Abstract
The management of multiligament knee injury is a complex process starting with the adequate identification of the injury. A detailed physical and radiographic examination with a thorough understanding of knee anatomy is crucial to assess all damaged structures: anterior cruciate ligament, posterior cruciate ligament, posteromedial corner including the medial collateral ligament, and posterolateral corner including the lateral collateral ligament. Several surgical techniques have been developed throughout the years to adequately address these ligament insufficiencies. In this surgical technique description, we describe a reproducible method for the assessment and surgical management of a knee dislocation (KDIV) injury. Our approach includes using anatomic single-bundle cruciate ligament reconstructions with modified Bosworth technique for medial-side injuries and a combination of Müller popliteal bypass and Larson figure-of-8 techniques for posterolateral corner injuries. The orders of surgical steps is described concisely, and technical controversies such as graft choice, tunnel positioning, and sequence of graft fixation are discussed in detail.
Multiple ligament injuries (MLIs) are rare but potentially disabling traumatic events that involve at least two of the 4 major ligaments of the knee (anterior cruciate ligament [ACL], posterior cruciate ligament [PCL], posteromedial corner [PMC] including the medial collateral ligament [MCL], and posterolateral corner [PLC] including the lateral collateral ligament [LCL]).1 The degree of ligament, other soft-tissue, and neurovascular injury occurs across a spectrum in patients with a traumatic knee dislocation of the knee, and management of such complex injuries requires a systematic approach. Although these injuries have been increasingly recognized over the past several years, there appears to be a lack of consensus among experts regarding how to treat multiple-ligament knee injuries.
A recent systematic review of the literature demonstrated that early operative treatment of MLI yields improved functional and clinical outcomes compared with nonoperation or delayed surgery.1 Numerous surgical protocols have been proposed for the treatment of these unusual injuries.2, 3, 4, 5, 6, 7, 8, 9 In recent years, surgery of the major ligaments of the knee has evolved toward an anatomically oriented reconstruction. However, with evolving surgical techniques, additional problems developed, including tunnel convergence, either on the lateral or medial side of the knee, involving cruciate and collateral ligament reconstructions.10, 11 Furthermore, with revision rates of multiligament injured knees nearing 9%, the importance of bone stock preservation for potential future surgeries cannot be overstated.3, 12
In this article, we describe our approach to multiligament knee injuries including the preferred techniques for lateral- and medial-sided reconstructions. Our general approach includes using a Müller popliteal bypass for the popliteus tendon, Larson figure-of-8 technique for LCL and popliteofibular ligament (PRL) reconstructions, and modified Bosworth technique for MCL reconstructions. The senior author (M.D.M.) developed this combined approach to particularly address tunnel convergence problems in the case of multiligament injured knees that usually require multiple tunnels placed in the femoral condyles and proximal tibia.
Technique
Physical Examination and Imaging
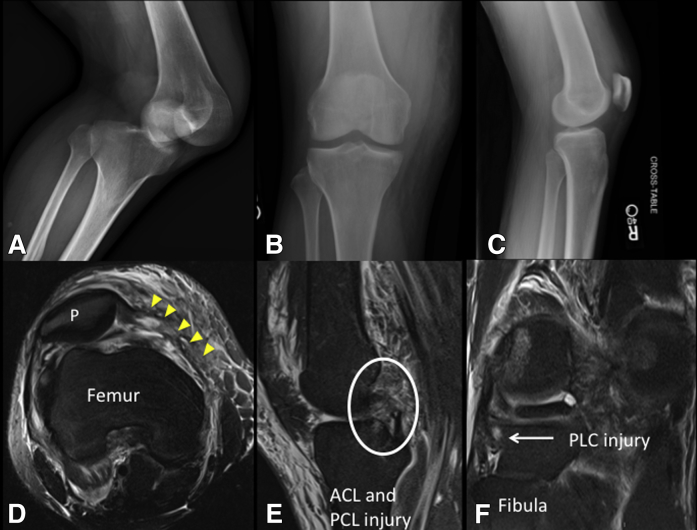
After life- and limb-threatening conditions are treated or excluded, attention is turned to characterizing the pattern and extent of ligamentous injury (Fig 1). Multiligament knee injuries involve injuries to at least 2 of 4 major ligamentous structures (ACL, PCL, PLC, and PMC), and knee dislocations generally involve injuries to at least 3 (Table 1).13 An examination under anesthesia (EUA) is always performed in the operating room as it confirms previous physical exam diagnoses and can provide an opportune time to obtain additional stress images of the knee with intraoperative C-Arm imaging. For patients who are unable to obtain preoperative stress radiographs to assess for combined PCL/PLC injuries or MCL injuries, the appropriate use of this EUA time cannot be overemphasized.
Fig 1.
First row: right knee radiographs. (A-C) Dislocated knee and immediate reduction anterior-posterior and lateral radiographs. Second row: right knee magnetic resonance images. (D) Axial image with yellow arrowheads reveals medial soft-tissue sleeve injury (medial collateral ligament, medial patellofemoral ligament, and medial retinaculum). (E) Sagittal image: bicruciate injury. (F) Sagittal image: posterolateral corner injury.
Table 1.
Knee Dislocation Classification System (Schenck et al.13)
| Type | Description |
|---|---|
| KD I | Knee dislocation with either ACL or PCL intact |
| KD II | Bicruciate injury with collaterals intact |
| KD III | Bicruciate injury with MCL or LCL intact
|
| KD IV | Bicruciate injury with both collaterals injured |
| KD V | Periarticular fracture dislocation |
NOTE. Subtypes include a (vascular) and n (neurologic) injury.
Assessment of the ACL is performed with the Lachman test and the pivot shift test. The Lachman test is essentially an anterior drawer test performed with the knee at 20° to 30° flexion. This test enables the surgeon to grade translation. In patients without an intact ACL, a soft endpoint and any difference in anterior translation between the injured and uninjured side should be indicative for ACL injury. A pivot shift test attempts to reproduce the rotary and transalatory instability in an ACL deficient knee by applying a combination of valgus force and axial load during a knee flexion from an extended position. With a positive pivot shift, the lateral tibial plateau subluxates anteriorly with internal rotation of tibia as the knee approaches full extension and then reduces as the knee flexes 30° to 40° secondary to the pull of the iliotibial band as it passes posterior to the axis of the knee. In the setting of MLIs, the pivot shift should be interpreted carefully, since injuries of the iliotibial band and medial side may alter the results of this test.
The PCL is examined by performing a posterior drawer test and observing the posterior sag test. The posterior drawer test is performed by adding a posterior directed force to proximal tibia with thumbs placed on the joint line, with the knee flexed at 90° and the foot stabilized in neutral rotation. A grade of 3 on posterior drawer testing and >12 mm of posterior tibial translation on stress radiography correlate with the presence of PLC injury in addition to a complete disruption of the PCL.14 The posterior sag test is performed when the patient lies supine and both knees are held at 90° of flexion to assess for loss of anterior tibial step-off, routinely appreciated as a 1-cm anterior tibial step-off in relation to the femoral condyles in an uninjured knee.
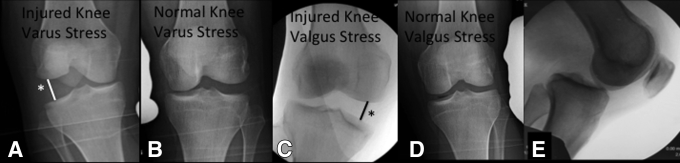
The MCL and LCL are examined with valgus and varus stress, respectively, at 30° flexion to isolate collateral ligaments. The routine assessment for >4 mm difference side-to-side comparison of the lateral and medial compartments at 20° to 30° of knee flexion with stress radiography is key15, 16 (Fig 2). Furthermore, valgus and varus laxity at full extension is suggestive for more severe injury. Excessive medial joint opening with valgus stress at full extension suggests posteromedial capsular injury and concomitant cruciate ligament injury.17 Likewise, excessive lateral joint opening at full extension is indicative for PLC and cruciate ligament injuries.18
Fig 2.
(A-D) Anterior-posterior images of injured right knee with marker compared to contralateral uninjured knee. Note the side-to-side difference under varus stress (A/B) and valgus stress (C/D). (E) Lateral injured right knee with posterior drawer test performed as exam under anesthesia. ∗Surgeons should confirm that the side-to-side difference is >4 mm.
The Slocum test is helpful to examine PMC injuries.19 The tibia is externally rotated 15° with the knee flexion at 90°, and the tibia is once pulled forward to determine the excessive anterior rotation of the medial tibial plateau. Asymmetric increased translation helps to identify injuries of posterior oblique ligament and posteromedial capsule.
The PLC is examined by performing posterolateral drawer and dial tests. The posterolateral drawer test is performed with the knee flexed 90° and the foot fixed in slight external rotation. With an isolated PLC injury, there will be more rotatory instability seen with slight external rotation than with neutral rotation because the PCL provides more translational stability with neutral rotation.20 The dial test is performed either in the supine or prone position. A maximal external rotation force is applied to both feet, and the foot-thigh angle is measured and compared with the other side at 30° and 90° flexion. External rotation difference greater than 15° is considered significant.21 Asymmetric increased external rotation indicates isolated injury of PLC if difference is observed at 30° only and not at 90°. In the senior author's experience, it can also mean that there is a PLC-ACL injury but not a concomitant PCL injury. Increased external rotation at both 30° and 90° of flexion indicates injury PLC and PCL (Table 2).
Table 2.
Physical Examination of Knee Ligament Injuries
| Structure: Test |
|---|
|
Magnetic resonance imaging (MRI) is a valuable tool to characterize ligament injuries after knee dislocation, as well as to identify extraligamentous or other soft-tissue knee injuries. However, it cannot demonstrate the functional consequences of ligament injuries, as it is a static study. Stress radiography offers the ability to obtain dynamic images to supplement MRI, providing an objective representation of the functional laxity resulting from ligament deficiency.22 In addition to preoperative assessment, stress radiography can be used to quantify and follow postoperative stability. At our institution, intraoperative stress radiographs are obtained on all patients to direct the reconstruction and repair of soft tissues.
Graft Selection/Preparation
Many times these cases require the use of an additional surgeon or physician's assistant given the time constraints that can be involved in a multiligament knee injury reconstruction. During routine graft preparation on the back table, we use ipsilateral hamstring (gracilis/semitendinosis) autograft for the ACL graft choice, bone patellar tendon bone (with occasional use of quadriceps tendon bone) for PCL reconstruction, and semitendinosis allografts for the PLC and MCL/PMC reconstructions. Soft-tissue allografts are prepared on the back table per routine locking Krackow whipstitches at each end of the graft with no. 2 fiberwire (Arthrex, Naples, FL). Our preferred techniques, grafts, and fixation for each structure are listed in Table 3.
Table 3.
Preferred Grafts and Techniques
| Structure | Preferred Technique | Graft | Fixation |
|---|---|---|---|
| ACL | Single-bundle anatomic reconstruction via independent tunnels | Quadrupled ipsilateral hamstring autograft | Tibia: interference screw/sheath. Femur: endobutton. |
| PCL | Single-bundle anatomic reconstruction via transtibial tunnel | Ipsilateral patella tendon autograft/ipsilateral quadriceps tendon autograft | Femur and tibia: interference screw |
| MCL/PMC | Primary repair + modified Bosworth or allograft reconstruction | Semitendinosus autograft (modified Bosworth) or semitendinosus allograft | Femur and tibia: screw and spiked washer |
| PLC/LCL | Primary repair + Larson figure-of-8 + Müller popliteal bypass | Hamstring allografts (2 or 3 tailed) | Femur (both grafts): screw and spiked washer. Tibia (Müller graft): interference screw/staple. Fibula (Larson graft): looped through tunnel. |
ACL, anterior cruciate ligament; LCL, lateral collateral ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner; PMC, posteromedial corner.
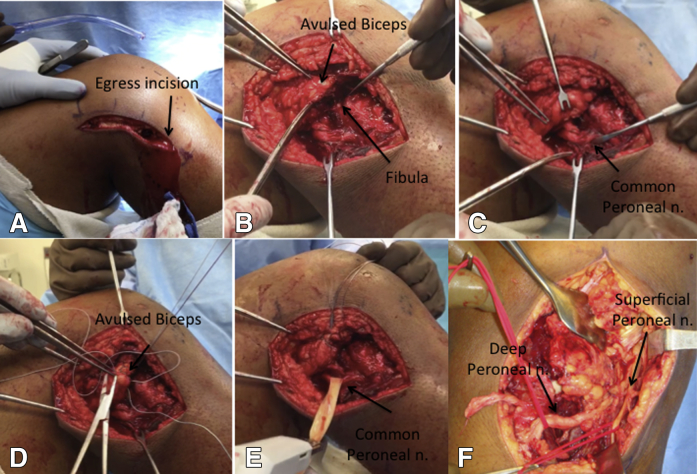
Lateral-Side Dissection
At the same time as the allograft preparation is performed, the lateral side of the knee dissection is performed with the lower extremity in an Alvarado limb positioner (Zimmer, Warsaw, IN). Palpating and marking Gerdy's tubercle and the fibular head, a 10-cm vertical incision is drawn out with the knee in full extension to ensure it is completely vertical in nature, midway between Gerdy's tubercle and the fibular head (Fig 3A). Satisfactory soft-tissue dissection is performed with layered development, and the incision is extended as needed. It is imperative to directly palpate the long head of the biceps as a constant landmark for the common peroneal nerve (CPN), given it is directly medial and posterior to the long head of the biceps. Three windows to the PLC of the knee are made as detailed by Laprade et al., either through this gross defect or through the injured tissue.18 The first window is oriented parallel to the fibers of the iliotibial tract, starting at the midpoint of Gerdy's tubercle, and extends proximally into the iliotibial tract. The second window is made between the posterior aspect of the iliotibial tract and the short head of the biceps femoris. The third window is made just posterior to the long head of the biceps femoris and is parallel to the CPN. There is usually a fascial reflection of the long head of the biceps that shields the CPN from direct visualization (Fig 3B). This fascia is split in line with the biceps. The CPN is routinely identified at this level or slightly higher given the more native, uninjured anatomy present there (Fig 3C). A Penrose drain is placed around the nerve and stapled onto itself (Fig 3E). A weighted clamp is never placed on the drain so as to not apply any significant tension to the nerve. In seriously injured cases, the iliotibial tract and biceps tendon are avulsed from insertion sites and may require repair (Fig 3D). It is important to note that the second window will many times communicate to capsular injuries and will serve as an egress incision to the main lateral approach during arthroscopy, which will lessen the risk of developing compartment syndrome. Great care is taken to dissect distally toward the fibular head to ensure no gross violation of the CPN, especially should the nerve split proximally into the superficial and deep components (Fig 3F). Many times, preoperative MRI can clearly identify the CPN, as well as identify whether there is a proximal split, any stretch or traction injury with resultant hematoma, or edema along its course. This can easily help identify the nerve as it approaches the fibular head. Once the lateral dissection is completed to satisfaction, for anticipated Larson and Müller PLC reconstructions, hamstring and bone patellar tendon bone autograft are harvested in standard fashion through a medial paramedian incision and prepared per the above technique. This incision allows access not only to graft harvest but also medial-sided reconstructions if indicated.
Fig 3.
Intraoperative images, right knee. (A) Lateral incision for posterolateral corner approach also used as an egress incision. (B) Avulsed biceps is dissected. (C) Peroneal nerve is dissected. (D) Biceps is secured with no. 2 fiber wire suture (Arthrex). (E) Peroneal nerve with a Penrose drain looped around it. (F) Intraoperative image, left knee showing common peroneal nerve split proximally into the superficial and deep branches.
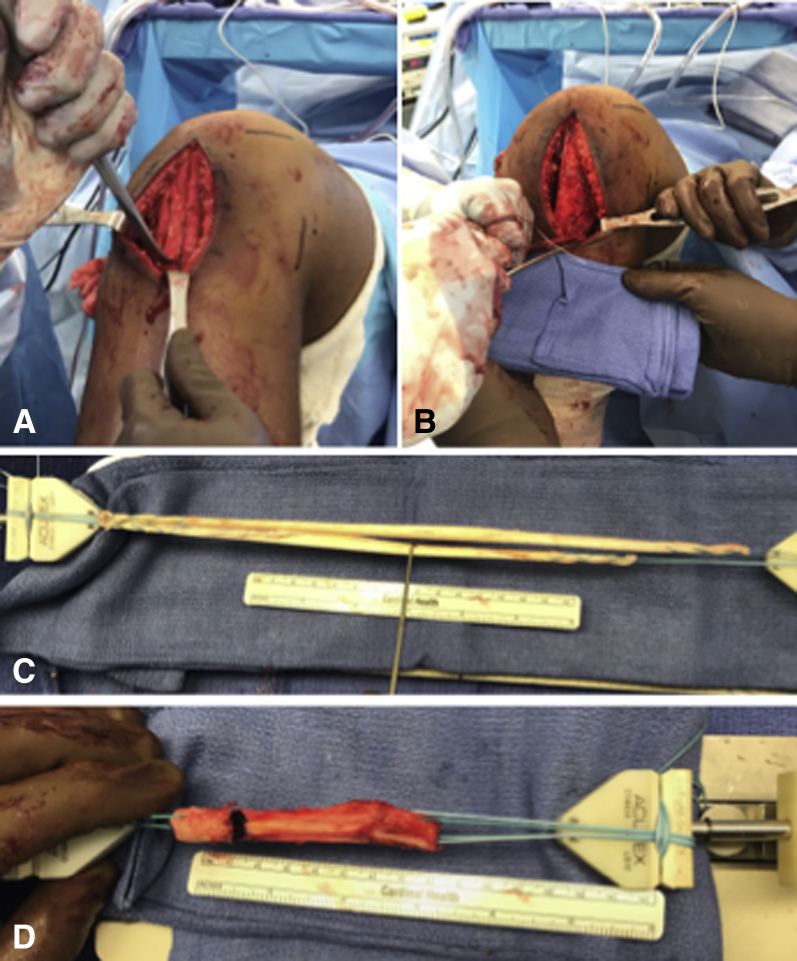
Autograft Harvest
Many times, a medial paramedian incision can be used to not only harvest the autografts but also to allow medial-sided exposure for required reconstructions for KDIIIM injuries (see Table 1 for the Schenk knee dislocation classification system13). However, we have found that for KDIV injuries, lateral, medial, and medial paramedian incisions are best used, with the latter providing exposure and access to autograft harvest. The patellar tendon bone autograft is harvested in standard fashion using a 1-cm oscillating saw to a size of a 22- to 25-mm bone segment (ensuring to not cross the midpatellar length) from both the patella and tibial tubercle. Alternatively, a quadriceps tendon bone autograft can be harvested as a 22- to 25-mm bone block with a 1-cm oscillating saw, still keeping it attached to the quadriceps tendon and harvested at a length of 6 to 7 cm. The bone blocks are fashioned and sized to a 9 to 10 mm graft with passing sutures passed into the bone block segment with a 1-mm drill. The gracilis/semitendinosis autograft tendons are then harvested in standard fashion and prepared on the back table in the above-listed manner for soft-tissue grafts (Fig 4).
Fig 4.
Intraoperative images, right knee. (A, B) Bone patellar tendon bone autograft harvest for posterior cruciate ligament graft and hamstring autograft harvest for ACL graft. (C) Hamstring allografts prepared for posterolateral corner and medial collateral ligament reconstructions. (D) Bone patellar tendon bone autograft preparation.
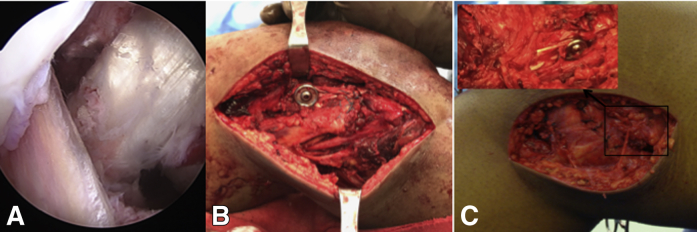
Diagnostic Knee Arthroscopy
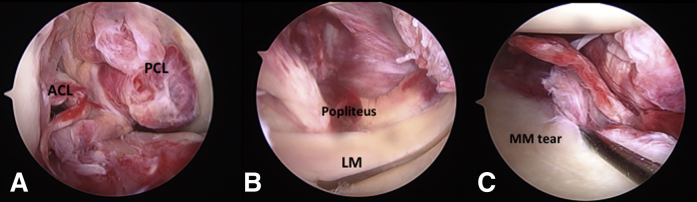
A diagnostic knee arthroscopy is performed per routine (Fig 5A). Prior medial and/or lateral dissections should allow fluid egress and reduce the risk of compartment syndrome. Any chondral lesions are probed and classified. For the sake of this technique discussion, the focus will be on the multiligament injured knee and reconstruction techniques. Any meniscal tears are addressed in standard fashion with routine use of all-inside meniscal repair devices should the repair be manageable by these devices (Fig 6). While we feel that all-inside techniques can many times manage these tears effectively with adequate healing rates, if there is a preference for inside-out repair, then a standard posteromedial approach and/or using the laterally based second window can be used to repair the meniscus tear(s) in standard fashion. It is recommended to address these meniscal tears prior to starting the ligament reconstructions. Also at the time of arthroscopy, PLC injuries can be confirmed by the arthroscopic “drive-through” sign of 10 mm gapping on the lateral side with the knee in the figure-of-4 varus stress position (Fig 5B). Furthermore, medial-sided injuries of the MCL can also be appreciated by the amount of gapping medially while the knee has a valgus stress in 20° to 30° of flexion as well as which direction the medial meniscus travels during this gapping (Fig 5C). Proximal displacement of the meniscus would indicate a deep and likely tibial-sided MCL injury, while distal displacement would correlate to a femoral-sided injury.
Fig 5.
Arthroscopic images, right knee. (A) Note the bicruciate ligament injury visualized through the anterolateral portal. (B) Lateral drive-through sign with gross hematoma appreciated at popliteus tendon. (C) Medial drive-through sign with medial meniscus tear, associated medial soft-tissue hemorrhage, and femoral-sided medial collateral ligament injury given the meniscus stays with the tibial surface during valgus stress.
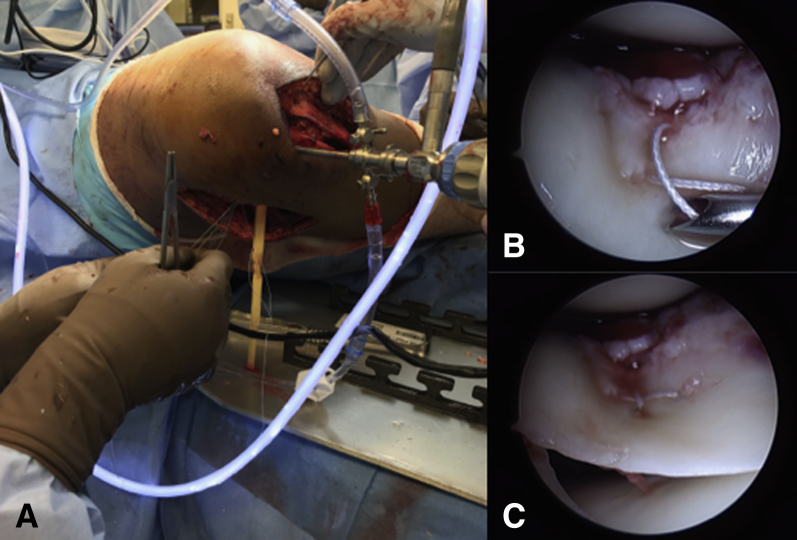
Fig 6.
(A) Intraoperative image, right knee. Inside-out lateral meniscus repair in figure-of-4 position using window 2 for suture placement. (B, C) Arthroscopic image, right knee lateral meniscus repair as a “cross stitch” viewed through the anterolateral portal.
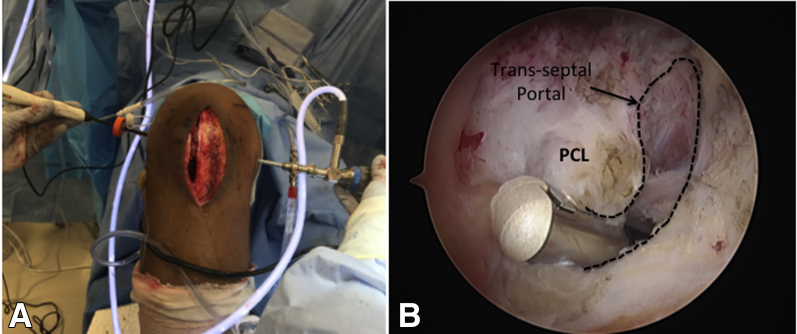
Next the notch is debrided of remnant native ACL/PCL. Finally, to address the PCL tibial tunnel, our preference is to create a posterior transseptal portal23 (Fig 7A). Measuring 2.5 cm distal to the medial epicondyle and then 2.5 cm posterior from that measured point, a spinal needle is inserted into the posteromedial compartment under direct arthroscopic visualization through the empty intercondylar notch.24 A double-dam flexible wall flanged cannula is placed. Next a posterolateral portal is created, by spinal needle localization and arthroscopic illumination, well anterior to the long head of the biceps femoris and proximal to the LCL, of which the long head of the biceps and CPN have been previously identified through the open posterolateral approach. A transseptal portal is then created in standard fashion so that direct visualization and adequate debridement can be performed to expose the PCL recess (Fig 7B). Furthermore, direct visualization of the posteromedial and posterolateral capsule can be performed with the transseptal technique, which can correlate to a posteromedial and PLC injury, respectfully. The femoral cruciate tunnels are then addressed.
Fig 7.
Intraoperative images, right knee. (A) Transseptal portal establishment. Camera is introduced through the posteromedial portal, and electocautery device is advanced through posteromedial portal. (B) Remnant posterior cruciate ligament stump is easily debrided by VAPR electrocautery device (Depuy) after establishment of posterior transseptal portal. Note the transseptal portal is made with the debridement devices aimed anteriorly to limit injury to the posterior neurovascular bundle.
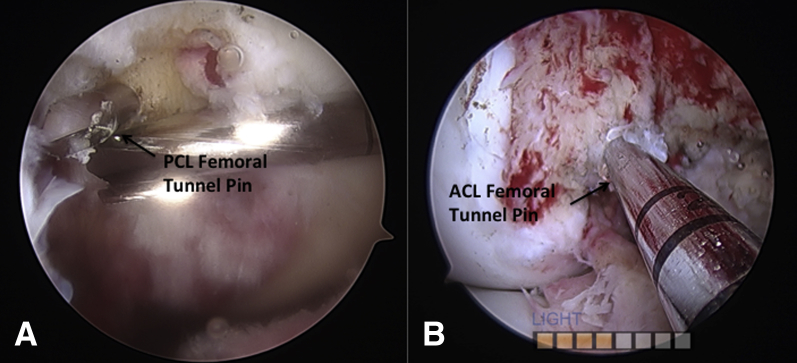
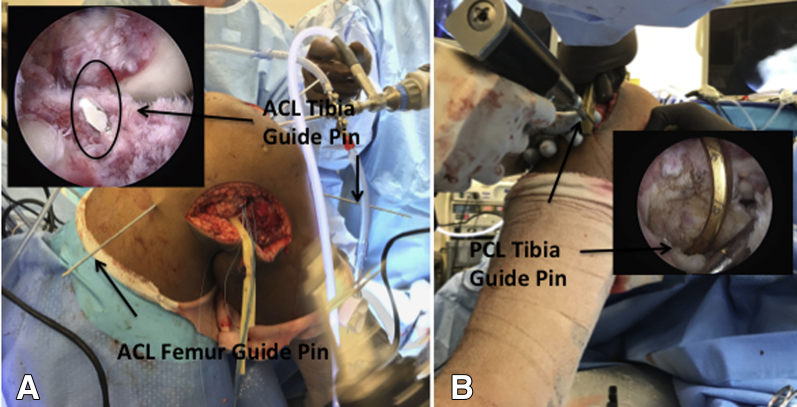
Femoral Tunnels
Using an outside-in technique, an oblique incision is made on the distal anteromedial femur so that a PCL femoral guide (Accufex/Smith & Nephew, Andover, MA) is placed 2 to 3 mm off the articular cartilage high on the medial wall near the superior aspect of the notch. With the knee in 90° of flexion, a 3/32″ pin is then placed in anterograde fashion from outside in, flush to the medial wall (Fig 8A). Next the ACL tunnel is drilled from inside out. We use an accessory anteromedial portal for tunnel obliquity and the initial placement of the ACL tunnel low on the wall. With the knee maximally hyperflexed, the beath pin is drilled in retrograde fashion, exiting the skin in the superolateral quadrant of the thigh. It is important to record the distance on the graduated pin measurements that it takes to perforate the lateral cortex. The pin is advanced so it is flush to the lateral wall (Fig 8B). Attention is then turned to the tibial tunnels.
Fig 8.
Arthroscopic images, right knee. (A) Outside-in posterior cruciate ligament femoral tunnel pin placement. (B) Accessory anteromedial anterior cruciate ligament femoral tunnel pin placement.
Tibial Tunnels
An elbow ACL tibial guide is then used to place a 3/32″ pin so that it enters the distal tibia medial and proximal to where the PCL tibial tunnel will be placed. It is important to limit ACL/PCL tibial tunnel aperture convergence. We routinely use an angle of 55° for the ACL tunnel and 65° for the PCL tunnel but are able to adjust it to be more acute if concern for distal tunnel aperture convergence exists with the planned PCL tunnel. The ACL tibial tunnel pin exits just anterior to the center of the tibial footprint (Fig 9A). With cannulas placed in the posterior working portals, a shaver and/or electrocautery device are introduced through the posteromedial portal and used to debride soft tissue at the PCL recess. Great care is taken to keep the shaver blades and electrocautery directed anteriorly to limit damage to the popliteal space neurovascular elements. Under intraoperative C-Arm imaging, the PCL tibial targeting guide (Accufex/Smith & Nephew) is started more lateral and distal to the ACL tibial tunnel site to once again limit convergence. The tibial PCL targeting guide is placed so that the pin's exit point will be directly in the center of the anatomic PCL recess. This is visualized routinely by placing the arthroscope through the posterolateral portal (Fig 9B). However, a safety incision, as described by Fanelli and Edson, can be used if the pin cannot be visualized and protected and can many times be performed through the posteromedial portal.25 The guide wire is advanced and visualized by lateral C-Arm images taken intermittently until the guide pin exits in the desired location in the PCL recess. Next, final AP and lateral C-Arm images are obtained of the 4 cruciate guide pins to assess the satisfactory position of the ACL and PCL femoral/tibial tunnels (Fig 10). Any adjustments are made at this time with corresponding targeting guides.
Fig 9.
Intraoperative and correlating arthroscopic images of right knee. (A, B) Guide pins placed to planned tunnel locations: (A) anterior cruciate ligament tibial tunnel pin placement and (B) posterior cruciate ligament tibial tunnel under direct visualization through posteromedial portal.
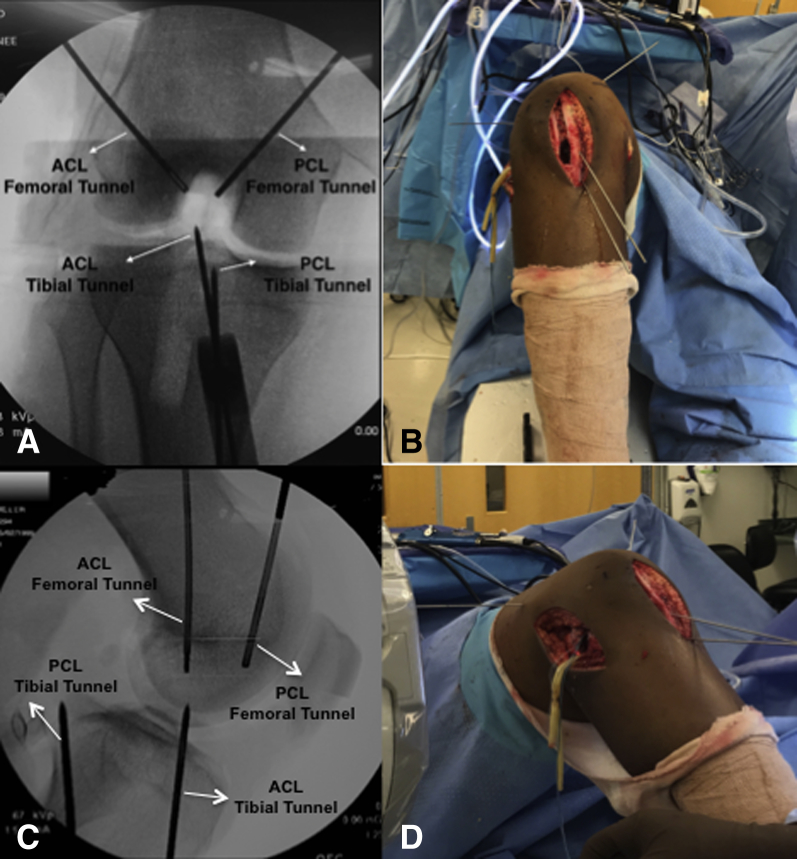
Fig 10.
Intraoperative images with corresponding C-Arm images of right knee. (A-D) Check guide pin positions and directions to prevent possible malpositioned tunnels and tunnel convergence.
Tunnel Reaming
Once satisfied with pin position, a single “half fluted” reamer, line-line to the measured quadrupled hamstring autograft and/or sized appropriately for the bone patellar tendon bone blocks, is used to create the ACL/PCL femoral tunnels. A skid is used to protect the medial femoral condyle during the ACL tunnel preparation. Routinely, we ream to a depth of 3 to 4 mm short of the previously measured beath pin cortical distance for the ACL tunnel when using soft-tissue grafts. If using bone patellar tendon bone, then we recommend drilling 5 mm longer than the bone block, which is typically 20 mm in length. For the PCL femoral tunnel, this is reamed from an outside-in position. A shaver then removes any excess bone debris. Passing sutures are placed through the ACL tunnel, and a luque wire is placed through the PCL femoral tunnel for anticipated graft passage. Using fully fluted tibial reamers, and the reamer sleeve so that bone graft can be collected for later patellar harvest site bone grafting, the ACL tunnel is drilled in standard fashion and its posterior edge rasped to limit sharp edges. Again, care is taken with the reamer to limit plunging and iatrogenic damage to the femoral condyle. A line-to-line tunnel dilator is placed into the ACL tunnel at this time. The PCL tunnel is reamed under direct lateral C-Arm imaging while using a curved PCL curette placed over the guide wire tip to limit its advancement. The reamer is stopped roughly 1 cm short of exiting the tibial cortex, and the remainder is performed by hand so as to limit plunging, which could injure the posterior popliteal neurovascular structures. The posterior aspect of the tibial PCL tunnel is also rasped. A second luque wire is placed in the tibial tunnel for anticipated shuttling of the graft.
Cruciate Graft Passage
First, the PCL graft is passed by the luque wire shuttling technique so that the bone block seats into the tibial docking site with sutures to keep relative tension maintained (Fig 11). The tibial PCL fixation, metal interference screw, is placed over a nitinol guide wire from outside in under direct arthroscopic visualization. Next, the ACL graft is shuttled through and an endobutton (Smith & Nephew) is confirmed to have deployed on the lateral cortex by feel as well as brief anterior-posterior and oblique C-Arm images of the knee. The graft is also marked at the femoral cortical distance + 6 mm, which allows for the button to adequately flip and seat on the lateral femoral cortex. Attention then turns to the MCL/PLC reconstructions. It is important to not complete the fixation for centrally based ACL/PCL reconstructions until later as detailed below.
Fig 11.
Intraoperative images with corresponding C-Arm images of right knee. (A) Rasp tunnel edges to facilitate graft passage. (B) Graft passing. Arthroscopic images. (C) Viewing through the notch, with the help of a probe advanced through the posteromedial portal, the posterior cruciate ligament graft is shuttled. (D) Anterior cruciate ligament graft is seated into the femoral tunnel.
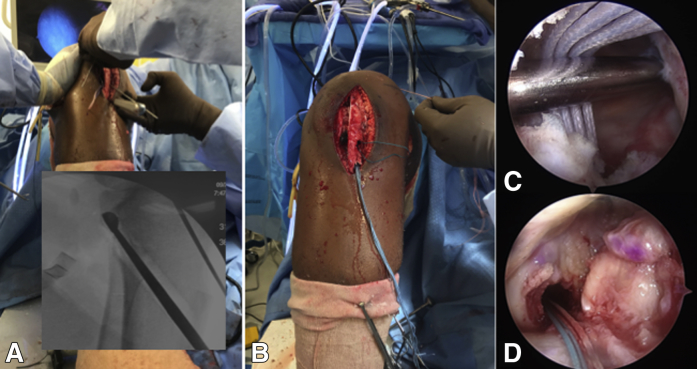
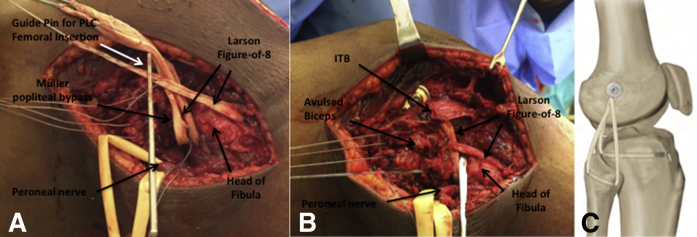
PLC Reconstruction
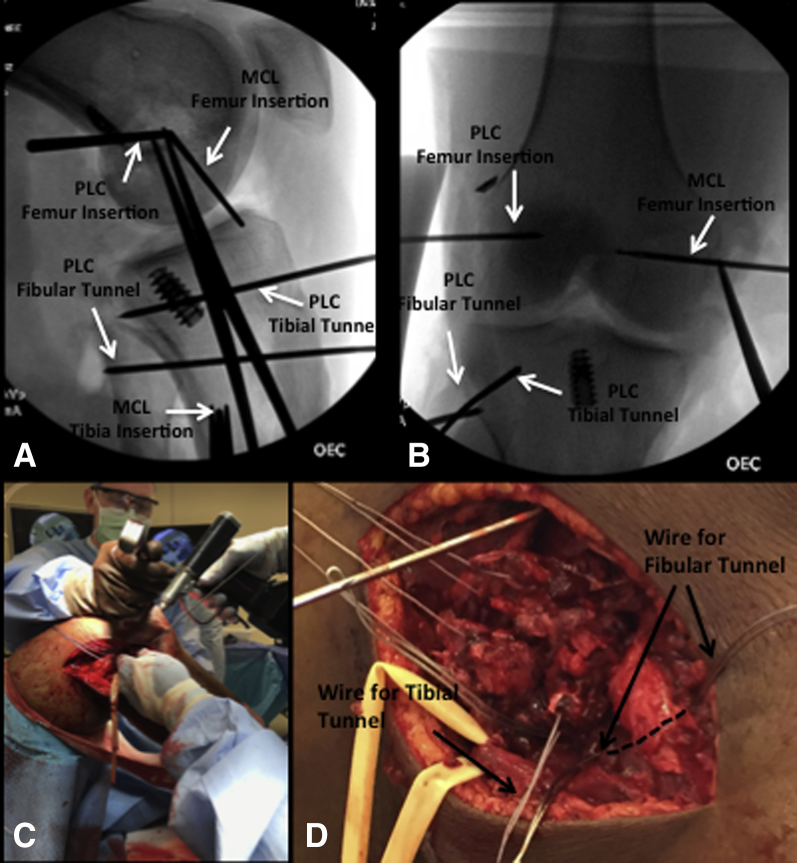
With the windows previously created, the origin of the LCL and insertion of the popliteus tendon is directly visualized, or if grossly disrupted, then radiographic landmarks are used. When possible, a primary repair is carried out prior to a formal PLC reconstruction. Using a perfect lateral intraoperative C-Arm image where the posterior condyles overlap, the center of the LCL origin is appreciated. This is at a point 58% of the distance from anterior to posterior on the Blumensats line and is 2 mm distal posterior to this measured distance.26 The popliteus tendon insertion is measured on an oblique line 18.5 mm anterior and distal to the center of the LCL origin. We routinely place our initial 3/32″ pin, and definitive fixation, at a midpoint between the LCL origin and popliteus insertion given we use a 6.5-mm fully threaded cancellous screw with a 20-mm spiked washer to fix the PLC reconstruction. This nicely spreads the reconstructed limbs of the PLC graft to the respective anatomic locations of the LCL and popliteus. A 3/32″ pin is placed at this midpoint location directed roughly 30° anterior and slightly proximal in the femur to limit ACL tunnel conversion with cruciate graft injury and violating the intercondylar notch. Next, a 3/32″ pin is placed in the fibular head roughly 1 to 1.5 cm distal to the tip of the fibula, aiming from caudad to cephalad and slightly lateral to medial. This will primarily be used for the figure-of-8 Larson laterally based repair of the LCL and PFL. Great care is taken to maintain adequate visualization of the CPN as it approaches the fibular head. Another 3/32″ pin is placed starting on the mid aspect of Gerdy's tubercle, roughly 1 to 1.5 cm distal to the joint line, and is routinely through a percutaneous incision. This pin is directed posteriorly, while a retractor is placed just along the posterior border of the tibia, through a window, to protect the popliteal vessels. The tip of the pin should exit posteriorly approximately 1 cm medial and 1 cm distal to the posterolateral edge of the tibia and is confirmed with C-Arm imaging. This will serve as the popliteal bypass reconstruction by the Müller technique. With PLC pins placed, final AP and lateral C-Arm images are obtained to provide a final assessment to ensure no gross tunnel convergence and satisfactory placement of the pins (Fig 12 A and B). A suture can be placed around the pins to ensure isometry is present and adjustments are made as necessary.
Fig 12.
C-Arm images of right knee. (A, B) Tunnel positions for posterolateral corner (PLC) and medial collateral ligament (MCL) reconstructions. Intraoperative images. (C, D) MCL and PLC are checked; note the luque wires (long arrows) used for the tibia and fibular tunnels (Larson and Müller reconstructions) and the proximity of the peroneal nerve (asterisks).
Should a lateral capsular-based repair be indicated, then 2 to 3 labral repair single-loaded suture anchors (Depuy, Raynham, MA) are placed on either the femoral or tibial side just above/below the articular margin, corresponding to the zone of injury, and the capsule is repaired. Next, the lateral-based PLC reconstruction pins in the femur are overreamed with a 4.5-mm cannulated reamer and tapped and the tibia and fibular pins are overreamed with appropriately sized reamers for the measured grafts, always protecting the CPN and with a retractor through the window to protect the neurovascular structures (Fig 12C). Luque wires are then passed through each of these tunnels (Fig 12D). A 6.5-mm cancellous screw (ConMed, Linvatec, Largo, FL) with spiked washer (ConMed, Linvatec) is then placed into the femoral location, however, it is not completely seated. A semitendinosis allograft is then shuttled through the Müller tibial tunnel and a 5.5 mm × 15 mm biocomposite screw (Arthrex) is placed in the anterior tibial aperture as an interference fit. The popliteal bypass reconstruction graft is then shuttled posterior to anterior around the screw after shuttling it under the short head of the biceps and iliotibial band. At the same time another semitendinosis allograft is shuttled through the fibular-based Larson reconstruction and its anteromedial limb is shuttled posteriorly around the femoral screw and the posterolateral limb is shuttled anteriorly around the screw (Fig 13A). During the passage of these grafts through the windows, it is vital to pass them under the short head of the biceps and posterior iliotibial band as well so they are not incarcerated in this tissue, which would drastically affect the isometry of the grafts (Fig 13 B and C). It is also vital to ensure the CPN is completely free and without tension.
Fig 13.
Right knee intraoperative images with schematic correlation. (A-C) Graft passage for posterolateral corner reconstruction of lateral collateral ligament, popliteofibular ligament, and popliteal bypass.
(With the permission of Mark D. Miller, Sports medicine conditions: return to play: recognition, treatment, planning, 1st ed., Lippincott Williams & Wilkins, 2013.)
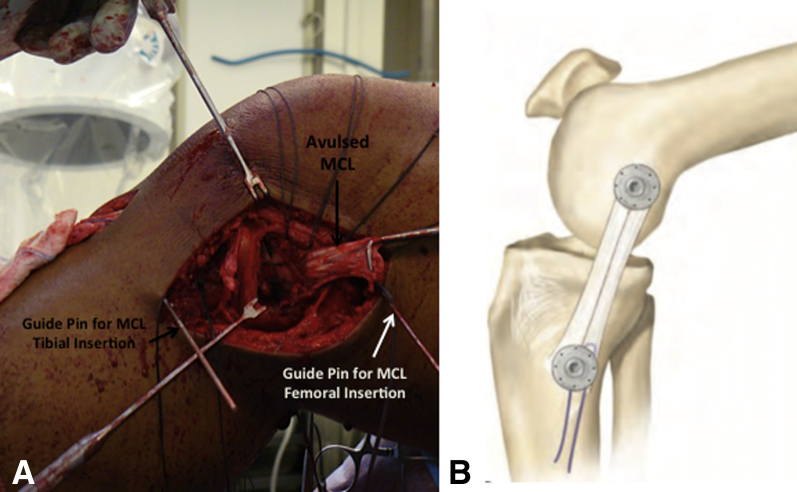
MCL Reconstruction
If the previously made utilitarian medial paramedian incision can be used for this exposure, then it is; however, if needed, a separate medially based vertical incision is used centered directly over the medial epicondyle extending distally over the palpated posterior tibia border. A primary repair, if possible, is completed, typically with suture anchors. The surgeon must then determine whether a supplemental reconstruction is indicated, depending on the quality of the tissue and repair. Our preferred medial reconstruction is to use a modified Bosworth technique in which the native semitendinosus is harvested but left attached to its distal insertion.27 When native semitendinosus is unavailable or has been harvested for a concurrent or previous ACL reconstruction, an allograft may be used to recreate the MCL. Upon dissection, the superficial MCL (sMCL) origin is identified, roughly 3 mm proximal to and 5 mm posterior from the medial epicondyle.28 Should this landmark be disrupted or difficult to find, then a perfect lateral radiograph is used and the pin is placed at a point that is a line drawn from the posterior femoral cortex, where it intersects the Blumensats line; a perpendicular line is drawn there, and then roughly 5 mm proximal and 2 mm posterior to this point is the sMCL origin.29 A pin is placed at this sMCL origin and aimed proximal to limit intersecting the PCL tunnel. The sMCL insertion on the tibia is routinely 6 cm distal to the joint line, and a pin is inserted there as well, routinely placed on the posterior aspect of the tibia28 (Fig 14A). With MCL pins placed, final AP and lateral C-Arm images are obtained to provide a final assessment to ensure no gross tunnel convergence and satisfactory placement of the pins (Fig 12 A and C). A suture is placed around the pins to ensure isometry is present and adjustments are made as necessary.
Fig 14.
Right knee intraoperative images and schematic correlation. (A, B) Medial-sided incision showing medial collateral ligament injury and planned reconstruction.
(With the permission of Mark D. Miller, Sports medicine conditions: return to play: recognition, treatment, planning, 1st ed., Lippincott Williams & Wilkins, 2013.)
The MCL reconstruction is finalized with overreaming the femoral and tibial pins with a 4.5-mm cannulated reamer. During reaming, particular attention is placed to ensure there is no tunnel convergence. Both of these are tapped to an adequate depth. Two 6.5-mm cancellous screws with a 17- or 20-mm spiked washers are placed at these locations (Fig 14B). A semitendinosis allograft is looped over the proximal screw, beneath the washer, and the screw is advanced to satisfaction. The distal screw is not fully seated.
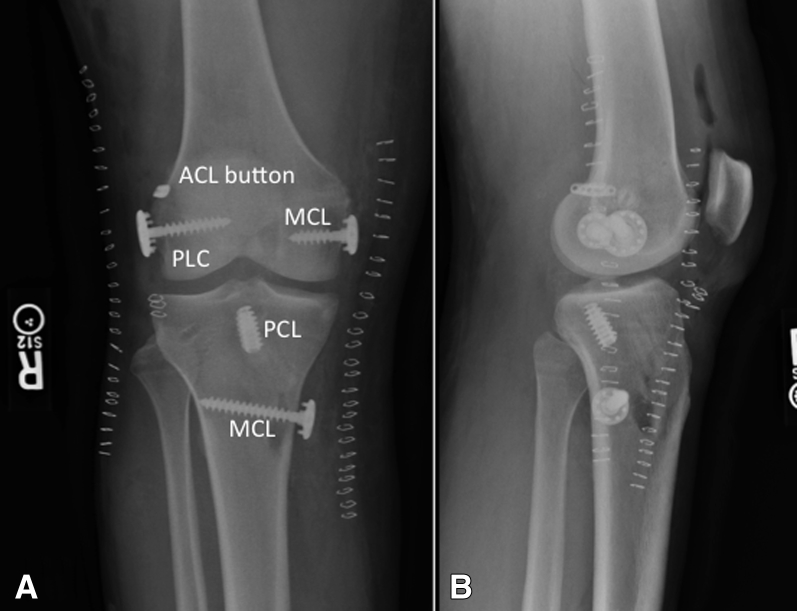
Final Graft Fixation
At this point it is important to work from central to peripheral. The PCL is fixed first. The PCL femoral fixation is placed with the knee in 90° of flexion and under graft suture tension with an anterior drawer placed to establish the normal tibial step-off. After fixation, a posterior drawer is checked for satisfactory stability. Occasionally, a fluoroscopic image is necessary to determine the proper amount of reduction. Once confirmed, the ACL tibial fixation is placed. The 4 limbs of the hamstring graft are splayed apart, and under a manual tensioner, a biocomposite sheath and screw are placed accommodating the size of the graft. This provides adequate fixation, and an intraoperative Lachman test is performed to ensure stable cruciate fixation (Fig 15A).
Fig 15.
Arthroscopic images of right knee. (A) Anterior cruciate ligament, posterior cruciate ligament graft assessment after finalizing tibial fixation. Intraoperative images. (B, C) Posterolateral corner and medial collateral ligament reconstruction, respectively, after final graft fixation.
For the femoral-based PLC reconstruction fixation, the grafts are already looped over the screw and under the washer and the graft ends are then tensioned while a slight valgus force is placed on the knee while in 30° of flexion. The femoral screw and washer are maximally tightened. We have found that using a mallet on the screwdriver will help to keep it engaged and limit screw stripping (Fig 15B).
Prior to placing the graft around the distal screw and tunneling it through any remaining soft tissue medially, if a deep MCL repair is needed, then 2 to 3 labral repair single-loaded suture anchors (Depuy) are placed either on the femoral or tibial side, corresponding to the zone of injury, and the capsule/deep MCL is repaired with the knee in full terminal extension. If a red-red zone meniscocapsular separation is present with gross capsule violation, then the sutures are passed through the meniscal tear to provide an open repair. Furthermore, if a positive Slocum test exists or concern for a PMC injury of the posterior oblique ligament (POL) is present, then this posteromedial soft-tissue window can be advanced with an additional suture anchor placed just below the articular margin. We have found that this is satisfactory for a PMC injury repair in the setting of closely reapproximating the deep MCL tissue as a direct repair and augmenting the medial-sided reconstruction with the allograft tissue as noted above (Fig 15C). The graft is tunneled through any remaining medial soft tissue distally. Next the semitendinosis graft is looped around the distal screw and beneath the washer. With the knee in 30° of flexion, a reasonable varus stress, and with maximum traction on the graft sutures with the grafts wrapped/looped deep to the washer, the washer/screw complex is tightened maximally. Similar to the lateral femoral screw, medial-sided screw and washer placement is made easier by malleting the screwdriver during hardware placement. This completes the medial-based repair/reconstruction.
The knee is checked for overall stability at 0° and 30° of flexion for collateral ligament evaluation as well as final check on cruciate ligaments at 30° and 90°. The wounds are thoroughly irrigated with copious normal antibiotic saline (bacitracin 50K/1L) by pulsatile lavage. It is recommended to pay close attention to the surgical time and to redose the antibiotics per routine guidelines as needed. Any provisional fixation is removed, and the wounds are closed in successive fashion from deep to superficial, once again checking the CPN to ensure it is in continuity and that it is unobstructed in its natural course to the fibular head. The skin is closed with staples, and the knee placed in a hinged knee brace (Fig 16). The order of surgical steps is summarized in Table 4.
Fig 16.
Postoperative radiographs of right knee. (A, B) AP/lateral status postsurgery completion.
Table 4.
Order of Surgical Steps
|
ACL, anterior cruciate ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner.
Steps performed under tourniquet.
Postoperative Rehabilitation
The goal of our postoperative rehabilitation protocol is to promote knee range of motion while protecting the reconstructed ligaments. A systematic review of severe multiple-ligament knee injuries demonstrated that early mobility was associated with better outcomes in comparison with immobilization and yielded fewer range-of-motion deficits, especially in acutely managed patients.30 We prefer to restrict weight bearing to 50% for the first 6 weeks. The initial phase of rehabilitation is similar in different patterns of MLIs. The operative knee is maintained in a hinged-knee brace locked in full extension, which is unlocked for passive prone range-of-motion exercises and continuous passive motion machine use. Isometric quadriceps exercises are started immediately. Maintaining full extension and avoiding full weight bearing is crucial to minimize excessive stress on ACL and PCL grafts. At 2 weeks, the brace is unlocked and set at 0° to 90° to allow the advancement of self-directed range-of-motion exercises in prone position. The patient is weaned from crutches at 6 weeks and advanced to full weight bearing at full extension. In this phase, rehabilitation should be tailored to the individual patient based on the pattern of injury. Status of the PCL drives the rehabilitation protocol for different patterns of MLIs, as it is considered the main static stabilizer of the knee.31 Active knee flexion involving the hamstrings is restricted for 12 weeks in cases with PCL injuries as hamstring contraction has the potential to subluxate the tibia posteriorly and compromise the reconstruction.32 The patient continues to focus on strength and function from 4 to 6 months, at which time he or she may be fitted with a functional brace. Strength and functional testing is performed monthly at this point to assess the ability to return to sports.
Discussion
The management of the MLI is based on the acuity and pattern of the injury, and many variables must be considered such as the vascular status of the involved extremity, the degree of instability, postreduction stability, the presence of open wounds, and the condition of the skin. A recent systematic review of the literature demonstrated that early operative treatment of MLI yields improved functional and clinical outcomes compared with nonoperation or delayed surgery.1 Under ideal circumstances, we favor single-stage reconstruction of all injured ligaments at the index procedure within 3 weeks after injury.
Arthroscopic reconstruction of ACL and PCL is a widely accepted treatment method among most surgeons. Arthroscopic evaluation of the joint is paramount to diagnose the concomitant knee pathologies such as meniscal and articular lesions. As stated above, we recommend addressing these meniscal tears prior to starting the ligament reconstructions, either in all-inside fashion or inside-out fashion through the incisions used for the collateral ligament reconstructions. Despite recent improvements in PCL reconstruction techniques, poor visualization of the tibial insertion could lead to an incorrect tunnel placement of the tibial tunnel, which seems to be one of the most common causes of PCL reconstruction failure.33 Noyes and Barber-Westin reported that placing the tibial tunnel proximal to the normal PCL anatomical tibial attachment site results in vertical graft position, which limited its ability to resist posterior tibial translation.34 We have adopted the posterior transseptal as described by Ahn et al.23 Furthermore, this technique allows addressing the obstacles that complicate graft passage, which are commonly encountered, particularly in severely injured knees.
Currently, the sequence of graft tensioning and fixation remains controversial. Wentorf et al. reported that tensioning and fixation of the ACL first in PLC deficient knees could result in excessive external rotation of the tibia. Therefore, the investigators suggested fixing the PLC prior to the ACL to avoid external tibial rotation.35 Kim et al.36 retrospectively reviewed their patients with multiligament knee injuries and reported higher functional scores and favorable posterior stress radiographs in patients treated with an ACL-first fixation approach compared with the PCL-first patients. Once all grafts have been passed, we prefer to tension and secure the PCL first in 90° of flexion to reestablish the anteroposterior relationship of the tibia relative to the femur, followed by ACL fixation at full extension to restore the central axis of knee rotation.1, 37 Intraoperative lateral fluoroscopy may be used to ensure that a proper relationship between the tibia and femur has been reestablished. Then medial- and lateral-based reconstructions are each secured with a slight varus or valgus stress, respectively, at about 30° of knee flexion. However, strict attention should be paid to deep MCL/PMC injury repairs to be performed near full extension.
PLC injury of the knee presents unique diagnosis and treatment challenges due to the complexity of the involved structures and function. It is well known that PLC reconstructions yield better results than repair procedures.3 Improved understanding of anatomical and biomechanic properties of posterolateral structures led surgeons to identify the reconstruction technique that provides optimal subjective and objective outcomes. In the current literature, there are numerous surgical techniques that have been proposed for the reconstruction of all 3 key posterolateral structures (LCL, popliteus tendon [PT], and PFL) in order to restore the entire functional unit; however, outcome data from these studies are still highly variable.2, 3, 4, 5, 6, 7, 8, 9 We prefer to use a combination of a Müller popliteal bypass for popliteus tendon and Larson figure-of-8 technique for LCL and popliteofibular reconstructions.38, 39 Grafts are secured to the lateral femoral epicondylar region with a screw and spiked washer to the anatomic insertion sites of the LCL and the popliteus tendon. Once the anatomical insertion sites of both LCL and PT are identified,4, 40, 41 grafts are secured at a midpoint between the LCL origin and popliteus insertion. We use a large 6.5-mm fully threaded cancellous screw with a 20-mm spiked washer to fix the PLC reconstruction. Using a 20-mm spiked washer nicely spreads the reconstructed limbs of the PLC graft to the respective anatomic locations of the LCL and popliteus. Although the clinical outcome studies are limited, reconstruction of the PLC using an allograft reconstruction of the PT, PFL, and LCL yielded a stable reconstruction resulting in improved clinical outcomes and objective stability.3, 42, 43 Securing the PLC structures to the lateral femoral condyle through a single screw and spiked washer may have theoretical advantages to prevent tunnel convergence, particularly encountered in patients having simultaneous ACL and PLC reconstructions with multiple short-ended and long tunnels present. Current anatomic ACL reconstruction techniques using accessory anteromedial portals cause more horizontal femoral tunnels, which anatomically are directed closer to the LCL and PT origins.10, 44 Furthermore, when a surgeon has to drill multiple tunnels in the distal femur, it may be difficult to determine the best angle for drilling so as to avoid tunnel collisions. Tunnel convergence may lead to iatrogenic graft rupture, graft fixation compromise, or even excessively short tunnels.45 Moreover, individual factors such as small lateral femoral condylar width may increase the risk of tunnel convergance and even femoral condyle fractures.11, 46
It is generally accepted that incomplete tears and isolated complete tears of the MCL can be treated nonoperatively due to their excellent healing capability.47 However, in the setting of multiligament knee injuries, the management of a medial ligamentous injury is more challenging and a subject of controversy.48 We prefer operative intervention in patients with significant valgus instability, tibial-sided injuries, an incarcerated MCL, or Stener lesions. If the MCL is avulsed as a thick sleeve from its attachment, we prefer to repair this primarily to a prepared bone bed with suture anchors or a screw and spiked washer. In the setting of midsubstance tears of the MCL, chronic tears, and tenuous repairs, we typically supplement this with either autogenous graft by a modified Bosworth reconstruction or with an allograft as described above.27 In severe injuries with a posteromedial instability, the posterior limb of the MCL graft may be looped around the semimembranosus tendon to reestablish the stability conferred by the POL. This technique yields reasonable clinical outcomes in patients with medial-sided injury in the setting of knee dislocations.49, 50 Alternatively, the POL can be imbricated into the posterior aspect of the MCL and graft.
The technique we used for PLC and MCL reconstructions may have some disadvantages. Spiked washers may cause irritation on the lateral or medial side of the knee once patients recover and return to activities of daily living. However, these washers can be removed through small incisions, and second-look arthroscopy can be used simultaneously to resect adhesions from inital trauma and minimize the risk of permanent arthrofibrosis or patellofemoral pain. In this Technical Note, we have described our approach to the management of multiple ligament knee injuries (Table 5, Video 1). As we continue to follow our patients' outcomes, we encourage further studies to evaluate our surgical techniques for long-term patient outcomes.
Table 5.
Pearls and Pitfalls
|
PCL, posterior cruciate ligament.
Acknowledgment
The authors thank Chris Jacobsen for his valuable assistance in formatting the video.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: M.D.M. is an Arthrex consultant; however, for the purposes of this described surgical technique, there is no gross conflict of interest. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates our preferred method for the assessment and surgical management of a multiligament right knee injury. Physical examination of each structure and stress radiography findings suggests a knee dislocation (KDIV) injury. Guide pins are placed at the desired cruciate ligament reconstruction tunnels and planned insertion sites of collateral ligaments and confirmed by fluoroscopy to avoid tunnel convergence and malposition. Anatomic single-bundle anterior cruciate ligament and posterior cruciate ligament reconstructions are performed with harvested autografts. A combination of Müller popliteal bypass and Larson figure-of-8 techniques is used to reconstruct posterolateral corner, and modified Bosworth technique is performed for medial collateral ligament reconstruction.
References
- 1.Levy B.A., Dajani K.A., Whelan D.B. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430–438. doi: 10.1016/j.arthro.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Fanelli G.C. Surgical treatment of lateral posterolateral instability of the knee using biceps tendon procedures. Sports Med Arthrosc. 2006;14:37–43. doi: 10.1097/00132585-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Stannard J.P., Brown S.L., Farris R.C., McGwin G., Jr., Volgas D.A. The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med. 2005;33:881–888. doi: 10.1177/0363546504271208. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 5.Angelini F.J., Helito C.P., Tozi M.R. Combined reconstruction of the anterior cruciate ligament and posterolateral corner with a single femoral tunnel. Arthrosc Tech. 2013;2:e285–288. doi: 10.1016/j.eats.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee K.H., Jung Y.B., Jung H.J. Combined posterolateral corner reconstruction with remnant tensioning and augmentation in chronic posterior cruciate ligament injuries: minimum 2-year follow-up. Arthroscopy. 2011;27:507–515. doi: 10.1016/j.arthro.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Rios C.G., Leger R.R., Cote M.P., Yang C., Arciero R.A. Posterolateral corner reconstruction of the knee: evaluation of a technique with clinical outcomes and stress radiography. Am J Sports Med. 2010;38:1564–1574. doi: 10.1177/0363546510363462. [DOI] [PubMed] [Google Scholar]
- 8.Kuzma S.A., Chow R.M., Engasser W.M., Stuart M.J., Levy B.A. Reconstruction of the posterolateral corner of the knee with achilles tendon allograft. Arthrosc Tech. 2014;3:e393–e398. doi: 10.1016/j.eats.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sekiya J.K., Kurtz C.A. Posterolateral corner reconstruction of the knee: surgical technique utilizing a bifid Achilles tendon allograft and a double femoral tunnel. Arthroscopy. 2005;21:1400. doi: 10.1016/j.arthro.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 10.Shuler M.S., Jasper L.E., Rauh P.B., Mulligan M.E., Moorman C.T., 3rd Tunnel convergence in combined anterior cruciate ligament and posterolateral corner reconstruction. Arthroscopy. 2006;22:193–198. doi: 10.1016/j.arthro.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Gali J.C., Bernardes Ade P., dos Santos L.C., Ferreira T.C., Almagro M.A., da Silva P.A. Tunnel collision during simultaneous anterior cruciate ligament and posterolateral corner reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:195–200. doi: 10.1007/s00167-014-3363-0. [DOI] [PubMed] [Google Scholar]
- 12.Levy B.A., Dajani K.A., Morgan J.A., Shah J.P., Dahm D.L., Stuart M.J. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. doi: 10.1177/0363546509352459. [DOI] [PubMed] [Google Scholar]
- 13.Schenck R.C., Jr., Hunter R.E., Ostrum R.F., Perry C.R. Knee dislocations. Instr Course Lect. 1999;48:515–522. [PubMed] [Google Scholar]
- 14.Sekiya J.K., Whiddon D.R., Zehms C.T., Miller M.D. A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90:1621–1627. doi: 10.2106/JBJS.G.01365. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 16.Laprade R.F., Bernhardson A.S., Griffith C.J., Macalena J.A., Wijdicks C.A. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010;38:330–338. doi: 10.1177/0363546509349347. [DOI] [PubMed] [Google Scholar]
- 17.Bollier M., Smith P.A. Anterior cruciate ligament and medial collateral ligament injuries. J Knee Surg. 2014;27:359–368. doi: 10.1055/s-0034-1381961. [DOI] [PubMed] [Google Scholar]
- 18.Devitt B.M., Whelan D.B. Physical examination and imaging of the lateral collateral ligament and posterolateral corner of the knee. Sports Med Arthrosc. 2015;23:10–16. doi: 10.1097/JSA.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 19.Slocum D.B., Larson R.L. Rotatory instability of the knee. Its pathogenesis and a clinical test to demonstrate its presence. J Bone Joint Surg Am. 1968;50:211–225. [PubMed] [Google Scholar]
- 20.Bronstein R.D., Schaffer J.C. Physical examination of knee ligament injuries. J Am Acad Orthop Surg. 2017;25:280–287. doi: 10.5435/JAAOS-D-15-00463. [DOI] [PubMed] [Google Scholar]
- 21.Veltri D.M., Warren R.F. Anatomy, biomechanics, and physical findings in posterolateral knee instability. Clin Sports Med. 1994;13:599–614. [PubMed] [Google Scholar]
- 22.Gwathmey F.W., Jr., Tompkins M.A., Gaskin C.M., Miller M.D. Can stress radiography of the knee help characterize posterolateral corner injury? Clin Orthop Relat Res. 2012;470:768–773. doi: 10.1007/s11999-011-2008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahn J.H., Chung Y.S., Oh I. Arthroscopic posterior cruciate ligament reconstruction using the posterior trans-septal portal. Arthroscopy. 2003;19:101–107. doi: 10.1053/jars.2003.50017. [DOI] [PubMed] [Google Scholar]
- 24.Cancienne J.M., Werner B.C., Burrus M.T. The transseptal arthroscopic knee portal is in close proximity to the popliteal artery: a cadaveric study. J Knee Surg. 2017;30:920–924. doi: 10.1055/s-0037-1599252. [DOI] [PubMed] [Google Scholar]
- 25.Fanelli G.C., Edson C.J. Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703–714. doi: 10.1053/jars.2002.35142. [DOI] [PubMed] [Google Scholar]
- 26.Kamath G.V., Redfern J.C., Burks R.T. Femoral radiographic landmarks for lateral collateral ligament reconstruction and repair: a new method of reference. Am J Sports Med. 2010;38:570–574. doi: 10.1177/0363546509350066. [DOI] [PubMed] [Google Scholar]
- 27.Bosworth D.M. Transplantation of the semitendinosus for repair of laceration of medial collateral ligament of the knee. J Bone Joint Surg Am. 1952;34:196–202. [PubMed] [Google Scholar]
- 28.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 29.Hartshorn T., Otarodifard K., White E.A., Hatch G.F., 3rd Radiographic landmarks for locating the femoral origin of the superficial medial collateral ligament. Am J Sports Med. 2013;41:2527–2532. doi: 10.1177/0363546513504895. [DOI] [PubMed] [Google Scholar]
- 30.Mook W.R., Miller M.D., Diduch D.R., Hertel J., Boachie-Adjei Y., Hart J.M. Multiple-ligament knee injuries: a systematic review of the timing of operative intervention and postoperative rehabilitation. J Bone Joint Surg Am. 2009;91:2946–2957. doi: 10.2106/JBJS.H.01328. [DOI] [PubMed] [Google Scholar]
- 31.Van Dommelen B.A., Fowler P.J. Anatomy of the posterior cruciate ligament. A review. Am J Sports Med. 1989;17:24–29. doi: 10.1177/036354658901700104. [DOI] [PubMed] [Google Scholar]
- 32.Shelburne K.B., Pandy M.G. Determinants of cruciate-ligament loading during rehabilitation exercise. Clin Biomech. 1998;13:403–413. doi: 10.1016/s0268-0033(98)00094-1. [DOI] [PubMed] [Google Scholar]
- 33.Lee S.H., Jung Y.B., Lee H.J., Jung H.J., Kim S.H. Revision posterior cruciate ligament reconstruction using a modified tibial-inlay double-bundle technique. J Bone Joint Surg Am. 2012;94:516–522. doi: 10.2106/JBJS.K.00030. [DOI] [PubMed] [Google Scholar]
- 34.Noyes F.R., Barber-Westin S.D. Posterior cruciate ligament revision reconstruction. Part 1. Causes of surgical failure in 52 consecutive operations. Am J Sports Med. 2005;33:646–654. doi: 10.1177/0363546504271210. [DOI] [PubMed] [Google Scholar]
- 35.Wentorf F.A., LaPrade R.F., Lewis J.L., Resig S. The influence of the integrity of posterolateral structures on tibiofemoral orientation when an anterior cruciate ligament graft is tensioned. Am J Sports Med. 2002;30:796–799. doi: 10.1177/03635465020300060701. [DOI] [PubMed] [Google Scholar]
- 36.Kim S.J., Kim S.H., Jung M., Kim J.M., Lee S.W. Does sequence of graft tensioning affect outcomes in combined anterior and posterior cruciate ligament reconstructions? Clin Orthop Relat Res. 2015;473:235–243. doi: 10.1007/s11999-014-3939-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fanelli G.C., Edson C.J. Surgical treatment of combined PCL-ACL medial and lateral side injuries (global laxity): surgical technique and 2- to 18-year results. J Knee Surg. 2012;25:307–316. doi: 10.1055/s-0032-1326997. [DOI] [PubMed] [Google Scholar]
- 38.Sidles J.A., Larson R.V., Garbini J.L., Downey D.J., Matsen F.A., 3rd Ligament length relationships in the moving knee. J Orthop Res. 1988;6:593–610. doi: 10.1002/jor.1100060418. [DOI] [PubMed] [Google Scholar]
- 39.Muller W. Springer-Verlag; Berlin, Heidelberg, New York: 1989. p. 273. (Das Knie: Form, Funktion und ligamentäre Wiederherstellungschirurgie). [Google Scholar]
- 40.Staubli H.U., Birrer S. The popliteus tendon and its fascicles at the popliteal hiatus: gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy. 1990;6:209–220. doi: 10.1016/0749-8063(90)90077-q. [DOI] [PubMed] [Google Scholar]
- 41.Moorman C.T., 3rd, LaPrade R.F. Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg. 2005;18:137–145. doi: 10.1055/s-0030-1248172. [DOI] [PubMed] [Google Scholar]
- 42.LaPrade R.F., Johansen S., Agel J., Risberg M.A., Moksnes H., Engebretsen L. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am. 2010;92:16–22. doi: 10.2106/JBJS.I.00474. [DOI] [PubMed] [Google Scholar]
- 43.Jakobsen B.W., Lund B., Christiansen S.E., Lind M.C. Anatomic reconstruction of the posterolateral corner of the knee: a case series with isolated reconstructions in 27 patients. Arthroscopy. 2010;26:918–925. doi: 10.1016/j.arthro.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 44.Neven E., D'Hooghe P., Bellemans J. Double-bundle anterior cruciate ligament reconstruction: a cadaveric study on the posterolateral tunnel position and safety of the lateral structures. Arthroscopy. 2008;24:436–440. doi: 10.1016/j.arthro.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 45.Gelber P.E., Erquicia J.I., Sosa G. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: computed tomography evaluation in a cadaveric model. Arthroscopy. 2013;29:257–265. doi: 10.1016/j.arthro.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 46.Werner B.C., Miller M.D. Intraoperative Hoffa fracture during primary ACL reconstruction: can hamstring graft and tunnel diameter be too large? Arthroscopy. 2014;30:645–650. doi: 10.1016/j.arthro.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 47.Indelicato P.A., Hermansdorfer J., Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990:174–177. [PubMed] [Google Scholar]
- 48.Stannard J.P., Black B.S., Azbell C., Volgas D.A. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25:429–434. doi: 10.1055/s-0032-1322605. [DOI] [PubMed] [Google Scholar]
- 49.Werner B.C., Hadeed M.M., Gwathmey F.W., Jr., Gaskin C.M., Hart J.M., Miller M.D. Medial injury in knee dislocations: what are the common injury patterns and surgical outcomes? Clin Orthop Relat Res. 2014;472:2658–2666. doi: 10.1007/s11999-014-3483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kovachevich R., Shah J.P., Arens A.M., Stuart M.J., Dahm D.L., Levy B.A. Operative management of the medial collateral ligament in the multi-ligament injured knee: an evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2009;17:823–829. doi: 10.1007/s00167-009-0810-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates our preferred method for the assessment and surgical management of a multiligament right knee injury. Physical examination of each structure and stress radiography findings suggests a knee dislocation (KDIV) injury. Guide pins are placed at the desired cruciate ligament reconstruction tunnels and planned insertion sites of collateral ligaments and confirmed by fluoroscopy to avoid tunnel convergence and malposition. Anatomic single-bundle anterior cruciate ligament and posterior cruciate ligament reconstructions are performed with harvested autografts. A combination of Müller popliteal bypass and Larson figure-of-8 techniques is used to reconstruct posterolateral corner, and modified Bosworth technique is performed for medial collateral ligament reconstruction.