Abstract
This study aimed to report our institution's experience in the diagnosis and treatment of chronic lateral ankle instability (CLAI) with ligamentum bifurcatum (LB) injury.
This retrospective study included 218 consecutive patients with CLAI who underwent surgery from January 2012 to December 2015. The 218 patients received tendon allograft reconstruction of the lateral ligament. CLAI was combined with LB injury in 51.4% (112/218) of patients. The 112 patients with concurrent LB injury had this treated simultaneously; 36 patients underwent excision of the anterior process of the calcaneus, 68 underwent LB repair, and 8 underwent LB reconstruction. Patients returned for a clinical and radiologic follow-up evaluation at an average of 31 (range, 24–35) months postoperatively. Outcomes were assessed by comparison of pre- and postoperative American Orthopaedic Foot and Ankle Society (AOFAS) scores, visual analog scale pain scores, Karlsson scores, and radiographic assessment.
Of the patients with concurrent LB injury, 82.1% (92/112) returned for final evaluation. Postoperatively, most patients recovered very well. However, the outcome was not ideal in those who underwent excision of the anterior process of the calcaneus; there were significant postoperative decreases in talar tilt (P < .05) and anterior drawer (P < .05), but there was no significant postoperative improvement in visual analog scale pain score and AOFAS score. Patients who underwent LB repair or reconstruction had an excellent or good outcome regarding patient subjective self-assessment, pain scores, Karlsson scores, and AOFAS scores at final follow-up.
Patients with CLAI often have concurrent LB injury. The diagnosis of LB injury can be missed or delayed. Clinicians should closely examine the LB in cases of CLAI, and should surgically repair or reconstruct the LB when necessary.
Keywords: ankle sprain, chronic lateral ankle instability, diagnosis and treatment, ligamentum bifurcatum injury
1. Introduction
Lateral ankle sprains are the most common musculoskeletal injury.[1,2] Especially in the active population, where lateral ankle sprain accounts for up to 20% of all sports-related injuries.[3,4] It is reported that 40.5% of patients with chronic lateral ankle instability (CLAI) have clinical signs of damage to the ligamentum bifurcatum (LB) of the midfoot[5]; missed or delayed diagnosis of LB injury is common, meaning that the true incidence of LB injury is probably higher.[6] Furthermore, LB injury has rarely been studied and is not frequently considered, so diagnosis of LB injury is not as easy as diagnosis of lateral ligament injury. However, the LB is essential for the stability of the transverse tarsal joint (Chopart lateral joint line).
The LB is a double ligament with a common origin on the lateral aspect of the anterior process of the calcaneus (APC).[7] It comprises with 2 components, medial and lateral. The medial component was comprised with the lateral calcaneonavicular ligament, which extends medially and anteriorly, and attached on the dorsolateral side of the navicular. The lateral component was comprised with the medial calcaneocuboid ligament, which extends anteriorly and anchored on the dorsomedial aspect of the cuboid. The calcaneonavicular part of the LB is thicker (average diameter 3 mm) and longer (average length 15 mm) than the calcaneocuboidal part (2 mm in diameter and 9 mm in length)[8] (Fig. 1).
Figure 1.
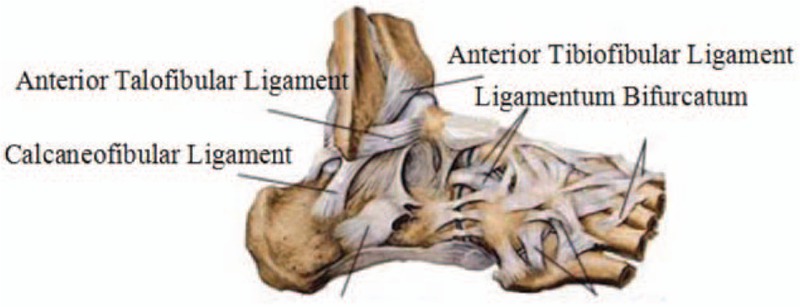
The anatomic location of the lateral ankle ligament and the LB. LB = ligamentum bifurcatum.
Patients with LB lesions experience substantially more pain in the region of the LB with radiation of pain to the forefoot compared with patients with only lesions in the region of the ankle joint. However, as patients with ankle sprain may have concurrent LB injury, the LB is often overlooked while the ankle joint is being examined.
We conducted this retrospective study with 2 aims: to investigate the incidence rate and characteristics of LB injury, and to identify the method of diagnosis and treatment of LB injury.
2. Materials and methods
This retrospective study included 218 consecutive patients with CLAI who underwent surgery from January 2012 to December 2015. In 51.4% (112/218) of these patients, CLAI was combined with LB injury. Our institutional review board approved the study, and all patients provided informed consent for study inclusion.
Inclusion criteria: history of CLAI for >6 months with pain, repeated episodes of ankle collapse, and swelling; positive anterior drawer test on physical examination; evidence of ankle instability on clinical or radiographic examination.[9–11]
Exclusion criteria: combined medial (deltoid ligament) and lateral ankle instability; local infection of the ankle joint; fracture of the tibia, fibula, talus, or calcaneus (except for the ankle avulsion of small bones).[12] Contraindications to this surgery included congenital collagen deficiency, bodyweight >120 kg, severe heart disease, lesions affecting liver and kidney function, severe diabetes, central nervous system diseases, and other medical diseases.
All included CLAI patients underwent allogeneic tendon reconstruction. Of the 112 cases of CLAI plus concurrent LB injury, 62 patients (55.4%) were men, and 50 (44.6%) were women. The average age at the time of surgery was 31.9 (range, 18–43) years. The left foot was involved in 69 cases (61.6%), and the right in 43 cases (38.4%). Thirty-six of the 112 patients had excision of the fracture fragment (the APC). Sixty-eight of the 112 patients underwent LB repair, and 8 underwent LB reconstruction using allogeneic tendon grafts. Median follow-up duration was 28 (range, 24–35) months.
Pre- and postoperative evaluation included history taking and physical examination, including the talus tilt test and anterior drawer test. Radiologic examinations were performed preoperatively and during final follow-up. As well as the routine anteroposterior and lateral radiographic views and oblique view of the midfoot (valgus 45°), computed tomography, and/or magnetic resonance imaging, some cases required varus stress radiography. As the calcaneocuboid joint is part of Chopart joint line, we also performed dorsoplantar, lateral, and stress radiographs with about 20 kp varus stress at the level of the calcaneocuboid joint to measure the calcaneocuboid angle.[13–15]
3. Operative procedures
Epidural anesthesia was administered, and the patient was placed in supine position with a thigh tourniquet. A curvilinear incision was then made approximately 7 cm below the lateral malleolus and along the peroneal muscle. The method used for reconstruction of the lateral ligaments of the ankle with allogeneic tendon grafts was the same as that used by Horibe et al.[16] When the anterior talofibular ligament and the calcaneofibular ligament were successfully reconstructed, the LB was checked for relaxation or complete rupture due to avulsion fracture. The operative procedure chosen depended on the fracture type. Surgical excision was performed for type I fractures (undisplaced fracture), while direct repair of the LB and fracture fragment fixation using a wire anchor was performed for type II fractures (displaced fracture that did not involve the articular surface, with a fracture fragment >2 mm). Type III fractures (large displaced fragment that involved the calcaneocuboid joint) underwent reconstruction with a graft. For LB reconstruction, the tendon was fixed to the calcaneus, the cuboid, and the navicular bones in turn at the LB attachment area with 5.0-mm resorbing screws (Depuy Mitek, MA) (Fig. 2). The incision was then rinsed with saline and sutured. The ankle joint was fixed in neutral position by lower leg plaster casting.
Figure 2.
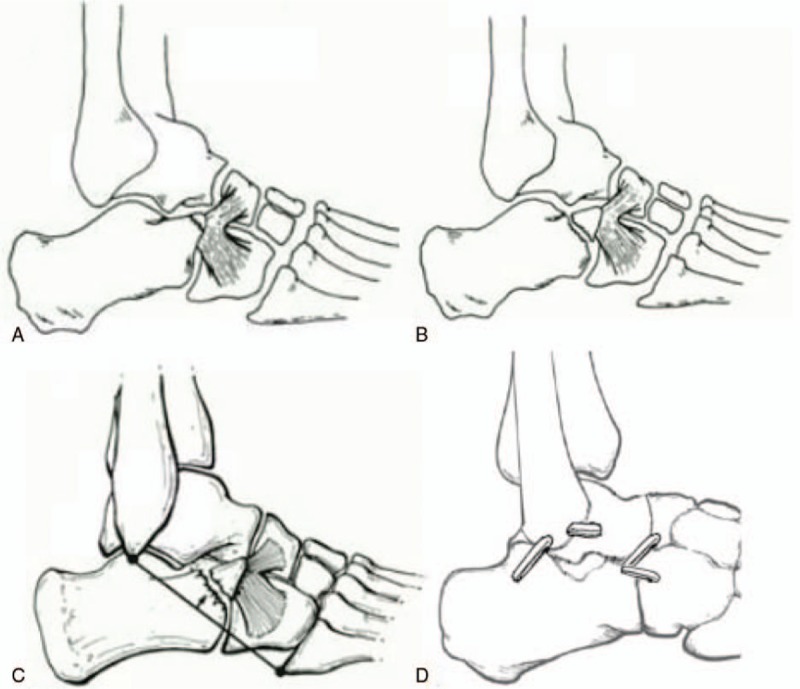
A: Type I fracture: undisplaced fracture; B: Type II fractures: displaced fracture; C: Type III fractures: large displaced fragment that involved the calcaneocuboid joint; D: Schematic drawing of the type III surgery method.
At 14 days postoperatively, the sutures were removed, and plaster fixation was applied for 4 weeks. After 4 weeks, the weight of the brace was partially loaded for 4 weeks. Walking exercise was permitted 10 weeks after the removal of auxiliary support, and patients were permitted to jog from 12 weeks postoperatively.
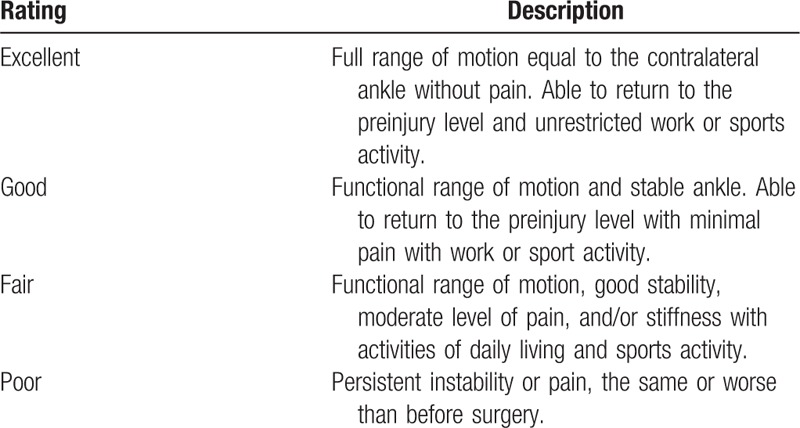
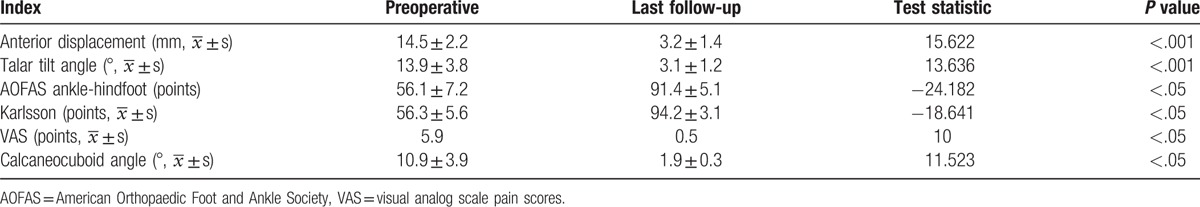
3.1. Efficacy evaluation criteria
Patients were asked to rate their overall satisfaction with the surgical results as “excellent,” “good,” “fair,” or “poor” (Table 1).[17] Outcomes were assessed by comparison of pre- and postoperative American Orthopaedic Foot and Ankle Society (AOFAS) scores, visual analog scale (VAS) pain scores, and Karlsson scores. All patients underwent pre- and postoperative radiographic assessment including talar tilt, anterior talar translation, and calcaneocuboid angle.
Table 1.
Clinical rating scale for postoperative ankle reconstruction[17].
4. Statistical analysis
Statistical analyses were performed with statistical software (SPSS version16.0; SPSS, Inc, Chicago, IL). The paired t test and Wilcoxon signed-rank test were used to determine the differences. Pre- and postoperative values (AOFAS ankle-hindfoot scores, VAS scores, Karlsson ankle scores, and radiologic measurements) of measurement. A P-value of <.05 was considered to indicate a statistically significant difference.
5. Results
Postoperatively, 98 patients with combined CLAI and LB injury returned for final evaluation (98 ankles; 87.5%), including 32 patients who underwent excision of the fracture fragment, 59 who underwent LB repair, and 7 who underwent LB reconstruction; 14 patients were uncontactable and were lost to follow-up. Of the patients who underwent excision of the fracture fragment, the surgical result was rated as excellent by 1/32 (3.1%) patients, good by 11/32 (34.4%) patients, and fair by 20/32 (62.5%) patients. Of the LB repair patients, the surgical result was rated as excellent by 55/59 (93.2%) patients, good by 3/59 (5.1%) patients, and poor by 1/59 (1.7%) patients. Of the LB reconstruction patients, the surgical result was rated as excellent by 6/7 (85.7%) patients, and poor by 1/7 (14.3%) patients.
The 1 patient who underwent LB repair and rated the surgical result as poor was very young (18 years old). The patient's parents were overly worried, and so she only began to partially weightbear at 2 months postoperatively. She did not complete the rehabilitation training, which led to ankle stiffness and an inability to return to the previous level of sports activity. However, ankle stress radiography showed that the patient had achieved mechanical stability. After 2 months of correct guidance and extracorporeal shockwave physiotherapy, the ankle stiffness had markedly improved. The patient who underwent LB reconstruction and rated the surgical result as poor was a 42-year-old man who had been involved in a motorcycle accident in which he sustained fractures of the right ankle; he returned to the hospital for open reduction and internal fixation of the calcaneal fractures, and recovered well after the second surgery.
At the time of final follow-up, 78.6% (77/98) of patients (92 ankles) were free of pain. Twenty patients had tenderness and clinically detectable swelling at the point of the LB, but the degree of ankle pain was significantly reduced compared with preoperatively. One patient reported mild pain after exercise with morning stiffness, but had no difficulty walking on even ground.
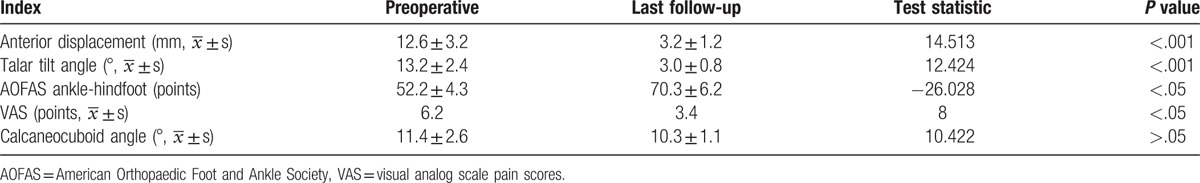
The VAS pain score was significantly reduced at the last follow-up compared with preoperatively (Table 2). The AOFAS score, Karlsson score, talar tilt angle, and anterior talar translation were improved significantly at final follow-up compared with preoperative values (Table 2). Mechanical stability was achieved in all cases. The calcaneocuboid angle was significantly reduced and the Chopart joint stability was significantly improved at final follow-up compared with preoperatively (Table 2).
Table 2.
Preoperative and final follow-up values of the assessed variables (n = 98).
6. Discussion
The most important finding of the present study was that diagnosis and treatment of LB injury resulted in significant improvements in AOFAS score, and achieved Chopart lateral mechanical stability without complications. Secondly, the incidence of LB was high in CLAI patients, >40% greater than the incidence described by Agnholt et al.[5]
We found that many patients with ankle instability also had Chopart lateral joint instability. In such cases, if we only repair the ankle joint and ignore the LB lesions, patients will still experience postoperative tenderness and swelling in the region of the LB. This is because the LB plays a very important role in maintaining the stability of the lateral transverse tarsal joint.
Patients with ankle sprain may have concurrent LB injury; so after examination of the ankle joint, the LB should be examined in detail (clinical side differences were noticed). In the present study, the LB was examined as described by Gellman[18] (Fig. 3); the extruding base of the fifth metatarsal can be palpated with the middle finger of the examiner, and the external malleolus be hold with the thumb, the marked tender point of the LB injury can be felt upon by the crooked index finger, between these 2 bones. If there were discoloration, local tenderness, or swelling at this area, the supplementary imaging will be ordered, including stress x-rays and oblique views of the midfoot. 80% patients with LB injury would present with all 3 clinical signs described above[17,19] (Fig. 4).
Figure 3.

Method of checking LB stability. LB = ligamentum bifurcatum.
Figure 4.
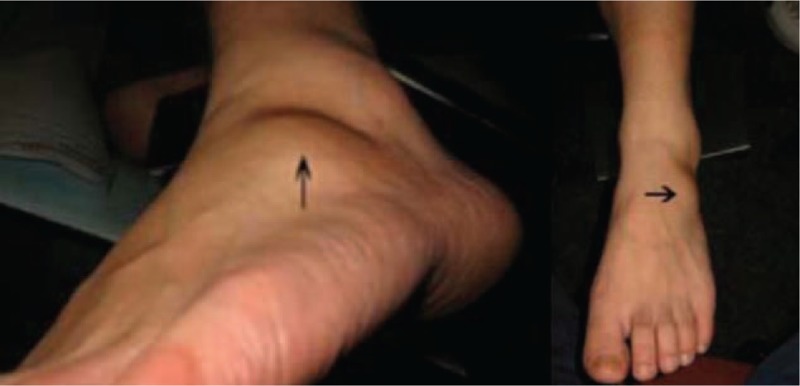
The patients with signs of swelling in the region of the LB. LB = ligamentum bifurcatum.
The LB is a major stabilizing factor for the lateral transverse tarsal joint (Chopart lateral joint line),[15] and so LB damage can result in laxity in the lateral part of the transverse tarsal joint; this can be demonstrated by the presence of a widened joint space in a roentgenogram performed while forcefully inverting the forefoot.[20] The LB also provides the main static stability of the lateral and medial columns, stabilizing the linking between the midfoot and the hindfoot.[15]
In patients with ankle sprain, anterior talofibular ligament injury may cause avulsion fracture. Similarly, LB injury may cause avulsion fractures of the APC.[19] These are the same mechanisms that produce a sprain of the anterior talofibular ligament of the ankle, which has been termed a sprainfracture. An epidemiological observational study of midtarsal joint sprain showed that the most frequent trauma mechanism was foot inversion (76% of cases), followed by plantar hyperflexion (21%), dorsal hyperflexion (2%), and foot eversion (1%)[6,18,21–24] (Fig. 5).
Figure 5.
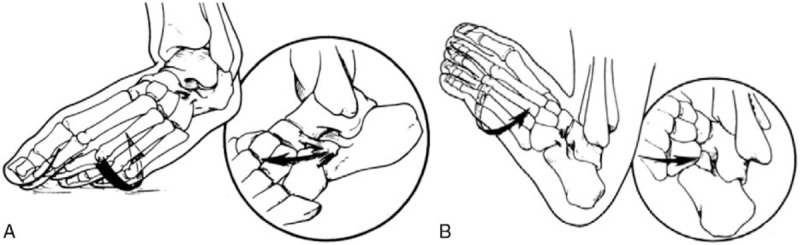
A: Inversion-adduction is the common mechanism causing the anterior talofibular ligament and the LB injury. B: An uncommon mechanism of fracture, consisting of dorsiflexion and eversion, causing a compression-type lesion. LB = ligamentum bifurcatum.
In routine examination of the foot, the avulsion of the APC can not be found, because on the lateral x-ray of the foot, the APC is projected on the talus. And so Backman and Johnson[22] and Parkes[25] proposes the oblique position of the foot (valgus 45), which will be clearly seen in this position (Fig. 6). Andermahr et al[14] suggested that lateral and stress radiographs with about 20 kp varus stress should be performed at the level of the calcaneocuboid joint, and then the calcaneocuboid angle should be measured. Under normal circumstances, the calcaneocuboid angle is <5°.[15] (Fig. 7).
Figure 6.

The APC is seen on the lateral view, but is projected over the talus. The oblique view clearly demonstrates the APC. APC = anterior process of the calcaneus.
Figure 7.
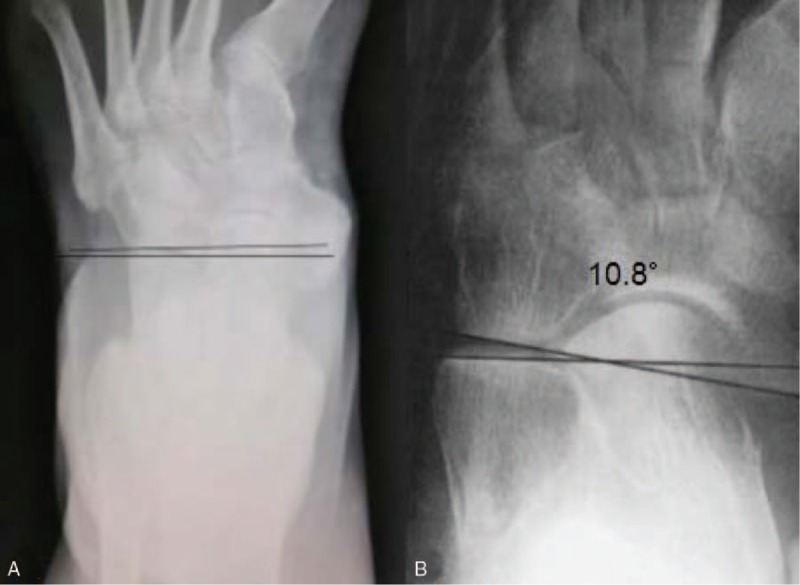
The calcaneocuboid angle at 20 kp varus stress. A: The calcaneocuboid angle is normal. B: The calcaneocuboid angle is 10.8°.
There are few reports of LB injury in the literature, and reports of diagnosis and treatment of LB injury are extremely rare. Hence, our treatment methods cannot be compared with those used by other organizations regarding the treatment and postoperative conditions. Our institution has treated 98 patients with lateral ligament injury combined with LB injury. Thirty-two patients were treated by excision of the APC, which resulted in a fair outcome; although the talar tilt and the anterior drawer were significantly reduced postoperatively, there were no significant improvements in VAS pain score, AOFAS score, and/or mean calcaneocuboid angle (Table 3). In contrast, patients who underwent LB repair or LB reconstruction showed significant improvements in VAS pain score and AOFAS score at the last follow-up. These results indicate that simple excision of the fracture fragment is not an ideal way to treat LB injury; it is worth mentioning that we cannot just excise the APC, as the scar tissue connection cannot compensate for LB function. Postoperatively, some patients still had clinically detectable signs (discoloration, tenderness, and swelling) at the point of the LB. Patients achieved satisfactory results after treatment with LB repair and reconstruction with an allograft, and achieved mechanical stability without serious complications. The results of the current study are encouraging, but LB repair and reconstruction is very complex, and surgeons need to have substantial experience to successfully treat such injuries. So we summarize the following experience for reference: in type I and type II injuries the fracture fragment should be removed and reconstructed with a wire anchor; cannulated screws were used to fix the fracture in type III patients, and the LB reconstruction was performed with autograft or allograft tendons.
Table 3.
Preoperative and final follow-up values of the assessed variables of excision of the fracture fragment (n = 32).
This study is limited by its retrospective nature. Furthermore, the senior surgeon performed the clinical evaluations subjectively, including the assessments of mechanical and functional stabilities, introducing the possibility of evaluation bias. Finally, as reports of LB injury are extremely rare, we cannot compare our method with methods used by other organizations. Further research is warranted to confirm the present findings.
7. Conclusion
Ankle sprain is often combined with LB damage. To reduce missed or delayed diagnosis of LB injury, CLAI patients should be thoroughly examined, and the LB should be treated via the method appropriate for the type of LB injury.
8. Author contributions
Fengqi Zhang designed the study; Yaning Sun, Yuchao Tang, Mingming Zhao, and Huijuan Wang inquired the EMR for variables of interest; Shiji Qin searched relevant literature and analyzed and interpreted the data; Yaning Sun and Huijuan Wang wrote the manuscript, and Fengqi Zhang approved the final version of the manuscript.
Acknowledgments
The authors are grateful to K. Liu and L. Zhang of the Department of Orthopedics, and to X. Song and G. Zhang of the Department of statistics and applications for their kind assistance.
Footnotes
Abbreviations: AOFAS = American Orthopaedic Foot and Ankle Society, APC = anterior process of the calcaneus, CLAI = chronic lateral ankle instability, LB = ligamentum bifurcatum, VAS = visual analog scale pain scores.
YS and HW have contributed equally to this work.
Funding support: This study was not supported by any funding.
All the authors declare that they have no conflict of interest.
References
- [1].Roos KG, Kerr ZY, Mauntel TC, et al. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med 2017;45:201–9. [DOI] [PubMed] [Google Scholar]
- [2].Donnelly L, Donovan L, Hart JM, et al. Eversion strength and surface electromyography measures with and without chronic ankle instability measured in 2 positions. Foot Ankle Int 2017;38:769–78. [DOI] [PubMed] [Google Scholar]
- [3].Doherty C, Delahunt E, Caulfield B, et al. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med 2014;44:123–40. [DOI] [PubMed] [Google Scholar]
- [4].Gerber JP, Williams GN, Scoville CR, et al. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int 1998;19:653–60. [DOI] [PubMed] [Google Scholar]
- [5].Agnholt J, Nielsen S, Christensen H. Lesion of the ligamentum bifurcatum in ankle sprain. Arch Orthop Trauma Surg 1988;107:326–8. [DOI] [PubMed] [Google Scholar]
- [6].Degan TJ, Morrey BF, Braun DP. Surgical excision for anterior-process fractures of the calcaneus. J Bone Joint Surg Am 1982;64:519–24. [PubMed] [Google Scholar]
- [7].Melão L, Canella C, Weber M, et al. Ligaments of the transverse tarsal joint complex: MRI-anatomic correlation in cadavers. AJR Am J Roentgenol 2009;193:662–71. [DOI] [PubMed] [Google Scholar]
- [8].Schmidt HM, Grünwald E. Ligament systems of talocrural and intertarsal joints in humans. Gegenbaurs Morphol Jahrb 1981;127:792–831. [PubMed] [Google Scholar]
- [9].Baumhauer JF, O’Brien T. Surgical considerations in the treatment of ankle instability. J Athl Train 2002;37:458–62. [PMC free article] [PubMed] [Google Scholar]
- [10].Knupp M, Lang TH, Zwicky L, et al. Chronic ankle instability (medial and lateral). Clin Sports Med 2015;34:679–88. [DOI] [PubMed] [Google Scholar]
- [11].Strauss JE, Forsberg JA. Chronic lateral ankle instability and associated conditions: a rationale for treatment. Foot Ankle Int 2007;28:1041–4. [DOI] [PubMed] [Google Scholar]
- [12].Kennedy JG, Smyth NA, Fansa AM, et al. Anatomic lateral ligament reconstruction in the ankle: a hybrid technique in the athletic population. Am J Sports Med 2012;40:2309–17. [DOI] [PubMed] [Google Scholar]
- [13].Lindner HO, Kaufner HK. Rupture of calcaneocuboid ligament. Zentr Bl Chir 1986;111:1250–4. [PubMed] [Google Scholar]
- [14].Andermahr J, Helling HJ, Rehm KE, et al. The vascularisation of the os calcaneum and the clinical consequences. Clin Orthop Relat Res 1999;212–8. [PubMed] [Google Scholar]
- [15].Andermahr J, Helling HJ, Maintz D, et al. The injury of the calcaneocuboid ligaments. Foot Ankle Int 2000;21:379–84. [DOI] [PubMed] [Google Scholar]
- [16].Horibe S, Shino K, Taga I, et al. Reconstruction of lateral ligaments of the ankle with allogeneic tendon grafts. J Bone Joint Surg Br 1991;73:802–5. [DOI] [PubMed] [Google Scholar]
- [17].Sammarco GJ, Idusuyi OB. Reconstruction of the lateral ankle ligaments using a split peroneus brevis tendon graft. Foot Ankle Int 1999;20:97–103. [DOI] [PubMed] [Google Scholar]
- [18].Gellman M. Fracture of the anterior process of the calcaneus. J Bone Joint Surg Am 1951;33-A:382–6. [PubMed] [Google Scholar]
- [19].Nielsen S, Agnholt J, Christensen H. Radiologic findings in lesions of the ligamentum bifurcatum of the midfoot. Skeletal Radiol 1987;16:114–6. [DOI] [PubMed] [Google Scholar]
- [20].Adler H. Ligamentous injuries of the foot arch. Orthop Trauma Surg 1982;99:183–7. [DOI] [PubMed] [Google Scholar]
- [21].Khalid FM, Abdulla AJ, Fahad A, et al. Weber B fracture of the lateral malleolus with concomitant anterior talofibular ligament injury following an ankle supination injury. Case Rep Orthop 2016;2016:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Bachman S, Johnson SR. Torsion of the foot causing fracture of the anterior calcaneal process. Acta Chir Scand 1953;105:460–6. [PubMed] [Google Scholar]
- [23].Plait AD. Fracture of the promontory of the calcaneus. Radiology 1956;67:386–90. [DOI] [PubMed] [Google Scholar]
- [24].Thiounn A, Szymanski C, Lalanne C, et al. Prospective observational study of midtarsal joint sprain: epidemiological and ultrasonographic analysis. Orthop Traumatol Surg Res 2016;102:657–61. [DOI] [PubMed] [Google Scholar]
- [25].Parkes J. Injuries of the hindfoot. Clin Orthop Relat Res 1977;28. [PubMed] [Google Scholar]


