Abstract
Objective
Classifying eating disorders in youth is challenging in light of developmental considerations and high rates of diagnostic migration. Understanding the transactional relationships among eating disorder symptoms, both across the transdiagnostic spectrum and within specific diagnostic categories, may clarify which core eating disorder symptoms contribute to, and maintain, eating-related psychopathology in youth.
Method
We utilized network analysis to investigate interrelationships among eating disorder symptoms in 636 treatment-seeking children and adolescents (90.3% female) ages 6–18 years (M age=15.4±2.2 years). An undirected, weighted network of eating disorder symptoms was created using behavioral and attitudinal items from the Eating Disorder Examination.
Results
Across diagnostic groups, symptoms reflecting appearance-related concerns (e.g., dissatisfaction with shape and weight) and dietary restraint (e.g., a desire to have an empty stomach) were most strongly associated with other eating disorder symptoms in the network. Binge eating and compensatory behaviors (e.g., self-induced vomiting) were strongly connected to one another, but not to other symptoms in the network. Network connectivity was similar across anorexia nervosa, bulimia nervosa, and otherwise specified feeding or eating disorder subgroups.
Conclusion
Among treatment-seeking children and adolescents, dietary restraint and shape- and weight-related concerns appear to play key roles in the psychopathology of eating disorders, supporting cognitive-behavioral theories of onset and maintenance. Similarities across diagnostic categories provide support for a transdiagnostic classification scheme. Clinical interventions should seek to disrupt these symptoms early in treatment to achieve maximal outcomes.
Keywords: Eating disorders, network analysis, classification, shape and weight concerns, dietary restraint, adolescent
Eating disorders, including anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), and otherwise specified feeding and eating disorders (OSFED), are serious psychiatric disorders that peak in adolescence (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011). Diagnosing eating disorders in children and adolescents can be challenging in light of developmental considerations (Bravender et al., 2007) and significant rates of diagnostic migration (Allen, Byrne, Oddy, & Crosby, 2013; Stice, Marti, & Rohde, 2012). The nosological complexity of eating disorders may reflect high degrees of symptom overlap among diagnoses and, as a consequence, potentially arbitrary boundaries between diagnostic categories. In particular, while the newly revised eating disorders diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5; American Psychiatric Association, 2013) have reduced rates of OSFED (Flament et al., 2015; Ornstein et al., 2013), this “catchall” taxon remains the most prevalent eating disorder diagnosis in pediatric and adult samples. Given the heterogeneity associated with OSFED, this diagnostic category may have limited prognostic utility, especially when considering treatment selection and outcome (Fairburn & Bohn, 2005). Because of these classification issues, researchers have increasingly called for alternative classification systems that are developmentally sensitive and prognostically meaningful (Keel, Brown, Holland, & Bodell, 2012). Yet, little is known about the relative importance of specific eating disorder features in children and adolescents or how these features differ between diagnostic categories.
Traditional approaches to the classification of psychopathology assume that symptoms of a psychiatric disorder reflect an underlying latent construct--the disorder itself (Borsboom & Cramer, 2013). For example, within this framework, AN is presumed to underlie a set of clinical symptoms (e.g., low body weight, intentional restriction of energy intake for weight control purposes) while BN underlies a separate symptom set (e.g., binge eating, purging). Yet this model does not take into account that certain symptoms, such as overvaluation of shape and weight (Tabri et al., 2015), are nearly ubiquitous among individuals with eating disorders, regardless of specific diagnosis. The DSM model also does not explain transitions among diagnostic categories following fractional changes in symptomatology (e.g., an individual could move from BN to BED simply by reducing the frequency of compensatory behaviors to less than once per week, or from BN to AN through weight loss). Alternative methods for diagnosing eating disorders have been proposed, including a transdiagnostic approach in which eating disorders are viewed as a sharing a common symptom structure (Fairburn, 2008b), and a dimensional approach in which diagnoses are broadly applied based on the dominant symptoms (Sysko & Walsh, 2011). In particular, such approaches minimize the problem of OSFED because all individuals with clinically significant eating pathology would be diagnosed with an eating disorder, irrespective of specific clinical presentation. However, such approaches have not been tailored according to developmental stage and thus assume that the presentation and core features of eating disorders are similar across the lifespan.
By contrast, the network approach views psychiatric diagnoses as representing a set of causally connected symptoms, rather than viewing symptoms as manifestations of an underlying latent condition (Fried et al., 2016). Network analysis, a technique that can be used to construct and analyze symptom networks, has the potential to identify symptoms that cluster together within individuals across diagnostic categories (e.g., mood and anxiety disorders; Curtiss & Klemanski, 2016), as well as within a subset of disorders (e.g., eating disorders; Forbush, Siew, & Vitevitch, 2016), or an even more specific subset of disorders (e.g., BN; Levinson et al., 2017). A major benefit of network analysis is that it enables examination of the contemporaneous relationships among a given set of symptoms, controlling for all other symptoms in the network, thus allowing for a global representation of the structure of a disorder at the symptom level, rather than attempting to characterize disorders along different dimensions or groups of people. Moreover, network analysis can be performed at the level of a single individual, marking it as more clinically useful than other statistical approaches in its ability to inform personalization of treatment (de Beurs, 2017).
In a recent application of network analysis to study the interconnectedness of disordered eating symptoms in a community-recruited sample of adults with eating disorders, symptoms reflecting body checking and overvaluation of weight and shape were found to be most central (Forbush et al., 2016). These findings are consistent with cognitive-behavioral theory (Fairburn, 2008a), which proposes a causal unfolding of eating disorder symptoms whereby over-concern with shape and weight leads to stringent attempts to control one’s eating for weight control purposes, which in turn promote binge eating and subsequent compensatory behaviors.
To date, network analysis has not been used to understand relations among eating disorder symptoms in children and adolescents. Utilizing a network analysis approach has the potential to inform future diagnostic schemes by identifying core symptoms among and between eating disorder categories, as well as developmental models of onset and maintenance of eating disorders. For example, it is possible that certain eating disorder symptoms become more or less central to the maintenance of the disorder throughout development since research suggests that the clinical presentation of eating disorders (including rate of weight loss, prevalence of restrictive eating relative to binge/purge-type behaviors, and severity of disordered eating cognitions and attitudes) varies according to age (Peebles, Wilson, & Lock, 2006; Walker et al., 2014). Understanding which symptoms are most central in children and adolescents with eating disorders could assist with early identification efforts and help maximize treatment outcomes by targeting these central symptoms.
To this end, the primary aim of the current study was to utilize a network analysis approach to identify the most central eating disorder symptoms (e.g., those that are most strongly connected to other symptoms) within a transdiagnostic sample of children and adolescents who presented for outpatient psychological treatment at an eating disorders specialty clinic. Based on previous research (Forbush et al., 2016; Tabri et al., 2015) and the cognitive-behavioral model (Fairburn, 2008a), we hypothesized that symptoms reflecting shape and weight over-concern would be most central in relation to other cognitive and behavioral symptoms of eating disorders. A secondary aim was to test whether symptom networks were similar or dissimilar across three independent eating disorder diagnoses (AN, BN, and OSFED) that frequently present for treatment (Ornstein et al., 2013). We hypothesized that central symptoms would be similar across specific diagnoses, consistent with previous research (Wilfley, Schwartz, Spurrell, & Fairburn, 2000) and reflecting the lack of meaningful boundaries between these syndromes in youth.
Method
Participants
Participants were 636 children and adolescents (90.3% female), ages 6–18 years (M age=15.4±2.2), presenting to The University of Chicago Medicine for eating disorders treatment through a specialty outpatient clinic, including those evaluated for eligibility in randomized controlled trials. Participants self-identified as White (88.1%), Black (6.8%), Asian (2.7%), American-Indian/Alaskan Native (0.8%), or mixed race/other (1.6%). Most participants met criteria for DSM-5 OSFED (40.3%; n=256), with the remainder meeting criteria for AN (31.8%; n=202), BN (25.3%; n=161), BED (1.3%; n=8), or ARFID (1.4%; n=9). All protocols were approved by the University of Chicago and University of California, San Francisco Institutional Review Boards (protocol numbers 10510 and 15-16093, respectively).
Measures
Participants were assessed after providing informed consent/assent and before initiating treatment. Weight and height were measured using a calibrated digital or balance-beam scale and a stadiometer, respectively, to calculate body mass index (BMI; kg/m2). Participants were administered the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993) a semi-structured interview that has evidence for good convergent and criterion-related validity (Berg, Peterson, Frazier, & Crow, 2012) and has been used in clinical research with children as young as six years old (O’Brien et al., 2016; e.g., Tanofsky-Kraff et al., 2009; Wade, Byrne, & Bryant-Waugh, 2008). Interviewers were trained by expert raters to administer the EDE, and regular meetings occurred to promote inter-rater reliability. All diagnoses were made in collaboration with a supervising clinician and in consultation with the treatment team. The EDE generates clinical diagnoses via its behavioral frequency items, as well as indices of eating disorder cognitions and attitudes via Restraint (α=.80 in the current sample), Eating Concern (α=.75), Weight Concern (α=.82), and Shape Concern (α=.92) subscales. DSM-5 diagnoses were derived based on EDE-assessed cognitive and behavioral items.
The current study utilized items related to dietary restraint, eating concern, shape concern, and weight concern; objective and subjective binge eating; compensatory behaviors, including self-induced vomiting, laxative, or diuretic use for weight control, and excessive exercise; and an additional item assessing vigilance about shape, given evidence highlighting the importance of this construct in previous research on eating disorder symptoms (Forbush et al., 2016). All items assessed functioning in the 28 days prior to assessment. Consistent with previous studies (Allen, Byrne, McLean, & Davis, 2008; Goldschmidt et al., 2011), and based on high inter-item correlations (rs>.70), items assessing importance of weight and importance of shape were combined, as were those assessing dissatisfaction with shape and dissatisfaction with weight. We chose not to combine other highly correlated items (e.g., “dissatisfaction with shape and weight” and “feelings of fatness,” r=.78) on theoretical grounds because although they may reflect similar core constructs (e.g., attitudes towards appearance), they are purported to differ conceptually (e.g., “feeling fat” does not necessarily imply that one will be dissatisfied with shape and weight). In addition, the dietary restriction outside of binge eating item was dropped due to excessive amounts of missing data (n=488 participants with missing data) as a consequence of forced “skip” rules (i.e., only administered to individuals who endorsed at least 12 objective binge eating episodes in the past 3 months). In total, 28 EDE items were included in the network analysis (see Supplemental Materials for inter-correlations among EDE items).1 Although EDE diagnostic data from many of the participants in the current study have been included in previous data analyses addressing eating disorders classification (Eddy, Celio Doyle, Hoste, Herzog, & Le Grange, 2008; Eddy et al., 2010; Vo, Accurso, Goldschmidt, & Le Grange, 2016), this was the first study utilizing a network analysis approach with specific individual EDE items, which distinguishes it from the categorical approaches adopted in our previous work.
Validation analyses utilized the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), a well-established self-report questionnaire measuring affective/somatic depressive symptoms (current study α=.91); the Rosenberg Self-Esteem Scale (RSE; Rosenberg, 1965), a self-report measure of global self-esteem with good psychometric properties in youth (current study α=.73); and a structured clinical interview assessing common psychiatric disorders diagnosed in youth (the Schedule for Affective Disorders and Schizophrenia for School-Age Children prior to 2013, and the Mini International Neuropsychiatric Interview for Children and Adolescents after 2013, both of which have adequate psychometric properties in youth; Kaufman et al., 1997; Sheehan et al., 1997).
Statistical Analysis
Network structures of baseline EDE items were estimated first for the entire transdiagnostic sample, and then separately in youth with AN, BN, and OSFED (because these diagnoses reflect the most frequent eating disorder presentations observed in outpatient treatment settings; Ornstein et al., 2013). Each matrix was created based on Least Absolute Shrinkage and Selection Operator (LASSO) correlations, which involves computing partial correlations between each set of two EDE items while holding all other items constant. The Extended Bayesian Information Criterion was used to select the best networks. The matrices were then analyzed using the R package qgraph. Each node in the network represented one of the 28 EDE items. Consistent with previous studies (Forbush et al., 2016), we computed the following centrality measures: 1) strength, or the summed weights of connections of a particular node with all other nodes, which reflects the size of a given node’s association with other nodes in the network; 2) closeness, or the inverse of the sum of distances from a particular node to all other nodes in the network, which reflects how central a given node is within the global network structure; and 3) betweenness, or the number of times a node appears in the shortest path between two other nodes, which reflects a node’s importance in terms of connections among other nodes. To provide a lay explanation of how centrality indices work conceptually, they can be understood within the context of social networks. For example, if we wanted to identify the most influential person within a group of friends, we could identify the person or persons with highest values of strength; these individuals would have a large number of friends (or “connections”) in their networks compared to people with low values of strength. A person with lower closeness is more peripherally located/ostracized relative to other people his or her social network; and finally, a person with higher betweenness has to go through fewer people or intermediaries to reach other people in his or her social network (Opsahl, Agneessens, & Skvoretz, 2010). In the current context, nodes represent eating disorder symptoms instead of people. For all centrality measures, higher values indicate greater relative centrality of a node in the network. Bootstrapped difference tests were used to compare the centrality values of the EDE items highest and lowest in strength, closeness, and betweenness, respectively.
To assess the stability of the centrality indices, bootstrapping tests were performed whereby the values of the three centrality indices were re-estimated after reducing the number of participants by up to 60% of the original sample, and then compared with the original values obtained in the full sample using correlations (Epskamp, Borsboom, & Fried, 2017). As a validation check, a series of generalized linear models were conducted using EDE items with the highest centrality to predict depressive symptoms, self-esteem, and psychiatric comorbidity (one or more versus no comorbid diagnoses). A separate model was conducted for each clinical validator.
The overall connectivity of the networks, which describes the global strength of the entire network (to use the lay example, how tight the overall friend group is, including both central and peripheral members), and is characterized by the weighted sum of the absolute connections, was determined for youth with AN, BN, or OSFED. The Network Comparison Test (NCT), a 2-tailed permutation test in which the difference between two groups (AN and BN; AN and OSFED; and BN and OSFED) was calculated 100,000 times for randomly regrouped individuals, was used to assess the difference in overall connectivity between networks of both diagnostic groups (van Borkulo et al., 2015). Permutation tests were used to assess differences between AN, BN and OSFED on centrality measures of individual EDE items (Ernst, 2004). Centrality measures were calculated for 1,000 permutated samples for randomly regrouped individuals, and p-values were derived from the permutated samples’ nodes centrality distributions. Due to the large number of tests, including strength, closeness, and betweenness comparisons for each of 28 EDE items, alpha was set at .001 to avoid inflation of Type I error.
Results
Full Sample
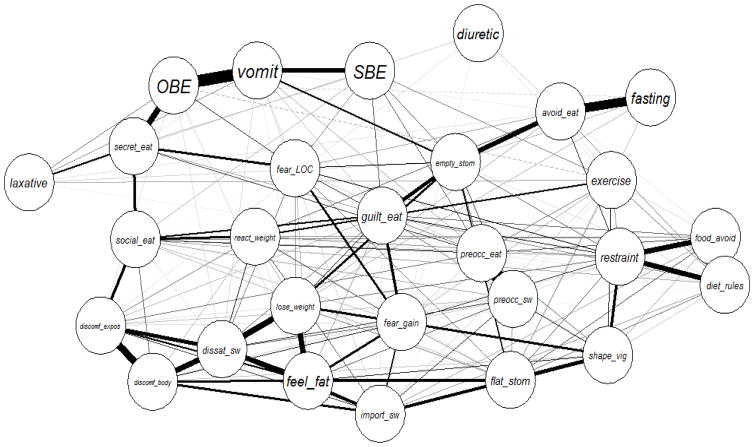
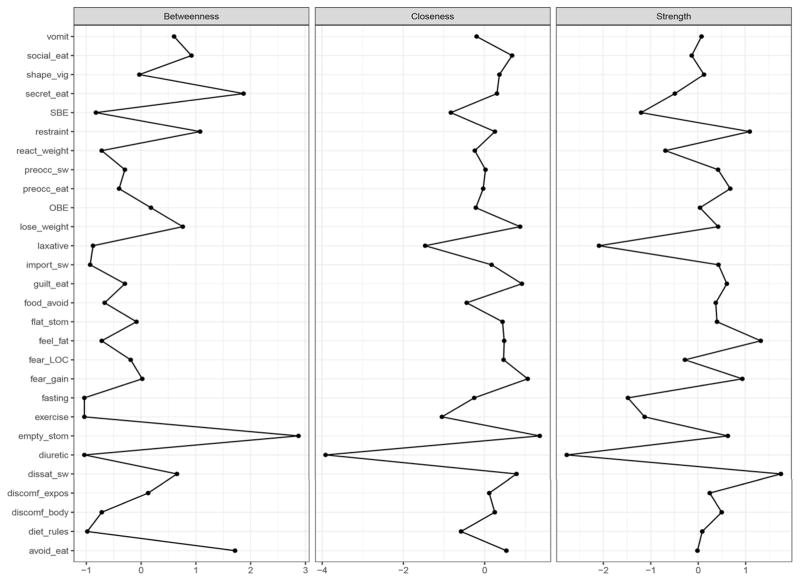
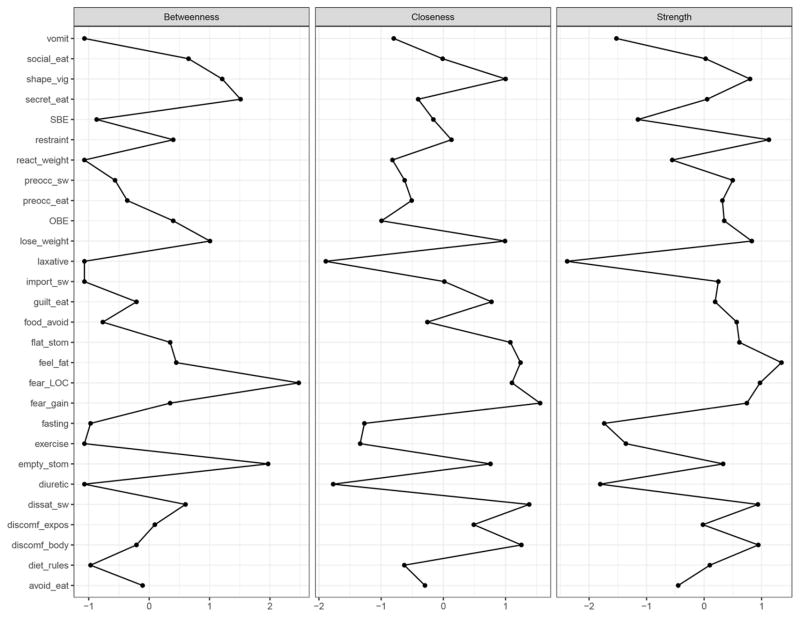
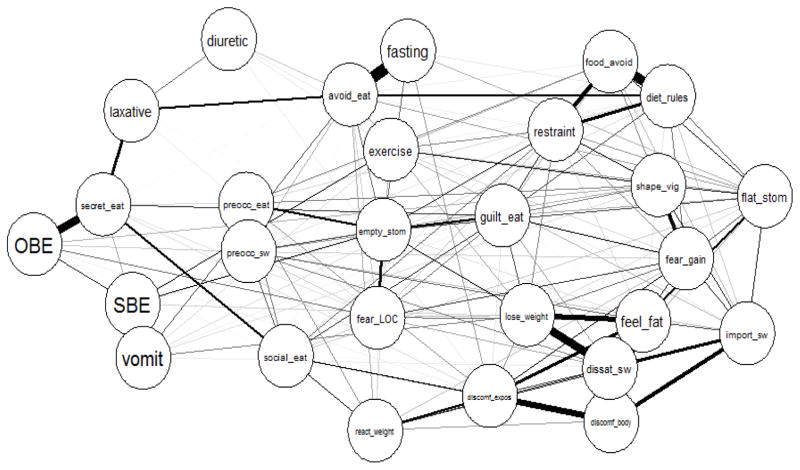
As illustrated in Figures 1 and 2, EDE items with the highest strength (i.e., those most strongly associated with other eating disorder symptoms in the network) included dissatisfaction with shape/weight, feelings of fatness, restraint over eating, fear of weight gain, and empty stomach. These items were significantly associated with depressive symptoms, self-esteem, and presence of a comorbid psychiatric disorder (all p<.001). Items with the highest closeness centrality (i.e., those located more toward the center of the network with shorter geometric distances to and from other symptoms) included empty stomach, fear of weight gain, guilt about eating, desire to lose weight, and dissatisfaction with shape/weight. Finally, items with the highest betweenness centrality (i.e., those most often emerging as “bridge” symptoms that connect other nodes in the network) included empty stomach, eating in secret, avoidance of eating, restraint over eating, and social eating. There were significant differences in the centrality values of EDE items highest and lowest in strength (dissatisfaction with shape/weight and diuretic use, respectively; 95% confidence interval=−1.3474 to −0.6525), closeness (empty stomach and diuretic use, respectively; 95% confidence interval=−0.0017 to −0.0001), and betweenness (empty stomach and diuretic use, respectively; 95% confidence intervals=−181.9500 to −44.0000), as reflected in the confidence intervals not containing zero. Bootstrapping tests for each centrality index are depicted in Figure 3, and illustrate that the strength index was the most stable of the centrality indices.
Figure 1.
Eating disorder symptom network in a transdiagnostic sample.
Note: Each node represents an item on the Eating Disorder Examination,1 and each link represents the zero-order correlation between each pair of items. Solid links indicate positive correlations, and dashed links indicate negative correlations. The thickness of a link represents the magnitude of the correlation.
Figure 2.
Centrality measures for eating disorder psychopathology network in the full sample
Note: See Footnote 1 for Eating Disorder Examination item (i.e., node) abbreviations.
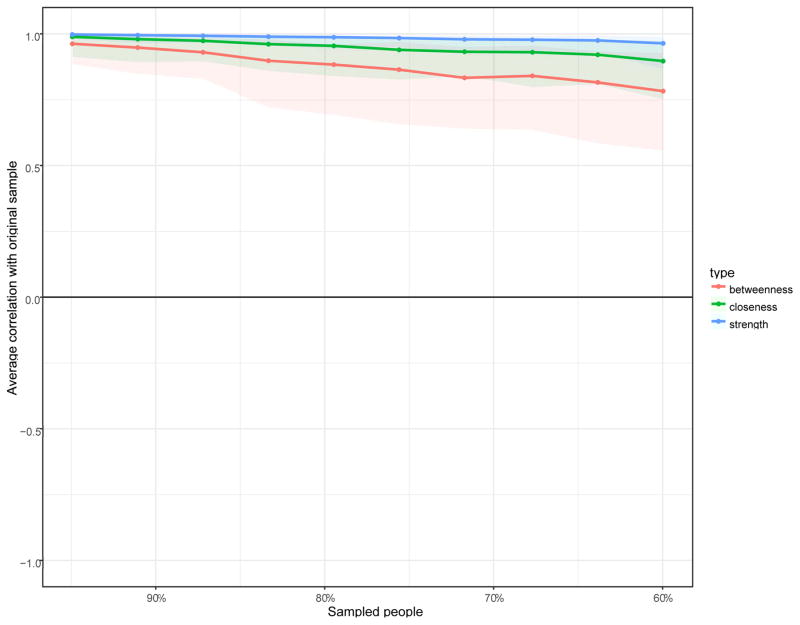
Figure 3.
Average correlations between centrality indices of networks sampled with persons dropped and the original sample.
Note: Lines indicate the means and areas indicate the range from the 2.5th quantile to the 97.5th quantile.
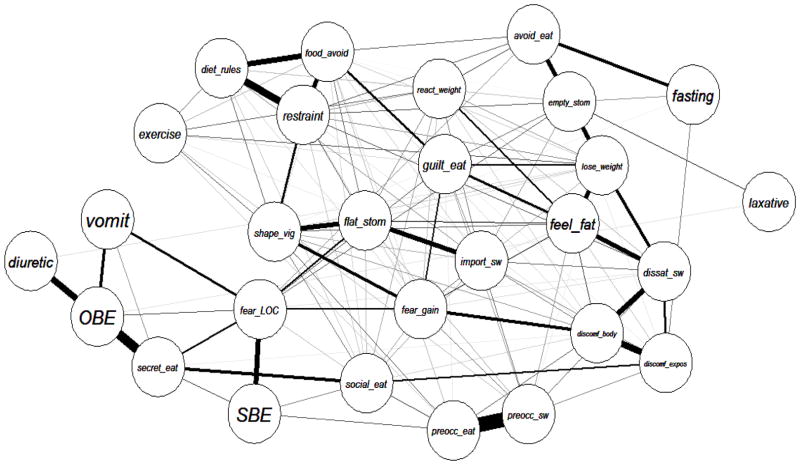
Diagnostic Subgroups
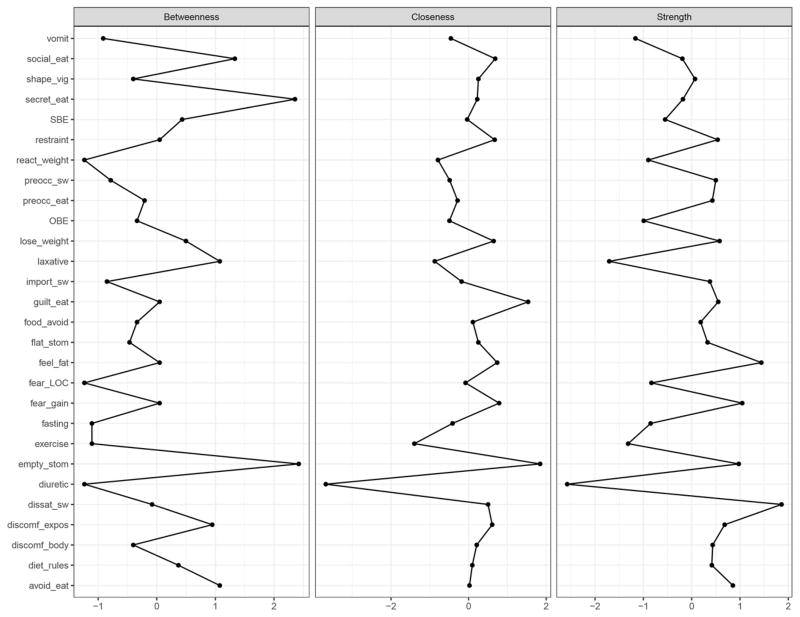
As illustrated in Figures 4 and 5, EDE items with the highest strength in AN included feelings of fatness, restraint over eating, fear of losing control over eating, discomfort seeing one’s body, and dissatisfaction with shape/weight. Items with the highest closeness centrality included fear of weight gain, dissatisfaction with shape/weight, discomfort seeing one’s body, feelings of fatness, and fear of losing control over eating. Finally, items with the highest betweenness centrality included fear of losing control over eating, empty stomach, eating in secret, vigilance about shape, and desire to lose weight.
Figure 4.
Eating disorder symptom network within individuals with anorexia nervosa.
Note: Each node represents an item on the Eating Disorder Examination,1 and each link represents the zero-order correlation between each pair of items. The thickness of a link represents the magnitude of the correlation.
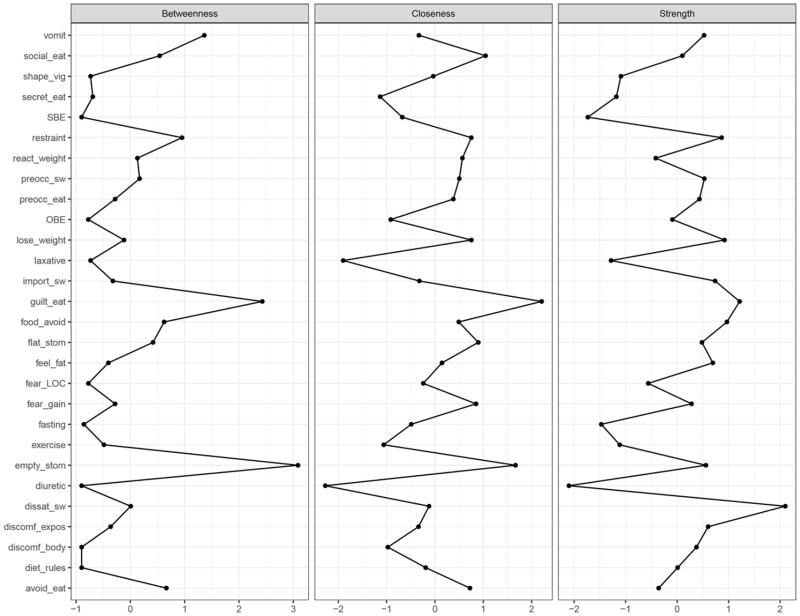
Figure 5.
Centrality measures for eating disorder psychopathology network in participants with anorexia nervosa
Note: See Footnote 1 for Eating Disorder Examination item (i.e., node) abbreviations.
As illustrated in Figures 6 and 7, EDE items with the highest strength in BN included dissatisfaction with shape/weight, guilt about eating, restraint over eating, desire to lose weight, and food avoidance. Items with the highest closeness centrality included restraint over eating, avoidance of eating, empty stomach, food avoidance, and dietary rules. Finally, items with the highest betweenness centrality included empty stomach, restraint over eating, guilt about eating, food avoidance, and avoidance of eating.
Figure 6.
Eating disorder symptom network within individuals with bulimia nervosa.
Note: Each node represents an item on the Eating Disorder Examination,1 and each link represents the zero-order correlation between each pair of items. Solid links indicate positive correlations, and dashed links indicate negative correlations. The thickness of a link represents the magnitude of the correlation.
Figure 7.
Centrality measures for eating disorder psychopathology network in participants with bulimia nervosa
Note: See Footnote 1 for Eating Disorder Examination item (i.e., node) abbreviations.
As illustrated in Figures 8 and 9, EDE items with the highest strength in OSFED included dissatisfaction with shape/weight, feelings of fatness, fear of weight gain, empty stomach, and avoidance of eating. Items with the highest closeness centrality included empty stomach, guilt about eating, fear of weight gain, feelings of fatness, and social eating. Finally, items with the highest betweenness centrality included empty stomach, eating in secret, social eating, avoidance of eating, and laxative misuse.
Figure 8.
Eating disorder symptom network within individuals with otherwise specified feeding or eating disorder.
Note: Each node represents an item on the Eating Disorder Examination (EDE),1 and each link represents the zero-order correlation between each pair of items. The thickness of a link represents the magnitude of the correlation.
Figure 9.
Centrality measures for eating disorder psychopathology network in participants with otherwise specified feeding or eating disorder
Note: See Footnote 1 for Eating Disorder Examination item (i.e., node) abbreviations.
The NCT test revealed that the overall connectivity of the networks did not significantly differ between those with AN and BN (p=.70), between those with AN and OSFED (p=.40), or between those with BN and OSFED (p=.70). Fear of losing control over eating (p=.001) and vigilance about shape (p<.001) had significantly larger strength indices for individuals with AN as compared to those with BN. Fear of losing control over eating had a significantly larger strength index for participants with AN as compared to those with OSFED (p<.001), and feelings of fatness had a significantly larger strength index for participants with OSFED as compared to those with BN (p<.001).
Fear of losing control over eating, flat stomach, fear of weight gain, dissatisfaction with shape/weight, discomfort seeing one’s body, feelings of fatness, and vigilance about shape had significantly larger closeness indices for individuals with AN relative to those with OSFED (all p<.001). There were no EDE items for which closeness significantly differed between participants with AN and BN, or between participants with BN and OSFED (all p>.001).
There were no EDE items for which betweenness significantly differed by diagnostic subgroup (p>.001).
Discussion
The aim of the current study was to investigate the transactional relationships among eating disorder symptoms within a transdiagnostic sample of children and adolescents seeking treatment for eating disorders. Overall, we found that shape- and weight-related concerns and dietary restraint played key roles in the psychopathology of eating disorders in youth. The overall connectivity of eating disorder networks did not differ between participants with AN, BN, and OSFED, and centrality measures of individual EDE items were largely similar across these subgroups, providing support for transdiagnostic theory. Future prospective studies should test whether the importance of individual nodes in the network fluctuates in relation to changes in diagnostic status, and how treatment impacts the eating disorder symptom network.
Previous research has suggested that the classification scheme for eating disorders is suboptimal, particularly for children and adolescents (Bravender et al., 2007), given high rates of diagnostic crossover (Allen et al., 2013; Stice et al., 2012) and similarities in clinical presentation (e.g., dietary restraint, binge eating and purging) across diagnostic subgroups (Goldschmidt et al., 2016; Peat, Mitchell, Hoek, & Wonderlich, 2009). The current findings indicate that the core features of eating disorders are similar across AN, BN, and OSFED subgroups, suggesting that a nosological scheme in which these are viewed as disparate disorders may not be ideal. Indeed, our findings support the use of broader, dimensional diagnostic schemes for eating disorders in children and adolescents, given the lack of significant differences between diagnostic subgroups in core eating disorder features. Future research is needed to determine whether dimensional approaches to nosology for eating disorders better predict treatment outcome and clinical impairment compared to categorically based diagnoses.
Overall, our findings support cognitive-behavioral theories of eating disorder onset and maintenance (Fairburn, 2008a) and have important clinical implications. Current cognitive-behavioral and family-based approaches for eating disorders focus on improving behavioral symptoms of eating disorders (e.g., normalizing eating patterns, reversing weight loss) early in treatment (Fairburn, 2008a; Lock, Le Grange, Agras, & Dare, 2001), while maladaptive cognitions and attitudes regarding shape and weight are typically addressed later in treatment. However, the centrality of restraint- and weight- and shape-related symptoms suggests that disrupting the overall connectivity among these distinct yet inter-related constructs may improve treatment outcome. For example, addressing the ways in which automatic negative thoughts about weight- and shape-related acutely impact one’s tendency or desire to engage in dieting behaviors, or engaging in body exposures activities, while simultaneously normalizing eating patterns, may exert stronger effects on the overall network of eating disorder psychopathology than the current sequential approach.
Importantly, binge eating and compensatory behaviors were strongly connected to one another but not to other symptoms in the network. This finding is consistent with previous research in adults (Forbush et al., 2016), and suggests that these behaviors are likely to perpetuate one another, in line with the cognitive-behavioral model (Fairburn, 2008b). Alternatively, binge eating and compensatory behaviors may be a reaction to other cognitions (e.g., overvaluation of shape and weight) or behaviors (e.g., prolonged restriction) in the network, rather than central to promoting or maintaining the eating disorder network. The lack of a strong connection between certain eating disorder behaviors and the remainder of the network suggests that simply breaking the binge-purge cycle may not significantly impact other eating-related cognitions and attitudes. Therefore, treatments that focus exclusively on interrupting binge eating and purging behaviors may not be sufficient to reduce other eating disorder psychopathology or sustain improvements over time, although dismantling studies are needed to more definitively address this possibility.
This study was marked by several strengths, including the large, diagnostically heterogeneous sample, and the use of a semi-structured interview with strong psychometric properties to characterize eating-related psychopathology. Moreover, the use of network analysis adds to the current literature on the classification of eating disorders in children and adolescents by describing, for the first time, the nature of inter-relationships among eating disorder symptoms both across and within diagnostic categories. The findings go beyond traditional approaches to classification, which generally attempt to characterize disorders at the population level, by identifying specific diagnostic features that are most central in maintaining the disorder and thus may be beneficial to target early in treatment.
Despite these strengths, several limitations warrant consideration. First, the prevalence of certain diagnostic categories, including BED and ARFID, was quite low, and the sample size for BN fell slightly below what has been recommended for network analysis (Fried & Cramer, in press). These constraints precluded the generation of networks within each eating disorder subgroup. Understanding how these subgroups are similar or distinct in terms of their overall networks and central features could be important in clarifying the nosology of pediatric eating disorders and highlighting treatment targets within specific subgroups. However, AN, BN, and OSFED have been observed to be the diagnostic subgroups that present most frequently for outpatient treatment (Ornstein et al., 2013), thus reducing concerns about the representativeness of this clinical sample. Related to the low frequency of BN diagnoses in our sample, missing data for the EDE item assessing dietary restriction outside of binge eating episodes (which is only administered to individuals who report recurrent binge eating) was substantial. Thus, future studies should evaluate how this item fits into networks of adolescent eating disorder symptoms. Second, findings were cross-sectional, which limits our ability to draw causal inferences. Therefore, the direction of influence among eating disorder symptoms in the network is unclear. Third, the sample was comprised exclusively of children and adolescents seeking treatment for eating disorders, and was predominantly female. Future research should assess whether eating disorder symptom networks differ between treatment-seeking and non-treatment seeking samples, or between males and females. Fourth, 28 EDE items were included in the network analysis, some of which were highly correlated and hence may reflect similar underlying constructs. Although the number of nodes included in our study is commensurate with that included in prior studies (Bringmann, Lemmens, Huibers, Borsboom, & Tuerlinckx, 2015; Forbush et al., 2016; McNally et al., 2014), future network analyses should consider more parsimonious methods for constructing eating disorder symptom networks (i.e., reducing the number of nodes). Finally, connections between symptoms may shift over time such that this network may not generalize to adults with eating disorders (although previous research in an adult sample produced similar findings; Forbush et al., 2016).
In summary, results suggested that among children and adolescents presenting for eating disorders treatment, dietary restraint and shape- and weight-related concerns play a key role in the psychopathology of eating disorders, which supports cognitive-behavioral theories of eating disorder onset and maintenance. Clinical interventions should seek to disrupt the strong connections among restraint- and appearance-related symptoms early in treatment so as to produce maximal treatment effects. Future research should further explore the optimal approach to organizing the eating disorders classification scheme in order to improve diagnosis and treatment for children and adolescents.
Supplementary Material
General Scientific Summary.
This study suggests that dietary restraint and appearance-related concerns are central in the psychopathology of pediatric eating disorders. Specific diagnostic subgroups, including anorexia nervosa, bulimia nervosa, and otherwise specific feeding or eating disorder, were largely similar in terms of their most central eating-related symptoms, suggesting that core features of eating disorders may be shared across diagnostic categorizations, consistent with a transdiagnostic approach to classification.
Acknowledgments
This work was supported by the National Institutes of Health grants K23 MH001923; R01 MH079979; R01 MH070620; and K23 DK105234). Parts of this manuscript were presented at the International Conference on Eating Disorders, June 8–10, 2017, Prague, Czech Republic.
Footnotes
The following 28 items from the Eating Disorder Examination (and their abbreviations, in parentheses) were included in each network analysis: restraint over eating (restraint); avoidance of eating (avoid_eat); empty stomach (empty_stom); food avoidance (food_avoid); dietary rules (diet_rules); preoccupation with food, eating, or calories (preocc_eat); fear of losing control over eating (fear_LOC); social eating (social_eat); guilt about eating (guilt_eat); eating in secret (secret_eat); flat stomach (flat_stom); preoccupation with shape or weight (preocc_sw); importance of shape and importance of weight, averaged (import_sw); fear of weight gain (fear_gain); dissatisfaction with shape and dissatisfaction with weight, averaged (dissat_sw); discomfort seeing body (discomf_body); discomfort about exposure (discomf_expos); feelings of fatness (feel_fat); reaction to prescribed weighing (react_weigh); desire to lose weight (lose_weight); vigilance about shape (shape_vig); objective binge eating (OBE); subjective binge eating (SBE); self-induced vomiting (vomit); laxative misuse (laxative); diuretic misuse (diuretic); driven exercising (exercise); fasting (fasting).
References
- Allen KL, Byrne SM, McLean NJ, Davis EA. Overconcern with weight and shape is not the same as body dissatisfaction: evidence from a prospective study of pre-adolescent boys and girls. Body Image. 2008;5(3):261–270. doi: 10.1016/j.bodyim.2008.03.005. [DOI] [PubMed] [Google Scholar]
- Allen KL, Byrne SM, Oddy WH, Crosby RD. DSM-IV-TR and DSM-5 eating disorders in adolescents: prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. J Abnorm Psychol. 2013;122(3):720–732. doi: 10.1037/a0034004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, D.C: 2013. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, Crow SJ. Psychometric evaluation of the eating disorder examination and eating disorder examination-questionnaire: A systematic review of the literature. Int J Eat Disord. 2012;45(3):428–438. doi: 10.1002/eat.20931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Bravender T, Bryant-Waugh R, Herzog D, Katzman D, Kreipe RD, Lask B, … Zucker N. Classification of child and adolescent eating disturbances. Workgroup for Classification of Eating Disorders in Children and Adolescents (WCEDCA) Int J Eat Disord. 2007;40(Suppl):S117–122. doi: 10.1002/eat.20458. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, Lemmens LH, Huibers MJ, Borsboom D, Tuerlinckx F. Revealing the dynamic network structure of the Beck Depression Inventory-II. Psychol Med. 2015;45(4):747–757. doi: 10.1017/s0033291714001809. [DOI] [PubMed] [Google Scholar]
- Curtiss J, Klemanski DH. Taxonicity and network structure of generalized anxiety disorder and major depressive disorder: An admixture analysis and complex network analysis. J Affect Disord. 2016;199:99–105. doi: 10.1016/j.jad.2016.04.007. [DOI] [PubMed] [Google Scholar]
- de Beurs D. Network Analysis: A Novel Approach to Understand Suicidal Behaviour. International Journal of Environmental Research and Public Health. 2017;14(3):219. [Google Scholar]
- Eddy KT, Celio Doyle A, Hoste RR, Herzog DB, Le Grange D. Eating disorder not otherwise specified in adolescents. J Am Acad Child Adolesc Psychiatry. 2008;47(2):156–164. doi: 10.1097/chi.0b013e31815cd9cf. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Le Grange D, Crosby RD, Hoste RR, Doyle AC, Smyth A, Herzog DB. Diagnostic classification of eating disorders in children and adolescents: how does DSM-IV-TR compare to empirically-derived categories? J Am Acad Child Adolesc Psychiatry. 2010;49(3):277–287. doi: 10.1016/j.jaac.2009.10.012. quiz 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. 2017 doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst MD. Permutation methods: A basis for exact inference. Statistical Science. 2004;19(4):676–685. [Google Scholar]
- Fairburn CG. Cognitive behavior therapy and eating disorders. New York, NY: Guilford Press; 2008a. [Google Scholar]
- Fairburn CG. Eating disorders: The transdiagnostic view and the cognitive behavioral theory. In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008b. pp. 7–22. [Google Scholar]
- Fairburn CG, Bohn K. Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM-IV. Behav Res Ther. 2005;43(6):691–701. doi: 10.1016/j.brat.2004.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. New York, NY: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Flament MF, Buchholz A, Henderson K, Obeid N, Maras D, Schubert N, … Goldfield G. Comparative distribution and validity of DSM-IV and DSM-5 diagnoses of eating disorders in adolescents from the community. Eur Eat Disord Rev. 2015;23(2):100–110. doi: 10.1002/erv.2339. [DOI] [PubMed] [Google Scholar]
- Forbush KT, Siew CS, Vitevitch MS. Application of network analysis to identify interactive systems of eating disorder psychopathology. Psychol Med. 2016;46(12):2667–2677. doi: 10.1017/s003329171600012x. [DOI] [PubMed] [Google Scholar]
- Fried EI, Cramer AOJ. Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science. doi: 10.1177/1745691617705892. in press. [DOI] [PubMed]
- Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psychiatry Psychiatr Epidemiol. 2016 doi: 10.1007/s00127-016-1319-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Accurso EC, O’Brien S, Fitzpatrick KK, Lock JD, Le Grange D. The importance of loss of control while eating in adolescents with purging disorder. Int J Eat Disord. 2016;49(8):801–804. doi: 10.1002/eat.22525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB, Wilfley DE, Eddy KT, Boutelle K, Zucker N, Peterson CB, … Le Grange D. Overvaluation of shape and weight among overweight children and adolescents with loss of control eating. Behav Res Ther. 2011;49(10):682–688. doi: 10.1016/j.brat.2011.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, … Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keel PK, Brown TA, Holland LA, Bodell LP. Empirical classification of eating disorders. Annu Rev Clin Psychol. 2012;8:381–404. doi: 10.1146/annurev-clinpsy-032511-143111. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Zerwas S, Calebs B, Forbush K, Kordy H, Watson H, … Bulik CM. The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. J Abnorm Psychol. 2017;126(3):340–354. doi: 10.1037/abn0000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lock J, Le Grange D, Agras WS, Dare C. Treatment manual for anorexia nervosa: A family-based approach. New York: The Guilford Press; 2001. [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, Borsboom D. Mental Disorders as Causal Systems. Clinical Psychological Science. 2014;3(6):836–849. doi: 10.1177/2167702614553230. [DOI] [Google Scholar]
- O’Brien A, Watson HJ, Hoiles KJ, Egan SJ, Anderson RA, Hamilton MJ, … McCormack J. Eating disorder examination: Factor structure and norms in a clinical female pediatric eating disorder sample. Int J Eat Disord. 2016;49(1):107–110. doi: 10.1002/eat.22478. [DOI] [PubMed] [Google Scholar]
- Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Social Networks. 2010;32:245–251. [Google Scholar]
- Ornstein RM, Rosen DS, Mammel KA, Callahan ST, Forman S, Jay MS, … Walsh BT. Distribution of eating disorders in children and adolescents using the proposed DSM-5 criteria for feeding and eating disorders. J Adolesc Health. 2013;53(2):303–305. doi: 10.1016/j.jadohealth.2013.03.025. [DOI] [PubMed] [Google Scholar]
- Peat C, Mitchell JE, Hoek HW, Wonderlich SA. Validity and utility of subtyping anorexia nervosa. Int J Eat Disord. 2009;42(7):590–594. doi: 10.1002/eat.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peebles R, Wilson JL, Lock JD. How do children with eating disorders differ from adolescents with eating disorders at initial evaluation? J Adolesc Health. 2006;39(6):800–805. doi: 10.1016/j.jadohealth.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, … Dunbar GC. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. Eur Psychiatry. 1997;12(5):232–241. doi: http://dx.doi.org/10.1016/S0924-9338(97)83297-X. [Google Scholar]
- Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. J Abnorm Psychol. 2012;122(2):445–457. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68(7):714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sysko R, Walsh BT. Does the broad categories for the diagnosis of eating disorders (BCD-ED) scheme reduce the frequency of eating disorder not otherwise specified? Int J Eat Disord. 2011;44(7):625–629. doi: 10.1002/eat.20860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabri N, Murray HB, Thomas JJ, Franko DL, Herzog DB, Eddy KT. Overvaluation of body shape/weight and engagement in non-compensatory weight-control behaviors in eating disorders: is there a reciprocal relationship? Psychol Med. 2015;45(14):2951–2958. doi: 10.1017/s0033291715000896. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord. 2009;42(1):26–30. doi: 10.1002/eat.20580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Borkulo C, Boschloo L, Borsboom D, Penninx BW, Waldorp LJ, Schoevers RA. Association of Symptom Network Structure With the Course of [corrected] Depression. JAMA Psychiatry. 2015;72(12):1219–1226. doi: 10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- Vo M, Accurso EC, Goldschmidt AB, Le Grange D. The impact of DSM-5 on eating disorder diagnoses. Int J Eat Disord. 2016 doi: 10.1002/eat.22628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TD, Byrne S, Bryant-Waugh R. The eating disorder examination: norms and construct validity with young and middle adolescent girls. Int J Eat Disord. 2008;41(6):551–558. doi: 10.1002/eat.20526. [DOI] [PubMed] [Google Scholar]
- Walker T, Watson HJ, Leach DJ, McCormack J, Tobias K, Hamilton MJ, Forbes DA. Comparative study of children and adolescents referred for eating disorder treatment at a specialist tertiary setting. Int J Eat Disord. 2014;47(1):47–53. doi: 10.1002/eat.22201. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG. Using the eating disorder examination to identify the specific psychopathology of binge eating disorder. Int J Eat Disord. 2000;27(3):259–269. doi: 10.1002/(sici)1098-108x(200004)27:3<259::aid-eat2>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.