Abstract
Rationale:
Patients with Parkinson's disease (PD) frequently suffer from psychiatric disorders, and treating these symptom whereas managing the motor symptoms associated with PD can be a therapeutic challenge.
Patient concerns:
We report a case of PD patient with severe depression and anxiety that refused to be treated with dopaminagonists or SSRIs, the most common treatments for PD patients suffering from psychiatric symptoms.
Diagnoses:
Parkinson's disease with severe depression and anxiety.
Interventions:
This man was treated with hyperbaric oxygen treatment for 30 days.
Outcomes:
Clinical assessment scores for depression and anxiety, including Unified Parkinson's Disease Rating ScaleI (UPDRS I), UPDRS II, Hanmilton Depression Rating Scale, and Hamiliton Anxiety Rating Scale, were improved following the hyperbaric oxygen treatment.
Lessons:
Hyperbaric oxygen treatment may be a potential therapeutic method for PD patient suffering from depression and anxiety. Further research is needed to validate this finding and explore a potential mechanism.
Keywords: anxiety, depression, hyperbaric oxygen, Parkinson's disease
1. Introduction
Patients with Parkinson's disease (PD) frequently suffer from nonmotor symptoms, with up to 40% to 60% of PD patients suffering from psychiatric symptoms.[1] Psychiatric symptoms can exacerbate the neuromotor symptoms of PD, complicating the care of patients with PD.[2,3] Previous research has suggested that psychiatric symptoms comorbid with PD decreases the quality of life for the patient and increases the burden on the caregiver.[4] However, the treatment options for psychiatric symptoms of patients with PD are limited. Currently, the main treatment strategies for these patients involve the use of dopamine agonists or selective serotonin reuptake inhibitors (SSRIs). This case report presents a PD patient with severe depression and anxiety who showed marked psychiatric improvement using hyperbaric oxygen treatment after refusing conventional pharmaceutical treatments.
2. Case report
The study was approved by the ethical committee of First Hospital of Jilin University, China. Written informed consent was obtained.
A 45-year-old male patient initially presented 1.5 years ago with resting tremor and bradykinesia in the left upper limb. Symptoms subsequently developed in the left lower limb and right limbs. He was diagnosed with PD, and anti-Parkinsonian agents were prescribed. The exact details of his prescription are unknown, as the patient refused any medication because he believed the drug treatment was ineffective.
Three months ago, the resting tremor and bradykinesia progressively intensified. Additionally, he began to present psychiatric symptoms, including a loss of interest in daily life, unwilling to communicate with others, and often having suicidal thoughts. He was diagnosed with severe depression and anxiety associated with PD at another hospital, and prescribed citalopram and pramipexole. However, again the patient refused to accept the drug treatment. At admission to our hospital, he had a poor diet, extremely inadequate sleep (about 2–3 hours per day on average), and weight loss of about 20 kg from the onset of PD. He had no previous history of medical illness. His mother had suffered from PD, with an initial onset around 40 years old. The neurological examination on admission found slightly clumsy speech patterns, masking face, and increased muscle tone and hyperactive deep tendon reflexes in the limbs. All other parameters of the neurological examination were within normal limits. In addition, nonenhanced cranial magnetic resonance imaging (MRI) scan and Doppler ultrasound of the head and neck did not identify any evidence of pathology. Depression and anxiety were assessed clinically using several rating systems, including the Unified Parkinson's Disease Rating Scale I (UPDRSI), UPDRS II, Hamilton Depression Rating Scale (HAM-D), and Hamilton Anxiety Rating Scale (HAM-A). The results are summarized in Table 1.
Table 1.
Patient scores on clinical tests before and after hyperbaric oxygen treatment.
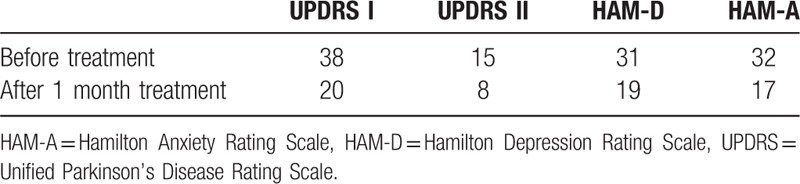
After admission, the patient again refused conventional drug treatment. He was instead treated with hyperbaric oxygen treatment as an alternative to pharmaceutical therapy. The protocols of hyperbaric oxygen treatment were as follows: the patient inhaled pure oxygen through a mask in 2 sessions of 40 minutes, separated by a 10 minute break, in hyperbaric chamber. The pressure was set at 2.0 ATA (atmosphere absolute). After 4 days of hyperbaric oxygen treatment, the patient had significantly improved sleeping quality, increasing sleeping duration from 2 to 3 hours prior to admission to about 5 hours per night. Coincidentally, his overall mood improved. The patient continued to receive hyperbaric oxygen treatment for 1 month. The treatment course was smooth and without complications. After ending treatment, the sleeping time recovered to within normal limits, with the duration of 8 to 10 hours, and body weight increased by about 10 kg. Additionally, the resting tremor and bradykinesia improved significantly. Table 1 summarizes the results of the clinical assessments performed both before and after the end of hyperbaric oxygen treatment. Although the scores after hyperbaric oxygen treatment decreased significantly, they remained in the abnormal range. Follow-up 1 month after discharge indicated that the improvements in the patient's sleep and mood persisted, and he did not need assistance in his daily life.
3. Discussion
PD occurs in 0.3% of the general population and about 1% to 2% of individuals older than 60 years.[5] Patients with PD often also suffer from depression and anxiety, which are the most common psychiatric complications for these patients. In fact, these 2 psychiatric disorders are more prevalent in PD patients than in the general population, with a lifetime risk of developing depression or anxiety of about 60%, with the cross-sectional prevalence for each disorder only being 30% to 40%.[1].
Idiopathic Parkinson disease is the most common cause of Parkinsonism, which has four cardinal manifestations including resting tremor, bradykinesia, rigidity, and gait disturbance.[6] Parkinson disease also causes important nonmotor symptoms, such as sleep disturbance, mood disorder, cognitive impairment, and autonomic dysfunction. The patient's initial symptoms presented in this paper were resting tremor and bradykinesia. Over time, he developed nonmotor symptoms, including sleep disturbance, and mood disorder. Affective disorders have a strong effect on quality of life and increase PD patient disability, so management of anxiety and depression for this patient, particularly because of his refusal of other drug treatments, was a priority.
Several medications are available for treatment of both the motor symptoms and nonmotor symptoms of PD. The choice of treatment for an individual patient is based on their specific symptoms, age, disease stage, functional disability, and general level of physical activity and productivity. In the clinic, levodopa or dopamine agonists, such as pramipexole, are the 2 recommended effective drugs for the treatment of the motor symptoms of PD.[7] Several randomized controlled trials have shown that dopamine agonists provide effective monotherapy in early PD, and in patients with more advanced disease who display suboptimal responses to levodopa.
Adverse effects can accompany the treatment with levodopa or dopamine agonists. For example, nausea, vomiting, and orthostatic hypotension may occur early in the treatment process of PD, whereas dyskinesia, visual hallucinations, and psychiatric symptoms sometimes occur after treatment in more advanced stages of the disease.[8] These adverse effects significantly decrease the treatment compliance in the clinic, and more efforts should be made to address them. Although motor function may worsen, stopping or reducing the levodopa or dopamine agonists to control the nonmotor symptoms, especially psychiatric symptoms, may be a better choice for the overall well-being of the patient. Additionally, selective serotonin reuptake inhibitors (SSRIs) may be effective in controlling the psychiatric symptoms. Psychiatric symptoms can exacerbate the debility of PD and create complexities in treating both the motor and nonmotor symptoms of patients with PD.
In the present study, the patient refused currently accepted drug therapies to treat his symptoms of PD. To treat this patient, we were compelled to explore other potentially effective treatment strategies. In recent years, hyperbaric oxygen treatment has emerged as a potential treatment for neurological disorders, including PD, by providing neuroprotective effects.[9,10] Several mechanisms underlying the neuroprotective effects of hyperbaric oxygen treatment in PD have been explored in the previous studies. One possibility is that hyperbaric oxygen treatment could reduce oxidative stress and inflammation, which are known factors in the pathogenesis of PD.[11] For example, in a rat model of middle cerebral artery occlusion, hyperbaric oxygen treatment dramatically reduced the formation of hydroxyl free radicals in the striatum, which was associated with increased superoxide dismutase and catalase activity and the reduction of malondialdehyde and lipid peroxidation levels.[12] Additionally, hyperbaric oxygen treatment is associated with reduced myeloperoxidase activity and inhibition of neutrophil infiltration, biomarkers indicating inflammation.[13,14] Although the potential mechanisms accounting for the effectiveness of hyperbaric oxygen treatment were not addressed for this patient, further studies should be conducted to verify the effectiveness of this treatment in other patients, as well as to understand the underlying molecular mechanism.
Studies have shown that hyperbaric oxygen treatment combined with other therapies is effective in improving the nonmotor symptoms of Parkinson's Disease.[15,16] However, a few report is available that evaluating the effects of hyperbaric oxygen treatment using specific scientific scales including UPDRSI, UPDRS II, HAM-D, and HAM-A as described in the present study. Further well-designed randomized controlled trials using abovementioned scientific scales are needed to evaluate the treatment efficacy.
In conclusion, this report suggests that hyperbaric oxygen treatment may be a potential therapeutic method for treating psychiatric symptoms in patients with PD. However, further research is needed to validate its effects and explore its mechanism.
Footnotes
Abbreviations: MRI = magnetic resonance imaging, PD = Parkinson's disease, SSRIs = selective serotonin reuptake inhibitors, UPDRS = Unified Parkinson's Disease Rating Scale I.
The authors declare no conflicts of interest.
References
- [1].Martinez-Martin P, Damian J. Parkinson disease: depression and anxiety in Parkinson disease. Nat Rev Neurol 2010;6:243–5. [DOI] [PubMed] [Google Scholar]
- [2].Chen JJ, Marsh L. Depression in Parkinson's disease: identification and management. Pharmacotherapy 2013;33:972–83. [DOI] [PubMed] [Google Scholar]
- [3].Chen JJ, Marsh L. Anxiety in Parkinson's disease: identification and management. Ther Adv Neurol Disord 2014;7:52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kano O, Ikeda K, Cridebring D, et al. Neurobiology of depression and anxiety in Parkinson's disease. Parkinsons Dis 2011;2011:143547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ahlskog JE. Parkinson disease treatment in hospitals and nursing facilities: avoiding pitfalls. Mayo Clin Proc 2014;89:997–1003. [DOI] [PubMed] [Google Scholar]
- [6].Latorre A, Bloise MC, Colosimo C, et al. Dyskinesias and motor symptoms onset in Parkinson disease. Parkinsonism Relat Disord 2014;20:1427–9. [DOI] [PubMed] [Google Scholar]
- [7].Ossig C, Reichmann H. Treatment strategies in early and advanced Parkinson disease. Neurol Clin 2015;33:19–37. [DOI] [PubMed] [Google Scholar]
- [8].Muller T. Pharmacokinetic considerations for the use of levodopa in the treatment of Parkinson disease: focus on levodopa/carbidopa/entacapone for treatment of levodopa-associated motor complications. Clin Neuropharmacol 2013;36:84–91. [DOI] [PubMed] [Google Scholar]
- [9].Neretin V, Lobov MA, Kotov SV, et al. Hyperbaric oxygenation in comprehensive treatment of Parkinsonism. Neurosci Behav Physiol 1990;20:490–2. [DOI] [PubMed] [Google Scholar]
- [10].Pan X, Chen C, Huang J, et al. Neuroprotective effect of combined therapy with hyperbaric oxygen and madopar on 6-hydroxydopamine-induced Parkinson's disease in rats. Neurosci Lett 2015;600:220–5. [DOI] [PubMed] [Google Scholar]
- [11].Mullin S, Schapira AH. Pathogenic mechanisms of neurodegeneration in Parkinson disease. Neurol Clin 2015;33:1–7. [DOI] [PubMed] [Google Scholar]
- [12].Ding Z, Tong WC, Lu XX, et al. Hyperbaric oxygen therapy in acute ischemic stroke: a review. Interv Neurol 2014;2:201–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Atochin DN, Fisher D, Thom SR, et al. Hyperbaric oxygen inhibits neutrophil infiltration and reduces postischemic brain injury in rats. Ross Fiziol Zh Im I M Sechenova 2001;87:1118–25. [PubMed] [Google Scholar]
- [14].Wang M, Yang H. Research advance about the effects of hyperbaric oxygen in ischemic stroke. Stroke 2010;9:9–14. [Google Scholar]
- [15].Li S. Effects of hyperbaric oxygen combined with rehabilitation in non-motor symptoms of Parkinson's disease. Neuro-injury and functional reconstructure 2015;10:261–3. [Google Scholar]
- [16].Pan Y, Luo M, Wang XY. Curative effect of pramipexole in combination with hyperbaric oxygen therapy in Parkinson's disease with dyssomnia. Chin J Geriatric Cardio-cerebral vas Dis 2016;18:125–8. [Google Scholar]


