Abstract
Anterior cruciate ligament (ACL) tears are an unfortunate and devastating injury in the athletic patient. Surgical reconstruction of the ACL with a taut graft construct is necessary to restore knee stability and help expedite the patient's return to an active lifestyle. Arthroscopy-assisted ACL reconstruction can be a technically involved procedure, where strong fixation limits graft motion to allow sufficient healing within the tibial and femoral tunnels at the bone-tendon interfaces. Loss of tension in a graft can cause symptomatic anterior or rotatory instability and potential retear of the ACL graft. We describe in this Technical Note and accompanying video a simple and effective technique to implant and retension a tendon graft during ACL reconstruction using a suspensory fixation device. The technical description uses a simple adjustable-loop device to provide strong cortical fixation, along with the unique ability to retension the graft in ACL reconstruction, not otherwise possible with previously described graft fixation techniques.
Injuries to the anterior cruciate ligament (ACL) are commonly encountered in athletic patients that participate in pivot sports.1, 2 The mechanism of injury for an ACL rupture occurs with noncontact twisting or pivoting on a knee that is fully extended. Approximately 200,000 ACL injuries occur in the United States each year.3 Of those injuries, as many as 125,000 will require surgical treatment.4 ACL reconstruction is indicated in active patients, with the goal to (1) restore knee stability by preventing anterior translation of the tibia relative to the femur and (2) limit tibial rotation.5 A knee with chronic ACL deficiency is at risk for developing subsequent meniscal and chondral injuries.6
The principal goal with every ACL reconstruction is to provide a stable initial graft fixation to allow tendon-to-bone healing and incorporation within the tibial and femoral tunnels.7 The modern era of arthroscopy-assisted ACL reconstruction has seen the emergence of several graft fixation techniques and devices available to the orthopaedic surgeon. Common graft fixation options include the use of interference screws and suspensory fixation devices, each with variable dependability and simplicity of use.8 The desired surgical end-product with any fixation device remains a taut ACL graft.9 However, the ability to retension the tendon graft after fixation is a unique technical feature not afforded by all fixation devices. The purpose of this Technical Note and accompanying video (Video 1) is to describe a straightforward technique to easily pass and retension a tendon graft following tibial fixation in ACL reconstruction using an adjustable suture loop and button device.
Surgical Technique
Preoperative Evaluation
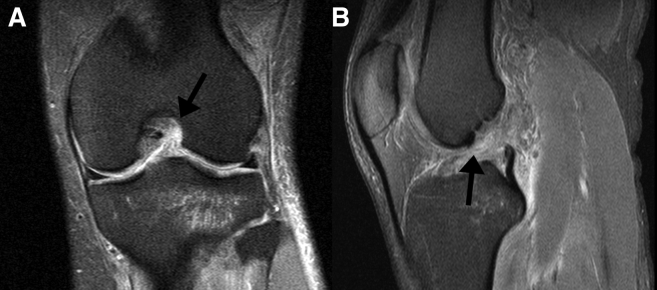
The diagnosis of an ACL tear is determined using a combination of the patient history, clinical examination, and medical imaging. The history is typically that of an athletic patient who sustains either a traumatic contact injury or a noncontact pivoting injury during a rapid acceleration or deceleration with change in direction. Patients with an ACL tear will present with a swollen and painful knee with difficulty bearing weight on the affected extremity. Lachman and anterior drawer tests are often positive, indicating an ACL-deficient knee. Radiographs of the knee are typically normal but may reveal a bony avulsion Segond fracture. Diagnosis is confirmed using advanced imaging such as magnetic resonance imaging, which will show ligament disruption and other associated meniscus or osteochondral injuries (Fig 1).
Fig 1.
Preoperative (A) coronal and (B) sagittal magnetic resonance imaging slices of the left knee showing a torn anterior cruciate ligament (black arrows) with fiber discontinuity.
Patient Setup
The patient is placed into the supine position on a standard operative table with an arthroscopic lateral stress post, and anesthetized using general anesthesia. A tourniquet is applied around the proximal thigh to minimize blood loss and maximize visualization. The operative leg is prepared proximally from the foot to the midthigh below the tourniquet, and is draped in a sterile fashion.
Arthroscopic Portal Placement
Standard knee arthroscopy is performed using a 30° 4.0-mm arthroscope. To establish the anterolateral portal, a vertical incision is made using a No. 11 blade, hugging the border of the lateral patellar tendon at the level of the inferior pole of the patella. The knee is then entered with a blunt trocar and scope sheath, and these are gently guided up to the suprapatellar pouch. A complete diagnostic arthroscopy is performed, inspecting for chondral damage, loose bodies, and meniscus tears. A spinal needle is used to localize the working anteromedial portal under arthroscopic visualization, and an incision is made in the same vertical fashion.
ACL Graft Preparation, Socket Placement, and Femoral Fixation
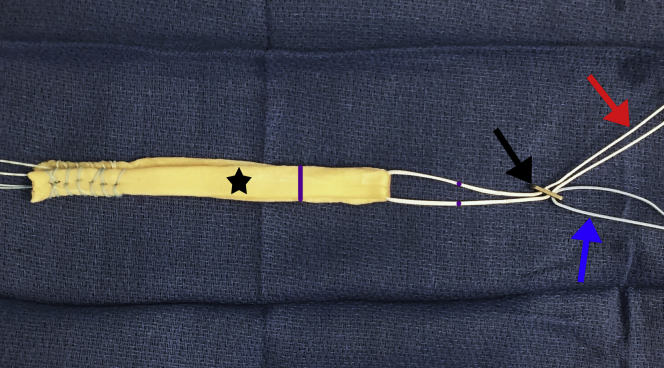
An appropriately sized autograft or allograft tendon (SpeedGraft, JRF Ortho, Centennial, CO) and ACL TightRope RT (Arthrex, Naples, FL) are prepared on the operating room back-table. The graft is folded in half over a No. 2 FiberWire suture strand (Arthrex) and trialed through a graft sizing block to measure the graft diameter and ensure proper fit. Autograft diameter is a minimum of 8.0 mm and maximum of 10.0 mm. The graft is then looped in half through the TightRope RT (Fig 2). A 3-mm, 90° radiofrequency ablation wand and 4-0 shaver are used to debride the femoral and tibial ACL footprints. An over-the-top ACL guide (Arthrex) is used to aim a spade-tip drill pin (Arthrex) at the desired location in the femoral ACL footprint. The knee is hyperflexed, and the drill pin with an open eyelet is advanced and exits the lateral femoral cortex. Condylar width is measured by pulling back on the spade-tip pin and reading the measurement on the pin in the notch. After measurement, the pin is advanced though the thigh skin and secured. A low-profile reamer (Arthrex) is then used to ream an appropriate depth socket. A suture is passed through the eyelet of the drill pin and then shuttled through the femoral socket. The knee is then extended to 90°, and a tibial drill guide (Arthrex), set to 55°, is placed through the medial portal. A 1.5-cm incision is made medial and distal to the tibial tubercle, and a drill pin is advanced to exit the posterior aspect of the anterior horn of the lateral meniscus. The femoral socket is then drilled equal to the diameter of the graft, using the pin as a guide.
Fig 2.
The presutured allograft tendon (star) with the adjustable-loop and button device (black arrow). The graft construct is advanced through the tibial tunnel by pulling on the blue passing suture (blue arrow) and advanced into the femoral tunnel by individually pulling on the white tensioning strands (red arrow) one at a time in alternate. The purple line of the TightRope is the width of the measured femoral condyle. The purple line on the graft is the width of the femoral socket with 5 mm subtracted.
ACL Graft Passage and Tibial Fixation
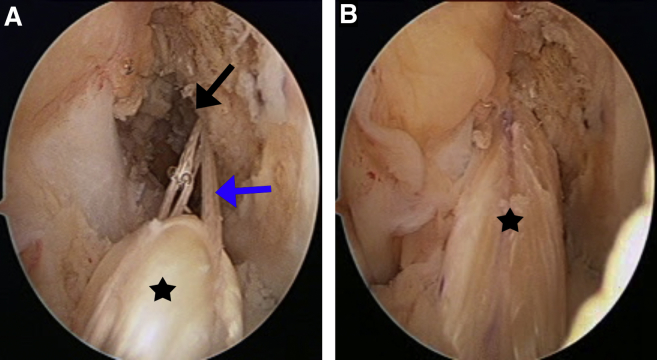
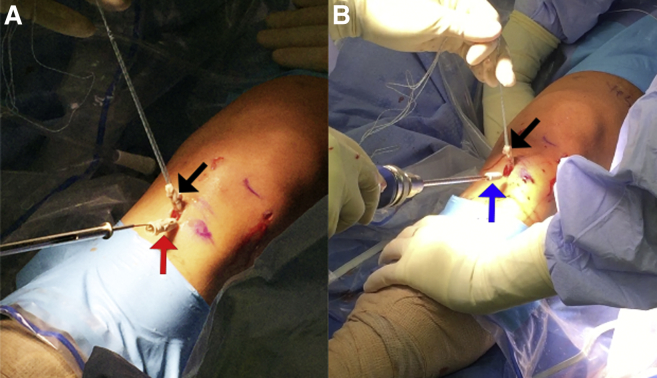
Prior to passage of the graft and Tightrope, the lateral condylar width measured is marked from the button to indicate when the button should flip on the cortex (Fig 2). The measured femoral socket depth should be marked on the graft minus 5 mm (Fig 2). This marking indicates when the graft has sunk into the socket 5 mm short of the socket terminus. The passing suture is used to pass the TightRope sutures and TightRope button through the tibial tunnel and the femoral socket. Under arthroscopic visualization through the anteromedial portal, the TightRope button is advanced through the femoral tunnel. Tension on the tibial end of the graft, while advancing the graft, should be maintained until the button has exited onto the lateral femoral cortex. Sterile mini-fluoroscopy is used to confirm that the button is flush on the lateral femoral cortex. To advance or “dunk” the graft into the femoral socket, each of the white tensioning sutures are pulled, alternating both sides (Fig 3). This is done until the graft has dunked to the graft marking, which leaves the graft approximately 5 mm short of the proximal femoral socket terminus, which remains for final tensioning of the graft (Fig 4). The knee is then cycled approximately 20 times to remove graft creep. With the knee in 20° of flexion and a constant posterior drawer force applied to the knee, the tibial tunnel is increasingly dilated, using a GraftBolt dilator (Arthrex), until a tight fit is achieved. A GraftBolt sheath and screw (Arthrex) is selected, typically of equal diameter to the final dilator. While maintaining constant tension on the tibial tails of the graft and with an applied posterior drawer, the sheath is impacted into the tibial tunnel at the level of the anterior tibial cortex, using the aid of a guidewire (Fig 5A). The screw is then inserted into the sheath and tightened using a driver until it is fully seated (Fig 5B).
Fig 3.
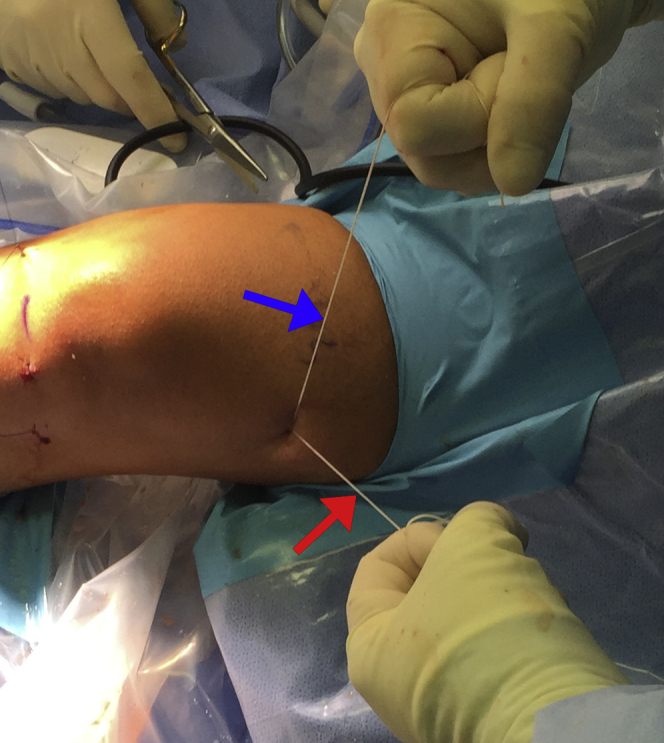
Intraoperative photograph showing the surgeon advance and tension the graft by alternating tension between the left (red arrow) and right (blue arrow) tensioning suture strands.
Fig 4.
Intraoperative arthroscopic views of the left knee viewed from the anterolateral portal. (A) The anterior cruciate ligament graft (star) is advanced into the femoral tunnel (black arrow) by pulling on the tensioning sutures (blue arrow). (B) The anterior cruciate ligament graft (star) is near fully seated in the femoral tunnel with approximately 5 mm of tunnel remaining for final tensioning.
Fig 5.
Intraoperative photographs showing graft laxity following tibial fixation with the (A) insertion of the interference sheath (red arrow) and (B) screw (blue arrow) into the tibial tunnel. Tension is maintained on the tibial tails of the ACL graft (black arrows). (ACL, anterior cruciate ligament.)
Performing the ACL Graft Retensioning Technique
Once tibial fixation has been completed, the knee is again cycled 20 times to remove residual graft creep. The ACL graft is re-examined under direct arthroscopic visualization and probed to evaluate laxity (Fig 6A). The technical pearl is to again pull on the white tensioning strands, one at a time. Alternating between both strands retensions the ACL graft and ensures that it is taut and fully seated in the femoral socket (Fig 6B). The ACL is examined in flexion and extension to determine the presence of femoral notch impingement. The ACL is again probed to ensure the graft is taut in flexion and extension. The tails of the graft are again pulled. Movement of the ACL and tibia together illustrates a strong femoral fixation. The blue passing suture is unloaded from the button and the white tensioning strands are cut below the skin surface.
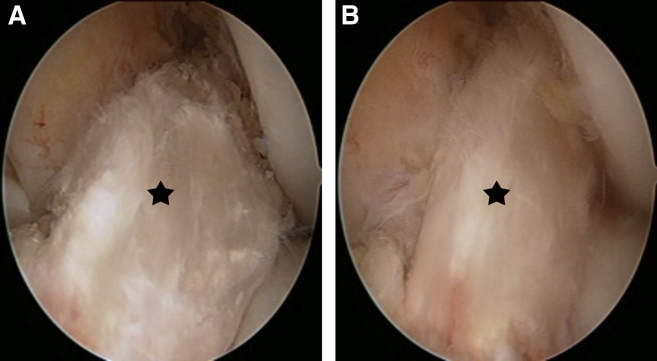
Fig 6.
Intraoperative arthroscopic views of the left knee viewed from the anterolateral portal. (A) The anterior cruciate ligament graft (star) shows laxity following tibial fixation. (B) The anterior cruciate ligament graft (star) is then retensioned until taut.
Final Examination and Postoperative Care
Lachman and pivot shift tests are performed to examine knee stability. A final intraoperative radiograph of the distal femur and proximal tibia is taken to ensure the ACL button sits flush on the lateral femoral cortex (Fig 7), and there is an adequate tibial tunnel trajectory. The excess ACL graft is then excised so that it is flush with the tibial tunnel cortex. The wounds are then irrigated and closed in the standard fashion. The knee is placed in a functional brace locked in extension. The brace is worn for a total of 6 weeks postoperatively, and held in extension immediately after surgery. The brace is unlocked to a maximum 90° of knee flexion with gradual increased range of motion over the next 48 to 72 hours postoperatively.
Fig 7.
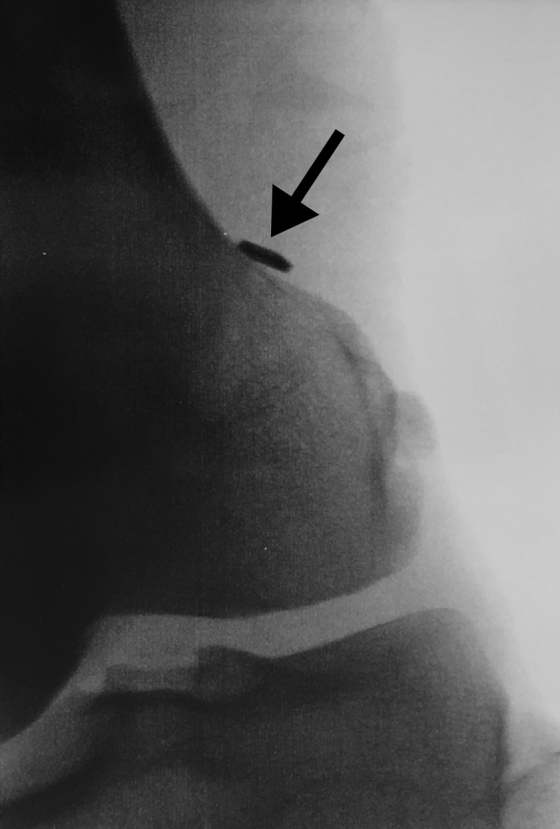
Final intraoperative anteroposterior radiograph of the left knee confirming correct placement of the button (arrow) and sitting flush on the lateral femoral cortex.
Discussion
A tensioned ACL tendon graft at the end of ligament reconstruction is essential to improve knee stability and patient outcomes, particularly during the critical tendon-to-bone healing period postoperatively.7, 10 Inadequate fixation and laxity within the ACL construct is an undesirable result that can lead to graft failure or knee instability. An unstable knee can lead to further chondral, meniscal, or ligamentous injuries.6 One of the inherent problems with ACL reconstruction and the use of interference screws is the loss of graft tension during fixation.11 Advancement of the sheath and interference screw into the tibial tunnel may cause proximal advancement of the ACL graft and subsequent loss of graft tension (Table 1). Loss of tension occurs despite efforts by the surgeon to minimize this, such as with maximum manual tension or a force-controlled device. A posterior drawer is also applied to the operative knee by a surgical assistant. Despite these efforts, there is loss of graft pretension and graft elongation even before the patient begins cycling the knee during postoperative rehabilitation. The ability of an adjustable-loop fixation device to retension the graft is what makes this such a valuable technique, and allows for improved knee stability until sufficient healing has occurred. The retensioning technique is accomplished by pulling on the tensioning sutures of the TightRope device, thereby removing graft laxity, resulting in a tight ACL construct.
Table 1.
Advantages and Disadvantages of the ACL Adjustable-Loop Fixation Technique
| Advantages |
| The expanding flaps of the GraftBolt sheath within the tibial tunnel and interference screw provides a strong tibial graft fixation. |
| Alternating between both of the white tensioning suture strands retensions the ACL graft and ensures a taut construct, with the graft fully seated within the femoral tunnel. |
| The ability to retension the graft after definitive tibial fixation may eliminate the need for a posterior drawer force on the knee during tibial sheath and interference screw insertion. |
| There is a low risk of wound healing complications given the small incisions required for this ACL reconstruction technique. |
| Disadvantages |
| Graft tension is lost after interference screw fixation by advancing the graft further into the tibial tunnel. This occurs even with strong countertraction on the tibial tails of the graft. |
ACL, anterior cruciate ligament.
There is consensus within the literature that cortical suspension constructs, both adjustable-loop and fixed-loop, have been shown to have high failure strengths and stiffness necessary for fixation of the graft within the femoral tunnel during ACL reconstruction.12 Unlike a fixed-loop device, the use of an adjustable-loop fixation device brings with it concerns of loop slippage and elongation with cyclic loading of the knee during postoperative rehabilitation.13 Petre et al.14 noted that adjustable-loop devices do have an increase in elongation with extended cyclic loading. The study authors reported 1.1 mm of elongation after 1,000 cycles of cyclic loading between 50 and 250 N. However, because the device is adjustable, the loop can be retensioned to remove that dynamic elongation. A closed or fixed-loop device is not dynamic, and therefore cannot retension the graft to the pretensioned state after tibial fixation.
Even with graft retensioning after tibial fixation using an adjustable-loop device like the TightRope RT, there is concern that loss of graft tension may again occur during the postoperative period with cyclic knee loading. Noonan et al.10 performed a cadaveric biomechanical study of retensioning using an adjustable-loop device with and without knot tying. Their technique reported an increase in construct elongation with extended cyclic loading in adjustable-loop devices that was reduced up to 80 percent by retensioning and knot tying compared with retensioning alone. However, their retensioning technique consisted of seating the graft into the socket terminus, performing cyclic loading, and then retensioning the graft by pulling on the tensioning sutures. In contrast, our described technique of leaving the graft 5 mm short of femoral socket terminus allows for space in the socket for retensioning to advance the graft further into the femoral socket. Their results suggest that graft retensioning removes graft laxity, and that knot tying is the optimal method to prevent additional loop slippage after retensioning.
The principal advantage of the retensioning technique using the TightRope RT adjustable-loop device in ACL reconstruction use the ability to retension the graft after tibial fixation (Table 2). A taut ACL construct is crucial during postoperative rehabilitation to reduce the risk of knee instability and re-rupture of the ACL graft. We conclude that the graft tensioning technique described here is both a simple and effective approach to minimize graft laxity, and thereby leave a snug ACL construct. In addition, retensioning of the graft after tibial fixation may eliminate the need for a posterior drawer on the knee, as the resulting laxity will be removed with retensioning. The potential of knot-tying to limit the loss of tension with loop slippage after graft retensioning is quite promising, and should be considered by the performing surgeon as an additional measure to ensure a lasting tight ACL construct for the patient.
Table 2.
Pearls and Pitfalls for the ACL Adjustable-Loop Fixation Technique
| Pearls |
| Maintain a forceful constant distal traction on the tibial tails of the graft during graft advancement to prevent the button from rapidly exiting the femoral socket and through the iliotibial band. Not doing so will prevent the button from sitting flush on the lateral femoral cortex. |
| Cycle the knee twice: (1) after advancing the graft into the knee and once the button sits flush on the lateral tibial cortex; and (2) after the tibial interference screw is tightened and fully seated within the sheath. |
| Leave the graft 5 mm short of the femoral socket terminus to allow for space in the socket for retensioning. |
| Use the aid of a guidewire when inserting and tightening the screw into the GraftBolt sheath. |
| After graft retensioning, consider knot tying of the white tensioning sutures to limit potential loop slippage that may occur with cyclic loading of the knee during postoperative rehabilitation. |
| Pitfalls |
| The cortical suspensory button may not sit flush on the lateral femoral cortex if it is accidentally advanced outside of the femoral socket and into surrounding soft tissues, such as the iliotibial band. |
| Failure to sufficiently retension the graft construct. Use Kelly clamps to pull forcefully on the white tensioning sutures after tibial fixation has been achieved to remove graft laxity and ensure the graft is tight in flexion and extension. |
ACL, anterior cruciate ligament.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.C. receives payment for lectures including service on speakers bureaus from Arthrex Medical Education. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
The investigation was performed at Advanced Orthopaedics & Sports Medicine, San Francisco, California, U.S.A.
Supplementary Data
Technique for tendon graft retensioning after implantation using an adjustable-loop fixation device in arthroscopic anterior cruciate ligament reconstruction. The video begins with sagittal and coronal views of a left knee magnetic resonance imaging showing an ACL tear with fiber discontinuity. The tendon allograft and adjustable-loop fixation device are then shown, illustrating correct assembly of the construct in the operating room prior to implantation. The blue passing suture is used to advance the ACL button and tendon construct through the femoral tunnel. To advance the graft, each of the white tensioning sutures are pulled, alternating both sides. This is done until approximately 5 mm of the proximal femoral socket remains, which is used for final tensioning of the graft. The knee is then cycled to remove graft creep. With the knee in slight flexion and a constant posterior drawer force applied to the knee, the tibial tunnel is increasingly dilated until a tight fit is achieved. While maintaining constant tension on the tibial tails of the graft, and with an applied posterior drawer, the sheath is impacted into the tibial tunnel at the level of the anterior tibial cortex using the aid of a guidewire. The screw is then inserted into the sheath and tightened using a driver until it is fully seated. Once tibial fixation has been completed, the knee is again cycled 20 times to remove residual graft creep. The ACL graft is re-examined under direct arthroscopic visualization and probed to evaluate laxity. The white tensioning strands are again pulled in alternate one at a time. Alternating between both strands retensions the ACL graft and ensures that it is taut and fully seated in the femoral tunnel. The ACL is again probed to ensure the graft is taut in flexion and extension. A final anteroposterior intraoperative radiograph of the distal femur is obtained to ensure the ACL button sits flush on the lateral femoral cortex. (ACL, anterior cruciate ligament.)
References
- 1.Ralles S., Agel J., Obermeier M., Tompkins M. Incidence of secondary intra-articular injuries with time to anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:1373–1379. doi: 10.1177/0363546515574061. [DOI] [PubMed] [Google Scholar]
- 2.Lubowitz J.H., Appleby D. Cost-effectiveness analysis of the most common orthopaedic surgery procedures: Knee arthroscopy and knee anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2011;27:1317–1322. doi: 10.1016/j.arthro.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Mall N.A., Chalmers P.N., Moric M. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363–2370. doi: 10.1177/0363546514542796. [DOI] [PubMed] [Google Scholar]
- 4.Mehran N., Bedi A. A review of current graft options for anterior cruciate ligament reconstruction. JBJS Rev. 2015;3:1–11. doi: 10.2106/JBJS.RVW.O.00009. [DOI] [PubMed] [Google Scholar]
- 5.Hwang M.D., Piefer J.W., Lubowitz J.H. Anterior cruciate ligament tibial footprint anatomy: Systematic review of the 21st century literature. Arthroscopy. 2012;28:728–734. doi: 10.1016/j.arthro.2011.11.025. [DOI] [PubMed] [Google Scholar]
- 6.Lamblin C.J., Waterman B.R., Lubowitz J.H. Anterior cruciate ligament reconstruction with autografts compared with non-irradiated, non-chemically treated allografts. Arthroscopy. 2013;29:1113–1122. doi: 10.1016/j.arthro.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 7.Kruse L.M., Gray B., Wright R.W. Rehabilitation after anterior cruciate ligament reconstruction: A systematic review. J Bone Joint Surg Am. 2012;94:1737–1748. doi: 10.2106/JBJS.K.01246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lubowitz J.H., Schwartzberg R., Smith P. Cortical suspensory button versus aperture interference screw fixation for knee anterior cruciate ligament soft-tissue allograft: A prospective, randomized controlled trial. Arthroscopy. 2015;31:1733–1739. doi: 10.1016/j.arthro.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Koga H., Muneta T., Yagishita K. Effect of initial graft tension on knee stability and graft tension pattern in double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2015;31:1756–1763. doi: 10.1016/j.arthro.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Noonan B.C., Dines J.S., Allen A.A., Altchek D.W., Bedi A. Biomechanical evaluation of an adjustable loop suspensory anterior cruciate ligament reconstruction fixation device: The value of retensioning and knot tying. Arthroscopy. 2016;32:2050–2059. doi: 10.1016/j.arthro.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Stadelmaier D.M., Lowe W.R., Ilahi O.A., Noble P.C., Kohl H.W. Cyclic pull-out strength of hamstring tendon graft fixation with soft tissue interference screws. Influence of screw length. Am J Sports Med. 1999;27:778–783. doi: 10.1177/03635465990270061501. [DOI] [PubMed] [Google Scholar]
- 12.Milano G., Mulas P.D., Ziranu F., Piras S., Manunta A., Fabbriciani C. Comparison between different femoral fixation devices for ACL reconstruction with doubled hamstring tendon graft: A biomechanical analysis. Arthroscopy. 2006;22:660–668. doi: 10.1016/j.arthro.2006.04.082. [DOI] [PubMed] [Google Scholar]
- 13.Johnson J.S., Smith S.D., LaPrade C.M., Turnbull T.L., LaPrade R.F., Wijdicks C.A. A biomechanical comparison of femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction under high loads. Am J Sports Med. 2015;43:154–160. doi: 10.1177/0363546514553779. [DOI] [PubMed] [Google Scholar]
- 14.Petre B.M., Smith S.D., Jansson K.S. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:416–422. doi: 10.1177/0363546512469875. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for tendon graft retensioning after implantation using an adjustable-loop fixation device in arthroscopic anterior cruciate ligament reconstruction. The video begins with sagittal and coronal views of a left knee magnetic resonance imaging showing an ACL tear with fiber discontinuity. The tendon allograft and adjustable-loop fixation device are then shown, illustrating correct assembly of the construct in the operating room prior to implantation. The blue passing suture is used to advance the ACL button and tendon construct through the femoral tunnel. To advance the graft, each of the white tensioning sutures are pulled, alternating both sides. This is done until approximately 5 mm of the proximal femoral socket remains, which is used for final tensioning of the graft. The knee is then cycled to remove graft creep. With the knee in slight flexion and a constant posterior drawer force applied to the knee, the tibial tunnel is increasingly dilated until a tight fit is achieved. While maintaining constant tension on the tibial tails of the graft, and with an applied posterior drawer, the sheath is impacted into the tibial tunnel at the level of the anterior tibial cortex using the aid of a guidewire. The screw is then inserted into the sheath and tightened using a driver until it is fully seated. Once tibial fixation has been completed, the knee is again cycled 20 times to remove residual graft creep. The ACL graft is re-examined under direct arthroscopic visualization and probed to evaluate laxity. The white tensioning strands are again pulled in alternate one at a time. Alternating between both strands retensions the ACL graft and ensures that it is taut and fully seated in the femoral tunnel. The ACL is again probed to ensure the graft is taut in flexion and extension. A final anteroposterior intraoperative radiograph of the distal femur is obtained to ensure the ACL button sits flush on the lateral femoral cortex. (ACL, anterior cruciate ligament.)