Abstract
Background
The effectiveness of the Latarjet largely depends on accurate graft placement, as well as on proper position and direction of the screws. We present our technique for an arthroscopically-assisted Latarjet comparing radiological results with the open technique.
Methods
We retrospectively reviewed the postoperative computed tomography scans of 38 patients who underwent a Latarjet procedure. For 16 patients, the procedure was performed with the open technique and, for 22 patients, it was performed using an arthroscopically-assisted technique. An independent radiologist evaluated graft and hardware position, as well as graft integration or resorption. Postoperative complications were also documented.
Results
The graft was correctly placed in only 18.8% of cases in the open group and 72.7% of cases in the arthroscopically-assisted group. There were no postoperative complications in the arthroscopically-assisted group, whereas one patient had a recurrence and two required hardware removal in the open group.
Conclusions
The Latarjet procedure is a challenging procedure for which a key point is the correct placement of the coracoid graft onto the glenoid neck and correct position of the screws. The present study substantiates a clear benefit for the use of a guide with an arthroscopically-assisted technique in terms of graft and hardware placement. At short-term follow-up, there appears to be a benefit for graft integration and avoidance of resorption.
Keywords: artroscopically-assisted, glenoid bone loss, glenoid guide, Latarjet, shoulder instability
Introduction
The Latarjet procedure is a reliable and widely accepted technique in the treatment of antero-inferior instability of the shoulder associated with glenoid bone loss, as well as in patients who have a high risk of recurrence. Recently, the Latarjet procedure has also been proposed as a primary intervention after an initial glenohumeral dislocation even if no glenoid bone loss is present.1
Many modifications have been proposed subsequent to the description of the original technique and recently the procedure has been performed both arthroscopically2,3 and with arthroscopical assistance.4
Reported results of the open Latarjet procedure are generally good, with short- and long-term results in terms of restored stability, patient satisfaction and SSV superior than the standard arthroscopic Bankart repair.1,5 According to Shah et al.,1 the rate of recurrent glenohumeral instability after Latarjet procedure is between 3% and 8% and most of the failures related to the procedure are attributed to coracoid graft malposition.6,7 Hovelius et al.8 reported a significantly higher incidence of redislocation in grafts that are placed too medially relative to the glenoid articular surface. Conversely, grafts placed too laterally are associated with a higher incidence of degenerative changes.6,8 Schmid et al.9 showed that the development of osteoarthritis in revision Latarjet procedures was related to malpositioning of the graft. The placement of the screws is also critical: screws that are not directed parallel to the articular surface run the risk of being too prominent laterally, therefore resulting in impingement of the screw heads against the humeral head, leading to premature joint degeneration. Furthermore, screws that exit near the scapular spine may also jeopardize the suprascapular nerve.10
We consider that successful treatment clearly depends on proper patient selection and pre-operative evaluation, although a correct graft positioning and a good fixation technique can avoid many failures.
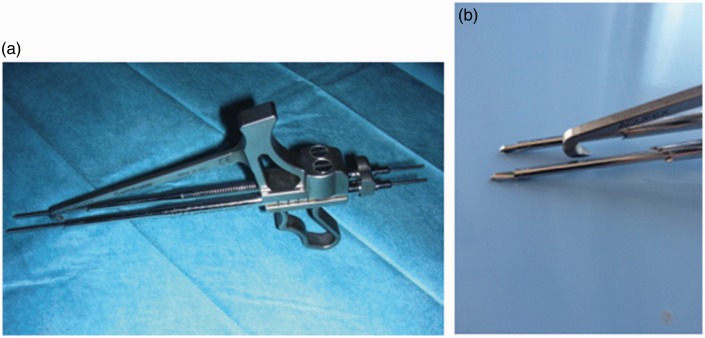
The aim of the present study was to compare the results in terms of graft and hardware position obtained on the one hand with the conventional open technique and, on the other, with an arthroscopically-assisted procedure4 using a new drill guide (Figure 1) employing a posterior approach.
Figure 1.
(a) Glenoid Guide™. (b) Detail.
Materials and methods
The Institutional Review Board waived approval because the present study is both retrospective and observational.
Starting in February 2011, we performed a retrospective study including 38 patients who had undergone the Latarjet procedure and for whom a postoperative computed tomography (CT) scan was available or could be obtained. In all cases, the indication for surgery was recurrent anterior glenohumeral instability, with a glenoid bone defect higher than 15%11 or in case of a failed soft tissue repair.
For 16 patients, the open procedure was performed without the help of arthroscopy and, for 22 patients operated after May 2012, the intervention was performed using an arthroscopically-assisted technique4 with a new drill guide (Glenoid Guide™; Smith and Nephew, London, UK), developed to improve the accuracy and reproducibility of the glenoid and coracoid bony tunnels. The precise drilling of the coracoid process and the glenoid allows optimal placement of the coracoid graft and the hardware for fixing it. There were three (18.8%) women in the open group and three (15.6%) in the arthroscopic-assisted group; mean age was 27.8 years (range 18.3 years to 43.1 years) and 28.5 years (range 15.5 years to 45.2 years) years, respectively. In the open Latarjet group, five (31.3%) procedures were performed for a failed soft tissue repair, whereas, in the arthroscopic group, eight (36.4%) procedures were revisions, the mean glenoid bone loss was 17.2% (range 15% to 27%) and 19.7 (range 15% to 29%), respectively. The average number of dislocation was similar in the two groups [5.7 (range 2 to 30) versus 7.2 (range 3 to 30), respectively]. Mean follow-up time was 9.5 months (range 6 months to 20 months).
Arthroscopically-assisted procedure
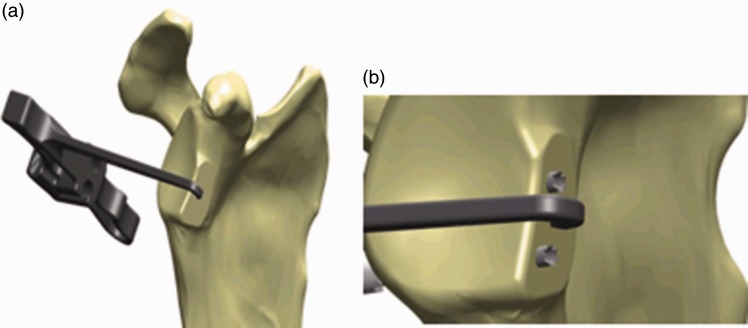
The goal of the arthroscopic time is the introduction and perfect placement from posterior to anterior of two metallic sleeves into the glenoid anterior neck, 1 cm apart, with a medial offset from the glenoid bony rim of 5 mm, therefore allowing an optimal placement of the screws parallel to each other and perpendicular to the glenoid neck4 (Figure 2).
Figure 2.
(a) Positioning of the drill guide centered on the bone defect. (b) Sleeves perpendicular to glenoid neck and parallel to each other.
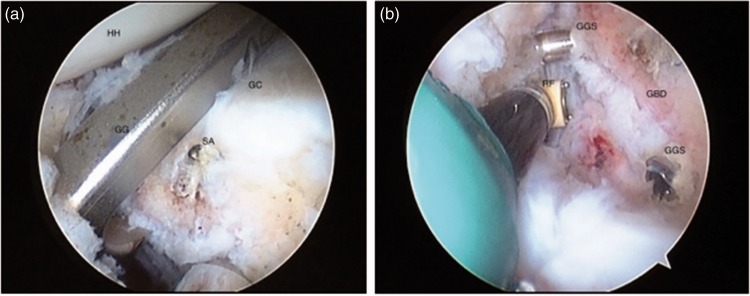
The surgery starts with arthroscopic glenohumeral inspection aiming to evaluate humeral and glenoid bone loss and to assess and treat concomitant articular pathology (if present). A high posterior lateral viewing portal is preferred for initial glenohumeral inspection to allow a subsequent posterior vector guide and double barrel guide sleeve to be inserted posteriorly into the joint. Standard anterior superior and midglenoid portals are made by means of 5.5 mm and 7.0 mm cannulas. The capsule and labrum are detached from the glenoid neck to freshen and flatten its surface using a motorized burr. Using the Glenoid Guide™, two sleeves are placed centered in the middle of the anterior glenoid bone loss (Figure 3), if present, or between the three and five o’clock positions if no bone loss is present. After this step, we stop the arthroscopic time and approach the glenohumeral joint through an open anterior approach.
Figure 3.
(a) Arthroscopic view: glenoid guide positioning (HH, humeral head; GC, glenoid cartilage; GG, glenoid guide; SA, suture anchor). (b) Arthroscopic view: sleeve insertion (GGS, glenoid guide sleeve; GBD, glenoid bone deficit; RF, radio frequency).
We perform the open part of the procedure as described by Young et al.12 using a limited deltopectoral approach incorporating the mid-glenoid portal at the top of the incision. After performing the coracoid osteotomy and preparation, we perform a subscapularis split to expose the glenoid.
A flexible metallic guide wire is then introduced posteriorly into the sleeve and through the coracoid holes to insert two 4.0 mm partially-threaded cannulated screws. After removing the sleeves and using the guidance of the wires that are left in place, we are able to fix the coracoid flush to the glenoid, compressed by two screws perfectly parallel to each other and with both perpendicular to the glenoid neck.
Open procedure
For the cases operated without the help of arthroscopy and without the Glenoid Guide™, we used an open approach as described by Young et al.12 Coracoid and glenoid drilling were performed free hand using only a standard drill guide. The inferior glenoid drill hole is performed only after placement of the superior screw to allow minor corrections of coracoid positioning.
Radiological evaluation
An independent radiologist, who was blinded to the type of procedure, was asked to evaluate coracoid graft and hardware position, as well as graft integration or resorption.
To assess the position of the graft, we applied a method recently proposed by Kraus et al.13
Defining the glenoid height for standardized assessment
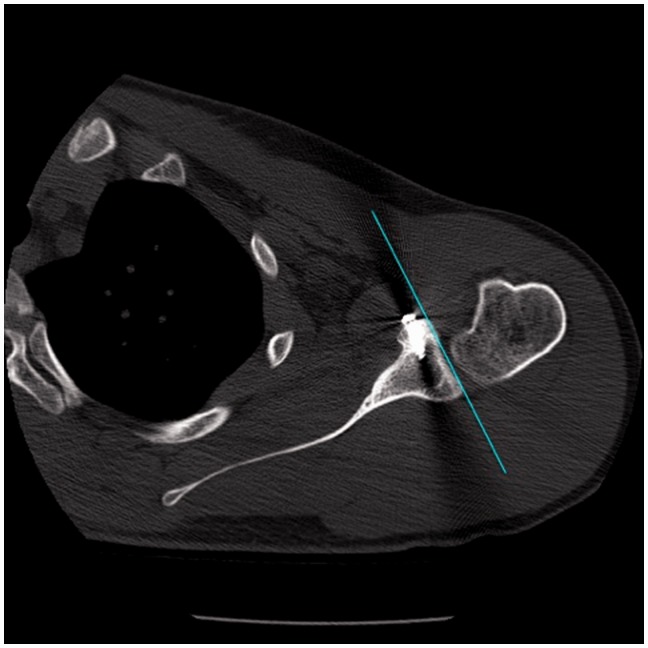
On the ‘en face’ view of the glenoid, a line was drawn connecting the superior tubercle (S) and the inferior tubercle (I). The distance S–I corresponds to the glenoid height; the heights of 25% and 50% of the distance S–I were defined and measurements were then taken in the corresponding axial views at 25% and 50% of the glenoid height (Figure 4).
Figure 4.
Defining glenoid and graft height.
Tangential (line) assessment: axial view
At both 25% and 50% of the glenoid height, a line was drawn alongside the glenoid. The anterior and posterior subchondral rims of the glenoid were used as reference points. In relation to the line drawn between the reference points, the graft was judged to be lateral, correct or medial. Tolerance range <1 mm (Figure 5).
Figure 5.
Defining graft positioning on the axial view.
Transplants were judged to be lateral if they were lateral at either one of the glenoid height levels.
The position of the coracoid graft was also assessed according to its height in relation to the glenoid equator: it was considered to be correct when the superior edge of the coracoid graft was either on the same level as, or just superior to, the glenoid equator (otherwise classified as high) aiming to keep the inferior part of the subscapularis below the centre of rotation during combined abduction and external rotation. We consider that a graft placed in a higher position it is not able to restore the natural glenoid’s pear shape, and hence could lead to recurrence of instability.
In addition, the radiologist evaluated and measured the angle between the two screws (considered parallel with an angle <5°) and the angle between the single screw and the glenoid plane (considered perpendicular with an angle <10°). The orientation of the screws in relation to the bony glenoid was measured in the axial plane, as previously described by Ladermann et al.14 This was performed by determining the plane of the bony glenoid, which lies between the anterior and posterior glenoid margin. The orientation of the screws was then measured with reference to this plane and the distance between the screw heads and the articular surface of the graft was also determined (Figure 6).
Figure 6.
Assessment of screw perpendicularity to the glenoid neck and the distance between the screw heads and the articular surface.
Bony union was determined by the presence of bridging bone between the graft and the scapular neck, while the graft resorption was defined as loss of substance (bone) leading to the reduction of the volume and size of the original graft on CT scans. For the evaluation of coracoid integration or resorption, cases with CT follow-up shorter than 6 months were not considered.
Postoperative complications, redislocation or reintervention were also documented.
Collected data was analyzed using SPSS, version 20 (SPSS Inc., Chicago, IL, USA).
Results
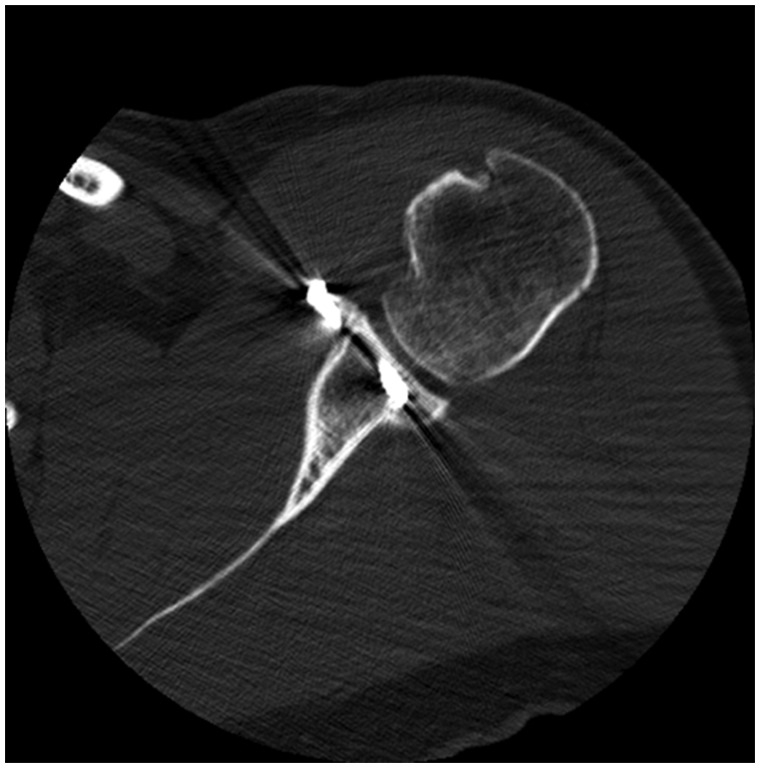
When comparing the results in terms of graft placement for the two techniques (Table 1), graft position was considered as good in 72.7% of the cases in the arthroscopically-assisted technique using the drill guide and only in 18.8% of cases in the freehand open group (p = 0.001, Fisher’s exact test) (Figs 7 and 8).
Table 1.
Graft placement.
| Graft position | Open | Arthroscopically- assisted |
|---|---|---|
| Good | 3/17 (17.6%) | 16/22 (72.7%) |
| Lateral | 1/17 (5.9%) | – |
| Medial | 3/17 (17.6%) | – |
| High | 13/17 (76.5%) | 6/22 (27.3%) |
Figure 7.
Arthroscopically-assisted Latarjet: good graft positioning.
Figure 8.
Arthroscopically-assisted Latarjet: flush graft positioning.
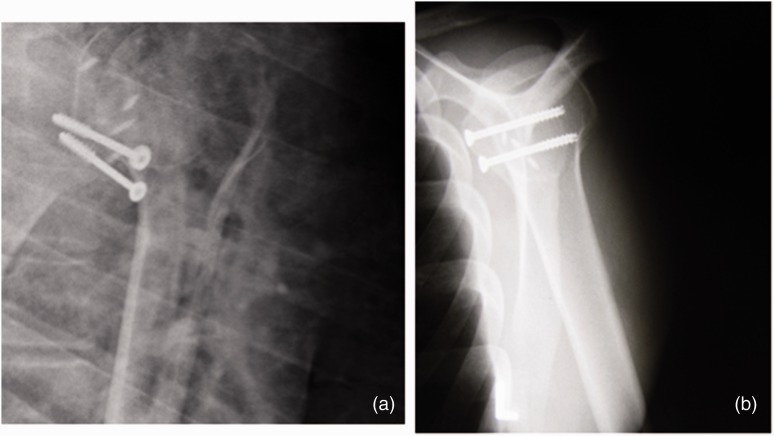
Considering hardware positioning, the use of the Glenoid Guide™ appeared to grant a better outcome in relation to perpendicularity of screws to glenoid neck (p = 0.000, Pearson chi-squared test) and screw head-articular surface distance (p = 0.317, Pearson chi-squared test) (Figure 9 and Table 2). Measurements of articular step-off yielded good results in both groups (p = 0.061, Pearson chi-squared test) (Table 2). Screw parallelism was more accurate in the arthroscopically-assisted group in which 95.5% (21 out of 22) of the screws were considered parallel to each other versus 62.5% (10 out of 16) in the open group (p = 0.010, Pearson chi-squared test) (Figure 10).
Figure 9.
Arthroscopically-assisted Latarjet: screw perpendicular to glenoid neck.
Table 2.
Hardware placement.
| Hardware position | Open | Arthroscopically-assisted |
|---|---|---|
| Mean screw-glenoid angle | 20.4° (range 6° to 45°) 8.3% < 10o | 2.5° (range 2° to 12°) 75.9% < 10° |
| Average articular step-off | 1.6 mm (range 0 mm to 8 mm) 50% < 1 mm | 1.6 mm (range 0 mm to 7 mm) 64.7% < 1 mm |
| Mean screw head-articular surface distance | 2.3 mm (range 1.6 mm to 3.5 mm) | 2.5 mm (range 0 mm to 5 mm) |
Figure 10.
(a) Open Latarjet: screws not parallel to each other. (b) Arthroscopically-assisted Latarjet: screws parallel to each other.
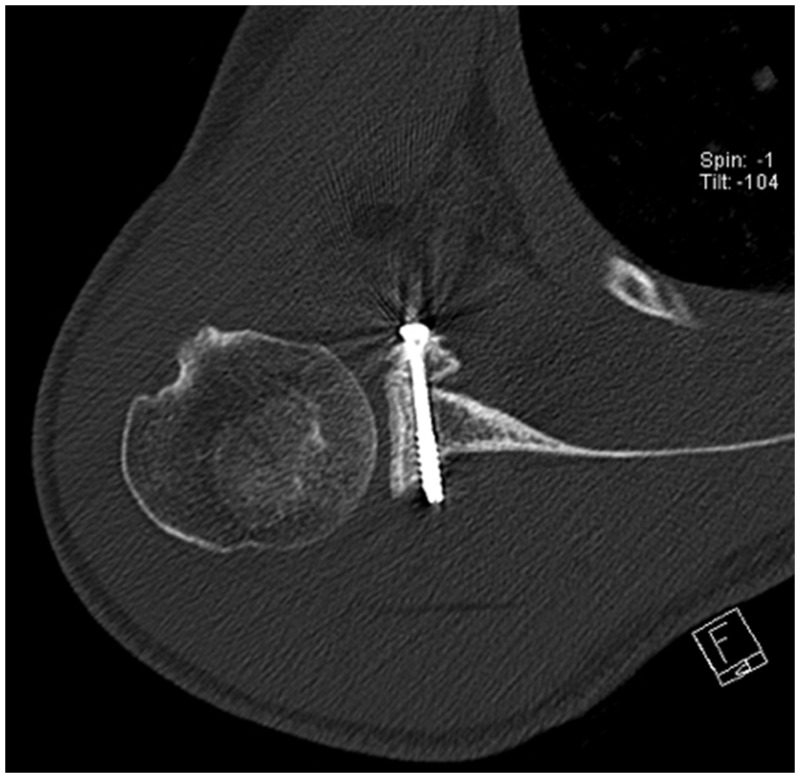
As to graft integration and resorption, there was evidence of coracoid integration in 10 out of 16 cases (62.5%) and of graft resorption in six out of 16 cases (37.5%) in the open Latarjet group. In the arthroscopically-assisted cases, there was evidence of coracoid integration in 18 out of 22 cases (81.8%) and of graft resorption in four out of 22 cases (18.2%) (p = 0.182, Pearson chi-squared test) (Figure 11).
Figure 11.
Arthroscopically-assisted Latarjet: graft integration without resorption.
In the open group, three cases (18.8%) underwent revision surgery (two for hardware removal and one as a result of coracoid displacement and redislocation of the shoulder); in the arthroscopically-assisted group, no cases required revision surgery.
Discussion
The Latarjet procedure is a confirmed method for the treatment of shoulder instability in the presence of bone loss.8,9,12,15–17 It is a challenging procedure for which a key point is the correct placement of the coracoid graft onto the glenoid neck.18–20 As noted in several studies, the main complications associated with the Latarjet procedure are a result of the imprecise positioning of the coracoid graft.6,8,17 However, accurate placement of the graft can be difficult, especially in young muscular athletes, where the exposure can be limited. If the glenoid is not well visualized, the ability to place the coracoid flush with the glenoid face is significantly compromised; for example, when drilling on the glenoid side. The benefit of the presented technique is that a single drill guide allows accurate placement of both the coracoid and glenoid screw holes, yielding reproducibly accurate positioning and optimal compression of the graft onto the glenoid neck as a result of the perfect position of the screws: perpendicular to the graft and the glenoid neck and parallel to each other. In addition, the ability to drill the glenoid holes practically parallel to the glenoid surface offers the safer positioning of the screws in relation to the suprascapular nerve as it runs distally through the spinoglenoid notch.
The present study substantiates a clear benefit of using the Glenoid Guide™ with an arthroscopically-assisted technique in terms of graft placement: when comparing postoperative CT scans, the interventions performed using the new drill guide yield a good coracoid placement in 72.7% of cases, versus only 18.8% of good positioning with the open procedure. The most common positioning mistake with the open procedure was a high placement of the graft (81.3%), which was reduced to 27.3% with the use of the drill guide. In one of the open procedure cases, the graft was too lateral, requiring revision surgery. There were no cases in the arthroscopic-assisted group with a laterally positioned graft.
In a recent anatomic study, Ladermann et al.14 demonstrated that the safe zone for placement of screws to avoid iatrogenic injury was within 10° relative to the face of the glenoid. In the present study, with the use of the drill guide, the mean angle of the screws in the axial plane was 3.1° (range 2° to 12°) and 77.3% were within the range 0° to 10°. We did not find any major difference in the two groups in terms of screw head–articular surface distance. Mean articular step-off and screw head-articular surface distances results were acceptable in both groups. Interestingly, quite a wide range of values for articular step-off and screw head articular distance was found even in the arthroscopically-assisted group (Table 2); this could be explained by the fact that we are missing a specific coracoid preparation tool and are therefore imprecise when drilling holes in the coracoid. We consider that a coracoid preparation tool could be useful for lowering this variability and we are currently developing one.
At the Nice Shoulder Course 2016, Neyton et al.21 presented the results of a study comparing 208 Latarjet procedures performed using three different techniques (open, arthroscopic with screw fixation and arthroscopic with Endobutton fixation positioned with an arthroscopic glenoid guide). They reported excellent radiological results with all the techniques, although the arthro-screw group was less reproducible on graft positioning on the axial plane compared to the open group and the arthro-buttons group. Both arthroscopic techniques were less reproducible than the open technique with respect to sagittal plane graft positioning. A positive effect of using a glenoid guide on coracoid positioning has also been reported by Klatte et al.22 in a cadaveric study.
With the arthroscopically-assisted procedure, we also had an improved outcome regarding coracoid integration (81.8% versus 62.5%) and less graft resorption (18.2% versus 37.5%). Better coracoid integration results could be related to a more favourable screw positioning, leading to an improved graft-glenoid compression and reduced mechanical stress on the screws and the graft. However, a longer follow-up is necessary to confirm these results.
No complications or reintervention were documented in the arthroscopically-assisted group, whereas, in the open group, 18.8% (three cases) required reintervention (arthroscopy and/or hardware removal).
It was beyond the aim of the present study to draw a correlation between the radiological and clinical outcomes, although we are continously collecting our data to investigate this.
There are of course some limitations to the present study; first of all, there is the short follow-up time, especially in the arthroscopically-assisted group (average of 12 months, range 9 months to 24 months). A longer follow-up is necessary to confirm these results. A small sample size is a further important limiting factor and we are continuing to collect our cases aiming to corroborate our findings.
Conclusions
The use the Glenoid Guide™ for an arthroscopically-assisted Latarjet procedure permits an accurate and reproducible positioning of the coracoid graft and reduces complications associated with hardware malpositioning.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The paper has not been presented at any society or meeting.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
Institutional Review Board waived approval because the resported work is a retrospective observational study.
References
- 1.Shah AA, Butler RB, Romanowski J, et al. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 2012; 94: 495–501. [DOI] [PubMed] [Google Scholar]
- 2.Lafosse L, Lejeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 2007; 23: 1242.e1–e5. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Bicknell RT, El Fegoun AB, et al. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficient capsule: the ‘belt-and-suspenders’ operative technique and preliminary results. Arthroscopy 2007; 23: 593–601. [DOI] [PubMed] [Google Scholar]
- 4.Taverna E, Ufenast H, Broffoni L, et al. Arthroscopically assisted Latarjet procedure: a new surgical approach for accurate coracoid graft placement and compression. Int J Shoulder Surg 2013; 7: 120–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimmermann SM, Scheyerer MJ, Farshad M, et al. Long-term restoration of anterior shoulder stability: a retrospective analysis of arthroscopic bankart repair versus open Latarjet procedure. J Bone Joint Surg Am 2016; 98: 1954–1961. [DOI] [PubMed] [Google Scholar]
- 6.Hovelius L, Sandstrom B, Saebo M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study II – the evolution of dislocation arthropathy. J Shoulder Elbow Surg 2006; 15: 279–289. [DOI] [PubMed] [Google Scholar]
- 7.Hovelius L, Sandström B, Olofsson A, et al. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg 2012; 21: 647–660. [DOI] [PubMed] [Google Scholar]
- 8.Hovelius L, Sandstrom B, Sundgren K, et al. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I – clinical results. J Shoulder Elbow Surg 2004; 13: 509–516. [DOI] [PubMed] [Google Scholar]
- 9.Schmid S, Farshad M, Catanzaro S, et al. The Latarjet procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair – a retrospective case series of 49 consecutive patients. J Bone Joint Surg Am 2012; 94: e75.1–e75.7. [DOI] [PubMed] [Google Scholar]
- 10.Maquieira GJ, Gerber C, Schneeberger AG. Suprascapular nerve palsy after the Latarjet procedure. J Shoulder Elbow Surg 2007; 16: e13–e15. [DOI] [PubMed] [Google Scholar]
- 11.Baudi P, Campochiaro G, Rebuzzi M, et al. Assessment of bone defects in anterior shoulder instability. Joints 2013; 1: 40–48. [PMC free article] [PubMed] [Google Scholar]
- 12.Young AA, Maia R, Berhouet J, et al. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg 2011; 20 (Suppl 2): S61–S69. [DOI] [PubMed] [Google Scholar]
- 13.Kraus TM, Graveleau N, Bohu Y, et al. Coracoid graft positioning in the Latarjet procedure. Knee Surg Sports Traumatol Arthrosc 2016; 24: 496–501. [DOI] [PubMed] [Google Scholar]
- 14.Ladermann A, Denard PJ, Burkhart SS. Injury of the suprascapular nerve during latarjet procedure: an anatomic study. Arthroscopy 2012; 28: 316–321. [DOI] [PubMed] [Google Scholar]
- 15.Edwards TB, Walch G. The Latarjet procedure for recurrent anterior shoulder instability: rationale and technique. Oper Tech Sports Med 2002; 10: 25–32. [Google Scholar]
- 16.Levine WN, Arroyo JS, Pollock RG, et al. Open revision stabilization surgery for recurrent anterior glenohumeral instability. Am J Sports Med 2000; 28: 156–160. [DOI] [PubMed] [Google Scholar]
- 17.Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 1998; 80: 841–852. [DOI] [PubMed] [Google Scholar]
- 18.Meehan RE, Petersen SA. Results and factors affecting outcome of revision surgery for shoulder instability. J Shoulder Elbow Surg 2005; 14: 31–37. [DOI] [PubMed] [Google Scholar]
- 19.Meyer DC1, Moor BK, Gerber C, et al. Accurate coracoid graft placement through use of a drill guide for the Latarjet procedure. J Shoulder Elbow Surg 2013; 22: 701–708. [DOI] [PubMed] [Google Scholar]
- 20.Walch G, Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg 2000; 1: 256–261. [Google Scholar]
- 21.Neyton L, Barth J, Boileau P, et al. Latarjet procedure: 2D CT analysis of bone block positioning and comparison between two arthroscopic techniques and one open technique. Shoulder Concepts. Arthroscopy, Artroplasty & Fractures. Nice Shoulder Course 2016. Montpellier: Sauramps Medical.
- 22.Klatte TO, Hartel MJ, Weiser L, et al. Accuracy of Latarjet graft and screw position after using novel drill guide. Eur J Trauma Emerg Surg 2016. Epub ahead of print 4 July 2016. DOI: 10.1007/s00068-016-0703-4. [DOI] [PubMed]