Abstract
A 40-year-old man was admitted to our hospital for chest pain after smoking. Coronary computed tomography angiography showed severe stenosis in the left anterior descending artery. The stenosis site had no plaque on stretched curved multiplanar reconstruction and short-axis images. Coronary angiography revealed improvement of the severe stenosis after the intracoronary administration of isosorbide dinitrate in the left anterior descending artery. Intravascular ultrasound demonstrated negative remodeling without a plaque and diffuse intima with media thickening at the stenosis site. The chest pain was likely caused by coronary spastic angina, which was treated with diltiazem hydrochloride.
Keywords: Coronary spastic angina, Coronary artery disease, Coronary computed tomography angiography, ST elevation
Introduction
Coronary computed tomography angiography (CCTA) has recently been used for the diagnosis of urgent chest pain because of its high negative predictive value and noninvasiveness. An important differential diagnosis of chest pain is coronary spasm, which is difficult to definitively diagnose by CCTA alone. We report a patient with coronary spasm that was detected by CCTA, and confirmed by coronary angiography (CAG) and intravascular ultrasound (IVUS).
Case report
A 40-year-old man visited our hospital for chest pain that lasted for about 5 minutes after smoking in the morning. This was his first time to experience chest pain, which prompted him to visit our hospital 3 hours after he felt the pain. He was subsequently admitted to the emergency ward.
On admission, he had a heart rate of 60 beats/min (bpm) and a blood pressure of 140/72 mm Hg, with unremarkable physical findings. He had no coronary risk factors except for smoking. His resting electrocardiogram showed sinus rhythm and not a typical ST change because of ischemic heart disease (Fig. 1). Echocardiography revealed normal left ventricular wall motion and an ejection fraction of 65%. He has not taken any oral medications. He had a serum creatinine level of 0.74 mg/dL with an estimated glomerular filtration rate of 93.6 mL/m/1.73 m2. His creatine kinase and MB fraction levels were within the normal limits (79 U/L and 4.4 ng/mL, respectively). However, his laboratory test was positive for troponin T.
Fig. 1.

Electrocardiogram findings. On admission, the T wave amplitude of V2 to V5 was higher; however, this was not the typical ischemic ST segment change. The following day, the ST segment of V3 to V5 was slightly decreased. Two weeks later, the ST segment of the anterior leads clearly decreased.
As the patient no longer felt the chest pain during the emergency admission, CCTA was performed. A β-blocker was not used before CCTA because of his 60 bpm heart rate. CCTA was performed following the sublingual administration of nitroglycerin. CCTA revealed a patent right coronary artery and left circumflex artery, but severe stenosis in the middle portion of the left anterior descending artery (LAD) (Fig. 2). Myocardial bridging was not evident at the stenosis site on axial and multiplanar reformation images. The patient felt no chest pain during the CCTA. On the following day, CAG revealed severe stenosis (90%) in the middle portion of the LAD. This severe stenosis of the LAD was improved to 25% after isosorbide dinitrate (ISDN) administration into the left coronary artery (Fig. 3 A, B). IVUS showed negative remodeling without a plaque, as well as diffuse intima, thick media, and a high echoic area on the intimal surface at the stenosis site even after intracoronary ISDN administration (Fig. 3 C-E). The acetylcholine provocation test was not performed because of the confirmation of coronary spasm by CAG without ISDN administration. With the occurrence of vasospasm, diltiazem hydrochloride (100 mg/d) was started from the evening following CAG. The patient has since then stopped smoking and has not felt any chest pain for 1 year. Based on his electrocardiogram progression, myocardial ischemia is considered to have occurred on the day of his admission (Fig. 1).
Fig. 2.
Coronary computed tomography angiography findings (A, volume rendering; B, short axis). Coronary computed tomography angiography (CCTA) revealed severe stenosis in the middle portion of the left anterior descending artery. The patient no longer felt the chest pain during the admission CCTA.
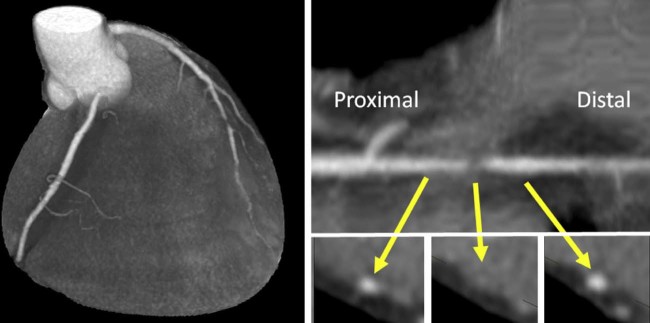
Fig. 3.
Coronary angiography and intravascular ultrasound findings. (A) Coronary angiography revealed severe stenosis in the middle portion of the left anterior descending artery (red arrow). (B) After isosorbide dinitrate (ISDN) administration into the left coronary artery, the stenosis was improved (red arrow). (C and E) At the proximal and distal stenotic sites, the vascular lumen was preserved and intimal shrinkage was not evident. However, a high echoic area was observed on the intimal surface (yellow arrow). (D) At the spasm site, intravascular ultrasound showed diffuse intima and thick media even after intracoronary ISDN administration.
Discussion
In this case, coronary spasm was detected by CCTA and confirmed by CAG and IVUS. There are currently few reports on cases of coronary spasm detection by CCTA [1], [2], [3], [4], [5]. Most of these cases used adenosine perfusion or a β-blocker, which often causes coronary spasm as a side effect [4], [6]. In our patient, neither perfusion stimuli nor a β-blocker was administered to reduce the heart rate. Based on the improvement of his severe stenosis following ISDN administration and the IVUS findings, his chest pain was confirmed to be caused by coronary spasm.
A myocardial bridge is one of the important causes of chest pain. The middle portion of the LAD is a common myocardial bridge site. The CCTA clearly showed the presence, course, and anatomic features of the intramuscular coronary arteries [7]. Myocardial bridging was diagnosed and evaluated when an intramuscular segment of the coronary artery was visualized on axial and multi planar reconstruction images. However, myocardial bridging was not shown in the stenosis site from the four-dimensional findings and on the short axial images using CCTA.
One of the distinct features of CCTA is its high plaque detectability. However, assessment of the presence of plaque may be difficult in severe cases of coronary spasms. IVUS was helpful for confirming the diagnosis of coronary spasm in this case. The IVUS findings at the coronary spasm sites showed morphological changes in the vascular wall, such as atherosclerosis, negative remodeling, diffuse intima, thick media, and wrinkles in the internal elastic membrane even in the absence of a significant coronary stenosis [8], [9], [10].
The coronary spasm of our patient was observed in the same site for 2 consecutive days by CCTA and CAG without a provocation test. Endothelial dysfunction, local vascular smooth muscle hyperactivity, and deficiency of endothelial nitric oxide activity are thought to be associated with the mechanisms of coronary spasm, which can cause morphological changes in the vascular wall including negative vessel remodeling [10].
With the favorable progress in the performance of computed tomography equipment, the frequency of computed tomography usage not only for detecting elective effort angina but also for diagnosing emergency chest pain has gradually increased. However, the definitive diagnosis of coronary spasm remains difficult. Opportunities for detecting coronary spasm by CCTA may increase with an increase in the scan frequency. Myocardial infarction and life-threatening arrhythmias often occur in patients with vasospastic angina. Coronary spasm is usually fatal, and the appropriate management of patients with coronary spasm is expected through improvements in the detection frequency.
Conclusion
Coronary spasm was successfully detected by CCTA in a patient who consulted for an assessment of his chest pain which occurred at rest. CAG without a provocation test and IVUS were valuable for confirming and making a definitive diagnosis of coronary spasm.
Acknowledgment
We thank Dr. Edward Barroga (http://orcid.org/0000-0002-8920-2607) for reviewing and editing the manuscript.
Footnotes
Competing Interests: The authors declare that they have no conflicts of interest associated with this case report.
References
- 1.Hamon M., Hamon M. Images in clinical medicine. Asymptomatic coronary artery spasm. N Engl J Med. 2006;355:2236. doi: 10.1056/NEJMicm054005. [DOI] [PubMed] [Google Scholar]
- 2.Ito K., Ogawa T., Yoshimura M. Severe coronary spasm occasionally detected by coronary computed tomography. Eur Heart J. 2009;30:2768. doi: 10.1093/eurheartj/ehp344. [DOI] [PubMed] [Google Scholar]
- 3.Ota M., Anan I., Morimoto S., Minai K., Komukai K., Ogawa T. Severe lasting coronary spasm detected by multi-detector row computed tomography. Int J Cardiol. 2011;153:e62–e64. doi: 10.1016/j.ijcard.2011.02.062. [DOI] [PubMed] [Google Scholar]
- 4.Nakahara T., Toyama T., Tsushima Y., Kurabayashi M. Coronary vasospasm during CT angiography. J Cardiovasc Comput Tomogr. 2014;8:328–330. doi: 10.1016/j.jcct.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Nam J.G., Choi S.H., Kang B.S., Bang M.S., Kwon W.J. Development of coronary vasospasm during adenosine-stress myocardial perfusion CT imaging. Korean J Radiol. 2015;16:673–677. doi: 10.3348/kjr.2015.16.3.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakayama M., Morishima T., Chikamori T., Aiga M., Takazawa K., Yamashina A. Coronary arterial spasm during adenosine myocardial perfusion imaging. J Cardiol. 2009;53:288–292. doi: 10.1016/j.jjcc.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Konen E., Goitein O., Sternik L., Eshet Y., Shemesh J., Di Segni E. The prevalence and anatomical patterns of intramuscular coronary arteries: a coronary computed tomography angiographic study. J Am Coll Cardiol. 2007;49:587–593. doi: 10.1016/j.jacc.2006.09.039. [DOI] [PubMed] [Google Scholar]
- 8.Koyama J., Yamagishi M., Tamai J., Kawano S., Daikoku S., Miyatake K. Comparison of vessel wall morphologic appearance at sites of focal and diffuse coronary vasospasm by intravascular ultrasound. Am Heart J. 1995;130:440–445. doi: 10.1016/0002-8703(95)90349-6. [DOI] [PubMed] [Google Scholar]
- 9.Ota H., Kawase Y., Kondo H., Miyake T., Kamikawa S., Okubo M. A case report of acute myocardial infarction induced by coronary spasm. Intravascular findings. Int Heart J. 2013;54:237–239. doi: 10.1536/ihj.54.237. [DOI] [PubMed] [Google Scholar]
- 10.Miyao Y., Kugiyama K., Kawano H., Motoyama T., Ogawa H., Yoshimura M. Diffuse intimal thickening of coronary arteries in patients with coronary spastic angina. J Am Coll Cardiol. 2000;36:432–437. doi: 10.1016/s0735-1097(00)00729-4. [DOI] [PubMed] [Google Scholar]