Abstract
Patient: Female, 59
Final Diagnosis: Spinal tuberculosis
Symptoms: Back pain • tiredness • night sweats
Medication: —
Clinical Procedure: Surgery and medical treatment
Specialty: Neurosurgery
Objective:
Challenging differential diagnosis
Background:
The aim of this study was to draw attention to rare spinal infections in recurrent failed spinal surgeries.
Case Report:
A 59-year-old female was admitted to the hospital for back pain, which was assessed as a 9 on the visual analogue scale (VAS); the patient reported tiredness and night sweats. She had an operation for L3–4 far lateral disc herniation four years ago. Then another operation for L4–5 disc herniation six months ago and immediately three months later she has an operation with L3–4–5 fixation again. She had hypothyroidism, diabetes mellitus, and hypertension. Her daughter was cured of pulmonary tuberculosis 20 years ago. We performed an operation by L4–5 discectomy; all granulation formation with inflammatory processes were debrided and irrigated with antibiotics at levels of L3–5. The old fixation was controlled and replaced. Her back pain improved immediately after surgery; she had a score of 2 on the VAS. Two days after her surgery, our Infection Disease Department reported acid resistant bacillus (ARB+) in samples and began anti-tuberculosis medication.
Conclusions:
Spinal infections should always be taken into consideration in recurrent failed back surgeries.
MeSH Keywords: Disease Management; Failed Back Surgery Syndrome; Tuberculosis, Central Nervous System
Background
Tuberculosis is caused by the Mycobacterium tuberculosis bacteria by hematogenous spread of the infection. Except for a reported case of spinal tuberculosis in a 5,000-year-old Egyptian mummy, the first modern case was described by Percival Pott in 1779. According to the World Health Organization, tuberculosis kills an estimated 1.68 million people a year, worldwide [1]. The spine is the most common extrapulmonary site of tuberculosis infection [2,3]. Magnetic resonance imaging (MRI) is the gold standard for radiological diagnosis through follow-up [4,5]. Treatment for spinal tuberculosis is not easy. The main treatment of spinal tuberculosis requires the use anti-tuberculosis medication before and after surgical debridement, the careful debridement of the entire focus of infection, and reconstruction for spinal stability [1,6].
Failed back surgery is a very common problem for surgeons nowadays. With the increase in spinal surgeries, there has been an increase in complications such as instrumentation-related complications and infections.
We have presented an interesting case of failed back syndrome, where the patient presented with low back pain and fever after multiple lumbar surgeries. We found acid resistant bacillus in a routine surgical specimen. The aim of this study was to draw attention to rare spinal infections in recurrent failed back spinal surgeries.
Case Report
A 59-year-old female was admitted to the hospital in August 2017 for back pain, which was assessed as a 9 on the visual analogue scale (VAS); the patient reported tiredness and night sweats.
She had prior back surgery, including an operation for L3–4 far lateral disc herniation in 2009. The patient had not participated in recommended controls or follow-up after surgery for a longtime, until her back pain reoccurred. Then L4–5 discectomy was performed in December 2016 and three months later she had another operation for L3–4–5 fixation. She had hypothyroidism, diabetes mellitus, and hypertension. Her daughter was cured of pulmonary tuberculosis in 1997.
In the patient’s preoperative diagnostic tests, she had increased values of C-reactive protein and erythrocyte sedimentation rate. MRI studies showed L3–4 and L4–5 laminectomy defects with an abscess in the L4–5 disc area. Granulation and inflammatory reaction was occurring around the dura and disc spaces in L3–4 and L4–5 levels. L4–5 was intensely contrast enhanced, which was in concordance with spondylodiscitis (Figures 1, 2). Blood samples were taken for cultures.
Figure 1.
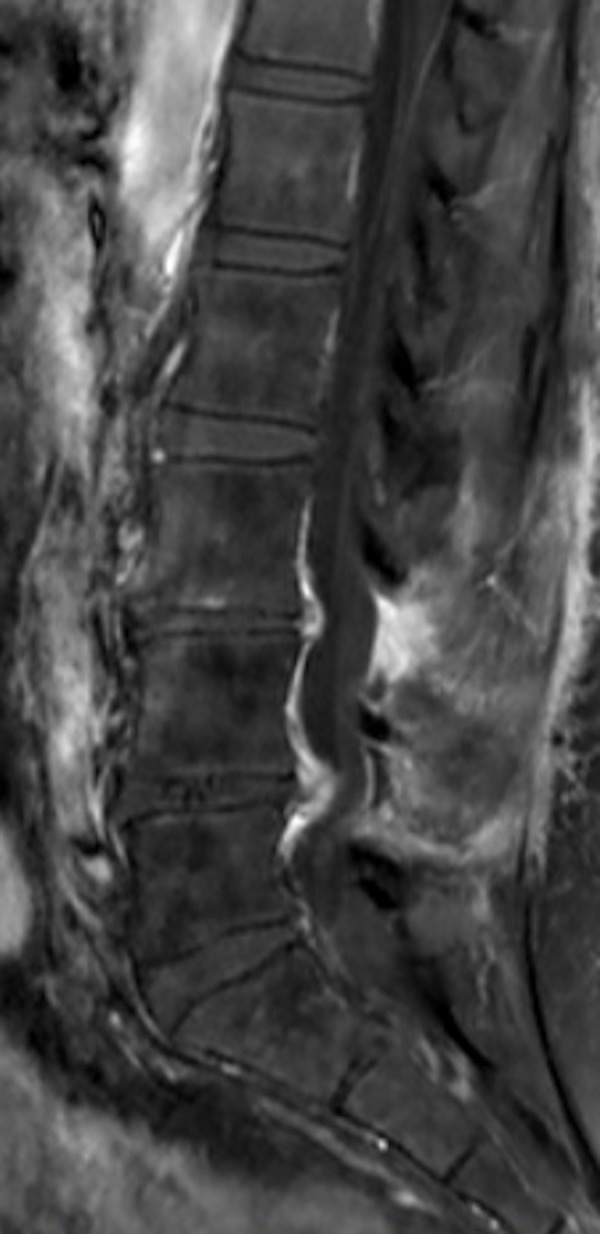
Preoperative contrast enhancing magnetic resonance imaging sagittal view.
Figure 2.
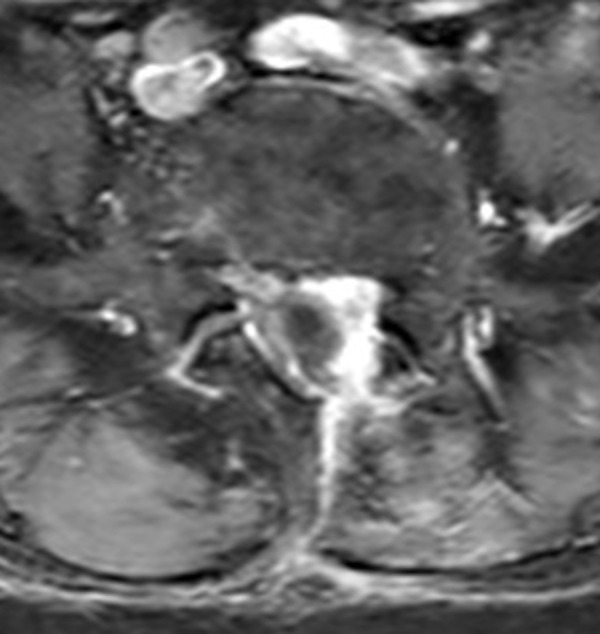
Preoperative contrast enhancing magnetic resonance imaging axial view.
During the operation, we performed L4–5 discectomy and all granulation tissue with inflammatory processes were debrided and irrigated with vancomycin at the level of L4–5. We performed curettage of the endplates and again irrigated the intervertebral disc space with vancomycin solution. We removed previous pedicle screws and replaced them with thicker screws (Figures 3, 4). We made an interbody fusion with an autograft from the iliac bone.
Figure 3.
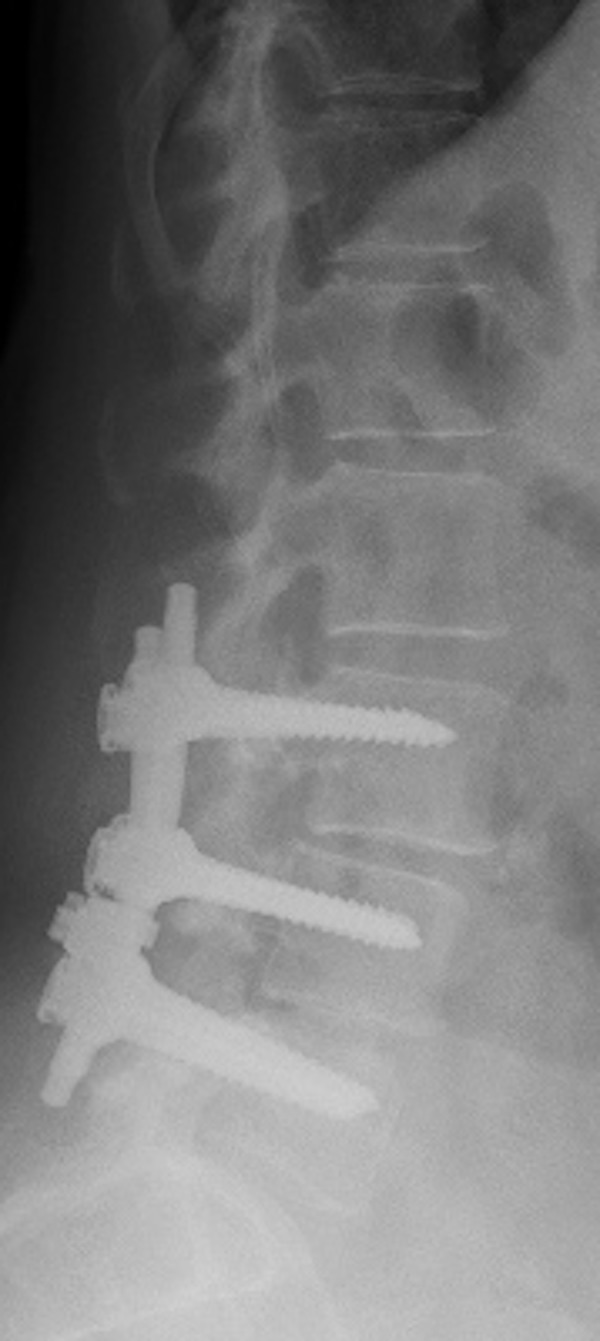
Postoperative x-ray lumbar sagittal view.
Figure 4.
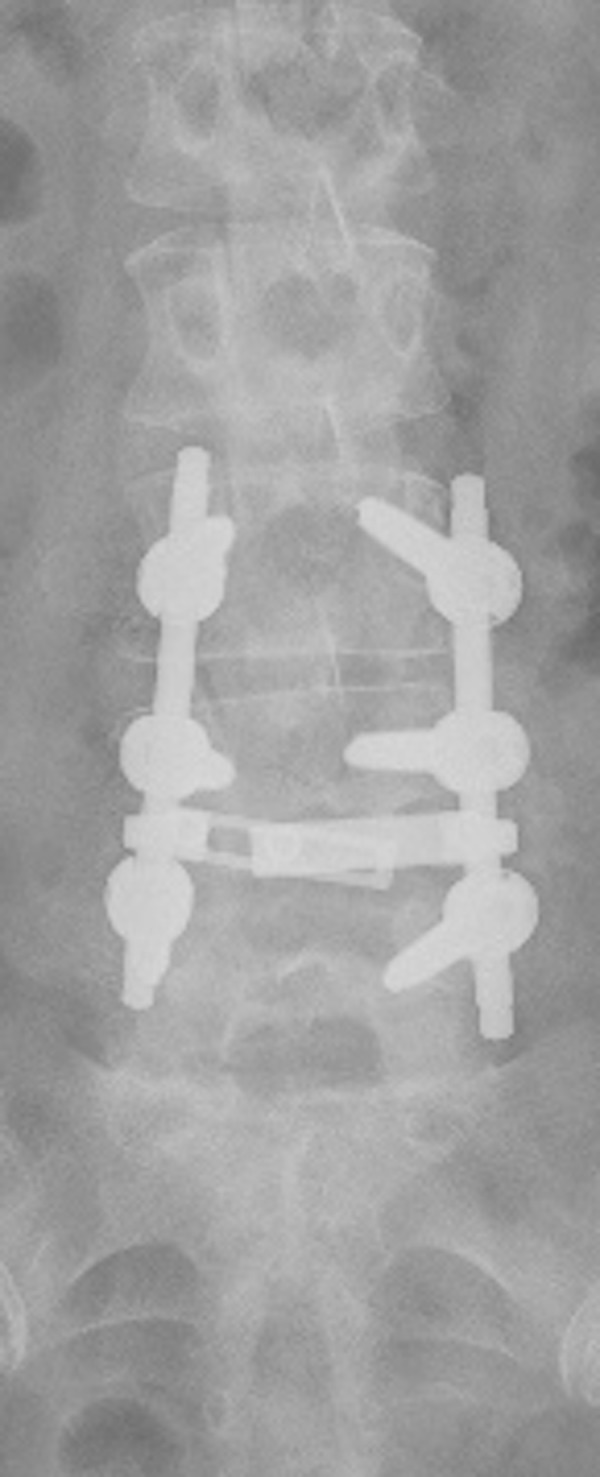
Postoperative x-ray lumbar coronal view.
Postoperatively, her back pain improved immediately after surgery and she had a score of 2 on the VAS. Two days after her surgery, the Infection Disease Department reported acid resistance bacillus (ARB+) in samples and suggested anti-tuberculosis medication to prevent hematogenous spread. Pathological diagnosis confirmed granulomatous infection. A distant focus of tuberculosis was not found after the patient was evaluated with diagnostic and radiologic tests.
The patient was cured after three months of medical treatment and she was referred to the Physiotherapy Department to improve muscle strength.
Discussion
The etiology of failed back surgery syndrome is varied. Wrong diagnosis, wrong sided surgery, inadequate surgery, instability, missed lateral stenosis, recurrent disc herniation, non-fusion, facet pain, infections, root injury, granulation tissues, arachnoiditis, meningeal cysts, and psychiatric problems are potential causes. Infections accounts for 3% of these causes [7]. Discitis is the main cause of infections, but tuberculosis can be a cause, although rare nowadays. In our case, we had concluded that the patient’s infection was a staphylococcal spondylodiscitis due to instrumentation failure; however, our treatment strategy changed when acid resistant bacillus was demonstrated in a surgical specimen.
Pande et al. reported a large case series of 684 patients who had operations for herniated lumbar disc: 87 patients had failed back syndrome and 12 were confirmed to have tuberculous infection of the same disc interval [8]. Our case differs from this study in that we report incidental finding of post-surgical spinal tuberculosis.
There are variations in practice with regards to spinal tuberculosis treatments. Some centers give medical treatment until a neurological deficit appears [2,3,9,10]. Another method is surgery with medical treatment. Spinal tuberculosis surgery also has variations in practice. Posterior spinal decompression, single stage fixation, short or long segment instrumentation with or without interbody fusion, anterior-lateral or posterior approaches, are some of the strategies used [6,9–14]. In our case, the patient had already undergone previous instrumentation; we changed the implanted screws, cleaned the granulation tissues and established an iliac autograft for interbody fusion.
Sahoo et.al. reported on 16 thoraco-lumbar spinal tuberculosis patients who had an operation for posterior decompression and transpedicular screw fixation in a single stage along with antitubercular drug treatment [6]. At follow-up of 24 to 46 months, bony fusion was achieved in 55.5% of the patients. Neurological recovery occurred in 94.4% of the patients. Finally, they observed that all patients became pain free, with a final VAS of 0 to 2 points.
Kumar et al. arranged a prospective follow-up of 25 patients with active thoraco-lumbar spinal tuberculosis who underwent posterior spinal instrumentation with pedicle screws and rods [12]. These patients had posterior stabilization of the involved segment of the spine without anterior or posterior bone grafting. All patients had interbody bony fusion despite the absence of anterior bone grafting or cages.
Arora et al. performed a retrospective review of 24 patients with tuberculosis of the posterior spinal elements, vertebra corpus, and intervertebral disc space [9]. They found that the patients who had undergone operations for decompression for epidural abscess with neurological deficits had poorer outcome compared with patients who received medical treated without neurological deficits [9].
Wang et al. followed 102 patients with mono-segmental spinal tuberculosis retrospectively [13]. They divided patients into two groups: single-segment and short-segment. They observed responses to postoperative chemotherapy and changes in the Cobb angle for kyphosis, fusion time, and Frankel grading. Each patient’s quality of life and ability to return to work, as determined by the Oswestry Disability Index (ODI), were also evaluated. They found that the differences between the two groups were not significant, but after bone fusion, single-segment fixation was effective in restoring and maintaining spinal stability and retaining normal segment motion more than the short-segment fixation approach.
Zhang et al. reported on 37 patients who suffered lumbar tuberculosis [14]. The patients were treated by two different surgical procedures, which were 1) one-stage posterior debridement, TLIF and instrumentation, and 2) posterior instrumentation, anterior debridement and bone graft in a single-stage procedure. Operative duration and blood loss of the first group was less than the other. Lumbar tuberculosis was completely cured, and the grafted bones were fused within 10 months in all patients. There was no persistence or recurrence of infection and no differences in the radiological results between the two groups. Kyphosis was significantly corrected within three months in all patients.
Chandra et al. treated 212 patients who had spinal tuberculosis [1]. They divided the patients into two groups: medical or surgical treatment. After surgery, the improvement of paraplegia was better. Bladder symptoms correlated with the timing of surgery, and they observed that medical treatment was the main stay; however radical, instrumented surgeries should be offered when indicated. They also concluded that the presence of paraplegia should not preclude surgery.
Conclusions
Tuberculosis spondylodiscitis as a cause of recurrent failed back surgery, but is rare. However, spinal infections should always be taken into consideration in recurrent failed back surgeries.
Footnotes
Conflict of interest
None.
References:
- 1.Chandra SP, Singh A, Goyal N, et al. Analysis of changing paradigms of management in 179 patients over 12 year period & proposal of a new management algorithm. World Neurosurg. 2013;80(1–2):190–203. doi: 10.1016/j.wneu.2012.12.019. [DOI] [PubMed] [Google Scholar]
- 2.Rasouli M, Mirkoohi M, Vaccaro AR, et al. Spinal tuberculosis: Diagnosis and management. Asian Spine J. 2012;6:294–308. doi: 10.4184/asj.2012.6.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wibaux C, Tiatsop MM, Andrei I, et al. Changes in the incidence and management of spinal tuberculosis in a French University Hospital Rheumatology Department from 1966 to 2010. Joint Bone Spine. 2013;80(5):516–19. doi: 10.1016/j.jbspin.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Gehlot PS, Chaturvedi S, Kashyap R, Singh V. Pott’s spine: Retrospective analysis of MRI scans of 70 cases. J Clin Diagn Res. 2012;6(9):1534–38. doi: 10.7860/JCDR/2012/4618.2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalid M, Siddiqui MA, Qaseem SMD, et al. Role of magnetic resonance imaging in evaluation of tubercular spondylitis: Pattern of disease in 100 patients with review of literature. J Nepal Med Assoc. 2011;51(183):116–21. [PubMed] [Google Scholar]
- 6.Sahoo MM, Mahapatra SK, Sethi GC, Dash SK. Posterior-only approach surgery for fixation and decompression of thoracolumbar spinal tuberculosis. J Spinal Disord Tech. 2012;25:E217–23. doi: 10.1097/BSD.0b013e31826a088e. [DOI] [PubMed] [Google Scholar]
- 7.Raphael H, Southall JL, Gnanadurai TV, et al. Long-term experience with implanted intrathecal drug administration systems for failed back syndrome and chronic mechanical low back pain. BMC Musculoskelet Disord. 2002;3:1–8. doi: 10.1186/1471-2474-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pande KC, Pande SK, Babhulkar SS. An atypical presentation of tuberculosis of the spine. Spinal Cord. 1996;34(12):716–19. doi: 10.1038/sc.1996.130. [DOI] [PubMed] [Google Scholar]
- 9.Arora S, Sabat D, Maini L, et al. Isolated involvement of the posterior elements in spinal tuberculosis. J Bone Joint Surg Am. 2012;94:e151. doi: 10.2106/JBJS.K.01464. (1–8) [DOI] [PubMed] [Google Scholar]
- 10.Wang Z, Shi J, Geng G, Qui H. Ultra-Short-course chemotherapy for spinal tuberculosis: five years of observation. Eur Spine J. 2013;22:274–81. doi: 10.1007/s00586-012-2536-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jun W, Jun KY, Fei C, et al. Application of an antibiotic crescent-shaped poly-methylmethacrylate strut in thoracic vertebral tuberculosis. Turk Neurosurg. 2013;23:107–12. doi: 10.5137/1019-5149.JTN.4218-11.0. [DOI] [PubMed] [Google Scholar]
- 12.Kumar MN, Joseph B, Manur R. Isolated posterior instrumentation for selected cases of thoraco- lumbar spinal tuberculosis without anterior instrumentation and without anterior or posterior bone grafting. Eur Spine J. 2013;22(3):624–32. doi: 10.1007/s00586-012-2528-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Z, Wu Q, Geng G. Anterior debridement and bone grafting with posterior single-segment internal fixation for the treatment of mono-segmental spinal tuberculosis. Injury. 2013;44:253–57. doi: 10.1016/j.injury.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Zhang H, Lin M, Li J, et al. One-stage posterior debridement, transforaminal lumbar interbody fusion and instrumentation in treatment of lumbar spinal tuberculosis: A retrospective case series. Arch Orthop Trauma Surg. 2013;133(3):333–41. doi: 10.1007/s00402-012-1669-2. [DOI] [PubMed] [Google Scholar]


