Abstract
Cannabis is one of the most commonly used psychoactive substances among adolescents in the United States. Adolescent cannabis use has multiple consequences including academic, health, and psychiatric problems. The Marijuana Adolescent Problem Inventory (MAPI) is a 23-item scale adapted from the Rutgers Alcohol Problem Index and used in the current literature to assess cannabis use problem severity. Psychometric testing for the MAPI has yet to be reported. The current investigation assessed the psychometric characteristics of the MAPI with cannabis-using adolescents (n = 727) from school and outpatient settings who enrolled in five separate randomized clinical trials focused on treatment of substance use. Findings suggested that the MAPI is internally consistent and reliable. Factor structure analyses suggested that the MAPI measures one latent construct, with no differences in factor structure between the outpatient and school settings, supporting a one-factor model. External validity of the MAPI was also demonstrated as evidenced by significant relations with concurrent diagnosis of cannabis dependence and abuse, longitudinal frequency of cannabis use, and mean times used per day. Overall, this initial test of the psychometric characteristics of the MAPI suggests that it can be considered a reliable and valid measure of problems associated with cannabis use among adolescents. Future work is now needed to replicate these findings by testing the psychometric properties of the MAPI in more diverse samples and developing a short version to be used as a brief assessment tool.
Keywords: Adolescent, Youth, Cannabis, Marijuana, Problems, Psychometrics
1. Introduction
In the United States (U.S.), cannabis is the most widely used psychoactive substance among youth (Center for Behavioral Health Statistics and Quality, 2016). Multiple short-term and long-term problems are associated with adolescent cannabis use (Fergusson, Horwood, & Swain-Campbell, 2002; Silins et al., 2014). For example, a recent longitudinal study detected relations between persistent adolescent cannabis use and neuropsychological impairment in adulthood, suggesting persistent use during the developmental period of adolescence may have negative consequences on neurodevelopment (Meier et al., 2012). This combined with the changing status of cannabis laws in the U.S. and decrease in perceived risk of regular cannabis use (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2016) underscore the importance of the need for valid assessment tools measuring key problems related to adolescent cannabis use.
The Rutgers Alcohol Problem Index (RAPI) (White & Labouvie, 1989) was developed to measure problems related to alcohol use specifically, and has contributed to the understanding of risky adolescent and young adult alcohol use in several ways. The RAPI has been used to identify adolescent problem trajectories, elucidate the drinking indices that predict the most risk among young adults, evaluate efficacy of interventions targeting alcohol use, and predict future diagnosis of alcohol dependence (Borsari & Carey, 2005; Borsari, Neal, Collins, & Carey, 2001; Dick, Aliev, Viken, Kaprio, & Rose, 2011; Diestelkamp et al., 2014; Warner, White, & Johnson, 2007). The RAPI evidences sound psychometric characteristics and is recommended for use as a unidimensional scale to measure problem drinking (White & Labouvie, 1989).
Two scales have been commonly used to index problem severity specific to cannabis use among youth. The Marijuana Adolescent Problems Inventory (MAPI) (Johnson & White, 1989) was adapted from the RAPI to measure problems related to youth marijuana use. While different names for this instrument have been used in the existing literature (e.g., Rutgers Marijuana Problem Index; Marijuana Problems Index; Marijuana Problem Inventory) (Blevins, Walker, Stephens, Banes, & Roffman, 2018; Esposito-Smythers, Spirito, Kahler, Hunt, & Monti, 2011; Vandrey, Budney, Kamon, & Stanger, 2005), this 23-item, problem index has adolescents rate each item on a 0–4 scale and yields one total scale score. Studies to date have used the MAPI as a unidimensional scale to investigate predictors of adolescent cannabis withdrawal, evaluate the longitudinal effects of interventions targeting youth cannabis use, and examine the utility of the Comprehensive Marijuana Motives Questionnaire in high school clinical populations (Blevins, Banes, Stephens, Walker, & Roffman, 2016; Vandrey et al., 2005; Walker et al., 2011). The other measure indexing youth marijuana-related problems, the 27-item Adolescent Cannabis Problems Questionnaire (CPQ-A) (Martin, Copeland, Gilmour, Gates, & Swift, 2006), has youth endorse yes or no to each problem item, and yields a total score and scores on three problem subscales (i.e., financial/psychosocial, physical, and acute negative consequences). The CPQ-A has been used to evaluate the validity of the Cannabis Use Problems Identification Test among adolescents and adults, characterize the psychiatric profile of treatment-seeking adolescents and adults with cannabis dependence and mental health problems, and examine the effects of an adolescent cannabis intervention among non-treatment seeking youth (Bashford, Flett, & Copeland, 2010; Ewing et al., 2013; Norberg, Battisti, Copeland, Hermens, & Hickie, 2012).
Psychometric testing for the MAPI has yet to be reported. In contrast, the CPQ-A has limited psychometric data reported in a study of 100 older adolescents aged 14–18 years across two interviews approximately a week apart (Martin et al., 2006). Psychometric testing of the MAPI is needed to better inform researchers and clinicians on its utility as an index of problem behavior related to cannabis use. Such data are needed to satisfy fundamental assumptions in data collection, analysis, and interpretation (Kazdin, 2003). It is important to verify the MAPI as a valid and reliable measure if it is to be used to advance knowledge about youth cannabis use. The MAPI has potential utility as a specific measure of cannabis use problem severity.
The current study examined the psychometric properties of the MAPI using a large and diverse sample of cannabis-using adolescents from school and outpatient settings who enrolled in five separate randomized clinical trials focused on treatment of substance use. Several sets of analyses were conducted to evaluate internal and external validity. The MAPI’s factor structure, reliability (i.e., internal consistency reliability, internal reliability, and test-retest reliability), and associations with cannabis-related variables (i.e., cannabis use frequencies and diagnosis of cannabis abuse and dependence) were examined. The cannabis-using samples were combined to provide a large enough sample to perform the planned analyses, and the diversity of samples provided variability in responses for the initial test of the MAPI’s psychometric characteristics.
2. Materials and methods
2.1. Participants and procedures
Data were combined from five randomized trials evaluating interventions for adolescent substance use across outpatient (Stanger, Budney, Kamon, & Thostensen, 2009; Stanger, Ryan, Scherer, Norton, & Budney, 2015; Stanger, Scherer, Babbin, Ryan, & Budney, 2017) and school settings (Walker et al., 2011; Walker et al., 2016). For the present investigation, we only included youth who reported cannabis use during the past 30-days or who had a cannabis-positive urinalysis result at baseline assessment. The final sample size was N = 727 (of 859 possible), with 110 excluded due to no MAPI at baseline and 22 due to no cannabis use at baseline. For the longitudinal analyses, inclusionary criteria comprised of cannabis use reported at that assessment interval; participants that reported no cannabis use or no MAPI at a follow-up assessment interval were excluded for that particular interval.
The purpose of the three outpatient clinical trials was to test interventions designed to increase the efficacy of Motivational Enhancement Therapy combined with Cognitive Behavioral Therapy (MET/CBT) for problematic substance use among clinically referred substance-using youth. All adolescents in the Arkansas 1 (AR-1) (Stanger et al., 2017), Arkansas 2 (AR-2) (Stanger et al., 2015), and the Vermont trials (VT) (Stanger et al., 2009), received 14 weeks of MET/CBT (Sampl & Kadden, 2001; Webb, Scudder, Kaminer, & Kaiden, 2002). Additionally, adolescents were randomly assigned to receive abstinence-based contingency management (CM) or no CM. The Institutional Review Board (IRB) of the University of Arkansas for Medical Sciences approved AR-1 and AR-2 trials, and the IRB at University of Vermont approved the VT trial. The inclusion criteria were as follows: (a) age 12–18 years and living with a legal guardian (b) cannabis use in the past 30-days or a cannabis-positive urinalysis for AR-2 and VT (c) diagnosis of cannabis abuse or dependence for AR-2, and alcohol use in the past 30-days or an alcohol-positive urinalysis and meeting criteria for alcohol abuse or dependence or at least one binging episode in the past 90-days for AR-1. Notably, the majority (71%) of those enrolled in AR-1 reported cannabis use or evidenced a cannabis-positive urinalysis at baseline despite the inclusionary criteria being contingent on alcohol use (Stanger et al., 2017). Adolescents received treatment for 14-weeks and completed follow-up assessments at 3-, 6-, 9-, and 12-months post-baseline (and 15-month post-baseline for AR-1).
The goal of the two school-based trails was to evaluate the efficacy and optimize outcomes for the MET-based intervention, Teen Marijuana Checkup, designed to intervene in schools with adolescents who endorse frequent cannabis use. The first school-based trial, Washington 1 (WA-1) (Walker et al., 2011) had three conditions: MET, Educational Feedback Control (EFC), and Delayed Feedback Control (DFC); however, adolescents in the DFC condition were not included in the current investigation because the MAPI was not administered at baseline. The MET condition included two sessions of MET, and the EFC condition involved two sessions of psychoeducation about cannabis use. MET and EFC conditions were offered four sessions of individual CBT (Sampl & Kadden, 2001). All adolescents in the second school-based trial, Washington 2 (WA-2) (Walker et al., 2016), received the same two-session MET intervention, and were offered optional CBT sessions as needed. Adolescents were randomized to either MET check-in sessions or “assessment-only” check-in sessions. The IRBs from University of Washington and Virginia Tech approved all procedures for WA-1 and WA-2. The inclusion criteria for the school-based trials were ages 14–19 years for WA-1, 14–17 years for WA-2, and at least nine days of cannabis use in the past 30-days for WA-1 and WA-2. Adolescents completed assessments at 3- and 12-months after the baseline assessment for WA-1 and 6-, 9-, 12-, and 15-month post-baseline for WA-2. Additional details are provided elsewhere for the clinical (VT; AR-2; AR-1) (Stanger et al., 2009; Stanger et al., 2015; Stanger et al., 2017) and school trials (WA-1; WA-2) (Walker et al., 2011; Walker et al., 2016).
2.2. Measures
2.2.1. Cannabis-related problems
The Marijuana Adolescent Problem Inventory (MAPI) is a 23-item measure indexing severity of problems related to cannabis use among youth (see Table 1 for full scale). Across trials participants endorsed the number of times problems happened to them as a result or while using marijuana by specifying 0 (0 Times/Never), 1 (1–2 Times), 2 (3–5 Times), 3 (6–10 Times), or 4 (10+ Times).
Table 1.
Full items and standardized item loadings from the one-component principal component analysis.
| Item # | Item | Loading |
|---|---|---|
| 01 | Not able to do your homework or study for a test | 0.61 |
| 02 | Got into fights, acted bad or did mean things | 0.53 |
| 03 | Missed out on other things because you spent too much money on marijuana | 0.66 |
| 04 | Went to work or school high | 0.40 |
| 05 | Caused shame or embarrassment to someone | 0.55 |
| 06 | Neglected your responsibilities | 0.66 |
| 07 | Relatives avoided you | 0.40 |
| 08 | Felt that you needed MORE marijuana than you used to in order to get the same effect | 0.59 |
| 09 | Tried to control your marijuana use by trying to smoke only at certain times of the day or certain places | 0.18 |
| 10 | Had withdrawal symptoms, that is felt sick (irritated or anxious) because you stopped or cut down using marijuana | 0.64 |
| 11 | Noticed an ongoing or unpleasant change in your personality | 0.67 |
| 12 | Felt that you had a problem with marijuana | 0.71 |
| 13 | Missed a day (or part of a day) of school or work | 0.53 |
| 14 | Tried to cut down or quit smoking marijuana | 0.49 |
| 15 | Suddenly found yourself in a place you could not remember getting to | 0.52 |
| 16 | Passed out or fainted suddenly | 0.38 |
| 17 | Had a fight, argument, or bad feelings with a friend | 0.60 |
| 18 | Had a fight, argument, or bad feelings with a family member | 0.53 |
| 19 | Kept smoking marijuana when you promised yourself not to | 0.62 |
| 20 | Felt you were going crazy | 0.60 |
| 21 | Had a bad time | 0.52 |
| 22 | Felt physically or psychologically dependent on marijuana | 0.71 |
| 23 | Was told by a friend or neighbor to cut down on smoking marijuana | 0.59 |
2.2.2. Cannabis use and cannabis abuse and dependence diagnoses
Within the outpatient setting (AR-1, AR-2, and VT), the Timeline Follow-Back interview (Sobell & Sobell, 1992) was utilized to assess the number of days and times per day the adolescent used cannabis the past 90-days (only the most recent 60 of the 90-days were used for analyses). The total number of times per day used was divided by the days used to calculate the average times per day used. The Vermont Structured Diagnostic Interview (Hudziak, Copeland, Stanger, & Wadsworth, 2004) is a clinical interview that was used to index DSM-IV cannabis dependence and abuse in this setting.
Within the school setting (WA-1 and WA-2), recent cannabis use (i.e., total days used and mean times used per day) was indexed via the Global Appraisal of Individual Needs assessment battery (GAIN) (Dennis, Titus, White, Unsicker, & Hodgkins, 2003) by asking the number of days and average times per day the adolescent used cannabis the past 60-days. Symptoms of cannabis abuse and dependence as described in the DSM-IV were assessed by adapting questions from the GAIN (Dennis, 1998) that were self-report (cf., interviewer-based in clinical trials). Participants were scored as having a DSM symptom if they endorsed any of the items assessing that criterion. For all trials, a variable was created comparing cannabis abuse-only to no diagnosis and another variable was created comparing diagnosis of cannabis dependence to diagnosis of cannabis abuse-only (for the latter variable, if a participant met criteria for abuse and dependence, they were coded as dependence).
2.3. General analytic strategy
Descriptive statistics were first conducted; frequencies and means were computed for demographic and cannabis-related characteristics. Chi-square analyses and analyses of variance were employed to investigate whether the demographic and cannabis-related characteristics differed as a function of the five-level categorical variable of randomized trial.
Principal component analysis (PCA) was utilized to examine the factor structure of the MAPI. Three methods for determining the number of components to retain that have demonstrated strong performance (Zwick & Veliger, 1986) were utilized: Cattell’s scree test (Cattell, 1966), the minimum average partial (MAP) test (Velicer, 1976a, 1976b) and Horn’s parallel analysis (Horn, 1965). As the MAPI was designed to measure one construct, marijuana problems, a one-component solution was hypothesized. As a validity check for the combined sample, follow-up analyses were conducted on the two settings that comprised the combined sample (outpatient and school settings). Confirmatory factor analysis (CFA) (Kline, 2011) was used to test the factor structure suggested by the PCA. Model fit was assessed with multiple indices, including the chi-square test, Comparative Fit Index (CFI), Nonnormed Fit Index (NNFI), and Root Mean Squared Error of Approximation (RMSEA). A significant chi-square test suggests fit could be improved, but this statistic is sensitive to large sample sizes and large numbers of variables (Bentler & Bonett, 1980; Hu & Bentler, 1999; Kline, 2011). Factorial invariance was also tested across the outpatient and school settings (Meredith, 1993).
Internal consistency reliability was assessed with Cronbach’s coefficient alpha (Cronbach, 1951). Internal reliability was tested with Spearman-Brown split-half reliability, and test-retest reliability was assessed with Pearson correlations across intervals ranging from baseline to 15 months. To examine the external validity of the MAPI, relations among scores, number of days cannabis used, and mean times used per day were tested among the intervals with Pearson correlations; baseline MAPI score was tested in relation to baseline diagnosis of cannabis dependence and abuse and also as a predictor of future cannabis use in a series of linear and logistic regression analyses. The five-level categorical variable of randomized trial was utilized as a covariate in the linear and logistic regression models instead of treatment condition considering adolescents in all trial conditions received some type of therapy. The covariate of race was coded dichotomously including White, non-Hispanic compared to all other races and ethnicities.
3. Results
3.1. Descriptive analyses
Mean age did not differ by trial; however, gender, race, ethnicity, cannabis dependence diagnosis, days of cannabis used, and mean times of cannabis used per day did differ across trials (Table 2). Some of the general trends of trial characteristics were as follows: WA-2 had the highest percentage of participants identifying as Hispanic, AR-1 had the lowest percentage of participants identifying as White and non-Hispanic and the lowest rates of cannabis dependence, WA-1 and WA-2 consistently reported the highest frequency of cannabis use, and finally VT and AR-1 had the highest percentages of male participants.
Table 2.
Sample characteristics at baseline combined and broken down by individual randomized trial.
| VT (n = 69) | AR 1 (n = 153) | AR 2 (n = 53) | WA 1 (n = 201) | WA 2 (n = 251) | χ2 or F | Combined sample (n = 727) | |
|---|---|---|---|---|---|---|---|
| Mean age | 16.0 (SD = 1.1) | 15.8 (SD = 1.3) | 16.2 (SD = 1.2) | 16.0 (SD = 1.2) | 15.8 (SD = 0.96) | 1.6 | 15.9 (SD = 1.2) |
| Gender (male) | 82.6% | 88.9% | 73.6% | 67.2% | 68.5% | 29.2* | 74.1% |
| Race (White) | 85.5% | 34.6% | 79.2% | 66.7% | 57.0% | 75.4* | 59.3% |
| Ethnicity (Hispanic) | 2.9% | 1.3% | 2.4% | 3.5% | 10.4% | 20.3* | 5.3% |
| DSM cannabis dependence | 43.5% | 29.4% | 54.7% | 62.7% | 52.2% | 40.8* | 49.7% |
| DSM cannabis abuse only | 44.9% | 69.9% | 37.7% | 22.4% | 17.9% | 40.3* | 34.1% |
| Days cannabis used (out of 60) | 29.1 (SD = 20.7) | 22.7 (SD = 18.9) | 25.5 (SD = 20.4) | 38.9 (SD = 15.3) | 37.1 (SD = 15.1) | 27.2* | 33.0 (SD = 18.2) |
| Mean times cannabis used per day | 2.0 (SD = 1.4) | 1.8 (SD = 1.0) | 2.0 (SD = 1.4) | 2.8 (SD = 1.9) | 2.8 (SD = 2.8) | 9.1* | 2.5 (SD = 2.1) |
p < 0.05
3.2. Primary hypothesis testing
3.2.1. Principal component analysis
PCA was performed on a randomly split half of the combined data (n = 363). Visual assessment of the scree plot (Fig. 1) suggested a one-component solution, with a very dramatic drop-off in variance explained from the first component (31.9%) to the second component (7.2%). In the MAP test, the squared partial correlation was the smallest for the one-component solution. In parallel analysis, the eigenvalue for the first and second components, were greater than their corresponding randomly generated data eigenvalues, which suggested a possible two-component solution. However, a one-component solution was selected based on the screen plot and MAP test results. The item-level loadings from PCA (Table 1) ranged from 0.18 to 0.71 with an average loading of 0.55. Separate PCAs were conducted on the outpatient clinic (n = 275) and school (n = 452) samples. As with the random half of the combined data, the scree plot and MAP test supported a one-component solution for both settings.
Fig. 1.
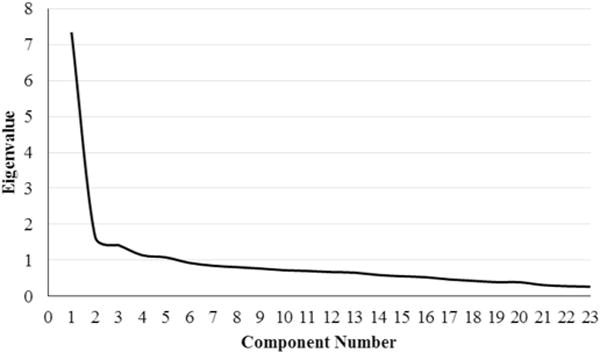
Scree plot of eigenvalues from PCA.
3.2.2. Confirmatory factor analysis
CFA was performed on the other half of the combined data (n = 364) to test the one-factor structure suggested by the PCA results. The model, with one factor and 23 items (Fig. 2), generally demonstrated a good fit, with CFI = 0.82, NNFI = 0.80, and RMSEA = 0.05. The chi-square test was statistically significant, likely due to the large number of indicators for the one factor: χ2 (230, n = 364) = 674.38 (p < 0.05). The standardized item loadings from CFA (Fig. 2) ranged from 0.23 to 0.66 with an average loading of 0.51. The highest level of factorial invariance tested, which required equal factor loadings and equal measurement variances, held across the outpatient (n = 275) and school (n = 452) settings with an acceptable level of fit compared to the combined data (CFI = 0.75, NNFI = 0.74, RMSEA = 0.05).
Fig. 2.
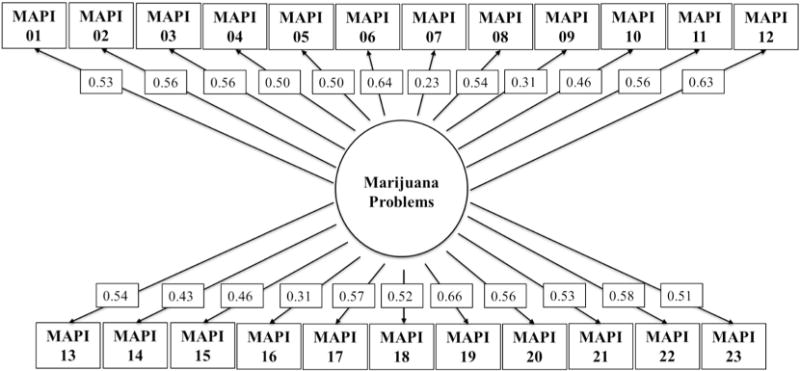
One-factor confirmatory factor analysis model with standardized loadings.
3.2.3. Reliability
Reliability was assessed with the full combined sample (N = 727). Cronbach’s coefficient alpha for internal consistency reliability was α = 0.89 and Spearman-Brown split-half reliability was ρ = 0.88, both of which suggest good internal reliability. The MAPI also demonstrated evidence of test-retest reliability; all but one (between MAPI at 3- and 15-months) of the correlations of MAPI scores across the follow-up interval were statistically significant (p < 0.05) (Table 3). The mean longitudinal correlation for MAPI scores 3 months apart (e.g., baseline MAPI score correlated with MAPI at 3-months) was r = 0.42, and r = 0.38 for the longest interval (15-months).
Table 3.
Test-retest reliability of total MAPI scores, baseline to 15 months.
| MAPI score 03 | MAPI score 06 | MAPI score 09 | MAPI score 12 | MAPI score 15 | |
|---|---|---|---|---|---|
| MAPI score 00 | 0.51* | 0.46* | 0.43* | 0.33* | 0.38* |
| MAPI score 03 | 0.42* | 0.41* | 0.54* | 0.25 | |
| MAPI score 06 | 0.69* | 0.56* | 0.56* | ||
| MAPI score 09 | 0.66* | 0.61* | |||
| MAPI score 12 | 0.75* |
Note. The reliability of the MAPI was assessed from baseline to 15 months using the following assessment intervals: 00 (baseline), 03 (3-months), 06 (6-months), 09 (9-months), 12 (12-months), and 15 (15-months).
p < 0.05.
3.2.4. External validity
In two logistic regression analyses, controlling for gender, race, and trial, baseline MAPI score was associated with increased odds of having a baseline diagnosis of cannabis abuse compared to no diagnosis OR = 1.13 (95% CI = 1.07–1.19, p < 0.001) and diagnosis of cannabis dependence compared to abuse-only, OR = 1.15 (95% CI = 1.12–1.18, p < 0.001). Correlations among MAPI scores and number of days cannabis used were assessed at all assessment intervals (Table 4). Of the 36 correlations, most (25/36) were positive and statistically significant. The mean cross-sectional correlation (e.g., MAPI score at 3 months correlated with number of days cannabis used at 3 months) was r = 0.27, and the mean longitudinal correlation was r = 0.12. Correlations among MAPI scores and the mean times cannabis used per day were also assessed at all assessment intervals (Table 4). Of the 36 correlations, more than half (20/36) were positive and statistically significant. The mean cross-sectional correlation was r = 0.18, and the mean longitudinal correlation was r = 0.11.
Table 4.
Correlations among total MAPI scores, number of days cannabis used, and mean times cannabis used per day, baseline to 15 months.
| a. Number of days cannabis used
| ||||||
|---|---|---|---|---|---|---|
| Days used 00 | Days used 03 | Days used 06 | Days used 09 | Days used 12 | Days used 15 | |
| MAPI score 00 | 0.32* | 0.17* | 0.07 | 0.04 | 0.06 | 0.06 |
| MAPI score 03 | 0.20* | 0.26* | 0.15 | 0.10 | 0.13* | 0.04 |
| MAPI score 06 | 0.16* | 0.24 | 0.18* | 0.14* | 0.18* | 0.07 |
| MAPI score 09 | 0.19* | 0.33* | 0.25* | 0.29* | 0.28* | 0.19* |
| MAPI score 12 | 0.17* | 0.22* | 0.23* | 0.23* | 0.35* | 0.17* |
| MAPI score 15 | 0.09 | 0.02 | 0.17* | 0.19* | 0.18* | 0.19* |
| b. Mean times cannabis used per day
| ||||||
|---|---|---|---|---|---|---|
| Mean used 00 | Mean used 03 | Mean used 06 | Mean used 09 | Mean used 12 | Mean used 15 | |
| MAPI score 00 | 0.15* | 0.19* | 0.18* | 0 | 0.01 | 0.12* |
| MAPI score 03 | 0.15* | 0.23* | 0.03 | − 0.01 | 0.18* | − 0.04 |
| MAPI score 06 | 0.09 | 0.22 | 0.30* | 0.21* | 0.25* | 0.04 |
| MAPI score 09 | 0.04 | 0.28* | 0.16* | 0.08 | 0.11* | 0.11 |
| MAPI score 12 | 0.04 | 0.22* | 0.14* | 0.11 | 0.16* | 0.13 |
| MAPI score 15 | 0.06 | − 0.02 | 0.26* | 0.19* | 0.25* | 0.18* |
Note. The correlations were assessed from baseline to 15 months using the following assessment intervals: 00 (baseline), 03 (3-months), 06 (6-months), 09 (9-months), 12 (12-months), and 15 (15-months).
p < 0.05.
Controlling for gender, race, DSM cannabis dependence, and trial, baseline MAPI score predicted mean times cannabis used per day 3 months later (overall model F(5, 437) = 22.67, p < 0.001; MAPI score t(1) = 2.41, p = 0.016, β = 0.13) and 6 months later (overall model F(5, 439) = 11.29, p < 0.001; MAPI score t(1) = 3.39, p = 0.001, β = 0.18). Baseline MAPI score did not significantly predict mean times cannabis used per day beyond 6 months or significantly predict the number of days cannabis used for any interval after accounting for covariates.
4. Conclusion
The current investigation assessed the psychometric properties of the MAPI, a widely-used youth measure of cannabis use problem severity. Factor structure and reliability findings suggest that the MAPI is internally consistent and reliable. Findings also suggest that the MAPI measures one latent construct, with no differences in factor structure between the outpatient and school settings. This finding is consistent with the recommended use of the RAPI as a unidimensional scale to measure adolescent problem drinking (White & Labouvie, 1989). External validity of the MAPI was demonstrated as evidenced by significant relations with frequency of cannabis use (i.e., days used and times per day used) across most assessment intervals. Further, MAPI baseline score predicted concurrent diagnosis of cannabis dependence compared to abuse-only and abuse compared to no diagnosis; baseline MAPI score also significantly predicted mean times per day used assessed at the 3- and 6-month follow-up intervals after accounting for covariates. Overall, this initial test of the psychometrics of the MAPI suggests that it can be considered a reliable and valid measure of problems associated with cannabis use.
Several important limitations of this study warrant discussion. First, the school and outpatient settings each utilized different indices of cannabis use and diagnosis of abuse and dependence that may have affected the precision and error of measurement. Research attention should be allocated to replicating the MAPI’s validity using a common index of cannabis use frequency and related diagnoses among samples of heterogeneous cannabis users. Second, the current study included samples of convenience from outpatient and school settings and the majority of youth were male and Caucasian and agreed to participate in cannabis intervention study. Relatedly, the MAPI was only collected post-baseline from adolescents that reported cannabis use in the 60 days prior to each assessment. An important next step in this line of work is to prospectively evaluate the MAPI’s psychometric properties across different contexts and among important subpopulations (e.g., homeless youth, ethno-racial minorities, adolescent females) (Ginzler, Garrett, Baer, & Peterson, 2007) to verify its factor structure, reliability, and validity across diverse settings and populations and outside the context of an intervention. If the psychometric properties are replicated in more diverse samples, it may be useful to include the MAPI in studies to help identify problematic trajectories for adolescent cannabis use, similar to problem-drinking trajectories (e.g., no or low problem, adolescent-limited problem, and escalating problem) (Warner et al., 2007). Further, studies comparing the cannabis- and alcohol-related problematic trajectories to evaluate their co-occurrence and overlap may help clarify our understanding of the polysubstance use commonly observed in adolescents.
Future research might also target development of a shorter version of the MAPI to serve as a brief assessment tool. To help inform the particular items to remove, investigators could examine the inter-correlations to reveal redundant items, perform factor analyses to replicate and detect the weaker-performing items (i.e., items 9 and 16 in the current study), or conduct differential item functioning analysis to identify items vulnerable to bias (e.g., potential sex biased items, as used to develop the brief RAPI) (Earleywine, LaBrie, & Pedersen, 2008). Identification of optimal cut off values that predict dependence would also be useful. Collectively, a short assessment tool with standardized cut off values could aid in quickly identifying those adolescents in need of treatment or most at risk in hospital or clinic settings, and also in elucidating the adolescent’s most problematic areas to optimize intervention efforts.
Given the timely importance of assessing the impact of cannabis use on developing youth, the goal of the current investigation was to evaluate the psychometric properties of the MAPI that measures problem severity related to cannabis use. Analyses suggested that the MAPI is unidimensional and a reliable, valid measure of cannabis use problems in adolescents, and thus a promising measure to assess severity that can be used to screen or measure change over time. Future work is now needed to extend the current findings by further testing the psychometric properties of the MAPI among unique subpopulations and developing a short version to be used as a brief assessment tool.
HIGHLIGHTS.
Marijuana Adolescent Problem Inventory (MAPI) indexes cannabis use problem severity.
Psychometric findings suggest that the MAPI is internally consistent and reliable.
Factor structure analyses support a one-component solution.
Initial tests suggest the MAPI is a promising measure to assess problem severity.
Acknowledgments
Role of funding sources
Research supported by National Institute on Alcohol Abuse and Alcoholism (NIAAA) and National Institute of Drug Abuse (NIDA) (T32DA037202, R01DA015186, 1R01DA014296, 1R01DA014296-01A1, R01AA016917, P30DA029926). NIAAA and NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Contributors
Dr. Budney and Dr. Stanger designed and conducted the AR-1, AR-2 and VT trials. Dr. Walker and Dr. Stephens designed and conducted WA-1 and WA-2 trials. Dr. Scherer assisted in data processing and data management for the AR-1, AR-2, and VT trial data. Dr. Babbin conducted the majority of statistical analyses and wrote the majority of the results section. Dr. Knapp conducted additional statistical analyses and completed the initial draft of the manuscript with Dr. Stanger and Dr. Budney. All authors contributed to and have approved the final manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest.
References
- Bashford J, Flett R, Copeland J. The cannabis use problems identification test (cupit): Development, reliability, concurrent and predictive validity among adolescents and adults. Addiction. 2010;105(4):615–625. doi: 10.1111/j.1360-0443.2009.02859.x. http://dx.doi.org/10.1111/j.1360-0443.2009.02859.x. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Blevins CE, Banes KE, Stephens RS, Walker DD, Roffman RA. Motives for marijuana use among heavy-using high school students: An analysis of structure and utility of the comprehensive marijuana motives questionnaire. Addictive Behaviors. 2016;57:42–47. doi: 10.1016/j.addbeh.2016.02.005. http://dx.doi.org/10.1016/j.addbeh.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CE, Walker DD, Stephens RS, Banes KE, Roffman RA. Changing social norms: The impact of normative feedback included in motivational enhancement therapy on cannabis outcomes among heavy-using adolescents. Addictive Behaviors. 2018;76:270–274. doi: 10.1016/j.addbeh.2017.08.030. http://dx.doi.org/10.1016/j.addbeh.2017.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Two brief alcohol interventions for mandated college students. Psychology of Addictive Behaviors. 2005;19(3):296–302. doi: 10.1037/0893-164X.19.3.296. http://dx.doi.org/10.1037/0893-164X.19.3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Neal DJ, Collins SE, Carey KB. Differential utility of three indexes of risky drinking for predicting alcohol problems in college students. Psychology of Addictive Behaviors. 2001;15(4):321–324. doi: 10.1037//0893-164x.15.4.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattell RB. The screen test for the number of factors. Multivariate Behavioral Research. 1966;1(2):245–276. doi: 10.1207/s15327906mbr0102_10. http://dx.doi.org/10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Key substance use and mental health indicators in the united states: Results from the 2015 national survey on drug use and health. 2016 Retrieved from http://www.samhsa.gov/data/
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;3:297–334. [Google Scholar]
- Dennis M. Global appraisal of individual needs (gain) manual: Administration, scoring and interpretation (prepared with funds from csat ti 11320) Bloomington, IL: Lighthouse Publications; 1998. [Google Scholar]
- Dennis M, Titus J, White M, Unsicker J, Hodgkins D. Administration guide for the gain and related measures. 5th. Bloomington, IL: Chestnut Health Systems; 2003. [Google Scholar]
- Dick DM, Aliev F, Viken R, Kaprio J, Rose RJ. Rutgers alcohol problem index scores at age 18 predict alcohol dependence diagnoses 7 years later. Alcoholism, Clinical and Experimental Research. 2011;35(5):1011–1014. doi: 10.1111/j.1530-0277.2010.01432.x. http://dx.doi.org/10.1111/j.1530-0277.2010.01432.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diestelkamp S, Arnaud N, Sack PM, Wartberg L, Daubmann A, Thomasius R. Brief motivational intervention for adolescents treated in emergency departments for acute alcohol intoxication - a randomized-controlled trial. BMC Emergency Medicine. 2014;14:13. doi: 10.1186/1471-227X-14-13. http://dx.doi.org/10.1186/1471-227X-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earleywine M, LaBrie JW, Pedersen ER. A brief Rutgers alcohol problem index with less potential for bias. Addictive Behaviors. 2008;33(9):1249–1253. doi: 10.1016/j.addbeh.2008.05.006. http://dx.doi.org/10.1016/j.addbeh.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. Journal of Consulting and Clinical Psychology. 2011;79(6):728–739. doi: 10.1037/a0026074. http://dx.doi.org/10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing S, McEachern A, Yezhuvath U, Bryan A, Hutchison K, Filbey F. Integrating brain and behavior: Evaluating adolescents’ response to a cannabis intervention. Psychology of Addictive Behaviors. 2013;27(2):510–525. doi: 10.1037/a0029767. http://dx.doi.org/10.1037/a0029767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Swain-Campbell N. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 2002;97(9):1123–1135. doi: 10.1046/j.1360-0443.2002.00103.x. [DOI] [PubMed] [Google Scholar]
- Ginzler J, Garrett S, Baer J, Peterson P. Measurement of negative consequences of substance use in street youth: An expanded use of the Rutgers alcohol problem index. Addictive Behaviors. 2007;32:1519–1525. doi: 10.1016/j.addbeh.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Horn JL. A rational and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hudziak JJ, Copeland W, Stanger C, Wadsworth M. Screening for dsm-iv externalizing disorders with the child behavior checklist: A receiver-operating characteristic analysis. Journal of Child Psychology and Psychiatry. 2004;45(7):1299–1307. doi: 10.1111/j.1469-7610.2004.00314.x. http://dx.doi.org/10.1111/j.1469-7610.2004.00314.x. [DOI] [PubMed] [Google Scholar]
- Johnson V, White HR. An investigation of factors related to intoxicated driving behaviors among youth. Journal of Studies on Alcohol. 1989;50(4):320–330. doi: 10.15288/jsa.1989.50.320. [DOI] [PubMed] [Google Scholar]
- Johnston L, O’Malley P, Miech R, Bachman J, Schulenberg E. Monitoring the future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- Kazdin A. Research design in clinical psychology. 4th. London, England: Pearson; 2003. [Google Scholar]
- Kline RB. Principles and practice of structure equation modeling. 3rd. New York, NY: The Guilford Press; 2011. [Google Scholar]
- Martin G, Copeland J, Gilmour S, Gates P, Swift W. The adolescent cannabis problems questionnaire (cpq-a): Psychometric properties. Addictive Behaviors. 2006;31(12):2238–2248. doi: 10.1016/j.addbeh.2006.03.001. http://dx.doi.org/10.1016/j.addbeh.2006.03.001. [DOI] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, Moffitt TE. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(40):E2657–2664. doi: 10.1073/pnas.1206820109. http://dx.doi.org/10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith W. Measurement invariance, factor analysis, and factorial invariance. Psychometrika. 1993;58:521–543. [Google Scholar]
- Norberg MM, Battisti RA, Copeland J, Hermens DF, Hickie IB. Two sides of the same coin: Cannabis dependence and mental health problems in help-seeking adolescent and young adult outpatients. International Journal of Mental Health Addiction. 2012;10(6):818–828. doi: 10.1007/s11469-012-9378-1. http://dx.doi.org/10.1007/s11469-012-9378-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampl S, Kadden R. Motivational enhancement therapy and cognitive behavioral therapy for adolescent cannabis users: 5 sessions, cannabis youth treatment (cyt) series, vol 1 (dhhs publication no Sma 01-3486) Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental health Services Administration (BKD384); 2001. [Google Scholar]
- Silins E, Horwood L, Patton G, Fergusson D, Olsson C, Hutchinson D, Mattick R. Young adult sequelae of adolescent cannabis use: An integrative analysis. Lancet Psychiatry. 2014;1(4):286–293. doi: 10.1016/S2215-0366(14)70307-4. http://dx.doi.org/10.1016/S2215-0366(14)70307-4. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stanger C, Budney AJ, Kamon JL, Thostensen J. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug and Alcohol Dependence. 2009;105(3):240–247. doi: 10.1016/j.drugalcdep.2009.07.009. http://dx.doi.org/10.1016/j.drugalcdep.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Ryan SR, Scherer EA, Norton GE, Budney AJ. Clinic- and home-based contingency management plus parent training for adolescent cannabis use disorders. Journal of American Academy of Child and Adolescent Psychiatry. 2015;54(6):445–453. (e442). doi: 10.1016/j.jaac.2015.02.009. https://doi.org/10.1016/j.jaac.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Scherer EA, Babbin SF, Ryan SR, Budney AJ. Abstinence based incentives plus parent training for adolescent alcohol and other substance misuse. Psychology of Addictive Behaviors. 2017 doi: 10.1037/adb0000279. http://dx.doi.org/10.1037/adb0000279. [DOI] [PMC free article] [PubMed]
- Vandrey R, Budney AJ, Kamon JL, Stanger C. Cannabis withdrawal in adolescent treatment seekers. Drug and Alcohol Dependence. 2005;78(2):205–210. doi: 10.1016/j.drugalcdep.2004.11.001. http://dx.doi.org/10.1016/j.drugalcdep.2004.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976a;41:321–327. [Google Scholar]
- Velicer WF. The relation between factor score estimates, image scores and principal component scores. Educational and Psychological Measurement. 1976b;36:149–159. [Google Scholar]
- Walker DD, Stephens R, Roffman R, Demarce J, Lozano B, Towe S, Berg B. Randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: A further test of the teen marijuana check-up. Psychology of Addictive Behaviors. 2011;25(3):474–484. doi: 10.1037/a0024076. http://dx.doi.org/10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens RS, Blevins CE, Banes KE, Matthews L, Roffman RA. Augmenting brief interventions for adolescent marijuana users: The impact of motivational check-ins. Journal of Consulting and Clinical Psychology. 2016;84(11):983–992. doi: 10.1037/ccp0000094. http://dx.doi.org/10.1037/ccp0000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner LA, White HR, Johnson V. Alcohol initiation experiences and family history of alcoholism as predictors of problem-drinking trajectories. Journal of Studies on Alcohol and Drugs. 2007;68(1):56–65. doi: 10.15288/jsad.2007.68.56. [DOI] [PubMed] [Google Scholar]
- Webb C, Scudder M, Kaminer Y, Kaiden R. The motivational enhancement therapy and cognitive behavioral therapy supplement: 7 sessions of cognitive behavioral therapy for adolescent cannabis users: Cannabis youth treatment (cyt) series. Vol. 2. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2002. [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50(1):30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Zwick WR, Veliger WF. Comparison of five rules for determining the number of components to retain. Psychological Bulletin. 1986;99(3):432. [Google Scholar]


