Abstract
Introduction: Rapid diagnostic testing (RDT) for HIV has a quick turn-around time, which increases the proportion of people testing who receive their result. HIV RDT in Thailand has traditionally been performed only by medical technologists (MTs), which is a barrier to its being scaled up. We evaluated the performance of HIV RDT conducted by trained lay providers who were members of, or worked closely with, a group of men who have sex with men (MSM) and with transgender women (TG) communities, and compared it to tests conducted by MTs.
Methods: Lay providers received a 3-day intensive training course on how to perform a finger-prick blood collection and an HIV RDT as part of the Key Population-led Health Services (KPLHS) programme among MSM and TG. All the samples were tested by lay providers using Alere Determine HIV 1/2. HIV-reactive samples were confirmed by DoubleCheckGold Ultra HIV 1&2 and SD Bioline HIV 1/2. All HIV-positive and 10% of HIV-negative samples were re-tested by MTs using Serodia HIV 1/2.
Results: Of 1680 finger-prick blood samples collected and tested using HIV RDT by lay providers in six drop-in centres in Bangkok, Chiang Mai, Chonburi and Songkhla, 252 (15%) were HIV-positive. MTs re-tested these HIV-positive samples and 143 randomly selected HIV-negative samples with 100% concordant test results.
Conclusion: Lay providers in Thailand can be trained and empowered to perform HIV RDT as they were found to achieve comparable results in sample testing with MTs. Based on the task-shifting concept, this rapid HIV testing performed by lay providers as part of the KPLHS programme has great potential to enhance HIV prevention and treatment programmes among key at-risk populations.
Keywords: Performance, HIV, rapid diagnostic test (RDT), lay providers, key population-led
Introduction
An HIV test-and-treat strategy is being implemented in many countries around the world, including Thailand, to improve the health of people living with HIV (PLWH) and to limit onward transmission [1]. Rapid diagnostic testing (RDT) for HIV offers advantages over laboratory-based serological testing, which include lower cost, an easier testing procedure, speed and ease of result interpretation, and transportability (i.e. testing can be performed in a mobile setting without electricity). The quick turn-around time of 20–60 minutes obviates the need for a second visit to get test results. Its simplicity offers the opportunity to engage non-laboratory professionals (i.e. lay providers) as test performers [2].
There were 445,504 PLWH in Thailand in 2014, and approximately 7700 new infections [3]. There are around 550,000 men who have sex with men (MSM) in the country and HIV prevalence among them is not decreasing (8.0% in 2010, 7.1% in 2012, and 9.2% in 2014 [3]). Currently, the estimated prevalence of HIV infection among MSM in Bangkok is about 24%, yet only 29% of MSM had tested for HIV in the previous year [4]. There is no evidence that the epidemic among MSM in Bangkok is receding [3]. As for transgender women (TG), HIV prevalence was 11.8% with only 34% having access to HIV testing services [3].
In October 2014, Thailand became the first country in Asia to implement a policy of offering free immediate antiretroviral treatment (ART) to all HIV-positive Thai citizens [4]. All Thai nationals are also eligible for free HIV testing twice a year. To increase testing among MSM and TG, actions such as public campaigns have been launched to improve HIV awareness and to promote HIV prevention activities among MSM and TG [3]. HIV testing in Thailand, however, is currently offered mainly in hospitals and clinics and can only be performed by MTs according to the Thai Medical Technologist Council policy. This requirement may greatly hinder the scaling up of HIV testing due to the limited number of MTs available to provide outreach HIV testing services and meet the demand of key populations, particularly young MSM and TG. Typical working hours for MTs have also been shown to conflict with MSM and TG lifestyles. Additionally, these key populations may be reluctant to visit clinics or hospitals for HIV testing because of concerns about stigma and discrimination [4,5].
In order to address the challenge of scaling up HIV testing for MSM and TG in Thailand, the Department of Disease Control, the Ministry of Public Health (MOPH), and the Thai Red Cross AIDS Research Centre (TRCARC), with support from the US Agency for International Development/Regional Development Mission for Asia (USAID/RDMA), established the Key Population-led Health Services (KPLHS) programme in 2015, based on the WHO Task Shifting recommendations and guidelines and WHO Guidelines for HIV Testing Services [6,7]. KPLHS is defined as health services that are well tailored and responsive to the specific needs of key populations and adhere to the rigorous principles of availability, accessibility and acceptability with non-discrimination and quality standards. The health service provision, including HIV RDT, can be led and provided by the empowered and well-trained community members of key populations as well as non-key populations. Six community-based organisations (CBOs), serving mainly MSM, TG and male sex workers, took part in this KPLHS programme in Bangkok, Chiang Mai, Chonburi and Songkhla. The primary objective of this report was to evaluate the performance of HIV RDT conducted by trained lay providers in this KPLHS programme, as compared to MTs.
Methods
This analysis was performed at six CBOs as part of an ongoing study that aims to evaluate the feasibility of the KPLHS strategy targeting MSM and TG using: (1) a key population-led service delivery model; and (2) enhanced key population-led outreach interventions to increase the uptake of services. These CBOs are in Bangkok (central Thailand – Service Workers IN Group or SWING, and Rainbow Sky Association of Thailand or RSAT), Chonburi (central Thailand – SWING and Sisters), Chiang Mai (northern Thailand – Caremat), and Songkhla (southern Thailand – RSAT). All relevant ethics committees approved these studies and each participant provided informed consent.
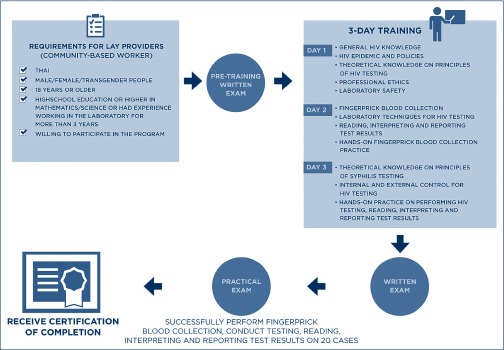
We asked each CBO to select their staff based on expressed interest from individuals to perform HIV RDT and the CBO director's endorsement of that candidate to perform the task after completion of the lay provider training. Lay providers were required to be of Thai origin, aged 18 years or older, to have graduated from high school in mathematics/science or to have had experience working in a laboratory for more than 3 years, and to be willing to take part in the programme. These lay providers may or may not have belonged to the MSM or TG populations. They also underwent an intensive 3-day training programme by a team of MTs from the TRCARC and Thailand MOPH–US CDC Collaboration. The training included sessions on the HIV epidemic and policies, professional ethics, laboratory safety, theoretical knowledge, laboratory techniques to perform finger-prick blood collection and HIV RDT, and procedures required for quality assessment of HIV RDT. Those who completed the training and successfully performed and interpreted 20 blinded samples using HIV RDT were allowed to perform this testing method in drop-in centres (Figure 1).
Figure 1.
Requirements, training modules and certification processes for lay providers to perform and provide HIV rapid diagnostic test in the Key Population-led Health Services programme
The HIV RDT algorithm is consistent with the Thai National Guidelines. Tests used include the following: Alere Determine HIV 1/2, first-line blood-based rapid test (Alere Medical Co, Ltd, Matsuhidal, Matsudo-shi, Chiba, Japan), followed by second- and third-line testing with DoubleCheckGold Ultra HIV1&2 (Orgenics, Yavne, Israel) and SD Bioline HIV 1/2 (Standard Diagnostics, Inc, Hagal-dong Giheung-gu, Yongin-si, Korea) [8,9]. These tests were selected based on their high sensitivity and specificity profiles. Samples were sent using EDTA capillary tubes to TRCARC for quality assurance testing by MTs using the Serodia HIV 1/2 assay (Fujirebio Inc, Tokyo, Japan). In addition, the lay providers who performed HIV RDT in their drop-in centres received quality assessment refresher training from MTs at TRCARC and local public health authorities every 3 months, as per the Thai Medical Technology Council's guidelines [10].
According to the standard operating procedures for sample storage and transportation, all HIV RDT samples were stored at 2–8° Celsius for up to 4 weeks at the CBOs prior to being transported under controlled temperature to TRCARC. All samples were sent to TRCARC with their results. At TRCARC, samples were re-sequenced and separated into HIV-positive and HIV-negative samples. All HIV-positive samples and one random tube out of every 10 HIV-negative samples were re-tested by MTs.
Results
From January 2015 to April 2016, 38 people were recruited in this lay provider training programme and 35 individuals successfully completed the 3-day training course. Among these 35 individuals, 14 identified as MSM, six as TG, two as heterosexual men, 12 as heterosexual women, and one as a cis-gender woman who has sex with women. They all received prior training in social support/case management as part of their organisations' training for current roles and responsibilities. Their mean age was 36 years (range 24–47) and average income was US$512 dollars per month (1.2 times the average household income in Thailand as of July 2016) [11].
The basic demographic characteristics of clients who accessed the HIV testing service at our participating CBOs were previously reported [12]. In brief, 71% were MSM and 29% were transgender women with a median (interquartile range) age of 24 (21–30) years. Only 27% had a bachelor degree or higher education, and 59% had a monthly income lower than US$285. Around half (48%) were first-time HIV testers. In the previous 6 months, 58% reported having multiple sex partners, 78% did not use condoms consistently, 12% had group sex and 7% used amphetamine-type stimulants.
During this period, these lay providers collected 1680 finger-prick blood samples and performed HIV RDT on these samples, 252 (15%) of which were reported to be HIV-positive and 1428 HIV-negative. There were no indeterminate test results. All of the 252 HIV-positive samples re-tested by MTs at TRCARC also showed positive results. Similarly, all of the 143 HIV-negative samples randomly selected showed negative results when re-tested by MTs.
Discussion
As part of the KPLHS programme among Thai MSM and TG, we have demonstrated for the first time in Thailand that well-trained lay providers can perform HIV RDT and provide HIV RDT results 100% similar to those performed by MTs. The quality of HIV testing suggests that these lay providers, who were members of, or worked closely with, MSM and TG communities, are capable of providing HIV RDT at drop-in centres throughout Thailand. In 2016, 42% of the overall HIV testing among MSM and TG in Thailand came from these CBOs, and resulted in 35% of the overall new HIV diagnosed cases among MSM and TG that year (Routine Integrated HIV Information System, National AIDS Management Center, MOPH 2016) [13].
In a randomised trial of universal HIV screening by lay providers and healthcare professionals in a Boston emergency room, the HIV RDT uptake was 57% (1382/2446) in the lay provider arm as compared to 27% in the healthcare provider arm (643/2409, P<0.001) [14]. In rural Malawi where lay providers were trained to perform RDT, the uptake of HIV testing with trained lay providers increased from 1300 tests per month in 2003 to 6500 in 2009, with an excellent quality assurance profile [15]. A study in Cambodia using midwives without laboratory experience as lay providers also reported high concordance rates of RDT results by lay providers and MTs [16] similar to that described in our study.
Our study is unique in that we have implemented HIV RDT by lay providers in drop-in centres for ‘key populations’ who are MSM, TG and male sex workers. Others have previously demonstrated the benefits of engaging lay providers in HIV testing scale-up among predominantly heterosexual populations in North America, Europe, sub-Saharan Africa, and Asia [17]. In 2015, the HIV RDT policies in 48 countries were assessed and 40% of these allowed lay providers to perform this type of testing, with over 60% of 25 African countries. However, a number of countries, such as Thailand, still limit HIV RDT to trained laboratory professionals.
The challenge for Thailand is to increase access to, and uptake of, HIV RDT among infected MSM and TG who are undiagnosed. In addition, we are also faced with the challenge to increase access to, and use of, HIV prevention tools among those not yet infected, but who are at high risk for acquiring HIV. The UNAIDS 90–90–90 goal aims for 90% of all people with HIV to be diagnosed, 90% of people with HIV diagnosed to receive ART, and 90% of those taking ART to have a suppressed viral load by 2020 [3,18]. Thailand will not be able to achieve this goal unless HIV testing increases among MSM and TG. We strongly believe that a new policy allowing and promoting trained lay providers to perform HIV RDT in community-based settings would be an important step in Thailand's effort to end the HIV epidemic.
Our model of empowering community members to provide HIV testing to clients from similar demographic and HIV-risk backgrounds offers a unique opportunity to provide support and testing for the clients, and also reinforces self-worth and sense of accomplishment for the testers [19]. As our study here demonstrates that lay providers are capable of performing accurate HIV RDT for MSM and TG communities, on a par with the quality of testing performed by MTs, it lays the foundation for Thailand to further enable policy and legal environment to allow lay providers to perform this task in a sustainable way as part of its national health care system.
Acknowledgements
We are grateful for the work performed by the lay providers and the staff at the six participating centres. SW was supported by co-operative agreements (W81XWH-07-2-0067, W81XWH-11-2-0174) between the Henry M Jackson Foundation for the Advancement of Military Medicine and the US Department of the Army.
We also would like to thank Dr Michael Martin for his valuable input to this short report.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Each author has made an equal contribution to the analysis and interpretation of data. In addition, all authors have been equally been involved in drafting this manuscript and revising important intellectual content. Each author has given final approval of the version to be published.
Disclaimer
The views expressed are those of the authors and should not be construed to represent the positions of the US Army or the Department of Defense or Columbia University.
References
- 1. Cohen MS, Chen YQ, McCauley M et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365: 493– 505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arora DR, Maheshwari M, Arora B. Rapid point-of-care testing for detection of HIV and clinical monitoring. ISRN AIDS 2013; 287269. [DOI] [PMC free article] [PubMed]
- 3. National AIDS Management Center. Department of Disease Control. Ministry of Health Thailand AIDS Response Progress Report 2015. Reporting Period: Fiscal Year of 2014 ; 2015. Available at: www.unaids.org/sites/default/files/country/documents/THA_narrative_report_2015.pdf ( accessed December 2017).
- 4. Nyberg R, Tanchaisawat M. Dressed to Test: empowered communities take HIV services to the streets. Online edition. Frontlines April, 2016. Available at: www.usaid.gov/news-information/frontlines/march-april-2016/dressed-test-empowered-communities-take-hiv ( accessed December 2017).
- 5. Logie CH, Newman PA, Weaver J et al. HIV-related stigma and HIV prevention uptake among young men who have sex with men and transgender women in Thailand. AIDS Patient Care STDS 2016; 30: 92– 100. [DOI] [PubMed] [Google Scholar]
- 6. Baggaley R. Update on the new WHO guidelines for HIV testing services. 2015. Available at: aidsfree.usaid.gov/sites/default/files/hts_webinar_baggaley_0.pdf ( accessed December 2017).
- 7. World Health Organization Task shifting: Global recommendations and guidelines; 2008. Available at: www.who.int/healthsystems/TTR-TaskShifting.pdf?ua=1 ( accessed December 2017).
- 8. Hongjing Y, Zhang R, Wei C et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect 2014; 90: 388– 393. [DOI] [PubMed] [Google Scholar]
- 9. Alere Alere Determine HIV-1/2. Ref. 7D2343; July 2015. Available at: www.alere.com/en/home/product-details/determine-hiv-1-2.html ( accessed December 2017).
- 10. Wattanasri N, Manoroma W, Viriyayudhagorn S. Laboratory accreditation in Thailand: a systematic approach. Am J Clin Path 2010; 134: 534– 540. [DOI] [PubMed] [Google Scholar]
- 11. Trading Economics Thailand average monthly wages 1999–2016. Available at: www.tradingeconomics.com/thailand/wages ( accessed December 2017).
- 12. Vannakit R, Jantarapakde J, Pengnonyang S et al. High linkage to ART and HIV RNA suppression among HIV-positive MSM and TG, along with PrEP uptake among HIV-negative MSM and TG, through community-led health service model in Thailand. IAS Conference. July 2017. Paris, France. Abstract: TUPED1313.
- 13. National AIDS Committee Thailand National Strategic Information and Monitoring and Evaluation Plan for HIV/AIDS Thailand, 2012 to 2016; updated 2013. Available at: namc.ddc.moph.go.th/namc2016/document/documentry/3-Strategy/National_SI_M&E_Plan2012-2016/Final_Thailand_National_SI_M&E_Plan%2021July2013.pdf ( accessed December 2017).
- 14. Walensky RP, Reichmann WM, Arbelaez C et al. Counselor- versus provider-based HIV screening in the emergency department: Results from the universal screening for HIV Infection in the Emergency Room (USHER) randomized controlled trial. Ann Emerg Med 2011; 58( Suppl 1): S126– S132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Molesworth AM, Ndhlovu R, Banda E et al. High accuracy of home-based community rapid HIV testing in rural Malawi. J Acquir Immune Defic Syndr 2010; 55: 625– 630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bemelmans M, Van Den Akker T, Ford N et al. Providing universal access to antiretroviral therapy in Thyolo, Malawi through task shifting and decentralization of HIV/AIDS care. Trop Med Int Health 2010; 15: 1413– 1420. [DOI] [PubMed] [Google Scholar]
- 17. Kennedy C, Fonner V. Annex 1: Should trained lay providers perform HIV testing and counseling services using HIV rapid diagnostic tests?: a systematic review. World Health Organization 2015. Available at: apps.who.int/iris/bitstream/10665/180203/1/WHO_HIV_2015.18_eng.pdf ( accessed December 2017).
- 18. UNAIDS 90-90-90 Ambitious treatment targets: writing the final chapter of the AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS; 2014. Available at: www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf ( accessed December 2017).
- 19. Kanal K, Chou TL, Sovann L, et al. Evaluation of the proficiency of trained non-laboratory health staffs and laboratory technicians using a rapid and simple HIV antibody test. AIDS Res Ther 2005; 2: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]