Abstract
[Purpose] To present the case of the non-surgical restoration of cervical lordosis in a patient suffering from chronic whiplash syndrome including chronic neck pain and daily headaches resulting from previous whiplash. [Subject and Methods] A 31 year old female presented with a chief complaint of chronic neck pain and headaches for 12 years, correlating temporally with a sustained whiplash. These symptoms were not significantly relieved by previous chiropractic spinal manipulative therapy. The patient had cervical hypolordosis and was treated with Chiropractic BioPhysics® protocol including extension exercises, manual adjustments and cervical extension traction designed to increase the cervical lordosis. [Results] The patient received 30 treatments over approximately 5-months. Upon re-assessment, there was a significant increase in global C2–C7 lordosis, corresponding with the reduction in neck pain and headaches. [Conclusion] This case adds to the accumulating evidence that restoring lordosis may be key in treating chronic whiplash syndrome. We suggest that patients presenting with neck pain and/or headaches with cervical hypolordosis be treated with a program of care that involves cervical extension traction methods to restore the normal cervical lordosis.
Key words: Cervical hypolordosis, Whiplash associated disorder, Extension traction
INTRODUCTION
Neck pain and headaches are a common patient complaint to the manual therapist1). It is now well recognized that the alignment of the cervical spine plays a key role in the production of patient symptoms of craniocervical origin2,3,4,5,6).
For patients having craniocervical symptoms, there is a growing evidence-base demonstrating that restoration of cervical lordosis may aid in the resolution of these ailments7,8,9,10,11,12,13). Methods involving cervical extension traction as part of multimodal rehabilitation programs have been shown to be superior to ‘standard’ physiotherapy treatments for long-term outcomes as classic physiotherapy may temporarily relieve a patients symptoms initially, but failing in the long-term as it does not restore/improve normal lordosis10,11,12,13)—a likely origin to chronic craniocervical symptoms.
Chronic or late whiplash syndrome (CWS) is the development and persistence of a collection of symptoms and disability for more than 6 months following a motor vehicle collision14). The symptoms are collectively known as whiplash-associated disorders (WAD)15) and include among others, neck pain, headaches, stiffness, and reduced mobility of the neck. More than a third of motor vehicle collision related whiplash patients develop CWS16).
The treatment of CWS is controversial17) and there is no consensus for treatment18). Of studies that have attempted to identify factors associated with poor prognosis in CWS, several have identified altered cervical spine alignment19,20,21). It would seem logical to treat CWS with a treatment proven to improve cervical lordosis.
We present a case of the restoration normal cervical lordosis in a patient having hypolordosis and suffering from 12 years of chronic neck pain and headaches following a whiplash event.
SUBJECT AND METHODS
A 31 year old female presented with a chief complaint of neck pain and headaches for 12 years. The patient worked as a coal mine heavy equipment operator and had a history of whiplash sustained at the coal mine 12 years prior. The patient was also bucked off a horse 8-months prior to presentation and suffered a concussion. She attempted previous chiropractic treatment with no relief.
Upon assessment, the patient rated her neck pain and headaches as a 3/10 (0=no pain; 10=worst pain ever) as well as being constant; and this was rated a 6–7/10 while wearing a hardhat at work.
The patient demonstrated an overall loss of cervical range of motion (ROM), numbness in her hands bilaterally, cold hands and feet, tinnitus, sinusitis, upper back pain, and right knee pain. Strength testing revealed both cervical flexion and right hip flexion to be a 4/5. Orthopedic testing revealed a positive maximum foraminal compression bilaterally. Visual posture assessment22) demonstrated a flexed head position (+RxH), a right posteriorly rotated thorax (−RyT), a right laterally translated thorax (−TxT), and an extended thorax (−RxT).
Radiographic assessment of the cervical spine was performed and analyzed using the Postureray system (Trinity, FL, USA). This method uses the Harrison posterior tangent method to measure sagittal cervical alignment23). This method measures cervical alignment from lines drawn over the posterior body margins of the vertebrae, and is repeatable and reliable23, 24), as is posture assessment25). The patient demonstrated a hypolordosis of the global cervical spine and had an absolute rotation angle (ARA) from C2–C7 of −18.8° (vs. −31–42° normal5, 6); negative indicates extension) (Fig. 1).
Fig. 1.

Neutral lateral cervical radiographs.
Left: Initial (4/4/17) showing cervical absolute rotation angle hypolordosis of −18.8° between C2–C7. Right: Follow-up (8/28/17) showing restoration of normal lordosis (−32.1°) after 30 treatment sessions. Green line represents ideal 42° curve; Red line highlights patient position.
The patient was treated using CBP methods26,27,28) which is a full-spine posture and spine correcting program first developed by Don Harrison. A treatment frequency of three times a week was recommended for 10 weeks. Each visit consisted of neck extension exercises, cervical extension traction and manual spinal therapy.
Pope 2-way cervical extension traction9, 10, 13) was used for a maximum of 20 minutes per session; the patient progressed to the weight of 30 pounds on the front pull (Fig. 2).
Fig. 2.

Pope 2-way cervical extension traction.
While performing neck extension exercises using a pro-lordotic (Circular Traction Supply Inc., Huntington Beech, CA, USA), the patient stood on a PowerPlate (Northbrook, IL, USA) and wore a thoracic-flex traction body weight (Circular Traction Supply Inc., Huntington Beach, CA, USA) to pre-stress the upper thoracic spine in order to get a better correction to the cervical spine (Fig. 3). Mirror image postural drop-table and manual adjustments were also performed.
Fig. 3.
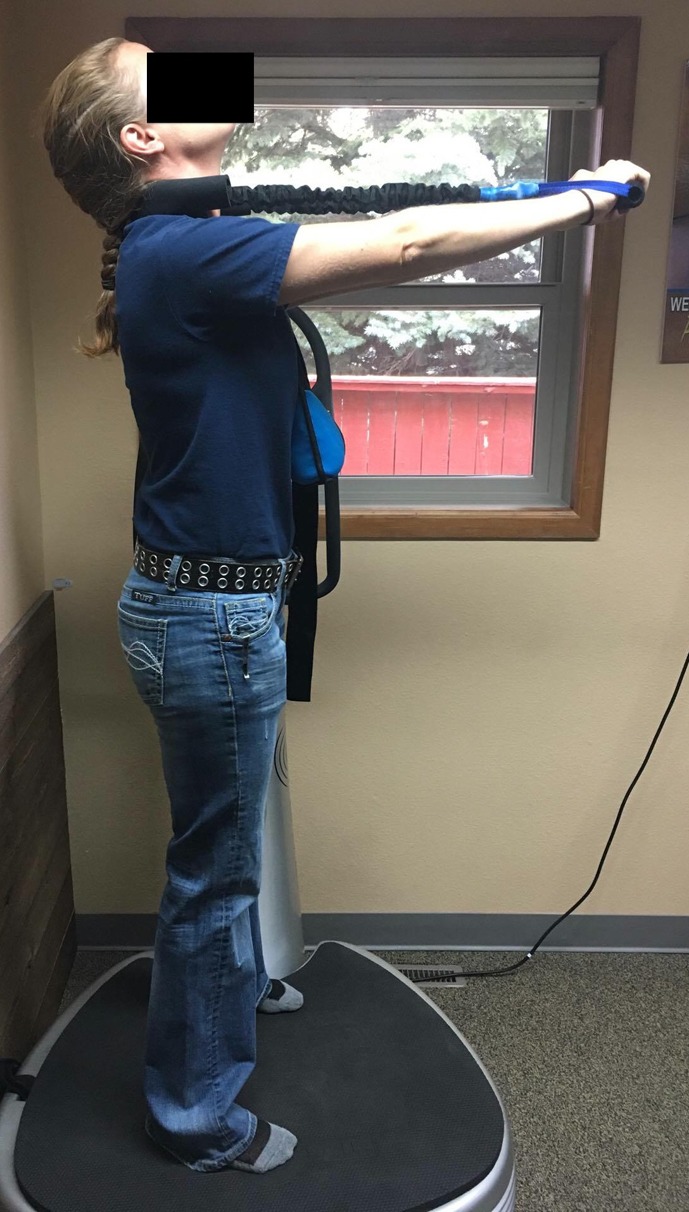
Cervical mirror image extension exercises.
The patient was also instructed in daily home care consisting of supine cervical traction on a large cervical Denneroll (Wheeler Heights, Australia), neck extension exercises with the Pro-lordotic, and use of an icepack for the neck as needed. The patient gave verbal and written consent to the publication of these results including all radiographs and pictures.
RESULTS
Due to rotating coal mine shifts, the patient was treated as frequently as her work schedule would allow; the follow-up radiograph was taken after 30 treatments, almost 5-months after beginning care (8/28/17).
The patient had a full restoration of the cervical curve (C2–C7 ARA= −32.1°) and a dramatic improvement in her headaches and neck pains (0/10 average; 2/10 at worst). The wearing of her hardhat no longer aggravated her pains and whenever she did happen to suffer from pain, the performance of the home exercise routine would alleviate it immediately. Cervical ROM, strength testing, and orthopedic tests were normal. She reported all previous health complaints to have been improved by 90–100%.
DISCUSSION
This case demonstrates the restoration of normal cervical lordosis and the corresponding alleviation of chronic neck pain and headaches associated with a previous whiplash incident suffered 12 years previous.
There have been two previous case reports of CBP treatment featuring cervical extension traction to restore more ideal alignment in WAD patients. Fortner et al.29) presented the case of a 29 year old female achieving a 13° improvement in lordosis after 36 treatments over 15 weeks with dramatic improvements in chronic neck pain and headaches and other symptoms that was maintained at a 13 month follow-up. She had suffered a whiplash 13 years prior. Ferrantelli et al.30) presented the case of the complete symptomatic resolution of WAD symptoms in a 40 year old male who had a 25° improvement in lordosis after 64 treatments over 18 weeks. This patient had suffered a whiplash 8 months previous and also had MRI-confirmed cervical and thoracic disc herniations, a C5 chip fracture and was given a whole body permanent impairment rating of 33% by an orthopedic surgeon.
The present case demonstrated a 13° improvement in cervical lordosis over almost 5 months, with significant resolution of chronic WAD symptoms from a whiplash 12 years previous. Both the Fortner et al.29) and Ferrantelli et al.30) cases were patients who had prior, unsuccessful treatment from both a chiropractor and physiotherapist. The present case also had previous unsuccessful treatment from a chiropractor. The reason these three cases continued to suffer despite receiving previous physiotherapy and/or chiropractic care is likely due to the fact that traditional, or classic physiotherapy and chiropractic methods do not use valid means to correct the cervical lordosis.
As has been proven by the trials from Moustafa et al.10,11,12,13), treatments that fail to restore the ideal cervical lordosis may reduce pain levels initially, however, patient symptoms will typically regress toward baseline at the termination of care, and this may occur as quickly as 12-weeks later. Alternatively, the Moustafa trials also demonstrate that patients getting a multimodal program of care that includes cervical extension traction were able to achieve an improved cervical alignment as well as symptom relief that did not regress, but remained stable for at least a years’ follow-up.
This case is the third whiplash case demonstrating the successful resolution of WAD symptoms after having improved cervical lordosis after CBP care in patients who failed to get relief from receiving traditional physiotherapy and/or chiropractic treatments previously. We agree with Oakley and Harrison31), and as discussed by Fortner et al.29), that the lack of normal cervical lordosis plays a key role in lingering symptoms associated with WAD patients. Future research needs to focus on the re-alignment of the cervical lordosis in treating patients with CWS.
Why does the loss of cervical lordosis cause symptoms? First it is known that the incidence of whiplash causes instantaneous cervical spine trauma through the ‘whiplash’ effect of posterior translation of the head followed by cervical spine extension and flexion32,33,34). The possibility of many tissues being injured exists during a whiplash if the crash-induced strain exceeds the tissues’ tolerance35). This includes any of the tissues involved including muscles, ligaments, facet joints, nerve roots, etc. Altered cervical spine alignment causes altered verterbral coupling patterns36, 37). Therefore, every day motions of the head and neck contributes to altered biomechanical stresses and strains onto the previously injured tissues by the cervical spine being in an altered (non-physiologic) neutral position (resulting from the initial whiplash event)31). Various cervical spine tissues may become pain generators and cause lingering symptoms in patients suffering from CWS35, 38).
This case has the inherent limitations of a case report, having only a single case. This case is also limited by lacking a long-term follow-up. Also since multiple treatments were used it is technically not known which of the treatments (exercise, adjustments, traction) contributed to the restoration of normal cervical lordosis. It is thought that extension traction contributes the most to an increase in lordosis due to ligamentous creep39) which causes a plastic deformation40), or permanent extension change to the spine as the anterior longitudinal ligament and anterior disc tissues are stretched. Evidence in support of this comes from the Moustafa trials10,11,12,13). Their treatment groups doing cervical extension traction had improvements in cervical lordosis, whereas, the patients getting the same treatment minus the extension traction did not get improved cervical alignment. Further, Moustafa et al.41) recently performed a trial of extension traction only treatment to asymptomatics showing lordosis improvements versus no improvement in lordosis in a control group.
Conflict of interest
PAO is paid by CBP NonProfit for writing the manuscript. DEH teaches chiropractic rehabilitation methods used and sells products to physicians for patient care used in this manuscript.
REFERENCES
- 1.Coulter ID, Hurwitz EL, Adams AH, et al. : Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine, 2002, 27: 291–296, discussion 297–298. [DOI] [PubMed] [Google Scholar]
- 2.Braaf MM, Rosne RS: Trauma of cervical spine as cause of chronic headache. J Trauma, 1975, 15: 441–446. [DOI] [PubMed] [Google Scholar]
- 3.Nagasawa A, Sakakibara T, Takahashi A: Roentgenographic findings of the cervical spine in tension-type headache. Headache, 1993, 33: 90–95. [DOI] [PubMed] [Google Scholar]
- 4.Vernon H, Steiman I, Hagino C: Cervicogenic dysfunction in muscle contraction headache and migraine: a descriptive study. J Manipulative Physiol Ther, 1992, 15: 418–429. [PubMed] [Google Scholar]
- 5.Harrison DD, Harrison DE, Janik TJ, et al. : Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine, 2004, 29: 2485–2492. [DOI] [PubMed] [Google Scholar]
- 6.McAviney J, Schulz D, Bock R, et al. : Determining the relationship between cervical lordosis and neck complaints. J Manipulative Physiol Ther, 2005, 28: 187–193. [DOI] [PubMed] [Google Scholar]
- 7.Harrison DD, Jackson BL, Troyanovich S, et al. : The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study. J Manipulative Physiol Ther, 1994, 17: 454–464. [PubMed] [Google Scholar]
- 8.Harrison DE, Cailliet R, Harrison DD, et al. : A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil, 2002, 83: 447–453. [DOI] [PubMed] [Google Scholar]
- 9.Harrison DE, Harrison DD, Betz J, et al. : Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther, 2003, 26: 139–151. [DOI] [PubMed] [Google Scholar]
- 10.Moustafa IM, Diab AM, Ahmed AM, et al. : The efficacy of cervical lordosis rehabilitation for nerve root function, pain, and segmental motion in cervical spondylotic radiculopathy. Physiotherapy, 2011, 97: 846–847. [Google Scholar]
- 11.Moustafa IM, Diab AA, Taha S, et al. : Addition of a sagittal cervical posture corrective orthotic device to a multimodal rehabilitation program improves short- and long-term outcomes in patients with discogenic cervical radiculopathy. Arch Phys Med Rehabil, 2016, 97: 2034–2044. [DOI] [PubMed] [Google Scholar]
- 12.Moustafa IM, Diab AA, Harrison DE: The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study. Eur J Phys Rehabil Med, 2017, 53: 57–71. [DOI] [PubMed] [Google Scholar]
- 13.Moustafa IM, Diab AA, Hegazy FA, et al. : Does rehabilitation of cervical lordosis influence sagittal cervical spine flexion extension kinematics in cervical spondylotic radiculopathy subjects? J Back Musculoskeletal Rehabil, 2017, 30: 937–941. [DOI] [PubMed] [Google Scholar]
- 14.Balla JI: The late whiplash syndrome. Aust N Z J Surg, 1980, 50: 610–614. [DOI] [PubMed] [Google Scholar]
- 15.Spitzer WO, Skovron ML, Salmi LR, et al. : Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine, 1995, 20: 1S–73S. [PubMed] [Google Scholar]
- 16.Seroussi R, Singh V, Fry A: Chronic whiplash pain. Phys Med Rehabil Clin N Am, 2015, 26: 359–373. [DOI] [PubMed] [Google Scholar]
- 17.Young WF: The enigma of whiplash injury. Current management strategies and controversies. Postgrad Med, 2001, 109: 179–180, 183–186. [DOI] [PubMed] [Google Scholar]
- 18.Hadanny A, Efrati S: Treatment of persistent post-concussion syndrome due to mild traumatic brain injury: current status and future directions. Expert Rev Neurother, 2016, 16: 875–887. [DOI] [PubMed] [Google Scholar]
- 19.Hohl M: Soft-tissue injuries of the neck in automobile accidents. Factors influencing prognosis. J Bone Joint Surg Am, 1974, 56: 1675–1682. [PubMed] [Google Scholar]
- 20.Norris SH, Watt I: The prognosis of neck injuries resulting from rear-end vehicle collisions. J Bone Joint Surg Br, 1983, 65: 608–611. [DOI] [PubMed] [Google Scholar]
- 21.Kristjansson E, Jónsson H, Jr: Is the sagittal configuration of the cervical spine changed in women with chronic whiplash syndrome? A comparative computer-assisted radiographic assessment. J Manipulative Physiol Ther, 2002, 25: 550–555. [DOI] [PubMed] [Google Scholar]
- 22.Harrison DD: Abnormal postural permutations calculated as rotations and translations from an ideal normal upright static posture. In: Sweere, JJ Chiropractic Family Practice. Gaithersburg: Aspen Publishers, 1992, chap 6–1, pp 1–22. [Google Scholar]
- 23.Harrison DE, Harrison DD, Cailliet R, et al. : Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine, 2000, 25: 2072–2078. [DOI] [PubMed] [Google Scholar]
- 24.Harrison DE, Holland B, Harrison DD, et al. : Further reliability analysis of the Harrison radiographic line-drawing methods: crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J Manipulative Physiol Ther, 2002, 25: 93–98. [DOI] [PubMed] [Google Scholar]
- 25.Harrison DE, Harrison DD, Colloca CJ, et al. : Repeatability over time of posture, radiograph positioning, and radiograph line drawing: an analysis of six control groups. J Manipulative Physiol Ther, 2003, 26: 87–98. [DOI] [PubMed] [Google Scholar]
- 26.Harrison DD, Janik TJ, Harrison GR, et al. : Chiropractic biophysics technique: a linear algebra approach to posture in chiropractic. J Manipulative Physiol Ther, 1996, 19: 525–535. [PubMed] [Google Scholar]
- 27.Oakley PA, Harrison DD, Harrison DE, et al. : Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc, 2005, 49: 270–296. [PMC free article] [PubMed] [Google Scholar]
- 28.Harrison DE, Harrison DD, Haas JW: Structural rehabilitation of the cervical spine. Evanston, WY: Harrison CBP® Seminars, Inc., 2002. [Google Scholar]
- 29.Fortner MO, Oakley PA, Harrison DE: Cervical lordosis restoration for late whiplash syndrome alleviates chronic headaches 13-years after motor vehicle collision: a CBP® case report with a 1-year follow-up. In Review.
- 30.Ferrantelli JR, Harrison DE, Harrison DD, et al. : Conservative treatment of a patient with previously unresponsive whiplash-associated disorders using clinical biomechanics of posture rehabilitation methods. J Manipulative Physiol Ther, 2005, 28: e1–e8. [DOI] [PubMed] [Google Scholar]
- 31.Oakley PA, Harrison DE: Cervical hypolordosis/kyphosis contribution to post-concussion and late whiplash syndromes: a hypothesis. Unpublished manuscript.
- 32.Grauer JN, Panjabi MM, Cholewicki J, et al. : Whiplash produces an S-shaped curvature of the neck with hyperextension at lower levels. Spine, 1997, 22: 2489–2494. [DOI] [PubMed] [Google Scholar]
- 33.Cusick JF, Pintar FA, Yoganandan N: Whiplash syndrome: kinematic factors influencing pain patterns. Spine, 2001, 26: 1252–1258. [DOI] [PubMed] [Google Scholar]
- 34.Kaneoka K, Ono K, Inami S, et al. : Motion analysis of cervical vertebrae during whiplash loading. Spine, 1999, 24: 763–769, discussion 770. [DOI] [PubMed] [Google Scholar]
- 35.Siegmund GP, Winkelstein BA, Ivancic PC, et al. : The anatomy and biomechanics of acute and chronic whiplash injury. Traffic Inj Prev, 2009, 10: 101–112. [DOI] [PubMed] [Google Scholar]
- 36.Sizer J, Phelps V, Brismee JM: Diagnosis and management of cervicogenic headache and local cervical syndrome with multiple pain generators. J Manual Manip Ther, 2002, 10: 136–152. [Google Scholar]
- 37.Takeshima T, Omokawa S, Takaoka T, et al. : Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine, 2002, 27: E348–E355. [DOI] [PubMed] [Google Scholar]
- 38.Harrison DE, Harrison DD, Troyanovich SJ: Three-dimensional spinal coupling mechanics: Part II. Implications for chiropractic theories and practice. J Manipulative Physiol Ther, 1998, 21: 177–186. [PubMed] [Google Scholar]
- 39.Oliver MJ, Twomey LT: Extension creep in the lumbar spine. Clin Biomech (Bristol, Avon), 1995, 10: 363–368. [DOI] [PubMed] [Google Scholar]
- 40.Panjabi MM, White AA, III: Biomechanics in the musculoskeletal system. New York: Churchill Livingstone, 2001, p 80. [Google Scholar]
- 41.Moustafa IM, Diab AA, Taha S, et al. : Demonstration of central conduction time and neuroplastic changes after cervical lordosis rehabilitation in asymptomatic subjects: a randomized, placebo-controlled trial. Proceedings of the 14th biennial congress of the World Federation of Chiropractic, March 15–18, 2017. [DOI] [PMC free article] [PubMed]


