Abstract
Background
An anterior cruciate ligament (ACL) reconstruction has become more common and the surgical morbidity has decreased, it has been performed not only in younger people to play sports but also middle-aged people, with satisfactory results. Therefore, some patients might have comorbidities for which they take medicines. Especially the medicines, such as systemic steroids, might influence the reconstructed ligament strength and durability.
Case report
A 49-year-old woman who was taking oral steroids for autoimmune hepatitis suffered a spontaneous ACL injury. She complained of unstable symptoms in the knee despite initial conservative treatment. Then, she was treated operatively with autologous hamstring tendon grafts. Three years postoperatively, her knee remained stable with 1.8 mm side-to-side difference on a Kneelax arthrometer and with 1.6 mm on anterior stress radiographs. There was no rerupture or instability.
Conclusion
The patient who had received systemic steroids for a long time recovered satisfactorily after the operation, with achievement of knee stability and possibility to prevent degenerative change in the knee joint. ACL reconstruction should be considered even in patients with such medication.
Introduction
Acute anterior cruciate ligament (ACL) rupture is a common and serious knee injury in the young active population. Untreated ruptures of the ACL lead to progressive degenerative lesions in the tibiofemoral joint, and progressive development of osteoarthritis (OA) over decades.1, 2, 3 Because ACL reconstruction has become more common and the surgical morbidity has decreased, it has been performed not only in younger people to play sports but also middle-aged people, with satisfactory results.4, 5, 6 Therefore, some patients might have comorbidities for which they take medicines. Especially the medicines, such as systemic steroids, might influence the reconstructed ligament strength and durability. It is known that long-term systemic or local steroid therapy reduces the number of fibroblasts,7, 8, 9 and may even cause partial necrosis of the tendon or ligament. However, to our knowledge there is no published report of an ACL reconstruction in a patient who has taken systemic steroids for a long time. We report on operative treatment of a spontaneous ACL injury in a patient on systemic steroid therapy, who achieved a stable knee for 3 years.
Case
A 49-year-old woman presented with left knee pain of insidious onset for 11 months' duration and instability expressed as giving way. She had been diagnosed with autoimmune hepatitis at 33 years old and had been taking prednisolone from 10 to 30 mg per day for 16 years. At 11 months before her first visit, she started to feel knee instability. There was no traumatic event except that she tottered on a bus. Since then, she had repetitive episodes of giving way during activities of daily living (ADL). On physical examination, there was slight swelling of the knee. Lachman test and pivot-shift test were positive. Magnetic resonance imaging (MRI) showed an ACL rupture without other ligament injuries or meniscus tear. There was no evidence of knee OA in radiographs. Stress radiographs with an anterior drawer force of 15 kg revealed 11.9 mm anterior displacement of the tibia compared to that of the contralateral side. Diagnosis was spontaneous ACL rupture and anatomic double-bundle ACL reconstruction was done using autogenous semitendinosus graft. Arthroscopy revealed the ACL rupture but no meniscus tear or cartilage lesion. Two femoral tunnels were drilled within the native ACL femoral footprint through an anteromedial portal, and two tibial tunnels were drilled within the tibial footprint in an outside-in fashion. Two double-folded semitendinosus tendon grafts were prepared. After the femoral fixation with TightRope RT (Arthrex, Inc., Naples, FL), each graft was fixed at the tibial end with a Double-spike plate (DSP; MEIRA Corp., Nagoya, Aichi, Japan) under tension of 20 N at 20° of knee flexion. Range of motion exercise and partial weightbearing with a functional knee brace (Breg, Inc., Carlsbad, CA) was begun 6 days after surgery. Full weightbearing was allowed 22 days after the surgery.
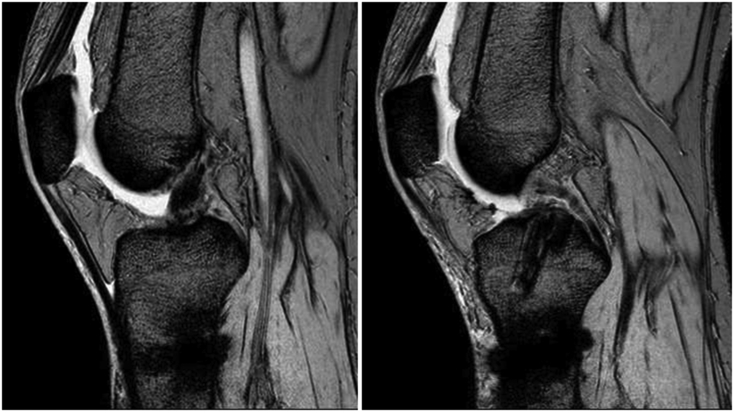
Function and stability of the knee were assessed 1, 2, and 3 years after surgery. At the 1-year postoperative visit, she felt no instability of her knee. On physical examination, range of motion was 0° to 140°. Lachman test and pivot shift test were negative. Laxity measurement with anterior stress radiographs revealed 2.2 mm of side-to-side difference. At 2 years postoperatively, the values for the knee injury and osteoarthritis outcome score (KOOS)10 subgroups were 92 for pain, 86 for symptoms, 81 for ADL function, 65 for sport, and 56 for knee-related quality of life. On MRI examination 2 years after the operation, the reconstructed graft had a homogeneous low-intensity signal indistinguishable from that of the PCL or patellar tendon on sagittal T2 images, demonstrating matured ligamentization, and there was no evidence of bone tunnel enlargement. The Howell graft signal assessment, which would correlate with graft maturity, was grade II (Fig. 1).11 Three years later at the last follow-up the patient was free of complaints. Laxity measurement with Kneelax arthrometer of Biodex, using a 132 N load revealed 1.8 mm of side-to-side difference and 1.6 mm difference on anterior stress radiographs. There was no evidence of OA. KOOS subgroups were 92 for pain, 93 for symptoms, 96 for ADL function, 65 for sport, and 75 for knee-related quality of life, indicating improvement from the score at the 2-year visit. Lysholm score12 was 84, suggesting a good result. Tegner activity score was 3. Informed consent was obtained from the patient.
Fig. 1.
Sagittal T2 images show that the reconstructed graft has a homogeneous low-intensity signal indistinguishable from that of the PCL or patellar tendon, and a good integration within the bone tunnel, demonstrating matured ligamentization. The Howell graft signal assessment was grade II11; Grade I designated a zone filled with a graft that had a homogeneous low-intensity signal indistinguishable from that of the PCL or patellar tendon, grade II designated a volume of the graft analyzed on multiple slices of at least 50% of the normal ligament signal intermixed with portions of the graft that had acquired increased signal intensity, grade III designated a graft within a zone that had less than 50% of its volume exhibiting a normal-appearing ligament signal, and grade IV designated a diffuse increase in the signal intensity with no normal-appearing strands of ligament.
Discussion
To our knowledge, there is no published report of ACL reconstruction in patients with systemic steroid administration who got injured with ACL rupture spontaneously. Although comorbidity with chronic arthritis is considered to be a contraindication of ACL reconstruction, some patients who are taking systemic steroid for diseases without joint inflammations may have ACL injuries. For such patients, ACL reconstruction should be considered as a treatment option. However, it is known that long-term systemic or local steroid therapy reduces the number of fibroblasts,7, 8, 9 and may even cause partial necrosis of the tendon or ligament. Systemic steroid administration must be implicated as the cause of the injury in this patient and might cause impaired healing or rerupture of the reconstructed ligament. Therefore, clinical experiences for such case should be shared. In our case, the patient recovered well without recurrent instability and expressed satisfaction, and did not experience rerupture up to 3 years. Patellar tendon (bone-tendon-bone) can be used as an alternative autograft, but we used a semitendinosus tendon graft because she often kneels during her ADLs.
As we mentioned above, systemic and local steroid therapy is well known to be a medicine that weakens ligaments and tendons.7, 8, 9 However, in one such report intramuscular testosterone helped reduce the loss of muscle mass and strength experienced after ACL injury and reconstruction, while rerupture due to steroid use was not mentioned.13 Because this case achieved a good result, we encourage ACL reconstruction even in patients on systemic steroid therapy. To enhance the graft healing process, biological augmentation using growth factors, stem cells, and scaffolds has been proposed for more than a decade.14, 15, 16 In the near future, these methods will be established well and support these patients to be treated successfully.
We present a case of ACL reconstruction in a patient who has received systemic steroids for a long time to show the efficiency of the procedure for patients with this comorbidity. The patient recovered satisfactorily after the operation, with achievement of knee stability and possibility to prevent degenerative change in the knee joint. Therefore, ACL reconstruction should be considered even in patients with systemic steroid administration.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Contributor Information
Tetsuro Ushio, Email: utflo@ortho.med.kyushu-u.ac.jp.
Ken Okazaki, Email: okazaki.ken@twmu.ac.jp.
Hideki Mizu-uchi, Email: himizu@ortho.med.kyushu-u.ac.jp.
Satoshi Hamai, Email: hamachan@ortho.med.kyushu-u.ac.jp.
Yukio Akasaki, Email: akasaki@ortho.med.kyushu-u.ac.jp.
Yasuharu Nakashima, Email: yasunaka@ortho.med.kyushu-u.ac.jp.
References
- 1.Filbay S.R., Culvenor A.G., Ackerman I.N., Russell T.G., Crossley K.M. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1033–1041. doi: 10.1136/bjsports-2015-094864. [DOI] [PubMed] [Google Scholar]
- 2.Louboutin H., Debarge R., Richou J. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009;16(4):239–244. doi: 10.1016/j.knee.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Segawa H., Omori G., Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8(1):5–11. doi: 10.1016/s0968-0160(00)00062-4. [DOI] [PubMed] [Google Scholar]
- 4.Blyth M.J.G., Gosal H.S., Peake W.M., Bartlett R.J. Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2- to 8-year follow-up. Knee surgery, Sport Traumatol Arthrosc Off J ESSKA. 2003;11(4):204–211. doi: 10.1007/s00167-003-0368-5. [DOI] [PubMed] [Google Scholar]
- 5.Brandsson S., Kartus J., Larsson J., Eriksson B.I., Karlsson J. A comparison of results in middle-aged and young patients after anterior cruciate ligament reconstruction. Arthroscopy. 2000;16(2):178–182. doi: 10.1016/s0749-8063(00)90033-1. [DOI] [PubMed] [Google Scholar]
- 6.Toanen C., Demey G., Ntagiopoulos P.G., Ferrua P., Dejour D. Is there any benefit in anterior cruciate ligament reconstruction in patients older than 60 years? Am J Sports Med. 2017 doi: 10.1177/0363546516678723. Epub ahead. [DOI] [PubMed] [Google Scholar]
- 7.Baruah D.R. Bilateral spontaneous rupture of the achilles tendons in a patient on long-term systemic steroid therapy. Br J Sports Med. 1984;18(2):128–129. doi: 10.1136/bjsm.18.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chechick A., Amit Y., Sheba C., Centre M., Aviv T. Recurrent rupture of the achilles tendon induced by corticosteroid injection. Br J Sports Med. 1982;16(2):89–90. doi: 10.1136/bjsm.16.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morgan J., McCarty D.J. Tendon ruptures in patients with systemic lupus erythematosus treated with corticosteroids. Arthritis Rheum. 1974;17(6):1033–1036. doi: 10.1002/art.1780170616. http://www.ncbi.nlm.nih.gov/pubmed/4433351 [DOI] [PubMed] [Google Scholar]
- 10.Roos E.M., Roos H.P., Lohmander L.S., Ekdahl C., Beynnon B.D. Knee injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 11.Howell S.M., Clark J.A., Blasier R.D. Serial magnetic resonance imaging of hamstring anterior cruciate ligament autografts during the first year of implantation: a preliminary study. Am J Sports Med. 1991;19(1):42–47. doi: 10.1177/036354659101900107. [DOI] [PubMed] [Google Scholar]
- 12.Lysholm J., Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 13.Wu B.W., Berger M., Sum J.C. Randomized control trial to evaluate the effects of acute testosterone administration in men on muscle mass, strength, and physical function following ACL reconstructive surgery: rationale, design, methods. BMC Surg. 2014;14:102. doi: 10.1186/1471-2482-14-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vojnits K., Pan H., Dai X. Functional neuronal differentiation of injury-induced muscle-derived stem cell-like cells with therapeutic implications. Sci Rep. 2017;7(1):1177. doi: 10.1038/s41598-017-01311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martinek V., Latterman C., Usas A. Enhancement of tendon-bone healing of anterior cruciate ligament. J Bone Joint Surg. 2002;84(7):1123–1131. doi: 10.2106/00004623-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Guo R., Gao L., Xu B. Current evidence of adult stem cells to enhance anterior cruciate ligament treatment: a systematic review of animal trials. Arthrosc J Arthrosc Relat Surg. 2017:1–10. doi: 10.1016/j.arthro.2017.07.010. [DOI] [PubMed] [Google Scholar]