Abstract
Objective
To quantify healthcare utilization in the week preceding sepsis hospitalization to identify potential opportunities to improve the recognition and treatment of sepsis prior to admission.
Design
Retrospective study.
Setting
Two large integrated healthcare delivery systems in the US.
Participants
Hospitalized sepsis patients.
Interventions
None
Measurements and Main Results
We quantified clinician-based encounters in each the 7 days preceding sepsis admission, as well as on the day of admission, and categorized them as: hospitalization, subacute nursing facility, emergency department, urgent care, primary care, and specialty care. We identified the proportion of encounters with diagnoses for acute infection based on 28 single-level Clinical Classification Software categories. We also quantified the use of antibiotics over the same interval and used linear regression to evaluate time trends. We included a total of 14,658 KPNC sepsis hospitalizations and 31,369 VA sepsis hospitalizations. Over 40% of patients in both cohorts required intensive care. A total of 7,747 (52.9%) KP patients and 14,280 (45.5%) VA patients were seen by a clinician in the week before sepsis. Prior to sepsis, utilization of subacute nursing facilities remained steady, while hospital utilization declined. Primary care, specialty care, and ED visits increased, particularly on admission day. Among those with a pre-sepsis encounter, 2,648 (34.2%) KPNC patients and 3,858 (27.0%) VA patients had at least one acute infection diagnosis. An increasing percentage of outpatient encounters also had infectious diagnoses (3.3% per day; 95% CI: 1.5%–5.1%, p<0.01), particularly in primary and specialty care settings. Prior to sepsis hospitalization, the use of antibiotics also increased steadily (2.1% per day; 95% CI: 1.1%–3.1%, p<0.01).
Conclusions
Over 45% of sepsis patients had clinician-based encounters in the week prior to hospitalization with an increasing incidence of diagnoses for acute infection and antibiotic use in the outpatient setting. These pre-sepsis encounters offer several potential opportunities to improve the recognition, risk stratification, and treatment prior to sepsis hospitalization.
Keywords: sepsis, hospitalization, critical care outcomes, utilization, patient readmission, subacute care
Introduction
Sepsis is the single most common, costly, and deadly cause of US hospitalization and a major source of long-term morbidity and healthcare utilization.(1, 2) Fortunately, hospital mortality from sepsis has declined steadily over time—an improvement due in part to the widespread use of sepsis-focused quality improvement programs.(3) These sepsis programs focus heavily on the medical care delivered during the ‘golden hours’ after hospital presentation, because timely treatment is associated with improved mortality.(4) However, as the delivery of timely treatments like antibiotics has steadily improved, investing in only in these earliest hours of hospital treatment may yield marginal additional benefits on outcomes.(5, 6)
The pre-hospital setting, however, has the potential to offer even earlier opportunities to deliver effective treatments, particularly since the evolution of infection and organ dysfunction that comprise sepsis are already underway before hospital presentation. For this reason, clinical trials are now testing whether antibiotics given en route to the hospital by emergency medical technicians can further improve outcomes.(7) We hypothesized that additional opportunities for prevention and early recognition of sepsis prior to hospitalization may be possible. However, little is known about healthcare utilization immediately prior to sepsis hospitalization (8). In this exploratory study, we measured pre-sepsis healthcare utilization and infection incidence in two large, integrated healthcare delivery systems.
Methods
This study was approved by the Institutional Review Boards of the Kaiser Permanente Northern California (KPNC) and Ann Arbor Veterans Health Administration (VA) systems. We retrospectively evaluated sepsis hospitalizations from KPNC and the VA to describe healthcare utilization in the week before sepsis. In KPNC, we evaluated sepsis patients whose hospitalization began in the emergency department (ED), while in the VA, we included sepsis patients admitted from any location, since many patients are admitted directly. We identified patients’ first sepsis hospitalizations using validated International Classification of Disease, 9th Edition, Clinical Modification (ICD9) diagnosis codes for infection and acute organ dysfunction from 21 KPNC hospitals (2010 to 2013) and 114 VA hospitals (2009).(9) We focused on patients with sepsis present on admission.
We categorized pre-sepsis clinical encounters occurring on the day of sepsis hospitalization or in the seven preceding days as: hospitalization, subacute nursing facility (SNF), emergency department (ED), urgent care, primary care visit, or specialty care visit. We excluded ED visits that led to the primary sepsis hospitalization of interest as well as visits without clinician interaction (i.e., laboratory, pharmacy, radiology). Each patient could have multiple encounters in the week prior to sepsis hospitalization. To quantify the proportion of pre-sepsis encounters that included an infectious diagnosis, we identified those including an ICD9-based code for acute infection based on 28 AHRQ Clinical Classification Software single-level categories (e.g., pneumonia [122], skin and subcutaneous infections [197]). We also evaluated outpatient pharmacy records to quantify the number of antibiotic prescriptions filled by sepsis patients prior to hospitalization.
Continuous data are reported as mean (standard deviation) or median (interquartile range); categorical data are reported as number (percent). We used linear regression to assess for time trends in the proportion of visits for infectious diagnoses excluding the day of sepsis hospitalization. We grouped visits as: hospitalization and SNF, ED and urgent care, and primary and specialty care. We also evaluated time trends in antibiotic usage based on the number of antibiotic prescriptions divided by the total number of outpatient visits. We considered p-values ≤0.05 significant. Analyses were performed using STATA/SE 14.2.
Results
We identified 14,658 KPNC sepsis hospitalizations and 31,369 VA sepsis hospitalizations (Table 1). Overall mortality was 15.9% in KPNC and 13.4% in VA, with >40% of patients in both cohorts using intensive care during sepsis hospitalization. A total of 7,747 (52.9%) KP patients and 14,280 (45.5%) VA patients were seen by a clinician in the week before sepsis. A total of 2,372 (16.2%) of KP and 7,226 (23.0%) of VA patients were seen on the day of admission. In-hospital mortality was higher among patients with pre-sepsis encounters than among those without encounters (15.2% v. 13.2%; p<0.01). Hospital mortality was also higher among patients whose sepsis episode represented a hospital readmission (18.9%), compared to those without a hospitalization in the week preceding sepsis (13.9%, p<0.01).
Table 1. Characteristics of sepsis inpatients stratified by site and pre-sepsis healthcare encounters.
Healthcare encounters represent clinician-based encounters (i.e., excluding laboratory, pharmacy, or radiology visits). Values are presented as median (interquartile range) or number (%). VA: Veterans Health Administration; KPNC: Kaiser Permanente Northern California. Sepsis hospitalizations from KPNC include only those originating in the emergency department while those from VA included those originating from any source.
| KPNC | VA | |||||
|---|---|---|---|---|---|---|
| Characteristic | Pre-Sepsis Healthcare Visits | Pre-Sepsis Healthcare Visits | ||||
| No | Yes | p-value | No | Yes | p-value | |
| Number | 6,911 (47.1%) | 7,747 (52.9%) | 17,089 (54.5%) | 14,280(45.5%) | ||
| Age, years | 75 (62–84) | 74 (62–83) | <0.01 | 68 (60–80) | 69 (61–80) | <0.01 |
| Male gender | 3,392 (49.1) | 3,849 (49.7) | 0.94 | 16,572 (97.0) | 13,846 (97.0) | 0.95 |
| Charlson Index | 1 (1 – 2) | 2 (1 – 3) | <0.01 | 3 (1–5) | 3 (1–5) | <0.01 |
| Length of stay, days | 5 (3 – 8) | 5 (3 – 9) | <0.01 | 7 (4–14) | 7 (4–14) | 0.57 |
| Emergency admission | 6,911 (100.0) | 7,747 (100.0) | -- | 9,619 (56.3) | 6,988 (48.9) | <0.01 |
| Intensive care utilization | 3,272 (47.3) | 3,838 (49.5) | 0.10 | 7,143 (41.8) | 5,638 (39.5) | <0.01 |
| Discharge disposition | ||||||
| Death | 953 (13.8) | 1,374 (17.7) | <0.01 | 2,219 (13.0) | 1,974 (13.8) | 0.03 |
| Home | 4,354 (63.0) | 4,223 (54.5) | <0.01 | 14,870 (87.0) | 12,306 (86.2) | 0.03 |
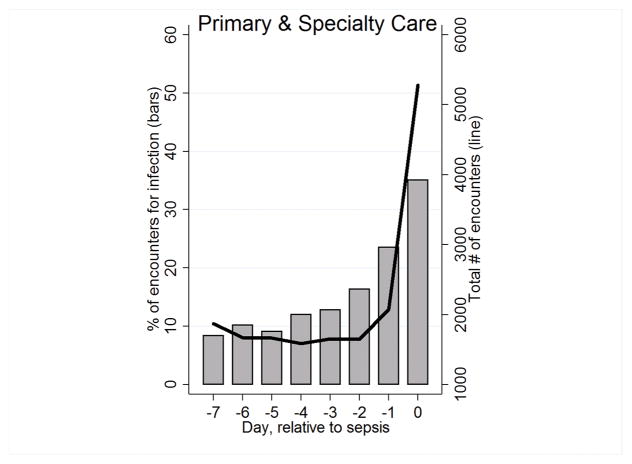
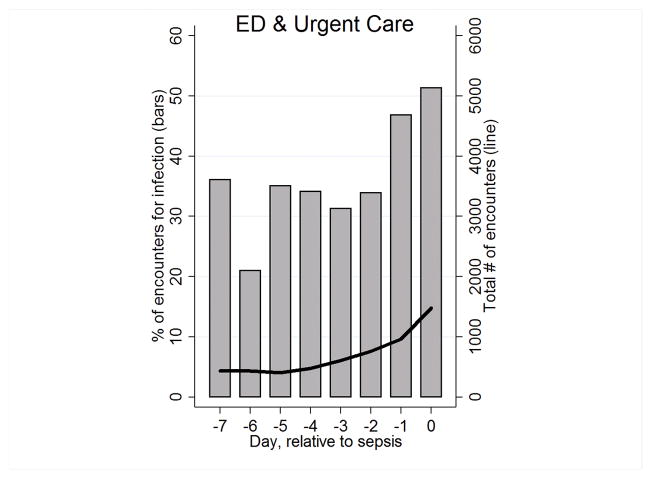
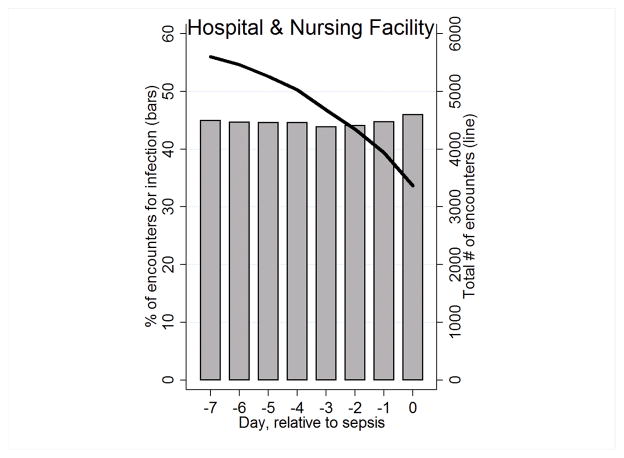
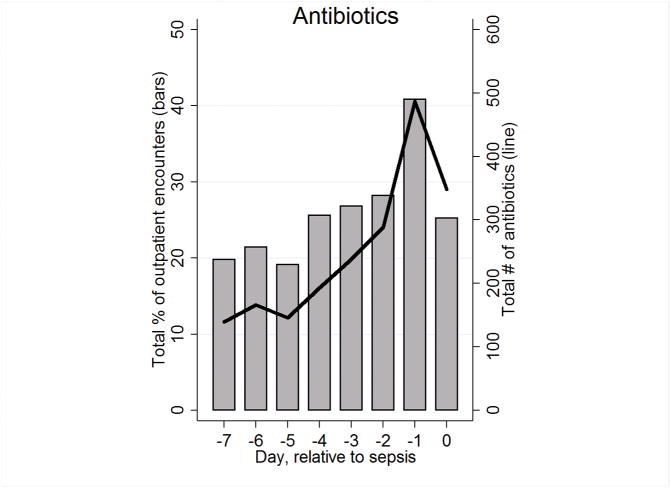
In the week prior to sepsis, primary care and specialty care visits increased, particularly on admission day (Figure 1a), with smaller increases in ED visits (Figure 1b). Before sepsis, SNF utilization remained steady, while hospital utilization declined over time (Figure 1c). Among those with a pre-sepsis encounter, 2,648 (34.2%) KPNC patients and 3,858 (27.0%) VA patients had at least one acute infection diagnosis, including 53.8% of those admitted with SNF or hospital utilization. An increasing percentage of outpatient encounters also had infectious diagnoses (3.3% per day; 95% CI: 1.5%–5.1%, p<0.01), particularly in primary and specialty care settings. Prior to sepsis hospitalization, the use of antibiotics also increased steadily (2.1% per day; 95% CI: 1.1%–3.1%, p<0.01; Figure 1d).
Figure 1. Figure panels show the total number of encounters or antibiotics (lines) and the percentage of encounters with infection or antibiotics (bars) in the week prior to sepsis hospitalization drawn from a total sample of 14,658 KP and 31,369 VA sepsis patients.
Panels display changes over time in: primary care and specialty care (Figure 1a); emergency department and urgent care (Figure 1b); hospitalization and nursing facility (Figure 1c); and in antibiotic usage relative to outpatient visits. On the x-axis, day 0 represents the day of sepsis admission while day −7 represents 7 days prior to admission.
Discussion
In two large multicenter cohorts including over 46,000 patients, 45% of sepsis patients were seen by clinicians in the week leading up to hospitalization, with sharp increases in utilization just prior to admission. Over the same period, infectious diagnoses and outpatient antibiotic use also increased steadily. These exploratory findings produce novel insight into three potential pre-hospital opportunities to improve the recognition and treatment of sepsis.
First, a proportion of sepsis hospitalizations were readmissions following a prior infection-related hospitalization, a finding consistent with the growing recognition that sepsis is a major contributor to hospital readmission.(10) Facilitating improved transitions in care with timely monitoring and evaluation of infectious symptoms after discharge may be an important step towards reducing post-sepsis re-hospitalization. While several general readmission risk models exist, it is not known whether they exhibit good discrimination or calibration for sepsis patients.
Second, many patients were transferred between healthcare settings on the day of hospitalization (e.g., SNF to hospital or ambulatory care to ED). Developing systems to administer timely sepsis care (e.g., antibiotics or intravenous fluids) prior to transfer could substantially reduce the time to effective treatment. This is particularly important since even hourly delays in antibiotic administration are associated with increased mortality.(5, 6)
Third, risk stratification models or theranostic tools for outpatients presenting with acute infectious symptoms could improve the identification of patients with the greatest risk of disease progression who might benefit from closer monitoring. Little is currently known about the clinical factors that can be used predict outpatients who have a high probability of requiring subsequent hospitalization. These data demonstrate increasing use of antibiotics in the period leading up to admission suggesting that clinicians are identifying concerning signs and symptoms of infection.
This study has important limitations. First, we used ICD9 codes to identify pre-sepsis acute infection which may underestimate the true incidence of infectious symptoms. Second, we were unable to compare sepsis patients with others presenting to outpatient encounters with similar symptoms who were not ultimately hospitalized for sepsis. In order to develop clinically useful risk prediction models, future studies should also include outpatients with infectious symptoms who are not hospitalized for sepsis since positive or negative predictive values, and corresponding screening strategies, are highly dependent on underlying prevalence. Third, we identified sepsis hospitalizations based on ICD-9 coding, which may misclassify hospitalizations. Fourth, we were not able to link specific sources of infection with antibiotic treatment patterns, which may lend insight into clinical features that distinguish patients at highest risk of subsequent hospitalization. Finally, we included two large independent cohorts with demographic and case-mix differences which impacts our ability to distinguish important distinctions in treatment patterns and outcomes. However, our findings were largely consistent across these diverse health systems.
In conclusion, nearly half of sepsis patients were seen by clinicians in the week leading up to hospitalization, with increasing utilization and diagnosis of acute infection particularly in the final days before admission. These clinical encounters are likely to yield novel opportunities to improve pre-hospital recognition, risk stratification, and treatment of sepsis.
Acknowledgments
Funding: This work was supported by funding from The Permanente Medical Group, IIR 11–109 from the US Department of Veterans Affairs Health Services Research and Development Service, NIH K23GM112018 (VXL), and NIH K08GM115859 (HCP). The authors have no other conflict of interest disclosures.
We thank Vanessa Dickerman, MS, Kyle Kepreos, MA, Jennifer Davis, MHSA, BA, and Brenda Vincent, MS (VA Center for Clinical Management Research in Ann Arbor) and Wendy Lu, MD MPH (Kaiser Permanente Division of Research) for their expert programming; they were not compensated for their contributions besides salary. We thank Jack Iwashyna, MD, PhD, Phillip Madvig, MD, and Stephen Parodi, MD, for thoughtful conversations related to this work. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Footnotes
Copyright form disclosure: Drs. Liu, Escobar, and Prescott received support for article research from the National Institutes of Health (NIH). Dr. Liu’s institution received funding from the National Institute of General Medical Sciences. Dr. Escobar’s institution received funding from Gordon and Betty Moore Foundation (grants to develop predictive models for in-hospital deterioration and rehospitalization) and Merck (grant to develop predictive model for recurrent Clostridium difficile infection). Dr. Prescott’s institution received funding from the NIH, and she disclosed government work. Dr. Chaudhary disclosed that he does not have any potential conflicts of interest.
References
- 1.Liu V, Escobar GJ, Greene JD, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA. 2014;312(1):90–92. doi: 10.1001/jama.2014.5804. [DOI] [PubMed] [Google Scholar]
- 2.Prescott HC, Langa KM, Liu V, et al. Increased 1-year healthcare use in survivors of severe sepsis. American journal of respiratory and critical care medicine. 2014;190(1):62–69. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevenson EK, Rubenstein AR, Radin GT, et al. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014;42(3):625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 5.Liu VX, Fielding-Singh V, Greene JD, et al. The Timing of Early Antibiotics and Hospital Mortality in Sepsis. Am J Respir Crit Care Med. 2017 doi: 10.1164/rccm.201609-1848OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seymour CW, Gesten F, Prescott HC, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med. 2017;376(23):2235–2244. doi: 10.1056/NEJMoa1703058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paramedic Initiated Treatment of Sepsis Targeting Out-of-hospital Patients (PITSTOP). Clinicaltrials.gov identifier: NCT03068741.
- 8.Novosad SA, Sapiano MR, Grigg C, et al. Vital Signs: Epidemiology of Sepsis: Prevalence of Health Care Factors and Opportunities for Prevention. MMWR Morb Mortal Wkly Rep. 2016;65(33):864–869. doi: 10.15585/mmwr.mm6533e1. [DOI] [PubMed] [Google Scholar]
- 9.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Mayr FB, Talisa VB, Balakumar V, et al. Proportion and Cost of Unplanned 30-Day Readmissions After Sepsis Compared With Other Medical Conditions. JAMA. 2017;317(5):530–531. doi: 10.1001/jama.2016.20468. [DOI] [PubMed] [Google Scholar]