Abstract
Rationale:
Video-based treatment in telemedicine is a potential alternative to face-to-face treatment. We describe our trial use of telemedicine to treat a patient with primary headache.
Patient concerns:
A 25-year-old woman visited our branch hospital with a chief complaint of recurrent headache. Our branch hospital had no headache specialist, so a headache specialist at our main hospital provided treatment remotely.
Diagnoses:
She was diagnosed with migraine without aura by the headache specialist using telemedicine.
Interventions:
The branch hospital physician and the headache specialist used video conferencing to interview and examine the patient and share cranial magnetic resonance imaging (MRI). Audio and camera angle/zoom could be adjusted during interviews, and high-quality video was continuously displayed at both hospitals simultaneously without lag between audio and video. Temporal/spatial resolution was sufficient for proper neurological evaluation. MRI had sufficient image quality and resolution for detailed interpretation. A prescription for medication was issued by the branch hospital physician and confirmed by the headache specialist.
Outcomes:
Zolmitriptan was effective in treating her migraine.
Lessons:
Telemedicine was useful for treating this primary headache patient and can contribute to regional health care. Future challenges in telemedicine include expanding its use to other areas within the purview of general physicians and headache specialists, covering implementation and maintenance costs, providing adequate explanations to patients and family members, ensuring security of video transmissions, maintaining patient medical records, and supervising treatment.
Keywords: face-to-face examination, face-to-face interview, medical treatment, primary headache, telemedicine
1. Introduction
Chronic headache affects around 40 million people in Japan, and headache sufferers experience varying degrees of impairment in daily life and at work.[1] Although a considerable number of chronic (primary) headache patients visit hospitals or clinics attended by headache specialists or general physicians, the “Clinical Practice Guideline for Chronic Headache” published by the Japan Headache Society (JHS) states that only around 50% of patients are accurately diagnosed and properly treated. Several reports in the literature argue that headache specialists play a useful role in the treatment of headache sufferers, and assert that general physicians who lack the equipment to perform cranial imaging such as computed tomography (CT) or magnetic resonance imaging (MRI) and who have trouble diagnosing the cause of the headache should promptly refer the patient to a headache specialist.[2–5] However, the number of headache specialists in Japan with expertise in the treatment of chronic headache is limited, at around 900 specialists in 2017. The development and spread of information and telecommunication technology (ICT) in recent years has created new possibilities for so-called telemedicine, where ICT devices are used to support the delivery of healthcare. There are growing expectations that telemedicine will be used to provide video-based treatment in place of traditional face-to-face treatment, but so far, there has been only limited uptake of telemedicine in the treatment of headache.
In this report, we describe the clinical utility of our attempt to use telemedicine to remotely treat a patient with primary headache via a connection between our branch hospital (which does not have a headache specialist) and our main hospital. In the context of this case, we describe this approach as “doctor-to-patient with doctor” telemedicine.
2. Case study
The patient was a 25-year-old female junior resident/intern with a chief complaint of recurrent headache. She did not have any remarkable past medical history and did not drink or smoke. From the age of 14 years, she started experiencing headaches in the superior left orbit several times a month. The headaches did not involve any visual aura but manifested as a throbbing sensation that continued for at least half a day with nausea in the absence of medication. She was examined at the internal medicine department of our branch hospital after a typical headache episode while working at the hospital as part of her residency.
Our branch hospital has no headache specialist, so we used the telemedicine system linking our main hospital which does have one, in order to have a face-to-face interview and examine the patient, to perform cranial MRI and electroencephalogram (EEG), to facilitate a discussion between the 2 physicians, and to prescribe medication, all via data and video transmission (Fig. 1-top). Our telemedicine program uses a video conferencing system (Life Size HD Visual Communication System; Hitachi High Technologies Corporation, Tokyo, Japan) comprising a 40-inch LCD monitor (Toshiba, Tokyo, Japan), camera, remote controller, and MicPod. The system enables real-time video-based communication via a high-speed internet connection [Nippon Telegraph and Telephone Corporation (NTT), Tokyo, Japan] between our main hospital and branch hospitals (Fig. 1-bottom).
Figure 1.
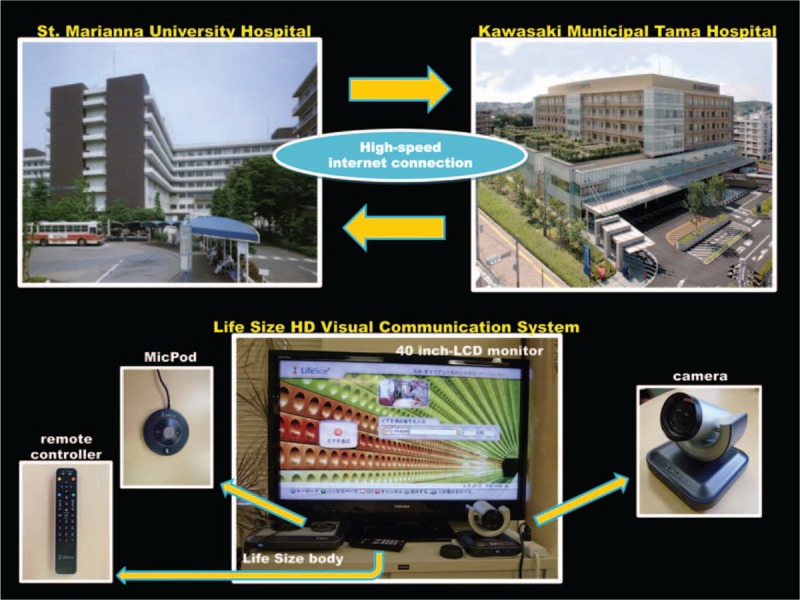
Our telemedicine system and interactive video conferencing system. Top: The telemedicine system operates via a high-speed NTT internet connection between our branch and main hospitals. Bottom: The interactive video conferencing system “Life Size HD Visual Communication System” (Hitachi High Technology Corporation) consists of a 40-inch LCD monitor, camera, remote controller, and MicPod.
2.1. Face-to-face interview
In the patient interview using our telemedicine system, we could adjust the audio and camera angle and zoom, and were able to maintain simultaneous video on each hospital's monitor without any disruption in image quality or lag between the audio and video. This setup allowed us to perform a detailed interview of the patient as though we were in the same room. We could also measure the patient's scores on the Migraine Disability Assessment Scale (MIDAS)[6] and Headache Impact Test-6 (HIT-6),[7] which are used to evaluate the extent to which a headache interferes with daily activities (Fig. 2).
Figure 2.
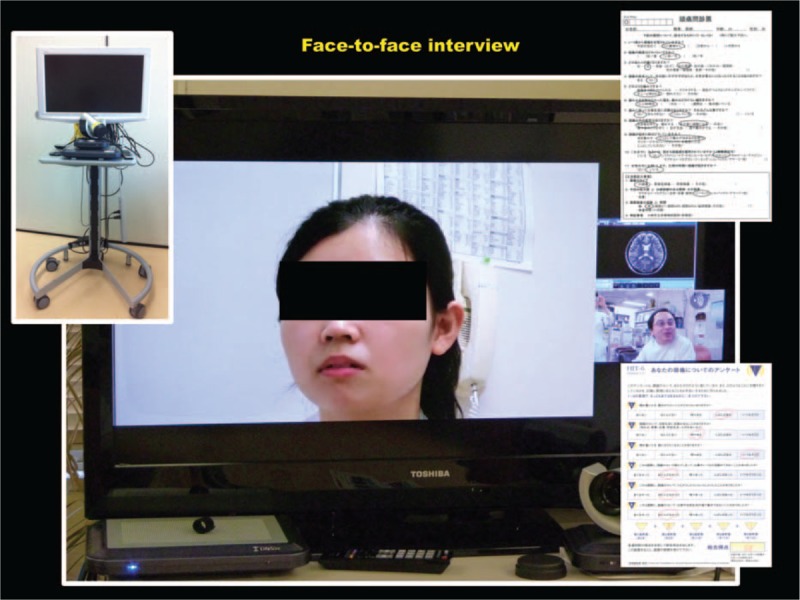
Face-to-face interview with the patient using the telemedicine system. We could adjust the audio and camera angle and zoom, and were able to maintain simultaneous video on each hospital's monitor without any disruption in image quality or lag between the audio and video.
2.2. Face-to-face examination
In addition to a physical examination, the physician at our branch hospital performed a neurological examination, including tests of consciousness, higher brain function, cranial nerves, motor system, reflexes, sensory system, and coordination. During these assessments, there was sufficient temporal and spatial resolution on both monitors (Fig. 3-left). In addition, the headache specialist at our main hospital could issue the necessary instructions and obtain clear, close-up images of the patient's eyes allowing us to evaluate the pupillary light reflex findings, which are generally difficult to examine on a monitor (Fig. 3-right).
Figure 3.
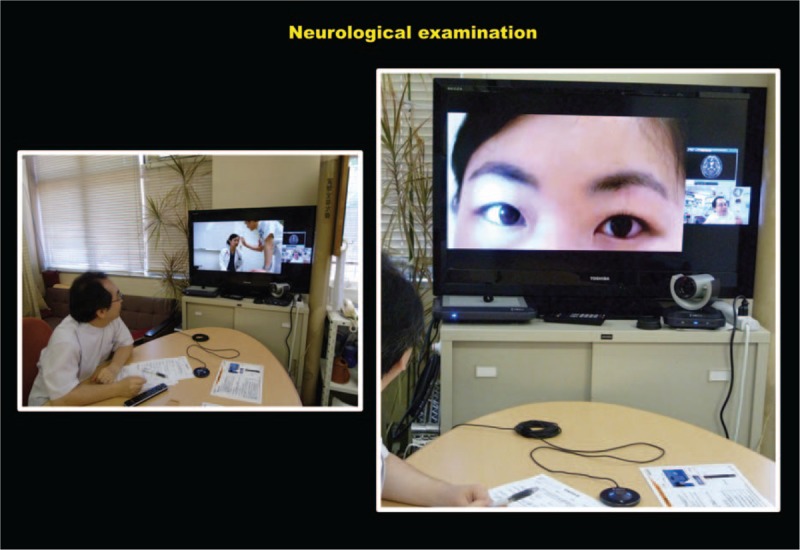
Face-to-face examination using the telemedicine system. In addition to a physical examination, the physician at the branch hospital performed a neurological examination, including tests of consciousness, higher brain function, cranial nerves, motor system, sensory system, and coordination. During these assessments, there was sufficient temporal and spatial resolution on both monitors.
2.3. Transmission of test results
Image quality and resolution were sufficient to enable detailed interpretation of the cranial MRI and EEG waveforms (Fig. 4-top). No abnormal findings were apparent on these images.
Figure 4.
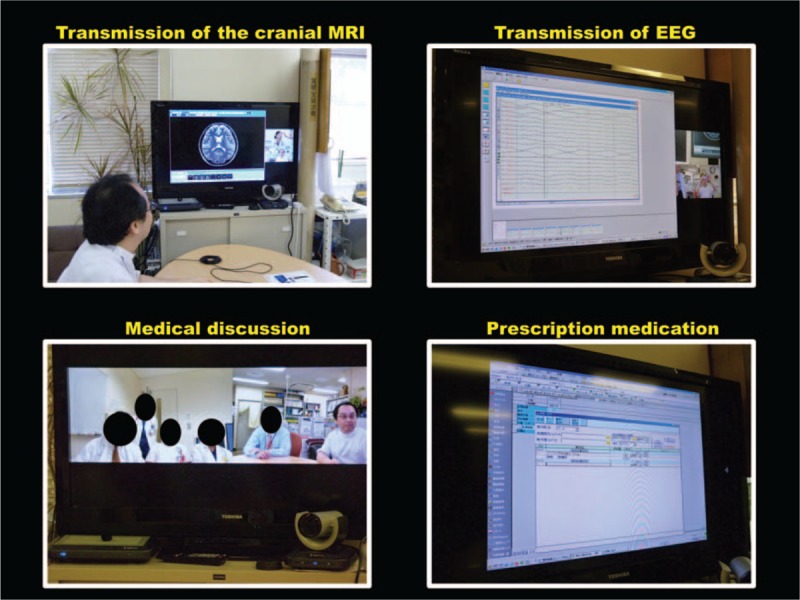
Data transmission, diagnosis, explanation to the patient, and prescription using the telemedicine system. Top: The cranial MRI and EEG also had sufficient image quality and resolution to enable detailed interpretation. Bottom left: We could also have a medical discussion in real time by gathering the physicians from both hospitals in front of the monitors. Bottom right: The headache specialist at the main hospital advised the nonspecialist physician at the branch hospital on the appropriate course of treatment. The branch hospital physician then issued a prescription for medication, which the headache specialist could visually confirm via the video link.
2.4. Diagnosis, explanation to the patient, and medical discussion
The headache specialist had no difficulty explaining the diagnosis and cause of the headache to the patient in real time using diagrams. We could also have a medical discussion in real time between the 2 physicians in front of the monitors (Fig. 4-lower left). The diagnosis reached was migraine without aura.
2.5. Prescription medication
The headache specialist advised the appropriate course of treatment to the branch hospital physician, who then issued a prescription for medication. The specialist was also able to visually confirm the prescription (Fig. 4-lower right). Zolmitriptan was effective in treating her migraine.
3. Discussion
Headache is a common illness among outpatients, and migraine in particular has been identified by the World Health Organization as the 19th highest cause worldwide of years lost to disability. However, despite the fact that headache, particularly primary headache, can cause significant interference in daily life and at work, only a small percentage of headache sufferers visit a clinic or hospital for treatment.[1,8] This situation can be attributed to several factors, including the following: a lack of awareness of headache as a legitimate illness; unwillingness to take time off work to visit the doctor due to feelings of guilt; attempts to remedy headaches with over-the-counter medication due to not knowing which doctor, clinic, or hospital to visit; and the tendency among general practitioners to treat consultations as one-off visits and prescribe analgesics without proper treatment after diagnosing the patient's condition as a simple headache while ruling out organic diseases on the basis of image findings. Furthermore, migraine is no longer the primary form of headache in adults alone, it is a serious problem for children as well. In the case of younger children who cannot yet express themselves, a nonspecialist physician may not be able to diagnose migraine. As a result, and despite reports in the literature describing the effectiveness of consulting a headache specialist with expertise in the treatment of chronic headache, as of 2017, there are only 900 headache specialists in Japan who are accredited by the JHS. Given that migraine is estimated to affect around 8.4 million people in Japan,[1] this means that each headache specialist would have to examine around 10,000 migraine patients, which is obviously infeasible. There are also regional disparities between Japan's urban and rural communities, such as a lack of even general practitioners in rural areas, so opportunities to visit headache specialists are obviously limited for patients who would have to travel long distances.
The type of telemedicine that we performed in this case would prove useful for clinics and hospitals without a headache specialist. Patients could overcome the geographical restraints of having to travel long distances to see a specialist and could have a new consultation and receive proper diagnosis and treatment from a facility with a headache specialist without the physical burden associated with an actual visit. Also, the headache specialist can not only diagnose migraine but also advise families of children with migraine by utilizing their knowledge of comorbidities such as low-quality emotional functioning, absenteeism from school, poor academic performance and cognitive functioning,[9,10] motor coordination impairment,[11] and sleep disorders,[12–18] which are common in children affected by migraine. Telemedicine also allowed our headache specialist to issue real-time instructions to the branch hospital physician on the techniques required to examine the patient, such as palpation and auscultation. Moreover, the physicians could consult before deciding on how the test data should be interpreted and which medication could be prescribed. Our experience suggests that this type of telemedicine system is an effective tool in the treatment of headache patients because it enables specialists to transmit the information required to perform a medical intervention. It also allows general practitioners in more remote areas where there is no specialist—especially general practitioners who do not specialize in internal medicine—to examine and treat the patients while receiving instructions from a specialist at a separate geographic location.
In terms of legislation, telemedicine was previously prohibited under Article 20 of the Medical Practitioners Act, which states that “No medical or dental practitioner shall provide medical care without personally performing a face-to-face examination, and telemedicine shall be performed only in a manner that complements face-to-face medical care.” However, the practice of telemedicine was legalized in December 1997 following issuance of a notification by the Ministry of Labour, Health and Welfare stating that “The practice of telemedicine does not directly infringe on Article 20 of the Medical Practitioners Act provided that it can be used to obtain useful information on the patient's physical or mental condition to the extent that it can be used as an alternative to face-to-face medical treatment even if it is not equivalent.” Indications for telemedicine were rapidly expanded in March 2011 to allow mainly doctor-to-patient treatments of chronic-stage patients who are receiving ongoing therapy and whose recent condition has been stable. These changes have led to the use of telemedicine not only in-home care situations but also on a trial basis in hyperacute stroke patients[19–22] in a doctor-to-patient with doctor setting.
The telemedicine system used by our hospitals’ nonspecialist physician and headache specialist to treat the present patient also proved to be effective and appears to share some similarities with telemedicine in other disease areas. However, a number of challenges remain, such as establishing the necessary infrastructure (e.g., communication networks, computer equipment, standardized specifications), covering the costs of implementing and maintaining this equipment, providing adequate explanations to patients and family members, ensuring the security of patient video transmissions, establishing a technique to maintain patient medical records, assigning suitable medical personnel to supervise the treatment, and covering the costs associated with developing financial incentives and remuneration.
It should be noted that certain circumstances in this case likely made our telemedicine approach successful. The telemedicine system used to treat the patient's primary headache made use of an existing high-speed NTT internet connection between our branch and main hospitals, and it had already been used to provide care to hyperacute stroke patients. Moreover, the treatment went smoothly because the patient was a junior resident who consented to participate in the use of telemedicine. Telemedicine performed at a different facility may not proceed as smoothly.
4. Conclusion
Our findings suggest that telemedicine can be used by a general physician and a headache specialist to facilitate treatment of patients with primary headache and can make a meaningful contribution to regional health care in the future. We believe that this case provides valuable insights for the development and spread of telemedicine in Japan. Future challenges to the use of telemedicine include expanding its use to other areas, covering the costs of implementing and maintaining the equipment, providing adequate explanations to patients and family members, ensuring the security of patient video transmissions, establishing a technique to maintain patient medical records, assigning suitable medical personnel to supervise the treatment, and covering the associated costs.
Acknowledgments
We thank Dr Kanako Teramoto and Dr Masahiro Horiuchi from the Department of Internal Medicine, Division of Neurology of Kawasaki Municipal Tama Hospital for the cooperation and participation in this telemedicine trial.
Footnotes
Abbreviations: CT = computed tomography, EEG = electroencephalogram, ICT = information and telecommunication technology, JHS = Japan Headache Society, MRI = magnetic resonance imaging.
Authorship: HA examined the patient by using telemedicine. HA drafted the manuscript and created the figures. YH helped to draft the manuscript. All authors read and approved the final manuscript.
St. Marianna University Hospital Human Research Ethics Committee waived approval because this is a case report.
Written informed consent for publication was obtained from the patient herself. A copy of the consent form is available for review by the Editor of this journal.
The authors declare that they have no competing interests.
References
- [1].Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia 2002;46:343–9. [DOI] [PubMed] [Google Scholar]
- [2].Lipton RB, Scher AI, Steiner TJ, et al. Patterns of health care utilization for migraine in England and in the United States. Neurology 2003;60:441–8. [DOI] [PubMed] [Google Scholar]
- [3].Lipton RB, Stewart WF, Simon D. Medical consultation for migraine: results from the American Migraine Study. Headache 1998;38:87–96. [DOI] [PubMed] [Google Scholar]
- [4].Bekkelund SI, Salvesen R. Are headache patients who initiate their referral to a neurologist satisfied with the consultation? A population study of 927 patients-the North Norway Headache Study (NNHS). Fam Pract 2001;18:524–7. [DOI] [PubMed] [Google Scholar]
- [5].Bekkelund SI, Salvesen R. Patients satisfaction with a neurological specialist consultation for headache. Scand J Prim Heath Care 2002;20:157–60. [DOI] [PubMed] [Google Scholar]
- [6].Stewart WF, Lipton RB, Kolondner KB, et al. Validity of the migraine disability assessment (MIDAS) score in comparison to a diary-based measure in a population sample of migraine sufferers. Pain 2000;88:41–52. [DOI] [PubMed] [Google Scholar]
- [7].Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res 2003;12:963–74. [DOI] [PubMed] [Google Scholar]
- [8].Takashima T, Ishizaki K, Fukuhara Y, et al. Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache 2004;44:8–19. [DOI] [PubMed] [Google Scholar]
- [9].Kernick D, Campbell J. Measuring the impact of headache in children: a critical review of the literature. Cephalalgia 2009;29:3–16. [DOI] [PubMed] [Google Scholar]
- [10].Esposito M, Pascotto A, Gallai B, et al. Can headache impair intellectual abilities in children? An observational study. Neuropsychiatr Dis Treat 2012;8:509–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Esposito M, Verrotti A, Gimigliano F, et al. Motor coordination impairment and migraine in children: a new comorbidity? Eur J Pediatr 2012;171:1599–604. [DOI] [PubMed] [Google Scholar]
- [12].Carotenuto M, Guidetti V, Ruju F, et al. Headache disorders as risk factors for sleep disturbances in school aged children. J Headache Pain 2005;6:268–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Vendrame M, Kaleyias J, Valencia I, et al. Polysomnographic findings in children with headaches. Pediatr Neurol 2008;39:6–11. [DOI] [PubMed] [Google Scholar]
- [14].Carotenuto M, Esposito M, Precenzano F, et al. Cosleeping in childhood migraine. Minerva Pediatr 2011;63:105–9. [PubMed] [Google Scholar]
- [15].Carotenuto M, Esposito M, Pascotto A. Migraine and enuresis in children: an unusual correlation? Med Hypotheses 2010;75:120–2. [DOI] [PubMed] [Google Scholar]
- [16].Esposito M, Gallai B, Parisi L, et al. Primary nocturnal enuresis as a risk factor for sleep disorders: an observational questionnaire-based multicenter study. Neuropsychiatr Dis Treat 2013;9:437–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Esposito M, Roccella M, Parisi L, et al. Hypersomnia in children affected by migraine without aura: a questionnaire-based case-control study. Neuropsychiatr Dis Treat 2013;9:289–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Esposito M, Parisi P, Miano S, et al. Migraine and periodic limb movement disorders in sleep in children: a preliminary case-control study. J Headache Pain 2013;14:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke system of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke 2009;40:2616–34. [DOI] [PubMed] [Google Scholar]
- [20].Schwamm LH, Audebert HJ, Amarenco P, et al. Recommendations for the implementation of telemedicine within stroke systems of care: a policy statement from the American Heart Association. Stroke 2009;40:2635–60. [DOI] [PubMed] [Google Scholar]
- [21].Meyer BC, Lyden PD, Al-Khoury L, et al. Prospective reliability of the STRokE DOC wireless/site independent telemedicine system. Neurology 2005;64:1058–60. [DOI] [PubMed] [Google Scholar]
- [22].Sakurai K, Imai T, Kato B, et al. Feasibility of NIH stroke scale evaluation and telestroke use via an interactive high-vision videoconferencing system. Jpa J Stroke 2012;34:414–20. [Google Scholar]


