Abstract
Anterior cruciate ligament (ACL) tears are usually managed by reconstruction with autograft or allograft, but primary repair in carefully selected patients is a reasonable option. Proximal avulsions presenting early with excellent tissue quality are amenable to repair and healing. Restoration of native ACL preserves its proprioceptive and kinematic functions. A repair is less invasive and avoids graft-related problems, and faster rehabilitation is possible. Protection for the repair in the early stages will allow better healing. We present our technique of ACL repair using knotless suture anchors with high-strength sutures and protection using high-strength sutures tapes inserted through the same anchors.
The treatment of anterior cruciate ligament (ACL) injuries has evolved from conservative management to ACL repairs and extra-articular procedures in the 1970s to open intra-articular reconstructions with various grafts in 1980s to the current “gold standard” of anatomic and individualized arthroscopic reconstruction.1 The aim of the treatment, however, continues to be the same, that is, to provide a stable joint allowing the patient to return to his or her preinjury level of activity, improve knee-related quality of life, and avoid late sequels of an ACL deficient knee. Although ACL reconstruction gives predictable and good results with objective and subjective scores, it seldom “feels” normal and has a host of problems like donor site morbidity, failure of graft, mismatch between footprint and graft diameter, and lack of proprioception.2 Advantages of a primary acute arthroscopic ACL repair are theoretically as follows3, 4:
-
1.
Is less invasive.
-
2.
Avoids graft donor site morbidity.
-
3.
Retains native ACL anatomy, collagen orientation, and bundles especially at the footprint.
-
4.
Possibly retains proprioceptive functions, which protects the knee from secondary changes.
-
5.
Preserves the complex biomechanical properties of the ligament allowing faster recovery.
-
6.
Allows a physeal sparing option in pediatric patients.
The indications and contraindications for primary ACL repair are summarized below (Table 1).
Table 1.
Indications and Contraindications for ACL Repair
| Indications∗ | Contraindications |
|---|---|
| Acute femoral avulsion type ACL injury (Type I Sherman) | Chronic tear with stump resorption |
| Subsynovial ACL tear/stretch injury | Midsubstance tears |
| Partial ACL tear (isolated AM/PL bundle injury) | Poor tissue quality |
| Pediatric patients |
ACL, anterior cruciate ligament.
The quality of tissue must be excellent with no fraying of the stump end.
Surgical Technique
General Preparation
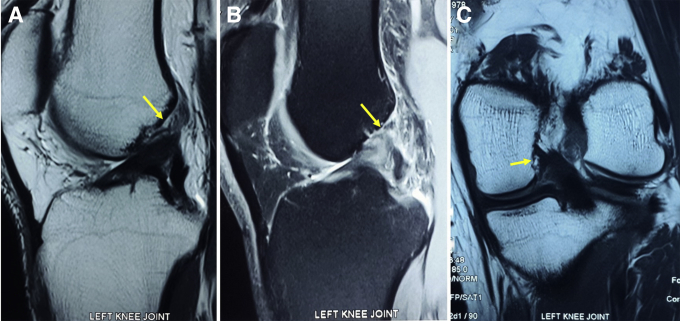
Patient is placed in the supine position. A high thigh tourniquet is applied with side support and table flat. Examination under anesthesia is performed to confirm the laxity and quantify the same. Magnetic resonance imaging is carefully studied to detect a proximal avulsion (Fig 1). All patients planned for a repair must be counseled about this procedure, and an informed consent must be obtained to proceed to a standard anatomic reconstruction should the tear be deemed unsuitable for repair. After preparation, tourniquet is inflated and a high anterolateral portal and standard anteromedial (AM) portals are created. A diagnostic round is performed to confirm the diagnosis of ACL tear and other associated pathologies. Careful probing of the stump is carried out to confirm a femoral-sided avulsion and quality of the tissue (Fig 2). Presence of the synovial sheath over the ACL indicates a low-velocity trauma. At this point, a central portal (CP) through the medial third of patella tendon is created, which allows excellent visualization of the femoral insertion site (FIS)5 (Fig 3). Decision to perform a primary repair is made if the tissue quality is deemed excellent.
Fig 1.
Magnetic resonance imaging scans to diagnose a proximal anterior cruciate ligament avulsion injury. Detection of such injury on preoperative scans can help counsel the patient about the possibility of a repair. A left knee magnetic resonance imaging scan (A) T2 sagittal, (B) PD fat saturated sagittal, and (C) PD coronal sequences showing the injury pattern (yellow arrows), with minimal marrow edema. (PD, proton density.)
Fig 2.
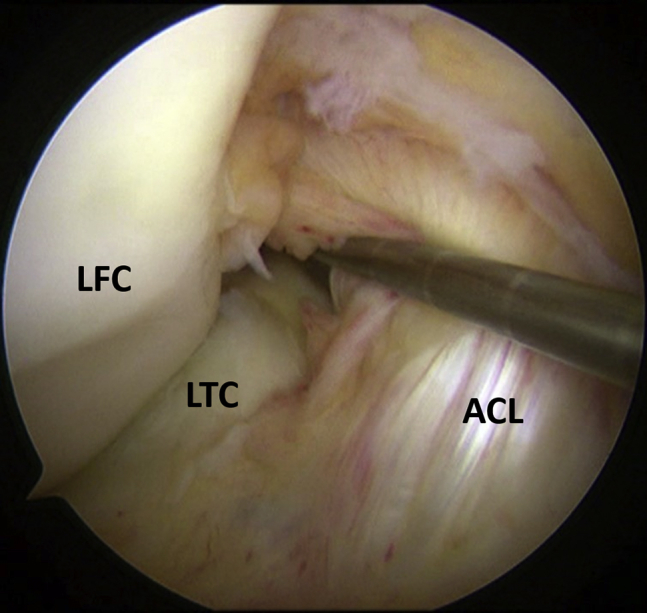
Arthroscopic detection of proximal avulsion of ACL. Right knee arthroscopy, viewing from the anterolateral portal with knee in 90° of flexion. A hook probe is inserted from the anteromedial portal, and probing of the ACL stump is performed. This confirms the presence of the tear and its location near the femoral attachment and assesses the quality of the tissue as well. Note the relatively well preserved synovial sheath over the ligament. (ACL, anterior cruciate ligament; LFC, lateral femoral condyle; LTC, lateral tibial condyle.)
Fig 3.
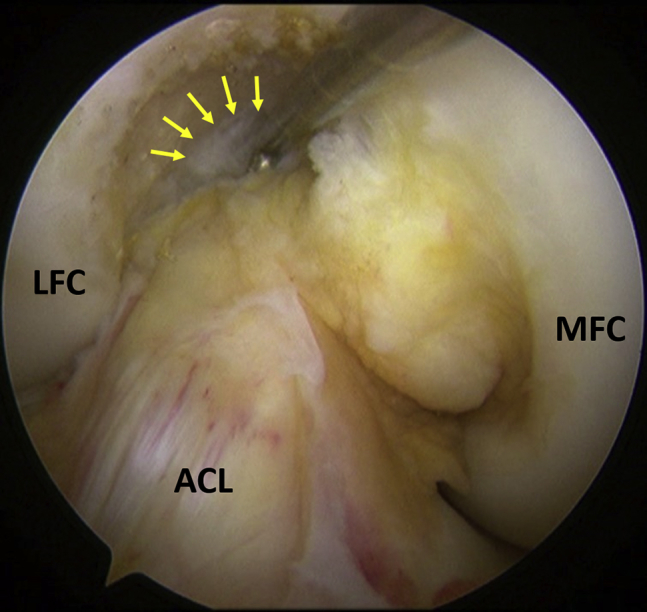
Viewing of the ACL femoral insertion site through the central portal. Right knee arthroscopy, viewing from the central portal with knee in 90° of flexion. A hook probe is inserted from the anteromedial portal to probe the ACL stump. The visualization of the femoral footprint (yellow arrows) and proximal avulsion injury is much better with this viewing. (ACL, anterior cruciate ligament; LFC, lateral femoral condyle; LTC, lateral tibial condyle; MFC, medial femoral condyle.)
Preparing the Notch and ACL Stump
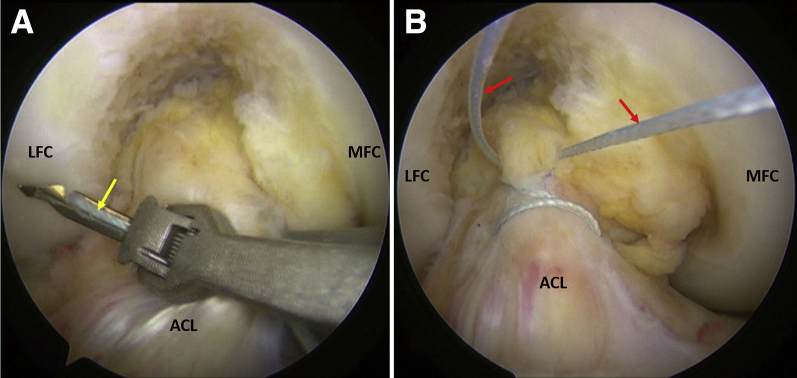
A bony notchplasty is not routinely done unless the notch is deemed too narrow. This is more commonly required in female patients with an ACL tear. Soft tissue around the FIS is cleared using a shaver. Three to 4 holes are created around the FIS with a microfracture awl to potentiate healing of the ACL stump (Fig 4). The ACL stump is then sutured with no. 2 FiberWire (Arthrex, Naples, FL) using a Labral Scorpion loaded with SureFire Scorpion needle (Arthrex) suture passing instrument through the AM portal. This instrument allows grasping the tissue, suture passage, and retrieval in a single step, thus minimizing tissue trauma. Suturing is begun distally and advanced proximally taking cruciate stitches so that 2 to 3 passes are taken through the ACL with each limb of the suture, to hold the tissue firmly (Fig 5). Utmost care is taken to avoid taking a bite through a previously passed stitch and thus lacerating the suture in the process. The 2 ends of the suture are then retrieved through the AM portal.
Fig 4.
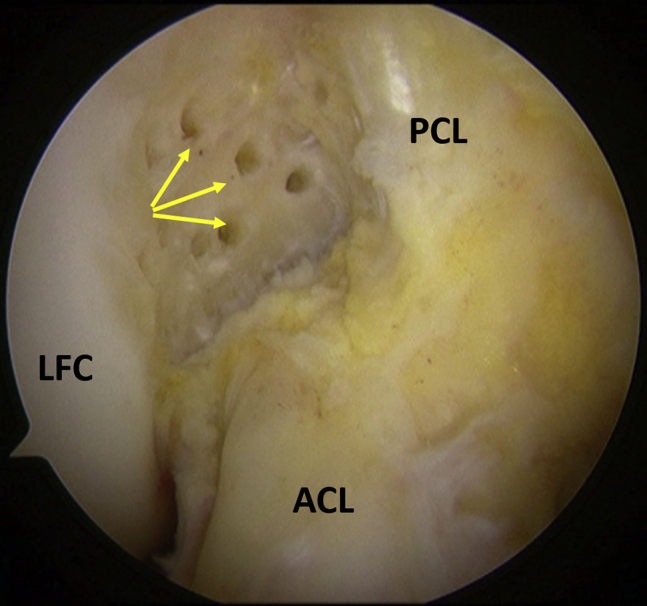
Microfractures near ACL femoral footprint. Right knee arthroscopy, viewing from the central portal with knee in 90° of flexion. Multiple microfractures (yellow arrows) performed on the medial wall of the lateral femoral condyle adjacent to the femoral insertion site of ACL. This procedure enhances healing response by recruitment of marrow elements at the repair site. (ACL, anterior cruciate ligament; LFC, lateral femoral condyle; PCL, posterior cruciate ligament.)
Fig 5.
Suturing of the ACL stump. Right knee arthroscopy, viewing from the central portal with knee in 90° of flexion. (A) Suturing is begun distally, using a Labral Scorpion (Arthrex) self-retrieving suture passer loaded with no. 2 FiberWire (yellow arrow) inserted from the anteromedial portal. The suturing is progressed proximally using cruciate stitches, and 3-4 passes are made through the stump. (B) The 2 free ends of the no. 2 FiberWire suture are retrieved from the anteromedial portal (red arrows). (ACL, anterior cruciate ligament; LFC, lateral femoral condyle; MFC, medial femoral condyle.)
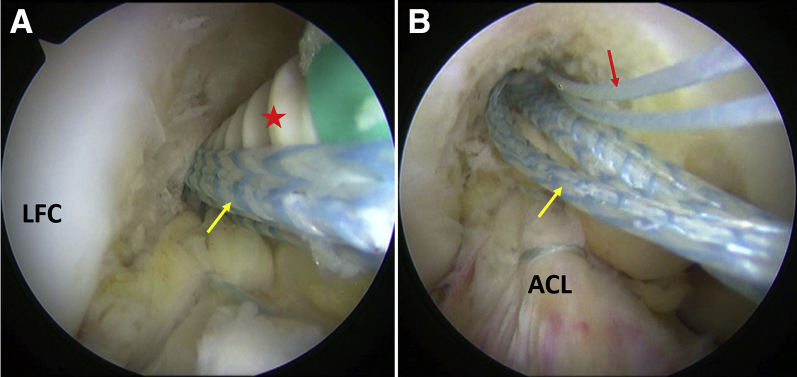
Insertion of the Stump at the FIS and Augmentation
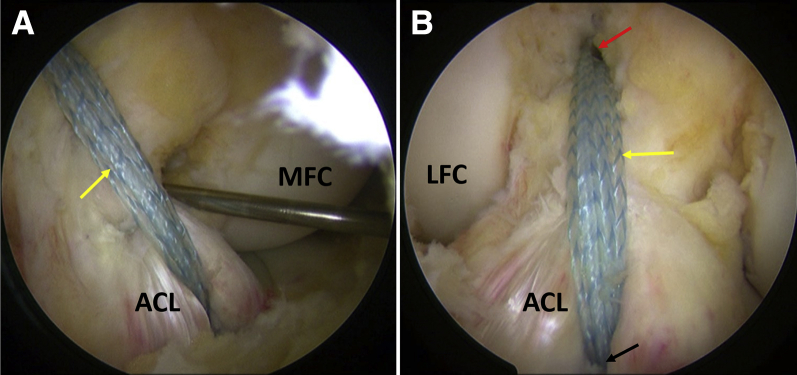
The FIS is identified accurately by viewing from the CP. A pilot hole is created at the anatomic midbundle position using an awl for the SwiveLock anchor introduced from an accessory low medial portal to obtain a straight trajectory (Fig 6). The 2 ends of FiberWire along with a FiberTape (Arthrex) are loaded into the eyelet of a 4.75 mm PEEK (polyether ether ketone) SwiveLock SP self-punching anchor (Arthrex). This additional augmentation with the FiberTape is like an InternalBrace and protects the repair until healing has occurred by providing initial stability. The driver is introduced through the accessory medial portal and inserted into the socket by tapping until the anchor tip is seen, while ensuring that there is no slack in any suture by pulling them individually. The anchor is inserted by turning the handle in a clockwise manner while viewing from the CP and knee in 90° of flexion and application of posterior drawer force to keep the ACL in tension (Fig 7). The driver is removed after the anchor is fully inserted and the tip retention suture is removed. The ends of FiberWire are cut flush using an open-ended suture cutter. Firm fixation of the stump is confirmed by probing. The arthroscope is then shifted to the anterolateral portal, and ACL tibial insertion is visualized. A socket is created at the center of the tibial footprint using the awl for SwiveLock. The 2 ends of the FiberTape are then loaded onto another 4.75-mm PEEK SwiveLock SP self-punching anchor. This is then inserted into the tibial socket in a similar manner (Fig 8). The knee is extended to confirm that there is no impingement. A final probing is done to confirm the strength and tension of the entire construct (Fig 9). The surgical technique can be reviewed in Video 1.
Fig 6.
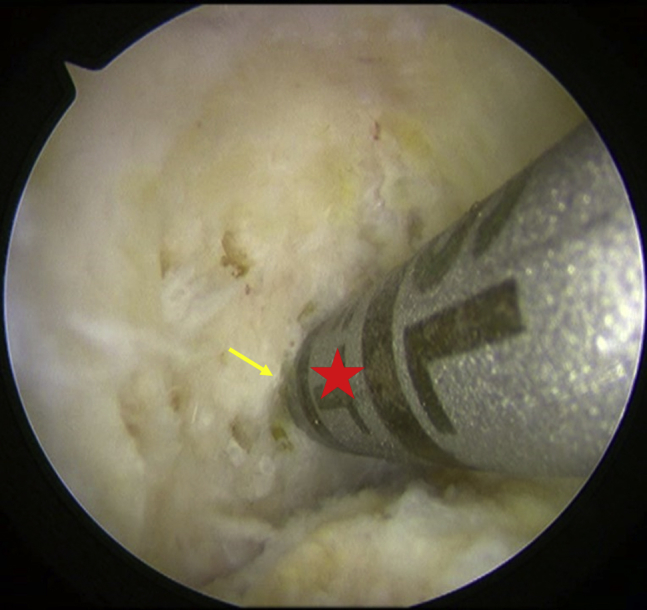
Pilot hole for suture anchor fixation. Right knee arthroscopy, viewing from the central portal with knee in 90° of flexion. Entry hole for 4.75 mm SwiveLock suture anchor being created at the center of the femoral footprint (yellow arrow) using an awl (red star) inserted through the accessory medial portal. This facilitates insertion of the suture anchor in the femur.
Fig 7.
Suture anchor insertion. Right knee arthroscopy, viewing from the central portal with knee in 90° of flexion. (A) A 4.75-mm SwiveLock suture anchor (red star), which is loaded with the no. 2 FiberWire used to stitch the ACL stump and another FiberTape (yellow arrow) being inserted into the previously created pilot hole at the center of femoral footprint through the accessory medial portal. (B) The ACL is anchored at its femoral attachment site with no. 2 FiberWire (red arrow) and FiberTape (yellow arrow) emerging from the same site. (ACL, anterior cruciate ligament; LFC, lateral femoral condyle.)
Fig 8.

Suture anchor insertion at the tibia for augmentation of repair. Right knee arthroscopy, viewing from the anterolateral portal with knee in 90° of flexion. Another 4.75-mm SwiveLock suture anchor (red star), which has been loaded with the FiberTape (yellow arrow) previously inserted with the femoral suture anchor, being inserted into a pilot hole at the center of tibial footprint through the anteromedial portal. (ACL, anterior cruciate ligament; MFC, medial femoral condyle.)
Fig 9.
Final repair and augmentation construct. Right knee arthroscopy, with knee in 90° of flexion. (A) Viewing from the anterolateral portal and probing of the repair construct through the anteromedial portal to confirm adequate tension in the ACL and FiberTape (yellow arrow). (B) Viewing from the central portal clearly demonstrates the suture anchor femoral insertion site (red arrow), FiberTape augmentation (yellow arrow), and tibial site of the suture anchor (black arrow). (ACL, anterior cruciate ligament; LFC, lateral femoral condyle; MFC, medial femoral condyle.)
Rehabilitation
A knee brace locked in extension is applied for 4 weeks. Weight bearing as tolerated is allowed immediately. Isometric exercises are begun along with early gentle range of motion. Cryotherapy is given for 3 weeks to control edema and pain. A hinge knee brace without lock is allowed after 4 weeks, and strengthening, stability training, and proprioception exercises are begun. Sports specific training is started after 6 months, and return to sports is allowed after 9 months.
Discussion
The first repair of the ACL in the English literature is attributed to A. W. Mayo Robson in 1895.6 In 1938, Palmer described the failure of spontaneous healing of a complete ACL tear and subsequent importance of repair. He advocated that early repair was critical to healing and used a repair technique using silk sutures and drawing them through a femoral tunnel.7 Following on Palmer's work, suture repair was described by several other investigators with modifications and variable results.8
After initial reports of suture repair, 2 randomized clinical trials were reported in the 1980s comparing suture repair versus nonoperative therapy for ACL injuries. In the study by Odensten et al., 95% patients in the repaired group had a stable knee at follow-up (with a negative pivot shift or Slocum test), while only 11% in the nonoperated group had a stable knee. In addition, the patients who did not have a repair needed meniscal surgery twice as often as patients undergoing suture repair in the first 18 months after injury.9 Another study reported similar results, but the investigators concluded that there was no functional difference between nonoperative and repair groups, in spite of their objective data showing a decrease in instability and need for meniscal surgery later.10 Thus, while both of these studies concluded that functional performance was comparable between the 2 groups, other important characteristics (stable knee, preservation of the menisci) appeared to be better in the group undergoing primary repair.
Although the results of the first primary open ACL suture repair techniques were initially promising, inconsistent long-term results with high rerupture rates of as high as 24%-36% and the inconsistent improvements in anteroposterior laxity led to the abandonment of these techniques.11, 12, 13 However, with improved understanding of the biology, biomechanics, and injury patterns of the ACL, there has been a paradigm shift in the concept of performing an ACL repair. The most remarkable of these is perhaps selecting the ideal patient with a tear pattern most amenable to repair. Sherman et al. classified ACL tears into 4 types. Type I in their classification was “an avulsion of the entire ligament off the femoral insertion, without a major bone fragment, leaving no remnant of proximal tissue.”14 In their cohort, better objective outcomes were seen with this group. Zantop et al. described approximately 12% of ACL tears as proximal avulsions with an intact stump.15 Steadman et al. suggested that proximal lesions have a higher healing potential than midsubstance ruptures of the ACL.16 Nguyen et al. investigated the intrinsic healing response of the ACL using standard histology and immunostaining of α-smooth muscle actin and collagen type 3. They concluded that the histologic features of the proximal third of the ACL and the MCL were similar and a similar healing response can be expected.17
Current literature advocates careful selection of patients for arthroscopic ACL repair. This includes patients with femoral-sided avulsion injuries guided by preoperative imaging and excellent tissue quality on arthroscopic examination. DiFelice et al. suggested that advances in imaging, surgical techniques, and hardware may allow us to select a specific patient cohort who will benefit from repair. In their small case series of 11 patients with proximal avulsion tears, the ACL was reattached to bone using 4.75-mm BioComposite SwiveLock suture anchors (Arthrex). At mean follow-up of 41 months, the mean International Knee Documentation Committee score was 86, the mean Lysholm score was 93, and the mean Cincinnati score was 91. These results are certainly encouraging.4 Weninger et al. described a double-bundle repair of proximal ACL tears using 2.9-mm PushLock (Arthrex) suture anchors.18 Achtnich et al. compared clinical and radiologic results of primary ACL suture anchor repair and microfracturing with anatomic ACL single-bundle reconstruction in patients with acute proximal ACL avulsion tears. They found no significant differences in knee stability between the groups on clinical examination.13 Thus, combined with direct suture repair of proximal ACL tears, microfracture improves the biological healing response by recruitment of marrow elements at the repair site, and augmentation with high-strength suture tape provides mechanical protection to the repair in the initial healing phase. Both these interventions could help improve the success of this procedure.
Risks and Limitations
The procedure is not without its limitations. Only a small subset of patients with ACL tear are fit for a primary repair, and this must be based only on criteria for which evidence is currently available, that is, proximal avulsions off the femoral attachment. It must be borne in mind that this surgery has failed historically due to poor patient selection, like attempting repair for midsubstance tears. There are no long-term data available about the success of this procedure and it does have a higher failure rate than single-bundle ACL reconstruction in the midterm, although not significant.17 Patients must be counseled about this. Rehabilitation has to be customized for each patient after a repair. The paucity of clinical data makes it imperative that caution must be exercised while taking a call regarding return to sports. An ACL graft is tensioned and fixed in 0-30° of flexion during single-bundle ACL reconstruction. A repair is, however, performed at 90° of flexion and tension is unknown. The effect that this can have on knee biomechanics is also unknown and merits further investigation to standardize the procedure. Table 2 highlights the technical pearls and pitfalls to be borne in mind while attempting the procedure.
Table 2.
Technical Pearls and Pitfalls
| Pearls |
| 1. Careful assessment of the ACL for suitability for repair determines outcome. Proximal avulsions with excellent tissue quality only are suitable for repair. In case of doubt, perform a standard anatomic ACL reconstruction with remnant preservation. |
| 2. A central portal greatly improves visualization of the femoral insertion site of ACL. |
| 3. Only high-strength suture material must be used, preferably with a self-retrieving suture passing instrument. |
| 4. A low accessory medial portal provides a straight trajectory for insertion of the suture anchor. |
| 5. Augmentation with high-strength suture tape provides initial stability, protects the repair, and allows early range of motion. |
| Pitfalls |
| 1. Strict selection of patients who are amenable for an ACL repair makes or breaks this surgery and its outcome. |
| 2. Visualizing the femoral insertion site through the anterolateral portal, as is usually done during ACL reconstruction, can compromise precise suture anchor placement at the femur. |
| 3. Passage of sutures through the ACL stump must be through the bulk of the tissue to improve grasp and purchase. This precision is possible by using a device, which allows simultaneous grasping of the stump and suture passage at the desired site. Also, sutures must be passed in the anteroposterior and mediolateral direction to improve purchase, and the slack in the suture must be removed after each pass. |
| 4. There is only one attempt possible for fixing the ACL stump with the suture anchor, and retensioning is not possible. Hence, utmost care has to be taken to maintain adequate tension and not leave the ACL slack after fixation. |
| 5. The awl and suture anchor are introduced through the accessory medial portal to maintain a straight trajectory, with the knee in 90° of flexion. |
ACL, anterior cruciate ligament.
Primary repair of the ACL in carefully selected patients with femoral avulsion is possible. It provides stability with preservation of biology, resulting in a more normal feeling knee while simultaneously eliminating graft harvest and incorporation-related issues. Augmentation with an ultra-high-strength tape provides initial protection to the repair.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.R.T. receives support from Zimmer Biomet India, Arthrex, Smith and Nephew, and Sanofi Biosurgery. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Primary ACL repair with augmentation. Right knee arthroscopy and ACL repair performed with the patient supine, knee in 90° of flexion. Viewing is from the anterolateral and central portals using a 30° arthroscope, while the anteromedial portal is used for suturing the stump with no. 2 FiberWire and accessory medial portal for 4.75-mm SwiveLock suture.
References
- 1.Irarrázaval S., Kurosaka M., Cohen M., Fu F.H. Anterior cruciate ligament reconstruction. Joint Disord Orthop Sports Med. 2016;1:38–52. [Google Scholar]
- 2.Fridén T., Roberts D., Ageberg E., Waldén M., Zätterström R. Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther. 2001;31:567–576. doi: 10.2519/jospt.2001.31.10.567. [DOI] [PubMed] [Google Scholar]
- 3.Proffen B.L., Sieker J.T., Murray M.M. Bio-enhanced repair of the anterior cruciate ligament. Arthroscopy. 2015;31:990–997. doi: 10.1016/j.arthro.2014.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DiFelice G.S., Villegas C., Taylor S. Anterior cruciate ligament preservation: early results of a novel arthroscopic technique for suture anchor primary anterior cruciate ligament repair. Arthroscopy. 2015;31:2162–2171. doi: 10.1016/j.arthro.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Araujo P.H., van Eck C.F., Macalena J.A., Fu F.H. Advances in the three-portal technique for anatomical single- or double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1239–1242. doi: 10.1007/s00167-011-1426-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robson A.W. V.I. Ruptured crucial ligaments and their repair by operation. Ann Surg. 1903;37:716–718. [PMC free article] [PubMed] [Google Scholar]
- 7.Palmer I. On the injuries to the ligaments of the knee joint. A clinical study. Acta Chir Scand Suppl. 1938;53:1–28. [Google Scholar]
- 8.Feagin J.A., Curl W.W. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med. 1976;4:95–100. doi: 10.1177/036354657600400301. [DOI] [PubMed] [Google Scholar]
- 9.Odensten M., Hamberg P.E.R., Nordin M., Lysholm J., Gillquist J.A.N. Surgical or conservative treatment of the acutely torn anterior cruciate ligament. Clin Orthop Rel Res. 1985;198:87–93. [PubMed] [Google Scholar]
- 10.Sandberg R., Balkfors B., Nilsson B., Westlin N. Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Joint Surg. 1987;69:1120–1126. [PubMed] [Google Scholar]
- 11.Jorjani J., Altmann D., Auen R., Koopmann C., Lyutenski B., Wirtz D. Mittel-bis langfristige Ergebnisse nach vorderer Kreuzbandruptur und Versorgung in Healing-Response-Technik. Z für Orthopädie Unfallchirurgie. 2013;151:570–579. doi: 10.1055/s-0033-1350874. [DOI] [PubMed] [Google Scholar]
- 12.Kubik-Huch R., Pfirrmann C., Grehn H., Bieg C., Eid K., Wasmaier J. Proximal anterior cruciate ligament tears: the healing response technique versus conservative treatment. J Knee Surg. 2012;26:263–272. doi: 10.1055/s-0032-1329720. [DOI] [PubMed] [Google Scholar]
- 13.Achtnich A., Herbst E., Forkel P. Acute proximal anterior cruciate ligament tears: outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy. 2016;32:2562–2569. doi: 10.1016/j.arthro.2016.04.031. [DOI] [PubMed] [Google Scholar]
- 14.Sherman M.F., Lieber L., Bonamo J.R., Podesta L., Reiter I. The long-term followup of primary anterior cruciate ligament repair: defining a rationale for augmentation. Am J Sports Med. 1991;19:243–255. doi: 10.1177/036354659101900307. [DOI] [PubMed] [Google Scholar]
- 15.Zantop T., Brucker P.U., Vidal A., Zelle B.A., Fu F.H. Intraarticular rupture pattern of the ACL. Clin Orthop Rel Res. 2007;454:48–53. doi: 10.1097/BLO.0b013e31802ca45b. [DOI] [PubMed] [Google Scholar]
- 16.Steadman J.R., Cameron-Donaldson M.L., Briggs K.K., Rodkey W.G. A minimally invasive technique (“healing response”) to treat proximal ACL injuries in skeletally immature athletes. J Knee Surg. 2006;19:8–13. doi: 10.1055/s-0030-1248070. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen D.T., Ramwadhdoebe T.H., van der Hart C.P., Blankevoort L., Tak P.P., van Dijk C.N. Intrinsic healing response of the human anterior cruciate ligament: an histological study of reattached ACL remnants. J Orthop Res. 2013;32:296–301. doi: 10.1002/jor.22511. [DOI] [PubMed] [Google Scholar]
- 18.Weninger P., Wepner F., Kissler F., Enenkel M., Wurnig C. Anatomic double-bundle reinsertion after acute proximal anterior cruciate ligament injury using knotless PushLock anchors. Arthrosc Techn. 2015;4:e1–e6. doi: 10.1016/j.eats.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primary ACL repair with augmentation. Right knee arthroscopy and ACL repair performed with the patient supine, knee in 90° of flexion. Viewing is from the anterolateral and central portals using a 30° arthroscope, while the anteromedial portal is used for suturing the stump with no. 2 FiberWire and accessory medial portal for 4.75-mm SwiveLock suture.