Abstract
Objective
Academic medical centers (AMCs) in North America are expanding their missions from the traditional triad of patient care, research, and education to include the broader issue of healthcare delivery improvement. In recent years, integrated Critical Care Organizations (CCOs) have developed within academic centers to better meet the challenges of this broadening mission. The goal of this article is to provide interested administrators and intensivists with the proper resources, lines of communication, and organizational approach to accomplish integration and CCO formation effectively.
Participants
The Society of Critical Care Medicine convened a taskforce entitled “Academic Leaders in Critical Care Medicine” on February 22, 2016 at the 45th Critical Care Congress using the expertise of successful leaders of advanced governance CCOs in North America to develop a toolkit for advancing CCOs. The Academic CCO Building section workgroup of the taskforce established regular monthly conference calls over the past year to reach consensus on the development of a toolkit utilizing methods proven to advance the development of their own academic CCOs.
Data Sources and Synthesis
Relevant medical literature was reviewed by literature search. Materials from federal agencies and other national organizations were accessed through the internet. Key elements of an academic CCO are outlined. The vital missions of multidisciplinary patient care, safety, and quality are linked to the research, education, and professional development missions that enhance the value of such organizations. Core features, benefits, barriers, and recommendations for integration of academic programs within CCOs are described. Selected readings and resources to successfully implement the recommendations are provided. Communication with medical school and hospital leadership is discussed.
Conclusions
We present the rationale for critical care programs to transition to integrated CCOs within academic medical centers and provide recommendations and resources to facilitate this transition and foster CCO effectiveness and future success.
Keywords: academic, critical care, critical care organization, education, professional development, research, quality improvement, patient safety
Introduction
Academic medical centers (AMCs) in North America are facing the need to evolve in response to a health care market that demands greater efficiency, lower cost, and more accountability (1). While each AMC will evolve differently depending on local conditions and preferences, streamlined “corporate-style” structures are poised to replace traditional administrative organizations through greater horizontal and vertical integration (1, 2). As a vital part of clinical operations, Critical Care Medicine (CCM) services are subject to the same market forces and evolutionary demands. Several AMCs have already chosen to integrate these services into larger Critical Care Organizations (CCOs) (3). This integration was most often initiated by hospital administration (3), and resulted in improvement of a variety of metrics including quality of care, patient satisfaction, resource use, support of hospital leadership, and in some cases hospital cost of care (4).
In the first article of this “how-to” series regarding CCO development, Leung et al presented the rationale for integration of the business and operations aspects of Critical Care and provided a roadmap for horizontal and vertical integration (4). The integrated multidisciplinary patient care, safety, and quality programs that are characteristic of CCOs may add value to the care of critically ill patients by focusing on improving outcomes and lowering cost (4,5). While these programs are central to healthcare delivery in the intensive care unit (ICU), the additional academic missions of research, education, and professional development programs may contribute to this value through dissemination of knowledge and support of discovery and innovation. These academic missions, however, are expensive to maintain, often requiring significant subsidization from revenue generated from clinical care (1). Integration of academic programs may lower costs by maximizing resource utilization, improve efficiency by reducing duplication of efforts, and result in better academic products through enhanced collaboration. We now continue the CCO development discussion by presenting concepts of academic program integration within CCOs as well as specific benefits, barriers, and recommendations pertaining to such integration.
Perceptions of Academic Program Integration
Data from a recent survey of 24 CCOs in North America by Leung et al (4) supports integration and CCO development. All CCOs reported improvements in quality of care, patient satisfaction, resource utilization, and support from hospital leadership following integration; and a majority of respondents reported improved hospital cost of care (3, 4). Notably, the impetus to transition to an integrated CCO is not limited to the CCM programs themselves. A recent description of 24 integrated CCOs in North America demonstrated that almost half (46%) of such transitions were initiated by hospital administration (3). This kind of data is lacking for integration of academic programs within CCOs; however, there is empiric data and expert opinion that falls on both sides of the issue (1, 6–8). Perhaps the biggest argument supporting integration is economy of scale. Horizontal integration provides flexibility and reliability benefits resulting from consolidation of resources, and improved accountability for academic endeavors similar to the improved accountability of single governance seen from the business and operations standpoint (3, 4). Additionally, integration often results in placing different disciplines in closer administrative and physical proximity, encouraging communication and academic collaboration in some instances (6). Anecdotal evidence demonstrates improved research and education efforts (8), and this broader collaboration is thought to be key to improving CCM research (9). Finally, proponents point to the potential for integration to control costs through greater efficiency (6).
Arguments opposing integration include the potential loss of individual program autonomy and visibility to the larger CCO. Attempts at integration in the absence of collaboration amongst CCO members may result in failure, with academic program directors possibly feeling that the loss of such autonomy forces them to accept decisions that are not in the best interest of their own program. Integration is complex and requires strong leadership within the institution to convince key stakeholders such as the medical school Dean and department chairs to undergo organizational change. Many department chairs and division chiefs will resist transferring traditional authority and autonomy of clinical and academic programs to the CCO leadership (7), and power struggles are likely to ensue as different departments attempt to lay claim to as much authority within the CCO as possible. Recruitment and retention of faculty may also be affected for those who are more comfortable with the traditional academic structure and have concerns about their own academic advancement within an integrated system (7), though there is some evidence that recruitment and retention are improved through integration (4). The financial benefit of integrating academic programs has limited data and is still unclear (7). Without such clear benefit, traditional academic silos will be more difficult to bridge. Some circumstances even discourage integration, such as a lack of a unified Critical Care specialty board examination, salary disparities between departments that would contribute to a CCO, or the adoption of different residency review committee (RRC) requirements for different CCM training programs (10–14).
All of these perceptions and the weight given to them by AMC and Critical Care leadership will determine whether a given institution is more or less enthusiastic about evolving Critical Care academic programs from their traditional structure. Strong and willing leadership will indeed be required (15); however the possibility of developing more efficient, reliable, and accountable academic programs and the possibility of reducing the number of clinical dollars needed to support these programs will prove compelling. New CCOs may first integrate clinical and business operations in response to current market conditions (4); however the individual divisions and departments contributing to the CCO are likely to also want to support their academic interests at lower cost. Administrative and physical proximity as well as the potential of better productivity through improved collaboration will also encourage academic integration.
Once integrated, the academic programs within the CCO must demonstrate enthusiasm for aligning goals and collaborating with other departments. Failure to do so will undermine the ability of CCOs to affect institutional improvement and improve patient care, resulting in decreased empowerment, effectiveness, and academic prestige. As the concerns of loss of autonomy, influence, and academic advancement are addressed with forethought and care, a stronger and more sustainable CCO will emerge. Integration will not follow a single pathway, but instead be based on local conditions and priorities. While the most common organizational models of current CCOs are free standing Critical Care Departments (38%) and Critical Care Centers (21%) there are a number of other organizational arrangements that represent a wide variety of strengths, responsibilities, collaborations, and reporting relationships that may work better for a given institution (3, 16). Whatever the pathway of integration, we offer the following set of recommendations to help institutions with this important transition.
Initial Steps toward Academic Integration
Integration of academic programs may follow or be concurrent with the integration of business and clinical operations. It is unlikely that academic integration would precede business integration given the economic drivers of the latter (4). While the details of integrating academic programs may vary greatly between institutions, the initial steps of introspection, outreach, collaboration, and communication with medical school and hospital administration should be similar (Table 1).
Table 1.
Initial steps of Integration
| Steps | Recommendations |
|---|---|
| Introspection |
|
| Outreach |
|
| Collaboration |
|
| Communication |
|
Even after an integrated CCO has been developed, continued efforts are needed to maintain its efficacy. A CCO is most successful and overall health care delivery improved when its clinical, academic, and financial goals align with those of hospital and academic leadership, when lines of communication are maintained between CCO and institutional leadership, and when opportunities to collaborate with clinical departments outside the CCO are actively pursued. Finally, demonstrating milestones of achievement and relaying those milestones to key stakeholders is an important factor for CCO success, particularly during the initial development phase when momentum for change is fragile (17).
Key Elements of CCOs
The key academic elements of CCOs include patient care and safety, quality, research, education, and professional development. These elements are closely linked to one another and to value-based care (Figure 1). For AMCs that feature most if not all of these elements, the full potential to enhance value-based care cannot be realized without integration of a broad range of missions. Table 2 lists the key elements of academic CCOs, core features specific to each element, and general aims for integration. Common to all of these elements are the need for buy-in from hospital and medical school leadership, fiscal understanding and oversight, close communication between stakeholders, and collaborative efforts both within and outside the CCO.
Figure 1. Relationship of Academic CCO Missions to Value-Based Care.
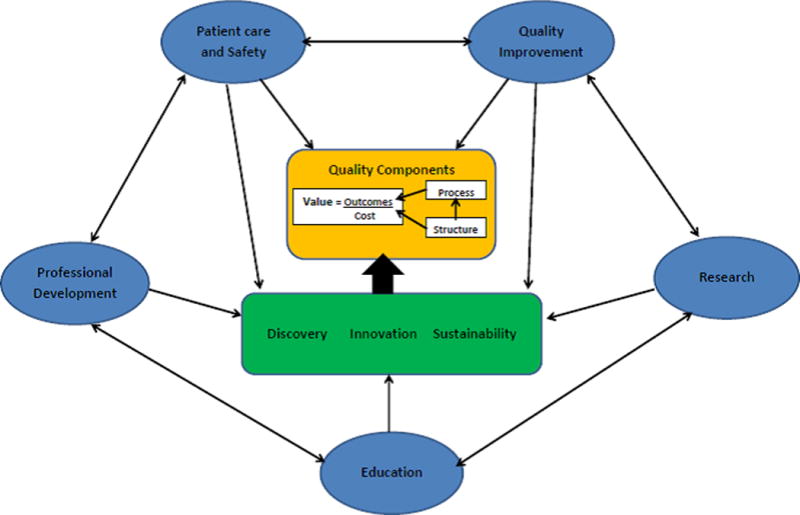
Patient Safety and Quality programs directly add to the value of patient care by improving outcomes and reducing cost. Other academic missions such as research, education, and professional development also contribute to value through supporting the patient safety and quality missions as well as contributing to discovery, innovation, and the sustainability of the CCO. (Adapted with permission from Murphy DJ, Ogbu OC, Coopersmith CM. ICU director data: using data to assess value, inform local change, and relate to the external world. Chest. 2015 Apr;147(4):1168–78)
Table 2.
Key Elements of Critical Care Organizations
| Element | Core Features | General Goals for Integration |
|---|---|---|
| Patient Care and Safety |
|
|
| Quality Improvement |
|
|
| Research |
|
|
| Education |
|
|
| Professional Development |
|
|
Patient Care and Safety Program
The provision of safe patient care remains the most important mission of AMCs and is particularly focused on patient outcome and value (4). The association between improved patient outcomes and inter-professional collaboration has been well established (18–20). Patient care and safety programs within CCOs must establish a culture of collaboration for solving complex patient care delivery issues. This culture should include reporting, review, and open discussion of adverse events; patient safety education; and checklist development (21). Educational experiences, including high-fidelity simulation (21), may enhance safety knowledge and behavior of inter-professional healthcare teams.
In addition to interdisciplinary collaboration, CCOs should develop a patient care delivery structure that features an electronic medical record (EMR) system that aids decision making, reduces waste, optimizes security of personal information, and minimizes interoperability problems between different medical information systems. Practitioners must be able to efficiently report adverse events (21) and information should flow seamlessly between hospital departments, communicating with frontline clinicians as well as leadership. While current generation EMR systems reduce medication errors through improved legibility (22) and improve adoption of proven therapies (23), future EMR generations may reduce delays in care and lower costs through clinical decision support (24–26). CCO leadership must advocate for those EMR features that will improve value. Digital Supplement 1 lists specific benefits, barriers, and recommendations for patient care and safety programs.
Finally, the alignment of patient care and safety program objectives with those of hospital leadership and other clinical departments within the institution is particularly important. Such broad collaboration enhances visibility of the CCO and strengthens its central position within the AMC as a necessary confederate for addressing hospital-based clinical issues. Failure to align goals and collaborate with other departments undermines the ability of CCOs to affect institutional improvement and results in decreased empowerment, effectiveness, and sustainability.
Quality Improvement Program
Quality Improvement (QI) programs are similar to patient safety programs with respect to their direct connection to value (Figure 1). Much has been written on how to create a highly functioning interdisciplinary QI program within an ICU (27–30). Digital Supplement 2 presents specific benefits, barriers, and recommendations for QI programs, particularly with respect to metrics, design and implementation, education, and information technology.
In the setting of an integrated CCO, QI projects must extend across ICUs as well as across professional disciplines and should be based on explicitly defined metrics. These metrics should be linked to specific QI program objectives and expected clinical outcomes based on hospital and CCO goals (5, 31). Information technology (IT) support must be leveraged in order to appropriately measure desired metrics (22). In addition to ICU-specific projects, metrics used for the CCO QI program may involve projects that extend outside the ICU (32). Critical Care QI programs should take the lead in developing both ICU-specific clinical protocols and protocols that partner with other departments to address issues that interface with Critical Care. If available, an integrated QI organization within the AMC may be leveraged to support specific projects, encourage multidisciplinary involvement, and assist with developing QI expertise through formal training programs. Growing partnerships between healthcare systems and industrial and systems engineering will further advance the efficiency and effectiveness of the design, education, and implementation of critical care QI programs in the future (33).
Research Program
Successful CCO research programs must pursue broad intramural and extramural collaboration and consolidation of both academic and administrative resources. The integration plan must seek to remedy barriers to research innovation and progress, including suboptimal collaboration among different healthcare professionals, an overly narrow focus on specific organ system research, and failure to use the expertise and insights of other non-medical disciplines (9). The goal of such an integrated research program is to improve overall research quality, productivity, and funding with relative cost savings resulting from resource consolidation. Specific deliverables include grant funding, promotion and national visibility of faculty, and development of a research mentor pool to enhance the professional careers of early-career physician-scientists. Digital supplement 3 describes specific benefits, barriers, and recommendations for integrated research programs.
CCOs should strive to have a research program that obtains federal funding for a broad range of research in critical care, including basic science, clinical trials, and healthcare outcomes, to a degree that is commensurate with that of any other major department within its institution. While some CCOs may not be able to maintain basic and clinical research programs, outcomes and healthcare systems research is particularly vital to the function of the CCO as a central part of the quality improvement mission and the structure, process, and outcomes of patient care (9, 27). Institutions wishing to become designated centers for certain clinical populations (e.g. stroke center) may need a particular type of research program as part of the requirements of that designation (34, 35).
Research program priorities should be thematic and align with institutional priorities, ensure protected time for research faculty and trainees, and leverage an electronic data collection system to organize clinical information (36). These priorities should be maintained throughout integration. Well-developed programs should seek to establish a training grant to enhance their CCO. Training opportunities such as NIH funded T32 programs in the United States are important for creating a sustainable physician-scientist workforce in Critical Care and are another way to achieve integration of learners outside of didactic and clinical training. As integration of the research program proceeds, cost savings and improved operations resulting from consolidation of human resources (e.g. coordinators, statisticians, and grant support staff) may be quickly realized, however developing a shared identity as a Critical Care research team may take longer.
Education Program
Critical Care education represents an amalgam of learners from various medical and surgical training specialties as well as nursing, pharmacy, respiratory therapy, and other professional disciplines. As with other aspects of the CCO, the educational program must break down traditional training “silos” and seek to create a shared identity amongst trainees as part of the Critical Care team. This integrated approach helps create a versatile workforce in Critical Care where trainees acquire the strengths and employ the best practices of a wide range of professional backgrounds. It is essential that the multidisciplinary nature of Critical Care be reflected in both clinical and didactic aspects of the CCO’s education program. Digital supplement 4 depicts the benefits, barriers, and recommendations for these and other core features.
Integration of CCO education programs center on the establishment of a culture of inter-professional training. Learners trained using an interprofessional education (IPE) approach are more likely to become collaborative and respectful team members who work towards improving patient outcomes (37). Trainees should share clinical rotations and didactic training. The clinical environment must support the notion that the different training backgrounds of Critical Care team members are equally vital to patient care and that differences in expertise should be considered a teaching opportunity. Didactic experiences may be integrated by selecting high yield topics from education consensus statements and program requirements (10–13, 38) and then leveraging online learning management systems to deliver didactic material in a learner-controlled manner. Subsequent pairing of online content delivery with interactive in-class team experiences such as high-fidelity simulation may help learners to better retain and consolidate Critical Care knowledge (39) while reinforcing the IPE culture.
Professional Development Program
Professional development represents a long term process of academic maturation and is essential to sustaining a pool of local expertise that supports each mission of the CCO. In addition, there is a need to produce CCM leaders with the political and administrative skill sets required to lead CCOs into the future (3). CCO professional development programs must help faculty and CCM trainees identify and pursue a desired career pathway (40), find robust mentorship, and acquire an understanding of a broad range of professional skills that will enhance their leadership abilities.
Many CCM trainees perceive the support to help them achieve their career goals as inadequate (41, 42). CCOs must develop a structured way of helping its members cultivate a career pathway. AMCs have developed tracks for faculty advancement and promotion, and this strategy may also work for training programs (43–45). Additionally, a robust mentorship program using an interprofessional pool of mentors is needed. Such mentorship has been shown to enhance professional success and improve overall career satisfaction (46).
A third important aspect of professional development is helping members establish basic leadership and professional skills and a broad-based fund of knowledge of the other academic missions of the CCO, including teaching, business, work/life balance, and scholarly writing skills that CCM team members require (47, 48). A recent study featuring a seminar-style curriculum established topics needed for broad-based professional development and suggested that this type of curriculum may help develop professional skills that are durable over time (49). Digital supplement 5 shows the benefits, barriers, and specific recommendations for CCO professional development programs. In addition to the set of recommendations for the various key elements above, Digital supplement 6 provides a set of readings and resources that may be helpful to institutions considering this transition.
Conclusion
Integration of Critical Care services into a collaborative, horizontally structured organization is likely to include academic programs as well. These academic programs could possibly benefit from integration in several ways both economically and professionally and contribute to value-based patient care. The recommendations provided for patient safety, quality, research, education, and professional development programs will help to establish effective and sustainable academic CCOs.
Supplementary Material
1. Patient Care and Safety Program Benefits/Barriers/Recommendations.
2. Quality Improvement Program Benefits/Barriers/Recommendations.
3. Research Program Benefits/Barriers/Recommendations.
4. Education Program Benefits/Barriers/Recommendations.
5. Professional Development Program Benefits/Barriers/Recommendations.
6. Readings and Resources.
Acknowledgments
Dr. Masur received support for article research from the National Institutes of Health, and he disclosed government work. Dr. Coopersmith’s institution received funding from Society of Critical Care Medicine (SCCM) as the president-elect of SCCM in 2014 and president in 2015. An honorarium for time spent in this role was paid to Emory University. Dr. Pastores received funding from Winthrop University Hospital, NY (Medical Grand Rounds) and New York Hospital Queens (Medical Grand Rounds), and he received other support from Theravanxe (Advisory Board Meeting).
Financial Support: None
APPENDIX
ALCCM Task Force Co-Chairs
Vladimir Kvetan, MD, FCCM, Montefiore Medical Center, Bronx, NY; Stephen M Pastores, MD, MACP, FCCP, FCCM, Memorial Sloan Kettering Cancer Center, New York, NY
ALCCM Task Force Members
Derek C Angus, MD, MCCM, University of Pittsburgh Medical Center, Pittsburgh, PA; Gregory Beilman, MD, FCCM, University of Minnesota, Minneapolis, MN; Daniel R Brown, MD, PhD, FCCM, Mayo Clinic, Rochester, MN; Timothy S Buchman, MD, FCCP, MCCM, Emory Critical Care, Atlanta, GA; John Christman, MD, The Ohio State University Wexner Medical Center, Columbus, OH; J Perren Cobb, MD, FCCM, University of Southern California, Los Angeles, CA; Craig M Coopersmith, MD, FACS, FCCM, Emory Critical Care, Atlanta, GA Jose Diaz-Gomez, MD, FCCM, Mayo Clinic, Jacksonville, FL; Christopher Doig, MD, University of Calgary, Calgary, CA; J Christopher Farmer, MD, FCCM, Mayo Clinic, Scottsdale, AZ; James Gasperino, MD, The Brooklyn Hospital Center, Brooklyn, NY; Sara R Gregg, MHA, Emory Critical Care, Atlanta, GA ; Neil A Halpern, MD, FACP, FCCP, MCCM, Memorial Sloan Kettering Cancer Center, New York, NY; Daniel L Herr, MD, FCCM, University of Maryland, Baltimore, MD; R Duncan Hite, MD, Cleveland Clinic, Cleveland, OH; A Joseph Layon, MD, Geisinger Medical Center, Danville, PA; Andrew Leibowitz, MD, FCCM, Mount Sinai Medical Center, New York, NY; Sharon Leung, MD, Montefiore Medical Center, Bronx, NY; Craig M. Lilly, MD, FCCP, FCCM, University of Massachusetts, Worcester, MA ; Jon Marinaro, MD, FCCM, University of New Mexico, Albuquerque, NM; Henry Masur, MD, FCCM, National Institutes of Health Clinical Center, Bethesda, MD; Jason Moore, MD, University of Pittsburgh Medical Center, Pittsburgh, PA; Joseph L Nates, MD, MD Anderson Cancer Center, Houston, TX; John M Oropello, MD, FACP, FCCP, FCCM, Mount Sinai Medical Center, New York, NY; Marc Popovich, MD, FCCM, University Hospitals, Cleveland Medical Center, Cleveland, OH; Kristen Price, MD, MD Anderson Cancer Center, Houston, TX; Curtis Sessler, MD, FCCP, FCCM, Virginia Commonwealth University, Richmond, VA; Daniel P Stoltzfus, MD, FCCM, Washington Hospital Center, Washington, DC; and Stephen Trzeciak, MD, FCCM, Cooper University Hospital, Camden, NJ
Footnotes
Disclosures: The authors report no financial conflict of interest.
Copyright form disclosure: The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Karpf M, Lofgren R. Commentary: Institutes versus traditional administrative academic health center structures. Acad Med. 2012 May;87(5):555–6. doi: 10.1097/ACM.0b013e31824d4237. [DOI] [PubMed] [Google Scholar]
- 2.Thaldorf C, Liberman A. Integration of health care organizations: using the power strategies of horizontal and vertical integration in public and private health systems. Health Care Manag (Frederick) 2007 Apr-Jun;26(2):116–27. doi: 10.1097/01.HCM.0000268614.41115.fc. [DOI] [PubMed] [Google Scholar]
- 3.Pastores SM, Halpern NA, Oropello JM, et al. Critical Care Organizations in Academic Medical Centers in North America: A Descriptive Report. Crit Care Med. 2015 Oct;43(10):2239–44. doi: 10.1097/CCM.0000000000001200. [DOI] [PubMed] [Google Scholar]
- 4.Leung S, Gregg SR, Coopersmith CM, et al. Critical Care Organizations: Business of Critical Care and Value/Performance Building. Crit Care Med. 2017 Aug 31; doi: 10.1097/CCM.0000000000002696. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Murphy DJ, Ogbu OC, Coopersmith CM. ICU director data: using data to assess value, inform local change, and relate to the external world. Chest. 2015 Apr;147(4):1168–78. doi: 10.1378/chest.14-1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kastor JA. Point-counterpoint: The Cleveland Clinic institute system is the right structure for academic health centers in the 21st century. Acad Med. 2012 May;87(5):558. doi: 10.1097/ACM.0b013e31824d5947. [DOI] [PubMed] [Google Scholar]
- 7.Kastor JA. Point-counterpoint: The traditional departmental model is the right structure for academic health centers in the 21st century. Acad Med. 2012 May;87(5):559. doi: 10.1097/ACM.0b013e31824d5932. [DOI] [PubMed] [Google Scholar]
- 8.Young JB, Cosgrove DM. Commentary: Change we must: putting patients first with the institute model of academic health center organization. Acad Med. 2012 May;87(5):552–4. doi: 10.1097/ACM.0b013e31824d5960. [DOI] [PubMed] [Google Scholar]
- 9.Deutschman CS, Ahrens T, Cairns CB, et al. Multisociety task force for critical care research: key issues and recommendations. Chest. 2012 Jan;141(1):201–209. doi: 10.1378/chest.11-2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ACGME. Program Requirements for Graduate Medical Education in Critical Care Medicine (Internal Medicine) Available at http://www.acgme.org. Accessed from Accreditation Council for Graduate Medical Education website on 28 November 2016.
- 11.ACGME. Program Requirements for Graduate Medical Education in Pulmonary and Critical Care Medicine. Available at http://www.acgme.org. Accessed from Accreditation Council for Graduate Medical Education website on 28 November 2016.
- 12.ACGME. Program Requirements for Graduate Medical Education in Anesthesiology Critical Care Medicine. Available at http://www.acgme.org. Accessed from Accreditation Council for Graduate Medical Education website on 28 November 2016.
- 13.ACGME. Program Requirements for Graduate Medical Education in Surgical Critical Care. Available at http://www.acgme.org. Accessed from Accreditation Council for Graduate Medical Education website on 28 November 2016.
- 14.Pastores SM, Martin GS, Baumann MH, et al. Training internists to meet critical care needs in the United States: a consensus statement from the Critical Care Societies Collaborative (CCSC) Crit Care Med. 2014 May;42(5):1272–1279. doi: 10.1097/CCM.0000000000000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.St Andre A. The formation, elements of success, and challenges in managing a critical care program: Part II. Crit Care Med. 2015 May;43(5):1096–101. doi: 10.1097/CCM.0000000000000856. [DOI] [PubMed] [Google Scholar]
- 16.Safar P. Critical Care Medicine – quo vadis? Crit Care Med. 1974 Jan-Feb;2(1):1–5. doi: 10.1097/00003246-197401000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Burns J. Establishing a Cardiovascular Institute: Foundational Elements. Cath Lab Digest. 2016 Apr;24(4):24–25. [Google Scholar]
- 18.Jordan J, Rose L, Dainty KN, et al. Factors that impact on the use of mechanical ventilation weaning protocols in critically ill adults and children: a qualitative evidence-synthesis. Cochrane Database Syst Rev. 2016 Oct 4;10:CD011812. doi: 10.1002/14651858.CD011812.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med. 2014 May;42(5):1024–36. doi: 10.1097/CCM.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnes-Daly MA, Phillips G, Ely EW. Improving Hospital Survival and Reducing Brain Dysfunction at Seven California Community Hospitals: Implementing PAD Guidelines Via the ABCDEF Bundle in 6,064 Patients. Crit Care Med. 2016 Nov 17; doi: 10.1097/CCM.0000000000002149. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Hesselink G, Berben S, Beune T, et al. Improving the governance of patient safety in emergency care: a systematic review of interventions. BMJ Open. 2016 Jan 29;6(1):e009837. doi: 10.1136/bmjopen-2015-009837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gummadi S, Housri N, Zimmers TA, et al. Electronic medical record: a balancing act of patient safety, privacy and health care delivery. Am J Med Sci. 2014 Sep;348(3):238–43. doi: 10.1097/MAJ.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 23.CHECKLIST-ICU Investigators and BRICNet. Machado F, Bozza F, Ibrain J, et al. A cluster randomized trial of a multifaceted quality improvement intervention in Brazilian intensive care units: study protocol. Implement Sci. 2015 Jan 13;10:8. doi: 10.1186/s13012-014-0190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rothman B, Leonard JC, Vigoda MM. Future of electronic health records: implications for decision support. Mt Sinai J Med. 2012 Nov-Dec;79(6):757–68. doi: 10.1002/msj.21351. [DOI] [PubMed] [Google Scholar]
- 25.Garcia-Jimenez A, Moreno-Conde A, Martínez-García A, et al. Clinical Decision Support using a Terminology Server to improve Patient Safety. Stud Health Technol Inform. 2015;210:150–4. [PubMed] [Google Scholar]
- 26.Algaze CA, Wood M, Pageler NM, et al. Use of a Checklist and Clinical Decision Support Tool Reduces Laboratory Use and Improves Cost. Pediatrics. 2016 Jan;137(1) doi: 10.1542/peds.2014-3019. Epub 2015 Dec 17. [DOI] [PubMed] [Google Scholar]
- 27.Curtis JR, Cook DJ, Wall RJ, et al. Intensive care unit quality improvement: a “how-to” guide for the interdisciplinary team. Crit Care Med. 2006 Jan;34(1):211–218. doi: 10.1097/01.ccm.0000190617.76104.ac. [DOI] [PubMed] [Google Scholar]
- 28.Gershengorn HB, Kocher R, Factor P. Management strategies to effect change in intensive care units: lessons from the world of business. Part I. Targeting quality improvement initiatives. Ann Am Thorac Soc. 2014 Feb;11(2):264–269. doi: 10.1513/AnnalsATS.201306-177AS. [DOI] [PubMed] [Google Scholar]
- 29.Gershengorn HB, Kocher R, Factor P. Management strategies to effect change in intensive care units: lessons from the world of business. Part II. Quality-improvement strategies. Ann Am Thorac Soc. 2014 Mar;11(3):444–453. doi: 10.1513/AnnalsATS.201311-392AS. [DOI] [PubMed] [Google Scholar]
- 30.Gershengorn HB, Kocher R, Factor P. Management strategies to effect change in intensive care units: lessons from the world of business. Part III. Effectively effecting and sustaining change. Ann Am Thorac Soc. 2014 Mar;11(3):454–457. doi: 10.1513/AnnalsATS.201311-393AS. [DOI] [PubMed] [Google Scholar]
- 31.Nates JL, Nunnally M, Kleinpell R, et al. ICU Admission, Discharge, and Triage Guidelines: A Framework to Enhance Clinical Operations, Development of Institutional Policies, and Further Research. Crit Care Med. 2016 Aug;44(8):1553–602. doi: 10.1097/CCM.0000000000001856. [DOI] [PubMed] [Google Scholar]
- 32.Martin-Delgado MC, Pericas LC, Moreno JR, et al. Quality Indicators in Critically Ill Patients. Available at http://www.semicyuc.org/temas/calidad/indicadores-de-calidad. Accessed from La Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (SEMICYUC) website on 23 November 2016.
- 33.Reid PP, Compton WD, Grossman JH, Fanjiang G, editors. Institute of Medicine and National Academy of Engineering. Building a better delivery system: A new engineering/health care partnership. Washington, DC: National Academies Press; 2005. http://www.nap.edu/openbook.php?record_id=11378. [PubMed] [Google Scholar]
- 34.American Trauma Society Level 1 Trauma Requirements – Trauma Levels Explained. Available at http://www.amtrauma.org. Accessed from American Trauma Society website on 4 January 2017.
- 35.The Joint Commission requirements for Comprehensive Stroke Center certification. Available at https://www.jointcommission.org. Accessed from The Joint Commission website on 4 January 2017.
- 36.Cohn S, Buchman T, Croce M, et al. Brief Report: EAST Workshop on How to Build a Clinical Research Program. Available at http://www.east.org/research/building-a-clinicial-research-program. Accessed from the Eastern Association for the Surgery of Trauma website on 23 November 2016.
- 37.Bridges DR, Davidson RA, Odegard PS, et al. Interprofessional collaboration: three best practice models of interprofessional education. Med Educ Online. 2011 Apr 8;:16. doi: 10.3402/meo.v16i0.6035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fessler HE, Addrizzo-Harris D, Beck JM, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: report of a multisociety working group. Chest. 2014 Sep;146(3):813–34. doi: 10.1378/chest.14-0710. [DOI] [PubMed] [Google Scholar]
- 39.Prober CG, Heath C. Lecture halls without lectures–a proposal for medical education. N Engl J Med. 2012 May 3;366(18):1657–9. doi: 10.1056/NEJMp1202451. [DOI] [PubMed] [Google Scholar]
- 40.St Andre A. The formation, elements of success, and challenges in managing a critical care program: Part I. Crit Care Med. 2015 Apr;43(4):874–9. doi: 10.1097/CCM.0000000000000855. [DOI] [PubMed] [Google Scholar]
- 41.St-Onge M, Mandelzweig K, Marshall JC, et al. Critical care trainees’ career goals and needs: A Canadian survey. Can Respir J. 2014 Mar-Apr;21(2):93–5. doi: 10.1155/2014/520237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel MB, Laudanski K, Pandharipande PP. An international career development survey of critical care practitioners. Crit Care Med. 2014 Apr;42(4):e300–3. doi: 10.1097/CCM.0000000000000137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weinert CR, Billings J, Ryan R, et al. Academic and career development of pulmonary and critical care physician-scientists. Am J Respir Crit Care Med. 2006 Jan 1;173(1):23–31. doi: 10.1164/rccm.200503-325OC. [DOI] [PubMed] [Google Scholar]
- 44.Smith CC, McCormick I, Huang GC. The clinician-educator track: training internal medicine residents as clinician-educators. Acad Med. 2014 Jun;89(6):888–91. doi: 10.1097/ACM.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 45.Ackerly DC, Sangvai DG, Udayakumar K, et al. Training the next generation of physician-executives: an innovative residency pathway in management and leadership. Acad Med. 2011 May;86(5):575–9. doi: 10.1097/ACM.0b013e318212e51b. [DOI] [PubMed] [Google Scholar]
- 46.Straus SE, Johnson MO, Marquez C, et al. Characteristics of successful and failed mentoring relationships: a qualitative study across two academic health centers. Acad Med. 2013 Jan;88(1):82–9. doi: 10.1097/ACM.0b013e31827647a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patel MB, Laudanski K, Pandharipande PP. An international career development survey of critical care practitioners. Crit Care Med. 2014 Apr;42(4):e300–3. doi: 10.1097/CCM.0000000000000137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Farley H, Casaletto J, Ankel F, et al. An assessment of the faculty development needs of junior clinical faculty in emergency medicine. Acad Emerg Med. 2008 Jul;15(7):664–8. doi: 10.1111/j.1553-2712.2008.00152.x. [DOI] [PubMed] [Google Scholar]
- 49.Moore JE, Pinsky MR. Faculty development for fellows: Developing and evaluating a broad-based career development course for critical care medicine trainees. J Crit Care. 2015 Oct;30(5):1152.e1–6. doi: 10.1016/j.jcrc.2015.05.032. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1. Patient Care and Safety Program Benefits/Barriers/Recommendations.
2. Quality Improvement Program Benefits/Barriers/Recommendations.
3. Research Program Benefits/Barriers/Recommendations.
4. Education Program Benefits/Barriers/Recommendations.
5. Professional Development Program Benefits/Barriers/Recommendations.
6. Readings and Resources.


