D., Masiga D., Villinger J.. 2016. Novel Rickettsia and emergent tick-borne pathogens: A molecular survey of ticks and tick-borne pathogens in Shimba Hills National Reserve, Kenya. Ticks and Tick-borne Diseases. [DOI] [PubMed] [Google Scholar]
- Ndip L. M., Fokam E. B., Bouyer D. H., Ndip R. N., Titanji V. P., Walker D. H., McBride J. W.. 2004. Detection of Rickettsia africae in patients and ticks along the coastal region of Cameroon. Am. J. Trop. Med. Hyg. 71: 363–366. [PubMed] [Google Scholar]
- Okabayashi T., Hasebe F., Samui K. L., Mweene A. S., Pandey S. G., Yanase T., Muramatsu Y., Ueno H., Morita C.. 1999. Short report: Prevalence of antibodies against spotted fever, murine typhus, and Q fever rickettsiae in humans living in Zambia. Am. J. Trop. Med. Hyg. 61: 70–72. [DOI] [PubMed] [Google Scholar]
- Okello-Onen J., Hassan S. M., Essuman S.. 1999. Taxonomy of African ticks. Icipe Science Press, Nairobi. [Google Scholar]
- Omballa V. O., Musyoka R. N., Vittor A. Y., Wamburu K. B., Wachira C. M., Waiboci L. W., Abudo M. U., Juma B. W., Kim A. A., Montgomery J. M., et al. 2016. Serologic evidence of the geographic distribution of bacterial zoonotic agents in Kenya, 2007. Am. J. Trop. Med. Hyg. 94: 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parola P., Paddock C. D., Raoult D.. 2005. Tick-borne rickettsioses around the world: Emerging diseases challenging old concepts. Clin. Microbiol. Rev. 18: 719–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaffle M., Littwin N., Muders S. V., Petney T. N.. 2013. The ecology of tick-borne diseases. Int J Parasitol. 43; 1059–1077. [DOI] [PubMed] [Google Scholar]
- Pretorius A. M., Birtles R. J.. 2002. Rickettsia aeschlimannii: A new pathogenic spotted fever group rickettsia, South Africa. Emerg. Infect. Dis. 8: 874.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raoult D., Fournier P. E., Fenollar F., Jensenius M., Prioe T., de Pina J. J., Caruso G., Jones N., Laferl H., Rosenblatt J. E., et al. 2001. Rickettsia africae, a tick-borne pathogen in travelers to sub-Saharan Africa. N. Engl. J. Med. 344: 1504–1510. [DOI] [PubMed] [Google Scholar]
- Raoult D., Roux V.. 1997. Rickettsioses as paradigms of new or emerging infectious diseases. Clin. Microbiol. Rev. 10: 694–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RCoreTeam 2014. R: A language and environment for statistical computing R Foundation for Statistical Computing; Vienna, Austria. [Google Scholar]
- Regnery R. L., Spruill C. L., Plikaytis B. D.. 1991. Genotypic identification of rickettsiae and estimation of intraspecies sequence divergence for portions of two rickettsial genes. J. Bacteriol. 173: 1576–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards A. L., Jiang J., Omulo S., Dare R., Abdirahman K., Ali A., Sharif S. K., Feikin D. R., Breiman R. F., Njenga M. K.. 2010. Human infection with Rickettsia felis, Kenya. Emerg. Infect. Dis. 16: 1081–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutherford J. S., Macaluso K., Smith N., Zaki S. R., Paddock C. D., Davis J., Peterso N., Azad A. F., Rosenberg R.. 2004. Fatal spotted fever rickettsiosis, Kenya. Emerg. Infect. Dis. 10: 910–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sang R., Lutomiah J., Koka H., Makio A., Chepkorir E., Ochieng C., Yalwala S., Mutisya J., Musila L., Richardson J. H., et al. 2011. Crimean-Congo hemorrhagic fever virus in Hyalommid ticks, northeastern Kenya. Emerg. Infect. Dis. 17: 1502–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarih M., Socolovschi C., Boudebouch N., Hassar M., Raoult D., Parola P.. 2008. Spotted fever group rickettsiae in ticks, Morocco. Emerg. Infect. Dis. 14: 1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stucky B. J. 2012. SeqTrace: a graphical tool for rapidly processing DNA sequencing chromatograms. Journal of Biomolecular Techniques 23. [DOI] [PMC free article] [PubMed]
- Thiga J. W., Beth K. M., Wurapa K. E., Zipporah N., Ju J., Allen L. R., John N. W.. 2015. High seroprevalence of antibodies against spotted fever and scrub typhus bacteria in patients with febrile illness, Kenya. Emerg. Infect. Dis. J. 21: 688.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker A. R., Bouattour A., Camicas J. L., Estrada-Peña A., Horak I. G., Latif A. A., Pegram R. G., Preston P. M.. 2003. Ticks of domestic animals in Africa: A Guide to identification of species. Bioscience Reports, Edinburgh Scotland, United Kingdom. [Google Scholar]
- Wanzala W., Ondiaka S. N.. 2013. Tick-borne lymphadenopathy-like condition in an African woman in Kenya. Journal of Research in Medical Sciences: The Official Journal of Isfahan University of Medical Sciences. 18: 918–921. [PMC free article] [PubMed] [Google Scholar]
- Yoshikawa H., Kimura M., Ogawa M., Rolain J. M., Raoult D.. 2005. Laboratory-confirmed mediterranean spotted fever in a Japanese traveller to Kenya. Am. J. Trop. Med. Hyg. 73: 1086–1089. [PubMed] [Google Scholar]