Abstract
Background
Hydrodilatation (HD) has been shown to improve pain and function in patients with adhesive capsulitis (AC). There is no consensus concerning how HD should be performed or what volume should be injected. It has distinct advantages compared to surgery; however, it is a painful procedure and is often poorly tolerated.
Methods
We retrospectively reviewed all patients referred for HD over a 2.5-year period aiming to assess whether volume injected influences outcome.
Results
There were 107 patients treated with HD; of these, 76 (43 female, 32 male) had full data for analysis. The majority were classified as primary AC (n = 57) with an average age of 55.5 years. The mean improvement in Oxford Shoulder Score (OSS) was 12.1, with females (13.9) and post-traumatic cases of AC (14.1) demonstrating the best outcome. No complications were observed during the HD process. There was a negative correlation observed between volume injected and OSS improvement. Only two patients experienced a poor outcome and required further treatment with manipulation +/– arthroscopic arthrolysis.
Conclusions
The present study supports the use of HD as a first line treatment for AC regardless of the underlying cause, and also demonstrates that the volume injected does appear to influence the outcome.
Keywords: adhesive capsulitis, arthrographic distension, frozen shoulder, hydrodilatation
Introduction
Adhesive capsulitis (AC), also known as frozen shoulder, is an intensely debilitating condition usually characterized by a gradual onset of severe pain and global limitation of both active and passive shoulder movements. It was first described in 1872 as an inflammatory process affecting the sub-acromial bursa,1,2 although the term ‘frozen shoulder’ was not introduced until 1934 by Codman.3 We do not fully understand the aetiology of AC and the majority of cases are classified as primary/idiopathic in nature. It has been linked to systemic illnesses such as diabetes mellitus4–6 and can also be precipitated by trauma to the glenohumeral joint. It is generally assumed to affect 2% to 5% of the general population,7 and a recent study approximated that there were 14,000 surgical interventions performed in England for AC each year.8
Hydrodilation (HD), also known as arthrographic distension, was first reported in 1965.9 It typically involves injecting a volume of liquid into the joint in an attempt to distend, dilate or ideally rupture the tight fibrotic capsule. It is usually combined with a steroid injection and followed by a course of physiotherapy to restore shoulder movements. A Cochrane review in 2008 concluded that there was ‘silver’ level evidence for arthrographic distension to provide short-term benefits in pain, range of movement and function.10 However, there have been several randomized controlled trials that have demonstrated no difference compared to steroid injection alone, or versus placebo.11–14
At present, there are a variety of different HD techniques described in the literature and there remains no clear consensus regarding the most effective technique. Rizk et al.15 injected the same volume (30 mL) for all 16 patients in their study and reported a 100% capsular rupture rate. The majority of studies, however, suggest that the volume injected should be adjusted or tailored to each individual patient.11,16,17 The procedural endpoint should ideally be radiological evidence of capsular rupture but, in practice, it is generally performed up to the patient’s individual tolerance. The volumes used in the current literature range from 10 mL to 100 mL. Tveita et al.14 reported rupture in their series with as little as 10 mL. The majority of HD studies report on the outcome after a single procedure, although some studies have described a protocol that involves attempted weekly HD over a 6-week period.12
The aim of the present study was to examine whether the volume injected during HD has any influence on the outcome of the procedure.
Materials and methods
Between April 2013 and October 2015, we collected data on all patients undergoing HD. Appropriate local review board approval for the research has been obtained. Data were collected prospectively but reviewed retrospectively.
Our inclusion criteria were all patients referred for HD by one of the three senior investigators (consultant orthopaedic surgeon). A clinical diagnosis of adhesive capsulitis was made based on Codman’s criteria, with pain and associated loss of both active and passive shoulder movements, particularly external rotation. All patients reported at least 2 months of symptoms. HD is the first line treatment for AC in our institution, and all procedures were performed by a single radiologist (RM).
The primary outcome measure used was the Oxford Shoulder Score (OSS). This is an easy to use and validated patient reported outcome measure consisting of 12 questions with a maximum score of 48. It assesses both shoulder pain and function, with a change of >6 being needed to be clinically relevant.18,19
The patient’s case notes, clinic letters and procedure reports were reviewed. Each patient’s age, hand dominance, history of presenting complaint and past medical history were recorded. Information available for each HD included a pre-procedural OSS, procedure technique, total volume of saline injected, use of Entonox (BOC Healthcare, Manchester, UK), whether the procedure was completed or abandoned, and whether it was considered to be a success. A success was either radiological evidence of capsular rupture or significant distension/audible pop with immediate improved range of movement. The physiotherapy notes and follow-up orthopaedic documentation were reviewed for each patient to establish a post procedural OSS, as well as the need for any further treatment with manipulation under anaesthetic (MUA) or arthroscopic arthrolysis (AA).
Entonox was introduced during the study period and was offered to all patients experiencing pain during the procedure.
Statistical analysis was performed using StatsDirect (StatsDirect Ltd, Altrincham, UK) and the integrated statistical tools of Excel (Microsoft Corp., Redmond, WA, USA). The Mann–Whitney U-test was used for continuous data and the chi-squared test was used for noncontinuous data. p < 0.05 was considered statistically significant.
Hydrodilatation technique
The patient lies on a fluoroscopy couch, supine with the shoulder to be injected exposed. A radiopaque marker (paperclip) is placed over the superior/medial quadrant of the humeral head above the epiphyseal line. Gentle pressure is applied to make an impression on the skin before it is cleaned with chlorhexadine solution and 2 mL of 1% lidocaine is injected.
A 21-gauge needle is inserted into the shoulder joint and 2 mL of saline is injected, if flowing freely (within rotator cuff interval), then a water soluble contrast is injected to confirm position. If intra-articular contrast is confirmed on screening, steroid (40 mg of Kenalog; Bristol-Myers Squibb Company, Princeton, NJ, USA) is injected via a three-way tap with a short connecting tube, followed by 10 mL of 0.5% chirocaine, which is injected slowly.
After a few minutes, the shoulder is injected with a mixture of saline and contrast during the screening. This is continued until there is radiological evidence of capsular rupture or the patient reaches their volume tolerance. A heavy duty luer lock syringe can be used to inject when large volume/pressures are required. Entonox via a mouth piece is supplied to the patient throughout the procedure to help alleviate any pain or discomfort experienced. After the procedure, the patient is examined to ensure increased range of motion, which can often take 5 minutes to 10 minutes.
A standardized physiotherapy regime was started within a week of the HD procedure. Patients had to satisfy an objective set of criteria prior to discharge, including a functional range of movement and patient-rated symptom improvement.
Results
In total, 107 patients were referred for HD and 80 of these had data available for analysis. Four patients were unable to tolerate the procedure and were not included, giving us a study cohort of 76 patients. Of the 27 patients with missing data, 15 had no pre-procedural OSS and 12 had either no documented follow-up or failed to attend follow-up and could not be contacted.
The average length of follow up post procedure was 3.5 months (range 1.5 months to 9 months), which represented the date of discharge from either clinician or physiotherapy follow-up. Final, postoperative OSS were collected at this final follow-up. The demographic characteristics of the cohort are reported in Table 1.
Table 1.
Study group demographics and Oxford Shoulder Scores.
| Group | All who had procedure |
|---|---|
| Number | 76 |
| Mean age (years) | 55.5 |
| Male | 32 |
| Female | 44 |
| Mean OSS Pre HD | 20.6 |
| Mean OSS Post HD | 32.7 |
| Mean change OSS | 12.1 |
HD, hydrodilatation; OSS, Oxford Shoulder Score.
There were 44 (58%) females and 32 (42%) males. The mean age was 55.5 years (range 43 years to 66 years). The mean (range) of pre-operative OSS was 20.3 (2 to 38). The mean (range) postoperative OSS was 32.2 (6 to 48) and the difference was significant (p < 0.00001), confirming the treatment effect of HD. The mean overall improvement in OSS was 12.1.
Fifty-seven (75%) patients were classified as primary (idiopathic) AC, and there were 11 (14%) diabetics. Eight (11%) patients developed AC after either a shoulder dislocation of proximal humeral fracture, and were classified as post-traumatic with a mean time from injury to intervention of 9 months. More details of each aetiological group are provided in Table 2.
Table 2.
Oxford Shoulder Scores for each sub-group.
| Males | Female | Idiopathic | Diabetic | Post trauma | |
|---|---|---|---|---|---|
| Number | 32 | 44 | 57 | 11 | 8 |
| Mean age (years) | 57.2 | 54.4 | 53.4 | 56.7 | 62.2 |
| Male | – | – | 22 | 5 | 5 |
| Female | – | – | 35 | 6 | 3 |
| OSS Pre | 20.9 | 20.4 | 20.8 | 21 | 19 |
| OSS Post | 30.6 | 34.3 | 32.9 | 32 | 33.1 |
| Change OSS | 9.7 | 13.9 | 12.1 | 11 | 14.1 |
OSS, Oxford Shoulder Score.
Female patients achieved a greater mean OSS improvement (13.9) compared to males (9.7), although the difference was not significant (p = 0.076). The treatment effect of HD was not affected by the aetiology or diabetic status of the patient. Patients who received HD for post traumatic AC made the greatest improvement in OSS (n = 8, 14.1), although this is difficult to interpret as a result of the small sample size and did not reach significance (p = 0.64).
Further sub-analysis was performed by categorized patients as having received low (<30 mL), standard (30 mL to 50 mL) or high (≥50 mL) volume HD. Fifteen (20%) patients received low, 45 (59%) received standard and 16 (21%) received high volume HD. The characteristic of each subgroup is detailed in Table 3.
Table 3.
Volume (mls) versus change in Oxford Shoulder Score.
| <30 mL | 30 mL to 50 mL | >50 mL | |
|---|---|---|---|
| Number | 15 | 45 | 16 |
| Mean age (years) | 51.25 | 55.9 | 56.4 |
| Male | 5 | 18 | 9 |
| Female | 10 | 27 | 7 |
| Mean OSS Pre | 18.3 | 20.6 | 22.8 |
| Mean OSS Post | 29.6 | 34.2 | 31.4 |
| Mean Change OSS | 11.3 | 13.6 | 8.6 |
OSS, Oxford Shoulder Score.
The treatment effect and improvement in OSS was lowest for the high volume dilatations (8.6; n = 16) and, when compared with the 30 mL to 50 mL volume group (13.6; n = 45), this trended towards significance (p = 0.064).
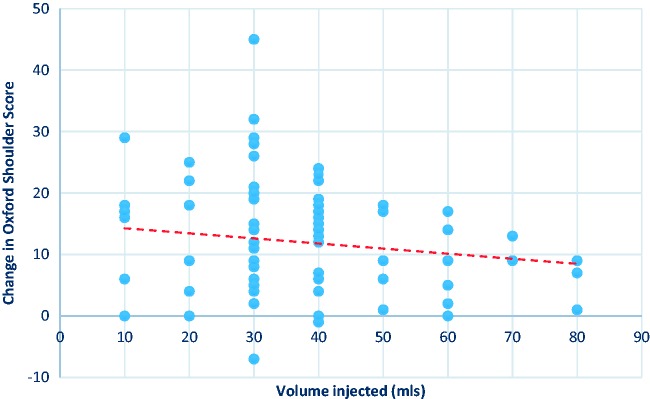
There was a negative correlation observed between HD volume and OSS improvement, as demonstrated in Figure 1. This suggests that larger HD volumes do not convey any additional treatment effect.
Figure 1.
Volume injected versus change in Oxford Shoulder Score (correlation: 0.15).
There was a total of 13 patients referred for HD who were unable to tolerate the procedure and it was therefore abandoned as a result of pain. During the study period, the HD technique evolved to include Entonox as an analgesic adjunct in an attempt to help patients manage any discomfort during HD. Although the addition of Entonox improved the overall tolerability (84% without versus 95% with), the mean improvement in OSS was similar to the treatment group as a whole (11.6 versus 12.1). There were no complications observed in any patient during the HD process.
Ten of the 107 patients referred for HD required surgical management with either MUA or AA; however, eight of these 10 patients had HD abandoned as a result of pain. Of the 94/107 patients who were able to tolerate HD, only two required surgical intervention (2%).
Discussion
This is the first study of HD to investigate the relationship between volume and outcome. Our results support the use of HD as an effective first-line treatment for AC. We found a mean improvement in OSS of 12.1, and this was seen within both primary and secondary cases of AC. Female patients and post-traumatic cases of AC demonstrated the best OSS improvements (13.9 and 14.1), although this was not statistically significant. Our mean OSS improvement (12.1) is lower than other studies have shown for both HD (16.9) and MUA (17); however, their scores were taken over a longer period of follow-up. Similar short-term results were reported (mean OSS improvement of 14) in a study of 51 patients treated with HD, and OSS was demonstrated to continue to improve over time.20,21
A study by Wolf et al.22 of 100 consecutive patients with AC identified that those with a greater number of medical comorbidities had significantly poorer scores on shoulder assessment forms. This poses a problem of having potentially the most difficult to treat patients not being sufficiently fit to undergo general anaesthesia (GA). HD has distinct benefits compared to surgical procedures for AC. There is a considerable reduction in risk to the patient because there is no requirement for GA, making it a very attractive options for patients with multiple comorbidities.
HD is a day-case procedure that is typically performed in a radiology department. Therefore, it requires no formal hospital admission or allocation to a theatre list. We found it to be quicker and easier to organize and it puts no additional pressures on surgical waiting times. There is also a significant cost benefit compared to surgery, ranging from £1440 for a manipulation to £2200 for an arthroscopic release.23
The volumes of saline injected in the present study ranged from 10 mL to 80 mL, with the majority of patients receiving 30 mL to 60 mL. There was no correlation observed between increasing volume and improvement in OSS. Surprisingly, those patients who were able to tolerate very large volumes (>50 mL) did not demonstrate larger improvements in OSS. This perhaps indicates that patients who can accommodate more than 50 mL in volume may have the wrong diagnosis, or that there is minimal or no capsular fibrosis, or even possibly a large rotator cuff tear is present.
Ten of the 107 patients required surgical treatment; however, this was largely a result of the procedure not being tolerated rather than HD not providing a therapeutic effect. Only two patients who completed their procedure required any further treatment (MUA or AA). Thirteen patients were unable to tolerate their procedure and it was abandoned; however, the majority11 of these failures were at the beginning of our study period before the introduction of Entonox.
Although we recognize the limitations of this retrospective study, it remains one of the largest reported series of patients treated with HD. The follow-up period was not standardized for each patient and we are reporting short-term results with an average of 3.5 months, although this does represent a fixed endpoint of discharge. We realize there is no data on shoulder range of motion; however, we consider that the OSS gives a more reliable and valid indication of outcome in this patient group.
As a result of the gradual onset of the disease, it is difficult to determine the exact duration of symptoms before patients underwent HD. However, all patients in the present study had at least a 2-month history of symptoms on presentation to our unit, and a typical wait of <4 weeks from being seen to undergoing HD. Of those patients with a definite preceding event/trauma, the average time from injury to intervention was 9 months. Interestingly, Thomas et al.21 demonstrated that the timing of MUA and a steroid injection in patients with frozen shoulder had no impact on outcome.
In conclusion, the results of the present study support the use of HD for all patient groups, especially in females and post-traumatic AC. However, given the paucity of level 1 evidence, further research is required to compare the different treatment modalities. We recommend that each patient undergoing HD should be injected in an attempt to achieve capsular rupture rather than a specific target volume; however, if achieving volumes >50 mL, then the diagnosis should be carefully considered. Entonox can be used as an effective analgesic adjunct to improve the tolerance of the procedure and, if tolerated, our results show that there is a very low need for further or surgical management.
Acknowledgements
The present report is based on work previously presented as podium presentation at the BESS 2016 Annual Congress, Dublin.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Not required for this article.
References
- 1.Duplay ES. De La Periarthote scapulohumerale. Arch Gen Med 1872; 20: 513–542. [Google Scholar]
- 2.DePalma AF, Brand RA. Loss of scapulohumeral motion (frozen shoulder). Clin Orthop Rel Res 2008; 466: 552–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Codman EA. Tendinitis of the short rotators. In: Codman ES. (ed). The shoulder: rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa, Boston, MA: Thomas Todd and Co, 1934. [Google Scholar]
- 4.Lequesne M, Bang N, Bensasson M, Mery C. Increased association of diabetes mellitus with capsulitis of the shoulder and shoulder-hand syndrome. Scand J Rheumatol 1977; 6: 53–56. [PubMed] [Google Scholar]
- 5.Sattar MA, Luqman WA. Periarthritis: another duration-related complication of diabetes mellitus. Diabetes Care 1985; 8: 507–510. [DOI] [PubMed] [Google Scholar]
- 6.Bridgman JF. Periarthritis of the shoulder in diabetes mellitus. Ann Rheum Dis 1972; 31: 69–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA. Current review of adhesive capsulitis. J Shoulder Elbow Surg 2011; 20: 502–514. [DOI] [PubMed] [Google Scholar]
- 8.Kwaees TA, Charalambous CP. Rates of surgery for frozen shoulder: an experience in England. Muscles Ligaments Tendons J 2015; 5: 276–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andren L, Lundberg BJ. Treatment of rigid shoulders by joint distension during arthrography. Acta Orthop Scand 1965; 36: 45–53. [DOI] [PubMed] [Google Scholar]
- 10.Buchbinder R, Green S, Youd JM, Johnston RV, Cumpston M. Arthrographic distension for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev 2008; 1: CD007005– CD007005. [DOI] [PubMed] [Google Scholar]
- 11.Buchbinder R, Green S, Forbes A, Hall S, Lawler G. Arthrographic joint distension with saline and steroid improves function and reduces pain in patients with painful stiff shoulder: results of a randomised, double blind, placebo controlled trial. Ann Rheum Dis 2004; 63: 302–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gam AN, Schydlowsky P, Rossel I, Remvig L, Jensen EM. Treatment of ‘frozen shoulder’ with distension and glucorticoid compared with glucorticoid alone. A randomised controlled trial. Scand J Rheumatol 1998; 27: 425–430. [DOI] [PubMed] [Google Scholar]
- 13.Corbeil V, Dussault RG, Leduc BE, Fleury J. [Adhesive capsulitis of the shoulder: a comparative study of arthrography with intraarticular corticotherapy and with or without capsular distension]. Can Assoc Radiol J 1992; 43: 127–130. [PubMed] [Google Scholar]
- 14.Tveitå EK, Tariq R, Sesseng S, Juel NG, Bautz-Holter E. Hydrodilatation, corticosteroids and adhesive capsulitis: a randomized controlled trial. BMC Musculoskelet Disord 2008; 9: 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rizk TE, Gavant ML, Pinals RS. Treatment of adhesive capsulitis (frozen shoulder) with arthrographic capsular distension and rupture. Arch Phys Med Rehabil 1994; 75: 803–807. [PubMed] [Google Scholar]
- 16.Quraishi NA, Johnston P, Bayer J, Crowe M, Chakrabarti AJ. Thawing the frozen shoulder. A randomized trial comparing manipulation under anaesthesia with hydrodilatation. J Bone Joint Surg Br 2007; 89: 1197–1200. [DOI] [PubMed] [Google Scholar]
- 17.Bell S, Coghlan J, Richardson M. Hydrodilatation in the management of shoulder capsulitis. Australas Radiol 2003; 47: 247–251. [DOI] [PubMed] [Google Scholar]
- 18.Dawson J, Fitzpatrick R, Carr A. Questionnare on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996; 78: 593–600. [PubMed] [Google Scholar]
- 19.van Kampen DA, Willems WJ, van Beers LW, Castelein RM, Scholtes VA, Terwee CB. Determination and comparison of the smallest detectable change (SDC) and the minimal important change (MIC) of four-shoulder patient-reported outcome measures (PROMs). J Orthop Surg Res 2013; 8: 40–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clement RG, Ray AG, Davidson C, Robinson CM, Perks FJ. Frozen shoulder: long-term outcome following arthrographic distension. Acta Orthop Belg 2013; 79: 368–374. [PubMed] [Google Scholar]
- 21.Thomas WJ, Jenkins EF, Owen JM, et al. Treatment of frozen shoulder by manipulation under anaesthesia and injection: Does the timing of treatment affect outcome? J Bone Joint Br 2012; 94: 574–574. [DOI] [PubMed] [Google Scholar]
- 22.Wolf JM, Green A. Influence of comorbidity on self-assessment instrument scores of patients with idiopathic adhesive capsulitis. J Bone Joint Surg Am 2002; 84: 1167–1173. [PubMed] [Google Scholar]
- 23.Maund E, Craig D, Suekarran S, et al. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess 2012; 16: 1–264. [DOI] [PMC free article] [PubMed] [Google Scholar]