Abstract
[Purpose] To present the case of the dramatic reduction in pain, disability, and neurologic symptoms following the reduction of forward head translation and increased cervical curvature in a patient suffering from post-surgical radiculopathy. [Subject and Methods] A 52-year-old male mechanic presented with chronic neck pain, unilateral paresthesia along the C5 and C6 dermatome distributions and diminished unilateral grip strength for 12 years following a C5–C6 cervical discectomy and fusion. Outcome measures included the neck disability index, the numerical pain rating scale, and the Zebris cervical range of motion system. Radiographs and computerized posture analysis revealed excessive forward head posture. Initial traditional ‘symptom-relief’ chiropractic rehabilitation was provided, followed by CBP® structural rehabilitation of head and neck posture with a 2.5 year follow-up. [Results] The initial traditional chiropractic rehabilitation did not improve posture or disability scores. CBP methods resulted in radiograph-verified postural alignment improvements corresponding with clinically significant improvements in the patient’s neurologic condition, pain and disability scores. These results were maintained at a 2.5 year follow-up with minimal treatment. [Conclusion] Patients with post-surgical axial symptoms and/or radicular complaints should be screened for altered cervical alignment and anterior head translation. Future studies should attempt to duplicate these positive results in a trial with long-term follow-up.
Key words: Cervical fusion, Forward head posture, CBP
INTRODUCTION
The point prevalence of neck pain is between 7–40% with a lifetime prevalence of 71%1). The average annual incidence of cervical radiculopathy is 0.1 per 1,000 (0.01%)1). Collectively, chronic spinal pain and radiculopathy unresponsive to conservative treatment are the most common reasons for surgical intervention2).
Problematically, a significant number of cervical spine post-surgical patients experience a negative outcome of persistent axial pain (19–38%) and extremity numbness or weakness (26%)2,3,4). Several theories have been put forth for probable causes of these types of post-surgical impairments, including: 1) failure to obtain a stable fusion; 2) subsidence (collapse into the superior endplate of the inferior vertebra) of the fused segment; 3) adjacent segment degenerative disc disease; 4) hyper-mobility of adjacent segments; 5) kyphotic alignment of the fused segments2,3,4,5).
In the lumbar spine, anterior translation of the thoracic spine has been shown to correlate to poor-outcomes after lumbar fusion6,7,8); thereby leading to sagittal alignment pre-surgical considerations9). More recently, efforts to establish similar pre-surgical alignment recommendations for the cervical spine have emerged10, 11).
The post-surgical cervical lordotic alignment is critical to prevent neurologic symptoms3, 12, 13), as is the sagittal head and cervical spine alignment10, 14). Tang et al.14) found that the severity of disability increases with positive cervical malalignment following fusion surgery. They determined a critical threshold of 40 mm, beyond which the correlations of disability and forward head posture were most significant. Ajello et al.10) determined that post-surgical forward head posture that is less than 25 mm was associated with positive outcomes.
To our knowledge, anterior translation of the head and upper cervical spine has not been investigated for its non-surgical reduction following surgery to treat lingering axial and radicular symptoms. The present case describes the simultaneous reduction in forward head posture and pain and disability impairment in a patient suffering from post-surgical axial symptoms and hand numbness/weakness treated with Chiropractic Biophysics® (CBP®) technique structural rehabilitative methods.
SUBJECT AND METHODS
In the summer of 2004, a 62-year-old male presented to the lead author’s spine clinic seeking treatment for neck pain, numbness and tingling in the right antero-lateral forearm, and right arm weakness. His occupation was a diesel mechanic and his condition was reported to interfere with his ability to work due to the inability to grasp and use tools with his right hand. The patient’s past history revealed previous cervical spine surgical intervention for a C5–C6 instability, vertebral spondylosis, and disc herniation. His initial cervical spine surgery was in 1991, where C5–C6 was fused using an autologous iliac crest bone graft. In 1992, the patient reported that this first surgery failed to stabilize the C5–C6 joint and a second surgery was performed using an anterior plate in addition to the autologous bone graft at C5–C6. Since 1992 the patient has suffered from post-surgical axial symptoms and radicular signs.
The male was 172.7 cm in height and weighed 83.9 kg. Cervical spine pain was diffuse, being bilateral extending from C4–T4 with pain, tenderness, and myofascial spasms identified with spinal palpation. A reduced sensation was identified on the right forearm at the C5–C6 dermatome. The brachioradialis reflex was hypo-active with right-sided weakness in grip strength.
The patient was administered the numerical rating scale (NRS) for neck pain intensity (0=no pain; 10=incapacitated due to pain)15), where he rated his pain as 6/10. The neck disability index (NDI)16) indicated an 18% disability (Table 1).
Table 1. Initial, 1-month, 2-month, 6-month, and 2.5 year follow-up assessment results for number of treatments, NRS, NDI, and CROM.
| Variable | Initial | 1st | 2nd | 6-month | 2.5-year |
|---|---|---|---|---|---|
| exam | re-exam | re-exam | f/up | f/up | |
| 7-21-04 | 8-18-04 | 9-27-04 | 1-15-05 | 3-12-07 | |
| #Treatments | 0 | 10/10 | 11/21 | 8/29 | 30/59 |
| since last/total | Relief visits | Corrective visits | 2/mnth | 1.15/mnth | |
| NRS | 6/10 | 2/10 | 1/10 | 1/10 | 2/10 |
| NDI | 18% | 22% | 12% | 10% | 8% |
| CROM | |||||
| Ext (−RxH) | 32° | 32° | 44° | N/R | N/R |
| Flex (+RxH) | 48° | 50° | 50° | ||
| L Rot (+RyH) | 23° | 27° | 23° | ||
| R Rot (−RyH) | 69° | 59° | 63° | ||
| R Lat Bend (+RzH) | 27° | 23° | 34° | ||
| L Lat Bend (−RzH) | 31° | 27° | 28° | ||
NRS: numeric rating scale; NDI: neck disability scale; CROM: cervical range of motion; f/up: follow-up; N/R: not reported.
For functional evaluation, the patient’s cervical spine range of motion (CROM) was assessed using the Zebris sonic range of motion equipment (www.zebris.com). All cervical rotational ranges of motion were significantly reduced for the patient’s age17) (Table 1).
A computerized postural analysis and cervical spine radiographs were performed for a structural evaluation. The PosturePrint® system provided by Biotonix (Montreal, Quebec, Canada) was utilized to assess the patients 3-D posture. Although this system uses three two-dimensional photographs (an anterior to posterior, a right lateral, and a left lateral), the computer uses a complex algorithm to reconstruct the estimated three-dimensional rotations and translations of the head, thorax, and pelvis. The PosturePrint’s algorithms have been found to be accurate to within 2 mm for translations and 2° for rotations, when compared to known rotations and translations of a mannequin’s postural components18, 19). The patient was found to have significant anterior translation of the pelvis relative to the feet (+TzP), anterior translation of the head relative to the thorax (+TzH), and head flexion (+RxH).
Lateral cervical, flexion and extension, and anterior-posterior cervical radiography was performed. Notably, the anterior plated and grafted fusion was found to be stable on flexion and extension movement. The lateral cervical radiograph was assessed using CBP® technique methods where segmental and total curvature was analyzed with the Harrison posterior tangent (HPT) method and anterior translation of C2 relative to C7 was measured20,21,22) (Fig. 1; Table 2). These measurements were performed by the PostureRay computerized analysis system (Trinity, FL, USA).
Fig. 1.
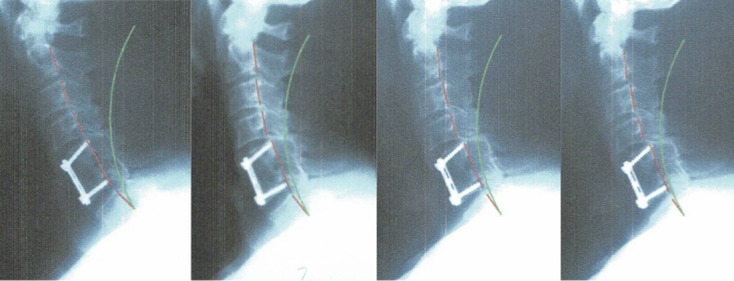
Initial and follow-up lateral cervical radiographs. A: 7-21-04; B: 9-27-04; C: 1-15-05; D: 3-12-07.
Note at C5–C6 the evidence of an anterior plate and autologous iliac crest bone graft. The green line represents ideal cervical lordosis, the red line highlights patient.
Table 2. Initial, 2-month, 6-month, and 2.5 year follow-up assessment results for radiographic parameters.
| Variable | Normal | Initial | 2nd exam | 6-month | 2.5-year |
|---|---|---|---|---|---|
| values41, 42) | exam | f/up | f/up | ||
| 7-21-04 | 9-27-04 | 1-15-05 | 3-12-07 | ||
| ARA C2–C7* | −34–42° | −25° | −31° | 31° | −30° |
| TzH** | 0–15 mm | 59 mm | 39.5 mm | 46 mm | 46 mm |
| APL*** | −24–29° | 3° | −6° | −4° | −4° |
| RRA C2–C3+ | −7–9° | −2° | −3° | −4° | −4° |
| RRA C3–C4+ | −6–8° | −3° | −4° | −7° | −6° |
| RRA C4–C5+ | ‘−6–8° | −8° | −12° | −9° | −9° |
| RRA C5–C6+ | ‘−6–8° | 0°++ | 0°++ | 0°++ | 0°++ |
| RRA C6–C7+ | ‘−6–8° | −12° | −12° | −11° | ‘−11° |
*ARA: Absolute rotation angle between posterior vertebral body tangents on C2 and C7. Negative values indicate spinal extension.
**TzH: Forward head translation distance: Horizontal distance of C2 posterior-superior body corner to posterior-inferior body corner of C7.
***APL: Atlas plane line: Angle between estimated cross-section of C1 to horizontal (negative indicates backward rotation compared to horizontal).
+ RRA: Relative rotation angle (segmental angle between posterior tangents). Negative values indicate spinal extension.
++ The C5–C6 segment is the one that is fused in this patient and no movement is possible.
The patient was treated with traditional chiropractic ‘functional relief care’ techniques for the initial 10 visits. These treatments included: 1) spinal adjustments directed to the non-fused segments of the cervical spine and upper thoracic spine; adjustments were performed by hand and with the Impulse™ hand held adjusting instrument23) (www.neuromechanical.com); 2) general stretching into the rotational ranges of motion of the cervical spine; 3) focused myofascial therapy directed to the cervical and thoracic spine; 4) cryotherapy of the cervical and thoracic regions following the above three treatment methods. Following these 10 treatments, a re-evaluation was performed and included all previous evaluations except radiography.
After this re-evaluation, ‘structural rehabilitative care’ using CBP technique methods24, 25) was performed lasting for an additional 11 visits. These methods included: 1) mirror image® postural adjustments using the PCT drop table (www.posturalcorrectiontools.com) and the Impulse adjusting instrument; 2) mirror image exercises; 3) mirror image cervical spine extension traction25). Following these 11 treatments, a re-evaluation was performed and included all initial questionnaires, posture evaluation, lateral cervical radiograph, and CROM. This study received IRB approved waiver of informed consent through IntegReview IRB (www.integreview.com) on August 30, 2017 (protocol No. CBP2017-002).
RESULTS
After the initial 10 treatments of ‘functional relief care,’ the NRS score decreased to a 2/10, however, the sagittal posture was not improved, the NDI disability increased to 22% and the CROM was not improved (Table 1).
Notably, after the 11 treatments of ‘structural rehabilitative care’ using CBP technique, all variables showed clinically significant improvements: CROM was improved 12° in extension and 7° in lateral bending, NDI decreased to 12%, NRS decreased to a 1/10, forward head translation decreased, and the C2–C7 cervical lordosis increased (Tables 1 and 2).
After the 21 treatments, the patient’s brachioradialis reflex was normal as was the C5–C6 dermatome sensation. The patient stated: “Now I’m sore in the morning when I get up, but before, the pain used to get me up several times during the night.” Further, the patient reported an increased capacity to work and increased grip strength. The patient returned to work and agreed to continue treatment on a twice a month basis and the treatment methods included a combination of all previous interventions.
Following 4-months of treatment, a further 8 visits (29 overall treatments), a follow-up re-evaluation was performed (Tables 1 and 2; Fig. 1). His health status and outcome measures were maintained with only a small loss of the initial correction of forward head posture (6.5mm). The patient reduced his frequency of treatments to one treatment per month. Following 26-months of this care (30 treatments using a combination of all previous interventions; 59 treatments overall), the patient returned for a final follow-up evaluation (Tables 1 and 2; Fig. 1). Again, his improved health status was maintained. The patient consented to the publication of his radiographs and treatment results.
DISCUSSION
This report demonstrates the positive effects of both relief care and corrective care in a patient suffering from post-surgical pain and impairment. Notably, the initial relief care (10 treatments) resulted in improvement of the patient’s subjective complaints on the NRS only, but not on the NDI nor in CROM. After the subsequent treatments incorporating CBP structural rehabilitative care (11 treatments), there was improvement in all measures, NRS, NDI, as well as increased flexibility, (12° in extension) corresponding with structural improvements of decreased forward head translation, and increased cervical lordosis (Fig. 1).
At long-term follow up, continuing ‘maintenance’ treatments at 1–2 per month, the 4-month, and 2.5 year check-ups revealed that the patient remained well symptomatically as well as the structural changes in reduced forward head posture and increased cervical lordosis remained stable.
The structural results in this case are consistent with that of clinical trials of extension traction26,27,28,29) that found long-term stability in cervical curve correction after 1–1.3 years. This case was also consistent with these trials in that with structural improvement of increasing lordosis and decreasing forward head posture, a decrease in pain and disability occurred26,27,28,29).
In one trial, Moustafa et al.26), demonstrated that increasing the lordosis in patients with cervical radiculopathy showed decreased arm and neck pain, decreased disability, as well as improvement in amplitude and latency of dermatomal somatosensory evoked potentials (DSSEPs), as well as improved central somatosensory conduction times (N13–N20). In comparison, their control group who got ‘standard’ physiotherapy care, not receiving cervical extension traction, showed initial improvement in pain (at 10-weeks), but then long-term (1 year) had a digression towards baseline, whereas, the treatment group receiving extension traction, had their improvements maintained at one year. The authors26) speculated that the improved cervical lordosis and reduced forward head posture contributed to the long-term positive outcome.
Research has indicated that anterior head posture contributes to and/or has strong correlation to neck and upper back pain30,31,32), chronic headaches33,34,35,36), cervical muscle weakness33), thoracic outlet and radicular symptoms37,38,39), reduced cervical spine range of motion (CROM)35, 36, 39, 40), as well as disability32).
The normal cervical spine has been modeled to be circular in shape with a range of 31–42° of extension as measured by the HPT method from C2–7 as being ‘normal’41,42,43,44). Anterior head translation should be less than 15 mm to be considered in the ‘normal’ range41). When the head is forward in the ‘neutral’ position, the cervical spine is known have lower cervical flexion and upper cervical extension45). It is easy to conceive that this malposition/subluxation of the cervical spine will exert abnormal stresses and strains onto the spinal tissues which then may elicit nociceptive tendencies to create a potential barrage of potential symptoms.
Fernandez et al. 35), for example, determined that forward head translation correlated to more headache parameters and proposed that this forward head position causes contraction of the suboccipital muscles and contributes to the origin or perpetuation of chronic tension-type headache.
In this case, the patient had a C5–C6 surgical fusion, which obviously would interfere with the normal spinal coupling patterns with a forward head position leading to an incongruent match between what the tissues would normally do to in an attempt to accommodate poor posture and the inability for natural spinal coupling to occur. The fusion of C5–C6 in this patient was not in an extended position of 7–9° as recommended by Harrison et al. 43), but straight in alignment. This would then force the other mobile joints to ‘take up the slack’ in terms of spinal coupling to allow the head to be in the forward position and thus could add further stressing of particular joints and tissues in the cervical area leading to the pain and functional limitations seen in this patient.
The forward head position and hypolordosis in the cervical spine, as seen in this case, leads to a lengthening of the spinal canal and traction effect on the spinal cord46). The radiculopathy in this case was also likely due to posture; this would explain why when the posture improved with CBP and cervical extension traction, the disability in our patient improved, whereas, only pain and not the disability measures improved after ‘relief care.’ We therefore, speculate that anterior head translation and cervical hypolordosis was the primary cause of the patient’s post-surgical pain and impairment.
As stated by Moustafa et al.26) ‘in populations with discogenic cervical radiculopathy, loss of cervical lordosis, and forward head posture that can tolerate extension positions, it would seem of value to conservatively restore cervical alignment as a first line of management.’ As a patient presenting with failed cervical discectomy and fusion, we contend by the outcome in this case, that it is not too late to restore the head and neck alignment and propose that better long-term outcomes can still be achieved treating these patients. The relevance of this case highlights the fact that manual therapists who are presented with post-surgical patients having anterior head translation and cervical hypolordosis should incorporate methods involving the correction of these deformities to improve their patient outcomes.
A limitation to this case is that it is only a single case (n=1). Further, no x-ray was performed between the initial ‘symptomatic’ treatments (initial 10 treatments) and when the patient transitioned to do ‘corrective’ care incorporating CBP methods. This is because the treatment of spinal manipulative therapy has not routinely been associated with structural changes in the spine29, 47,48,49).
Conflict of interest
PAO is paid by CBP NonProfit for writing the manuscript. DEH teaches chiropractic rehabilitation methods used and sells products to physicians for patient care used in this manuscript.
REFERENCES
- 1.Nachemson A, Jonsson E: Neck & back pain. 2000, Ch. 8 pp 172–173. [Google Scholar]
- 2.An HS, Cotler JM: Spinal instrumentation, 2nd ed. 1999, Ch. 8. [Google Scholar]
- 3.Kawakami M, Tamaki T, Yoshida M, et al. : Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord, 1999, 12: 50–56. [PubMed] [Google Scholar]
- 4.Sampath P, Bendebba M, Davis JD, et al. : Outcome in patients with cervical radiculopathy. Prospective, multicenter study with independent clinical review. Spine, 1999, 24: 591–597. [DOI] [PubMed] [Google Scholar]
- 5.Katsuura A, Hukuda S, Imanaka T, et al. : Anterior cervical plate used in degenerative disease can maintain cervical lordosis. J Spinal Disord, 1996, 9: 470–476. [PubMed] [Google Scholar]
- 6.Kawakami M, Tamaki T, Ando M, et al. : Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine, 2002, 27: 59–64. [DOI] [PubMed] [Google Scholar]
- 7.Kumar MN, Baklanov A, Chopin D: Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J, 2001, 10: 314–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glassman SD, Bridwell K, Dimar JR, et al. : The impact of positive sagittal balance in adult spinal deformity. Spine, 2005, 30: 2024–2029. [DOI] [PubMed] [Google Scholar]
- 9.Scheer JK, Tang JA, Smith JS, et al. : International Spine Study Group: Reoperation rates and impact on outcome in a large, prospective, multicenter, adult spinal deformity database: clinical article. J Neurosurg Spine, 2013, 19: 464–470. [DOI] [PubMed] [Google Scholar]
- 10.Ajello M, Marengo N, Pilloni G, et al. : Is possible to evaluate the ideal cervical alignment for each patient needing surgery? An easy rule to determine the appropriate cervical lordosis in pre-operative planning. World Neurosurg, 2017, 97: 471–478. [DOI] [PubMed] [Google Scholar]
- 11.Ames CP, Blondel B, Scheer JK, et al. : Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine, 2013, 38: S149–S160. [DOI] [PubMed] [Google Scholar]
- 12.Naderi S, Ozgen S, Pamir MN, et al. : Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery, 1998, 43: 43–49, discussion 49–50. [DOI] [PubMed] [Google Scholar]
- 13.Grosso MJ, Hwang R, Mroz T, et al. : Relationship between degree of focal kyphosis correction and neurological outcomes for patients undergoing cervical deformity correction surgery. J Neurosurg Spine, 2013, 18: 537–544. [DOI] [PubMed] [Google Scholar]
- 14.Tang JA, Scheer JK, Smith JS, et al. ISSG: The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery, 2012, 71: 662–669, discussion 669. [DOI] [PubMed] [Google Scholar]
- 15.Fejer R, Jordan A, Hartvigsen J: Categorising the severity of neck pain: establishment of cut-points for use in clinical and epidemiological research. Pain, 2005, 119: 176–182. [DOI] [PubMed] [Google Scholar]
- 16.MacDermid JC, Walton DM, Avery S, et al. : Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther, 2009, 39: 400–417. [DOI] [PubMed] [Google Scholar]
- 17.Cocchiarella L, Andersson GB: Guides to the evaluation of permanent impairment, 5th ed. AMA Press, 2001, pp 405–422. [Google Scholar]
- 18.Harrison DE, Janik TJ, Cailliet R, et al. : Validation of a computer analysis to determine 3-D rotations and translations of the rib cage in upright posture from three 2-D digital images. Eur Spine J, 2007, 16: 213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janik TJ, Harrison DE, Cailliet R, et al. : Description and validity of an algorithm to estimate three-dimensional rotations and translations of the head in upright posture from three two-dimensional digital images. J Manipulative Physiol Ther, 2007, 30: 124–129. [DOI] [PubMed] [Google Scholar]
- 20.Jackson BL, Harrison DD, Robertson GA, et al. : Chiropractic biophysics lateral cervical film analysis reliability. J Manipulative Physiol Ther, 1993, 16: 384–391. [PubMed] [Google Scholar]
- 21.Harrison DE, Harrison DD, Cailliet R, et al. : Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine, 2000, 25: 2072–2078. [DOI] [PubMed] [Google Scholar]
- 22.Harrison DE, Holland B, Harrison DD, et al. : Further reliability analysis of the Harrison radiographic line-drawing methods: crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J Manipulative Physiol Ther, 2002, 25: 93–98. [DOI] [PubMed] [Google Scholar]
- 23.Colloca CJ, Keller TS, Black P, et al. : Comparison of mechanical force of manually assisted chiropractic adjusting instruments. J Manipulative Physiol Ther, 2005, 28: 414–422. [DOI] [PubMed] [Google Scholar]
- 24.Oakley PA, Harrison DD, Harrison DE, et al. : Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc, 2005, 49: 270–296. [PMC free article] [PubMed] [Google Scholar]
- 25.Harrison DE, Harrison DD, Haas JW: Structural rehabilitation of the cervical spine. Harrison CBP® Seminars, Inc., 2002.
- 26.Moustafa IM, Diab AA, Taha S, et al. : Addition of a sagittal cervical posture corrective orthotic device to a multimodal rehabilitation program improves short- and long-term outcomes in patients with discogenic cervical radiculopathy. Arch Phys Med Rehabil, 2016, 97: 2034–2044. [DOI] [PubMed] [Google Scholar]
- 27.Moustafa IM, Diab AA, Harrison DE: The effect of normalizing the sagittal cervical configuration on dizziness, neck pain, and cervicocephalic kinesthetic sensibility: a 1-year randomized controlled study. Eur J Phys Rehabil Med, 2017, 53: 57–71. [DOI] [PubMed] [Google Scholar]
- 28.Harrison DE, Harrison DD, Betz JJ, et al. : Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: nonrandomized clinical control trial. J Manipulative Physiol Ther, 2003, 26: 139–151. [DOI] [PubMed] [Google Scholar]
- 29.Harrison DE, Cailliet R, Harrison DD, et al. : A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil, 2002, 83: 447–453. [DOI] [PubMed] [Google Scholar]
- 30.Haughie LJ, Fiebert IM, Roach KE: Relationship of forward head posture and cervical backward bending to neck pain. J Manual Manip Ther, 1995, 3: 91–97. [Google Scholar]
- 31.Griegel-Morris P, Larson K, Mueller-Klaus K, et al. : Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther, 1992, 72: 425–431. [DOI] [PubMed] [Google Scholar]
- 32.Yip CH, Chiu TT, Poon AT: The relationship between head posture and severity and disability of patients with neck pain. Man Ther, 2008, 13: 148–154. [DOI] [PubMed] [Google Scholar]
- 33.Watson DH, Trott PH: Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia, 1993, 13: 272–284, discussion 232. [DOI] [PubMed] [Google Scholar]
- 34.Marcus DA, Scharff L, Mercer S, et al. : Musculoskeletal abnormalities in chronic headache: a controlled comparison of headache diagnostic groups. Headache, 1999, 39: 21–27. [DOI] [PubMed] [Google Scholar]
- 35.Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, et al. : Trigger points in the suboccipital muscles and forward head posture in tension-type headache. Headache, 2006, 46: 454–460. [DOI] [PubMed] [Google Scholar]
- 36.Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, et al. : Forward head posture and neck mobility in chronic tension-type headache: a blinded, controlled study. Cephalalgia, 2006, 26: 314–319. [DOI] [PubMed] [Google Scholar]
- 37.Pascarelli EF, Hsu YP: Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil, 2001, 11: 1–21. [DOI] [PubMed] [Google Scholar]
- 38.Smith KF: The thoracic outlet syndrome: a protocol of treatment. J Orthop Sports Phys Ther, 1979, 1: 89–99. [DOI] [PubMed] [Google Scholar]
- 39.Abdulwahab SS, Sabbahi M: Neck retractions, cervical root decompression, and radicular pain. J Orthop Sports Phys Ther, 2000, 30: 4–9, discussion 10–12. [DOI] [PubMed] [Google Scholar]
- 40.Walmsley RP, Kimber P, Culham E: The effect of initial head position on active cervical axial rotation range of motion in two age populations. Spine, 1996, 21: 2435–2442. [DOI] [PubMed] [Google Scholar]
- 41.Harrison DD, Harrison DE, Janik TJ, et al. : Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine, 2004, 29: 2485–2492. [DOI] [PubMed] [Google Scholar]
- 42.Harrison DD, Janik TJ, Troyanovich SJ, et al. : Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine, 1996, 21: 667–675. [DOI] [PubMed] [Google Scholar]
- 43.Harrison DD, Janik TJ, Troyanovich SJ, et al. : Evaluation of the assumptions used to derive an ideal normal cervical spine model. J Manipulative Physiol Ther, 1997, 20: 246–256. [PubMed] [Google Scholar]
- 44.McAviney J, Schulz D, Bock R, et al. : Determining the relationship between cervical lordosis and neck complaints. J Manipulative Physiol Ther, 2005, 28: 187–193. [DOI] [PubMed] [Google Scholar]
- 45.Ordway NR, Seymour RJ, Donelson RG, et al. : Cervical flexion, extension, protrusion, and retraction. A radiographic segmental analysis. Spine, 1999, 24: 240–247. [DOI] [PubMed] [Google Scholar]
- 46.Breig A, Turnbull I, Hassler O: Effects of mechanical stresses on the spinal cord in cervical spondylosis. A study on fresh cadaver material. J Neurosurg, 1966, 25: 45–56. [DOI] [PubMed] [Google Scholar]
- 47.Plaugher G, Cremata EE, Phillips RB: A retrospective consecutive case analysis of pretreatment and comparative static radiological parameters following chiropractic adjustments. J Manipulative Physiol Ther, 1990, 13: 498–506. [PubMed] [Google Scholar]
- 48.Harrison DD, Jackson BL, Troyanovich S, et al. : The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study. J Manipulative Physiol Ther, 1994, 17: 454–464. [PubMed] [Google Scholar]
- 49.Hurwitz EL, Aker PD, Adams AH, et al. : Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine, 1996, 21: 1746–1759, discussion 1759–1760. [DOI] [PubMed] [Google Scholar]


