Abstract
Objective
To investigate factors associated with enrollment and participation in cardiac rehabilitation (CR) in Korea.
Methods
Patients admitted to four university hospitals with acute coronary syndrome between June 2014 and May 2016 were enrolled. The Cardiac Rehabilitation Barriers Scale (CRBS) made of 21-item questionnaire and divided in four subdomains was administered during admission. CRBS items used a 5-point Likert scale and ≥2.5 was considered as a barrier. Differences between CR non-attender and CR attender, or CR non-enroller and CR enroller in subscale and each items of CRBS were examined using the chi-square test.
Results
The CR participation rate in four hospitals was 31% (170 of the 552). Logistical factors (odds ratio [OR]=7.61; 95% confidence interval [CI], 4.62–12.55) and comorbidities/functional status (OR=6.60; 95% CI, 3.95–11.01) were identified as a barrier to CR enrollment in the subdomain analysis. Among patients who were enrolled (agreed to participate in CR during admission), only work/time conflict was a significant barrier to CR participation (OR=2.17; 95% CI, 1.29–3.66).
Conclusion
Diverse barriers to CR participation were identified in patients with acute coronary syndrome. Providing the tailored model for CR according to the individual patient's barrier could improve the CR utilization. Further multicenter study with large sample size including other CR indication is required.
Keywords: Cardiac rehabilitation, Exercise therapy, Acute coronary syndrome, Patient participation, Secondary prevention
INTRODUCTION
Cardiac rehabilitation (CR) has many benefits including reductions in cardiovascular mortality and unplanned hospital readmissions, and improved quality of life [1]. National guidelines recommend CR as a necessary treatment component in patients with coronary artery disease and chronic heart failure [2,3,4,5].
In Korea, CR has been implemented in only a limited number of tertiary and secondary hospitals. There has been no reimbursement by the National Health Insurance System for approximately 20 years. With the efforts by experts and governments, as of February 1, 2017, CR service began partially paid by the health insurance system in Korea. This coverage likely will increase, with more CR facilities becoming available and less economic burdens of CR participation. However, CR participation rate is still around 30% in Western developed countries [6] and many different aspects of barriers regardless of cost, including low referral rates, problems with transportations, work commitments, dislike of group therapy, lack of finances and insight to their illness have to be addressed in order to increase the CR participation [7,8,9,10]. Therefore, a systematic investigation of the multiple barriers to CR is urgently required to plan the appropriate strategy promoting CR utilization in Korea.
This study was designed to identify the barriers to CR participation in Korean patients with acute coronary syndrome (ACS) using the data from four university hospitals. The aim was to provide evidence to suggest a plan to overcome the barriers to CR. Korean version of the Cardiac Rehabilitation Barrier Scale (CRBS-K) [11] (Appendix 1), which has been validated in the Korean patients with myocardial infarction, was used in this study. It is an easy-to-use tool, which may enable comprehensive screening and detection of multiple variables proven as CR barriers in previous studies, and is helpful to investigate the barriers in the multiple domains.
MATERIALS AND METHODS
Data related with CR in patients with ACS from four university hospitals were used for this retrospective analysis. Data were from a total of 552 patients admitted to treat ACS (395 from Seoul National University Bundang Hospital between December 2014 and March 2016; 48 from Kangwon National University Hospital between May 2015 and April 2016; 44 from Chungnam National University Hospital between February 2016 and July 2016; 65 from Asan Medical Center between February 2016 and April 2016). The study protocol was approved by each Institutional Review Board (Seoul National University Bundang Hospital: B-1508/312-119, Kangwon National University Hospital: KNUH-2016-09-014-001, Chungnam National University Hospital: CNUH-2016-09-024, Asan Medical Center: 2016-1041).
CR protocols
CR protocols in each hospital were similar between four hospitals. Patients with ACS were automatically referred to the doctor responsible for the supervision of CR during the admission period. The CR coordinator, who was educated in the CR program, consulted the patients who had no problems in communication (e.g., severe cognitive impairment, unstable medical condition) concerning their interest in the CRBS-K. Patients were queried concerning their intent to participate in the CR program. Enrollers were defined as patients who agreed to participate in phase II CR program during the CR education session at admission. From one week to one month after discharge, patients who agreed to participate in CR visited CR outpatient clinic and were checked with symptom-limited cardiopulmonary exercise test (CPET) around 1 month after discharge if no contraindications for CPET were identified, and then proper exercise program was prescribed. If CPET was contraindicated on the first visit, patients were instructed to join the monitored exercise session for the target of moderate intensity CR exercise session. The patients who attended one or more hospital-based monitored CR sessions in the phase II within 3 months of discharge were considered CR attenders.
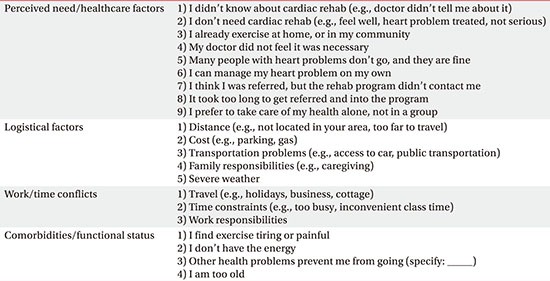
CRBS
The CRBS was developed to comprehensively investigate the barriers to CR [12]. The CRBS-K was developed and validated in patients with myocardial infarction from Seoul National University Bundang Hospital and Kangwon National University Hospital (Appendix 1) [11]. Patient's level of agreement with each CRBS item on a 5-point Likert scale, with response options ranging from 1 (strongly disagree) to 5 (strongly agree). Each item of CRBS was dichotomized; scores of 1 and 2 were considered as non-barrier, and scores of 3 to 5 considered as barrier. CRBS items was suggested to be categorized as four subscales in the previous original psychometric validation study (Appendix 2) [12]: perceived need for CR/healthcare factors (9 items), logistic factors (5 items), conflicts with work schedule/time (3 items), and comorbidities/functional status (4 items). Averages of the CRBS subscales were calculated from the scores in each item included in the subscale. Averages of total CRBS and four subscales were dichotomized with the cut-off value of 2.5, which was the median of the averages of the total CRBS: (1) ≥2.5 considered as barrier and (2) <2.5 considered as non-barrier in the present study.
Demographics and clinical data
Data collected from medical charts included age, gender, education level, working status, marital status, categories of health insurance, body mass index (BMI), family history of coronary heart disease, past medical history of diabetes, hypertension and hypercholesterolemia, smoking status before admission, ejection fraction (%) primarily measured by echocardiography during hospitalization, ACS type (ST-elevation myocardial infarction [STEMI], non-ST elevation myocardial infarction [NSTEMI], unstable angina) and percutaneous coronary intervention. Education level was categorized into high school entrance or higher and middle school graduate or lower. Health insurance was categorized into National Health Insurance and Medical Aid. Marital status was classified as married if the participant was married and currently living together with one's partner. If the participant never married, or has married but was not living with one's partner (living separately, divorced or has died) marital status was classified as ‘others’. Working status was dichotomized to employed and retired. Smoking status was dichotomized to currently smoking (smoking before admission within 1 month) and currently nonsmoking (non-smoker or ex-smoker).
Statistical analyses
Patients were divided into two groups (CR attender and CR non-attender). The differences between two groups in the demographic and clinical variables were tested using the chi-square test for the categorical variables and Student t-test for continuous variables. The group differences in each CRBS item and subscale were analyzed using chi-square test.
Subgroup analyses were performed with data from Seoul National University Bundang Hospital (n=395). The patients were grouped into those who agreed to participate in CR (CR enroller) and those who refused to participate in CR (CR non-enroller) during the education in the admission period. The differences between CR enroller and non-enroller in dichotomized CRBS subscales were analyzed using chi-square test. In addition, differences in CR attendance in the CR enrollers were tested using chi-square test in the dichotomized CRBS subscales.
RESULTS
A total of 552 patients were included in the analyses. They comprised 170 CR attenders and 382 CR non-attenders. Among the CR attenders, the median of the number of CR attendant was 2 (with range 1 to 33). A total of 395 patients among the 552 patients were underwent further analyses with the data of both enrollment and participation to the CR. They comprised 112 CR non-enrollers and 283 CR enrollers. A total of 138 patients participated CR among the 283 CR enrollers. The CR participation rate was 35% (138 of the 395), 23% (11 of 48), 14% (6 of 44) and 23% (15 of 66) in Seoul National University Bundang Hospital, Kangwon National University Hospital, Chungnam National University Hospital, and Asan Medical Center respectively. The CR participation rate in four hospital was 31% (170 of the 552). In Seoul National University Bundang Hospital, CR enrollment rate was 72% (283 of the 395). The actual participation rate among patients who enrolled to CR was 49% (138 of the 283).
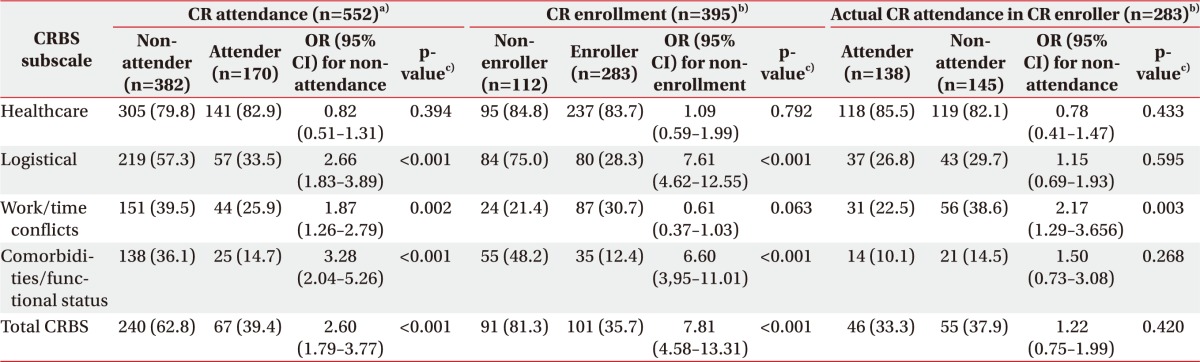
CR attenders had lower mean age, higher educational level, higher employment rate and fewer past history of hypertension compared to CR non-attenders (p<0.001, p=0.005, p=0.018, and p<0.001, respectively) (Table 1).
Table 1. Demographics in comparison with CR attendance.
Values are presented as mean±standard deviation or number (%).
CR, cardiac rehabilitation; CVD, cardiovascular disease; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention.
a)Independent t-test or chi-square test. b)n=169, c)n=369, d)n=167, e)n=344, f)n=159.
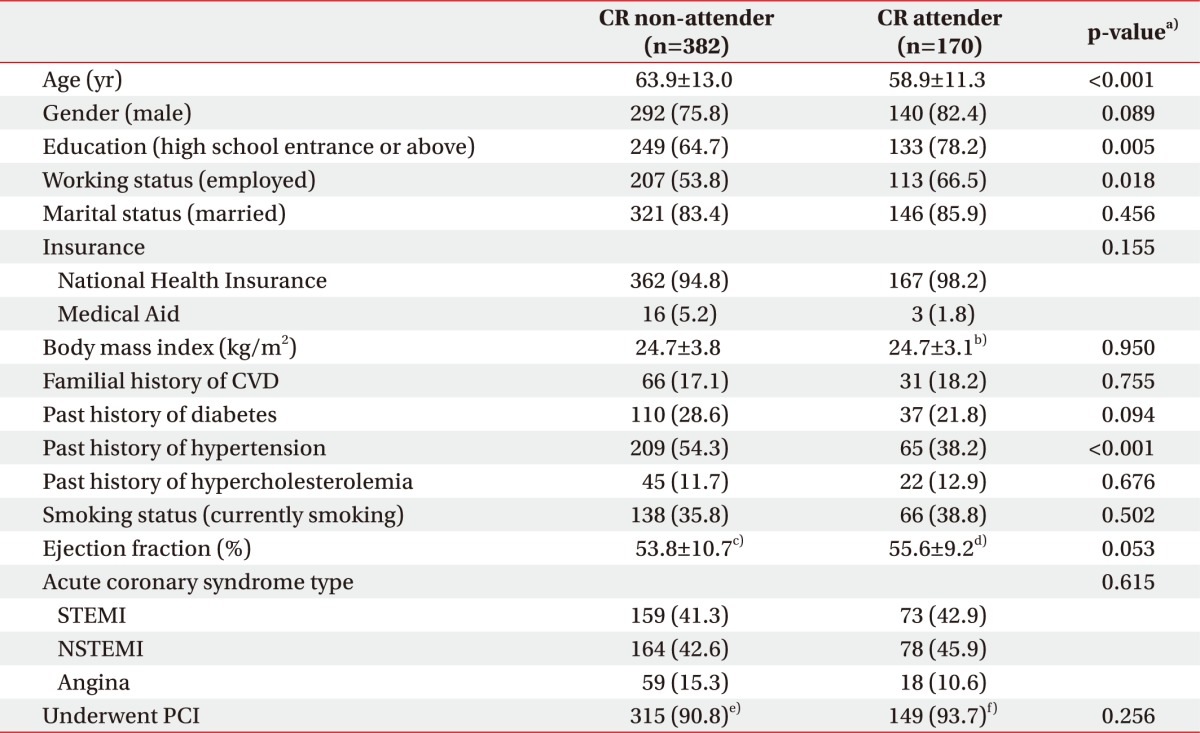
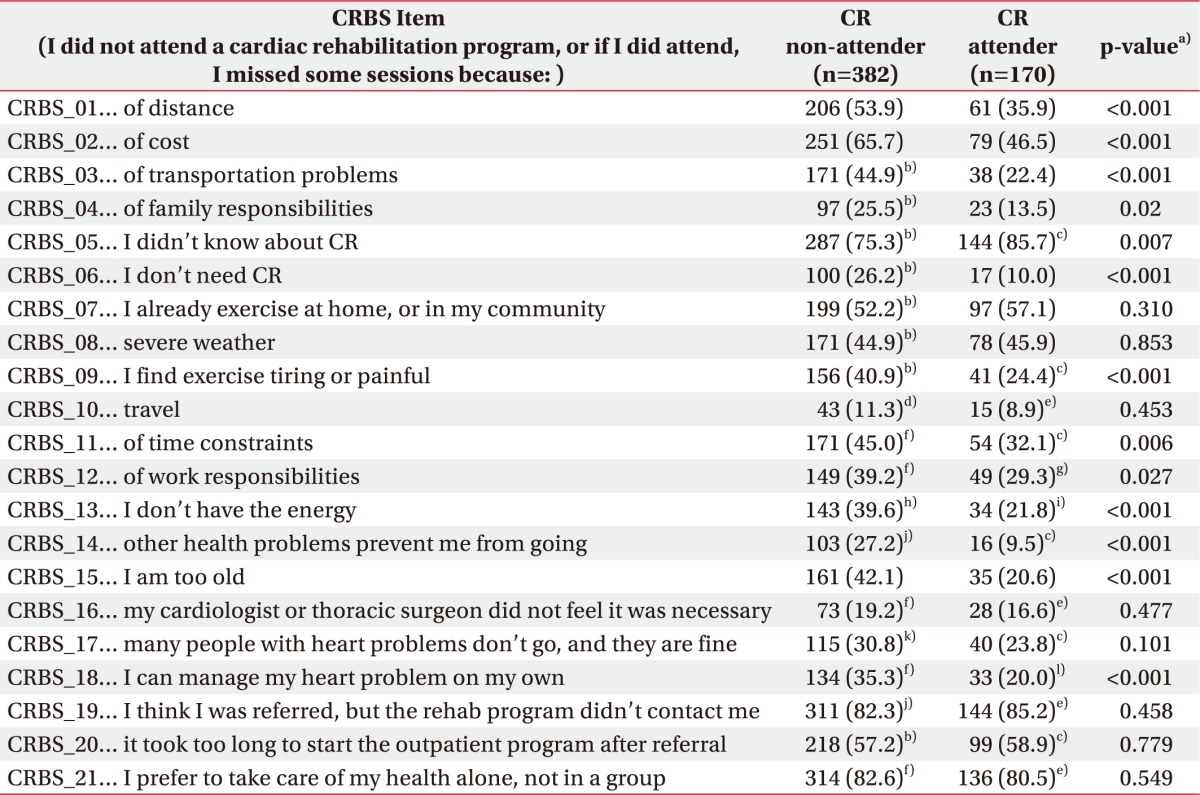
Table 2 presents the barriers identified using CRBS item by comparing CR non-attender with CR attender. The barriers were distance, cost, transportation problems, family responsibilities, lack of knowledge of CR, lack of need for CR, non-compliance with exercise, time constraints, work responsibilities, lack of energy, health problems, older age and desire of self-care instead of group care. The barriers identified by CRBS subdomains in CR attendance are presented in Table 3. Logistical factors (odds ratio [OR]=2.66; 95% confidence interval [CI], 1.826–3.885), work/time conflicts (OR=1.87; 95% CI, 1.255–2.792), comorbidities/functional status (OR=3.28; 95% CI, 2.044–5.264) and total CRBS (OR=2.60; 95% CI, 1.793–3.766) were significantly greater in CR non-attender than in CR attender (Table 3).
Table 2. CRBS items in comparison with CR attendance.
Values are presented as number (%).
CRBS, Cardiac Rehabilitation Barrier Scale; CR, cardiac rehabilitation.
a)Chi-square test. b)n=381, c)n=168, d)n=379, e)n=169, f)n=380, g)n=167, h)n=361, i)n= 156, j)n=378, k)n=373, l)n=165.
Table 3. OR with 95% CI for CR non-attendance or CR non-enrollment according to barriers in each subscale or total CRBS.
Values are presented as number of patients (%) who showed the averages of subscales in CRBS ≥2.5, unless otherwise indicated.
OR, odds ratio; CI, confidence interval; CR, cardiac rehabilitation; CRBS, Cardiac Rehabilitation Barrier Scale.
a)Data from all four hospitals. b)Data from one hospital. c)Chi-square test.
In CR enrollment, between CR enroller and non-enroller revealed logistical factors (OR=7.61; 95% CI, 4.618–12.549), comorbidities/functional status (OR=6.60; 95% CI, 3,952–11.013) were significant barriers to CR non-enrollment with CRBS subdomain analysis (Table 3). Concerning barriers to actual CR participation after enrollment, in the subgroup analysis among patients who were enrolled (agreed to participate in CR during admission), only work/time conflicts was the significant barrier to CR participation (OR=2.17; 95% CI, 1.290–3.657) (Table 3).
DISCUSSION
In this study, various items of CRBS were associated with CR enrollment and attendance among patients with ACS in Korea (Table 2). Old age [9,13], female gender [13,14], no recommendation from a cardiologist [13], no prior CR participation [13], no hospital referral for CR [13], patients denial of the severity of their illness [9], lower income/greater deprivation [9,15] and rural residence [15] have been identified as CR participation barriers. These barriers were mostly consistent with our study, except some demographic features such as female gender. CR barriers could be different from country to country [8,16,17,18] because of their health and medical care level and socioeconomic status. It is important, therefore, to investigate CR barriers in different country.
More barriers in subscales of logistical, work/time conflicts and comorbidities/functional status showed higher risk for CR non-attendance (Table 3). The CR barriers vary between patients, which indicate the need for different strategies to promote CR participation according to the individual patient barriers.
Subgroup analysis using four subscales revealed different results between enroller versus non-enroller, and participant versus non-participant among enrollers (Table 3). Patients who had the logistical factor or comorbidities/functional factor as a barrier showed 6.6 to 7.6 times higher chance of CR non-enrollment (Table 3). These patients did not come to outpatient clinic and the only chance to let them participate in CR comes during the admission period. More effort to provide the tailored CR program according to the patients' needs in the group with logistical or comorbidities/functional barriers is needed during the initial admission period. Logistical factors represent barriers to center-based cardiac rehabilitation due to reasonable issues (Appendix 2). Among logistical factors, cost is an important barrier to CR [19]. Cost will likely become less of an issue with the partial National Health Insurance coverage in Korea. However, distance, transportation problems and family responsibilities that are logistical factors [8,18] will remain hard to be overcome using the hospital-based CR program. One of the possible solutions is to refer the patients to the CR center near the residential area of the patient. This referral system can be more effective when the number of CR facility is increased, which is expected after the health insurance coverage of CR in Korea, and in the patients underwent cardiac surgery considering the fact that most of the cardiac surgery operated in the Seoul metropolitan area [20]. In the patients who cannot be referred to other CR facilities, providing an alternative CR program has to be considered in the education during the initial admission period. There are some global efforts to provide qualified community- or home-based CR as the alternative model for hospital-based CR in United States or United Kingdom [4,21]. These alternative models of CR have produced similar reductions in cardiovascular disease risk factors compared with hospital-based program with relatively higher rate of participation in CR [6,7,22].
The comorbidities/functional status in subdomains of CRBS (e.g., “I find exercise tiring or painful”, “I don't have the energy”, “Other health problems prevent me from going”, “I am too old”) were significant barriers to CR enrollment. Elderly patients (≥75 years) can derive similar benefits from CR in terms of physical function improvement, compared with younger patients [23]. But older patients are less likely than younger cardiac patients to participate in outpatient CR programs [23]. For these patients, an alternative low intensity exercise protocol considering individual fitness level, personal goals and preferences as well as medical conditions musculoskeletal disorders can be provided at the stage of education during admission and follow-up CR session [24]. In addition, an adapted CR model for persons with physical disabilities, such as stroke survivors, can be considered to provide specifically designed education sessions and adequate supervision through small class size with lower staff-to-participant ratio [25].
Among patients who agreed to join the CR during admission period, 51% did not participate in the CR program (Table 3). In this group of patients, the only significant subscale in CR barriers was work/time conflicts including time constraints and work responsibilities (Table 3). These individuals may want to join the CR program during the admission (with no significant barriers in logistical or comorbidities/functional status) but may not participate in CR after coming back to their previous usual life. To overcome the barriers in work/time conflicts, some strategies are available. Early appointment to first outpatient clinic visit is one option, which may increase the follow-up rate and can be used to facilitate the CR participation with further counseling according to individual patient's need [26]. Opening the CR clinic in the evenings or on the weekend is another strategy to overcome time/conflicts barriers. The healthcare policy to promote the CR participation after returning their usual jobs or duties is important [27]. For example, there are workplace wellness programs supported by the American Heart Association, which are an important strategy to prevent the major shared risk factors for cardiovascular disease including cigarette smoking, obesity, hypertension, dyslipidemia, physical inactivity and diabetes [28]. CR could be linked with these programs. Providing a convenient time and location for exercise and wellness programs during the workday and offering employer-provided paid time off during the workday for exercise can be promoted the participation of these programs [28].
Although the healthcare factor was not identified as a barrier in subscale analyses, it was identified as a barrier in analysis with each CRBS item: lack of need for CR and wants of self-care. Lack of understanding of their illness is one of the possible explanations for the role of healthcare factor. If patients do not understand the nature of acute myocardial infarction and/or the underlying chronic process leading to acute myocardial infarction, they may be less likely to understand the relevance of behavioral interventions such as CR [29]. Therefore, the comprehensive educations to make patients understand features of acute myocardial infarction, chronic heart disease and the role and benefits of CR may be important to overcome these healthcare-related barriers.
There are several limitations in our study. First, the data were only from the four university hospitals. Different referral system or patients' characteristics according to the regional differences can affect the results of CR barrier analysis. In order to establish generalizability and representativeness, a multicenter study with a larger sample size is needed. Second, CR barriers were assessed only at admission. Subjective barriers can change after returning to their usual life. Follow-up assessment after the patient's decision on CR participation could provide more information for CR barriers. At last, patients with other indications for CR except ACS (e.g., chronic heart failure, cardiac transplantation or cardiac surgery) were not included in this study. They have different characteristic and barriers in CR participation and enrollment from patients with ACS. For example, patients with chronic heart failure may complain heart failure symptoms such as fatigue and dyspnea as significant barriers to start exercising [30]. Therefore, further study to identify CR barriers is needed in these disease categories.
In conclusion, various barriers to CR participation were identified in Korean patients with ACS. In patients with barriers associated with logistical or comorbidities/functional status, provision of regional referral or alternative CR programs may be considered in the early education period. Patients who have time/work conflicts without the significant barriers in logistical or comorbidities/functional status showed high risk for CR non-attendance even they agreed to join CR during admission period. Other strategies such as early CR appointment, provision of evening or weekend session, healthcare policy to guarantee CR attendance during work can be considered. Further multicenter study with large sample size including other CR indication in addition to acute coronary syndrome is required.
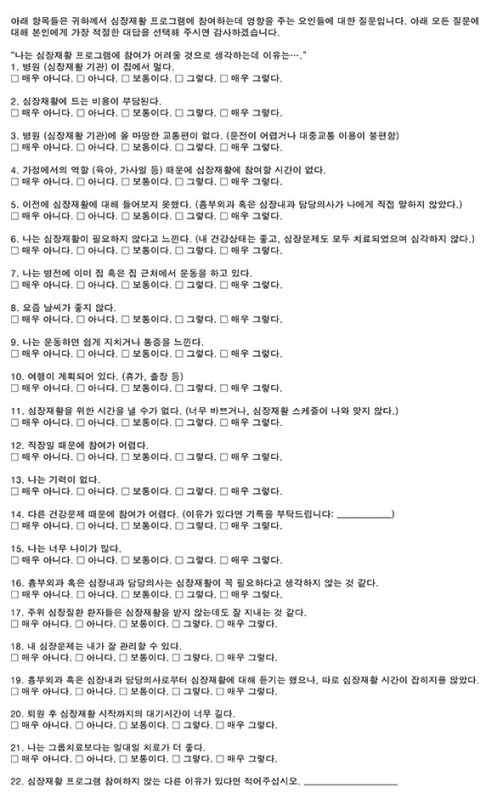
Appendix 1
Korean version of Cardiac Rehabilitation Barrier Scale (CRBS-K)
Appendix 2
Cardiac Rehabilitation Barrier Scale (CRBS) items by subscale
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67:1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 2.Smith SC, Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 3.American Association of Cardiovascular and Pulmonary Rehabilitation; American College of Cardiology Foundation; American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation) Thomas RJ, King M, Lui K, et al. AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services endorsed by the American College of Chest Physicians, the American College of Sports Medicine, the American Physical Therapy Association, the Canadian Association of Cardiac Rehabilitation, the Clinical Exercise Physiology Association, the European Association for Cardiovascular Prevention and Rehabilitation, the Inter-American Heart Foundation, the National Association of Clinical Nurse Specialists, the Preventive Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2010;56:1159–1167. doi: 10.1016/j.jacc.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. Core components of cardiac rehabilitation/ secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 5.Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ. 2015;351:h5000. doi: 10.1136/bmj.h5000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015;22:35–74. doi: 10.1177/2047487313501093. [DOI] [PubMed] [Google Scholar]
- 7.Dalal HM, Taylor RS. Telehealth technologies could improve suboptimal rates of participation in cardiac rehabilitation. Heart. 2016;102:1155–1156. doi: 10.1136/heartjnl-2016-309429. [DOI] [PubMed] [Google Scholar]
- 8.Endo N, Goto A, Suzuki T, Matsuda S, Yasumura S. Factors associated with enrollment and adherence in outpatient cardiac rehabilitation in Japan. J Cardiopulm Rehabil Prev. 2015;35:186–192. doi: 10.1097/HCR.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 9.Cooper AF, Jackson G, Weinman J, Horne R. Factors associated with cardiac rehabilitation attendance: a systematic review of the literature. Clin Rehabil. 2002;16:541–552. doi: 10.1191/0269215502cr524oa. [DOI] [PubMed] [Google Scholar]
- 10.Kim C, Lim HS, Ahn JK, Bang IK, Lee SM, Kim YJ. The reasons that cardiac patients did not participate in and drop out from the cardiac rehabilitation program. J Korean Acad Rehabil Med. 2002;26:790–796. [Google Scholar]
- 11.Baek S, Park HW, Lee Y, Grace SL, Kim WS. Translation, cross-cultural adaptation and psychometric validation of the Korean-Language Cardiac Rehabilitation Barriers Scale (CRBS-K) Ann Rehabil Med. 2017;41:858–867. doi: 10.5535/arm.2017.41.5.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shanmugasegaram S, Gagliese L, Oh P, Stewart DE, Brister SJ, Chan V, et al. Psychometric validation of the cardiac rehabilitation barriers scale. Clin Rehabil. 2012;26:152–164. doi: 10.1177/0269215511410579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunlay SM, Witt BJ, Allison TG, Hayes SN, Weston SA, Koepsell E, et al. Barriers to participation in cardiac rehabilitation. Am Heart J. 2009;158:852–859. doi: 10.1016/j.ahj.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grace SL, Gravely-Witte S, Kayaniyil S, Brual J, Suskin N, Stewart DE. A multisite examination of sex differences in cardiac rehabilitation barriers by participation status. J Womens Health (Larchmt) 2009;18:209–216. doi: 10.1089/jwh.2007.0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shanmugasegaram S, Oh P, Reid RD, McCumber T, Grace SL. Cardiac rehabilitation barriers by rurality and socioeconomic status: a cross-sectional study. Int J Equity Health. 2013;12:72. doi: 10.1186/1475-9276-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Melo Ghisi GL, Oh P, Benetti M, Grace SL. Barriers to cardiac rehabilitation use in Canada versus Brazil. J Cardiopulm Rehabil Prev. 2013;33:173–179. doi: 10.1097/HCR.0b013e3182930c9f. [DOI] [PubMed] [Google Scholar]
- 17.Babu AS, Veluswamy SK. Barriers to cardiac rehabilitation in India. J Prev Cardiol. 2016;5:871–876. [Google Scholar]
- 18.Chamosa S, Alarcon JA, Dorronsoro M, Madruga FJ, Barrera J, Arrazola X, et al. Predictors of Enrollment in Cardiac Rehabilitation Programs in Spain. J Cardiopulm Rehabil Prev. 2015;35:255–262. doi: 10.1097/HCR.0000000000000126. [DOI] [PubMed] [Google Scholar]
- 19.Harlan WR, 3rd, Sandler SA, Lee KL, Lam LC, Mark DB. Importance of baseline functional and socioeconomic factors for participation in cardiac rehabilitation. Am J Cardiol. 1995;76:36–39. doi: 10.1016/s0002-9149(99)80797-8. [DOI] [PubMed] [Google Scholar]
- 20.Statistics Korea. Operation by province and type of medical institution (general hospital) in Korea. Daejeon: Statistics Korea; 2015. [Google Scholar]
- 21.National Clinical Guideline Centre. MI-secondary prevention: secondary prevention in primary and secondary care for patients following a myocardial infarction: partial update of NICE CG48. London: Royal College of Physicians; 2013. [PubMed] [Google Scholar]
- 22.Buckingham SA, Taylor RS, Jolly K, Zawada A, Dean SG, Cowie A, et al. Home-based versus centre-based cardiac rehabilitation: abridged Cochrane systematic review and meta-analysis. Open Heart. 2016;3:e000463. doi: 10.1136/openhrt-2016-000463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Audelin MC, Savage PD, Ades PA. Exercise-based cardiac rehabilitation for very old patients (≥75 years): focus on physical function. J Cardiopulm Rehabil Prev. 2008;28:163–173. doi: 10.1097/01.HCR.0000320066.58599.e5. [DOI] [PubMed] [Google Scholar]
- 24.Perez-Terzic CM. Exercise in cardiovascular diseases. PM R. 2012;4:867–873. doi: 10.1016/j.pmrj.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Tang A, Marzolini S, Oh P, McIlroy WE, Brooks D. Feasibility and effects of adapted cardiac rehabilitation after stroke: a prospective trial. BMC Neurol. 2010;10:40. doi: 10.1186/1471-2377-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pack QR, Mansour M, Barboza JS, Hibner BA, Mahan MG, Ehrman JK, et al. An early appointment to outpatient cardiac rehabilitation at hospital discharge improves attendance at orientation: a randomized, single-blind, controlled trial. Circulation. 2013;127:349–355. doi: 10.1161/CIRCULATIONAHA.112.121996. [DOI] [PubMed] [Google Scholar]
- 27.Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124:2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 28.Carnethon M, Whitsel LP, Franklin BA, Kris-Etherton P, Milani R, Pratt CA, et al. Worksite wellness programs for cardiovascular disease prevention: a policy statement from the American Heart Association. Circulation. 2009;120:1725–1741. doi: 10.1161/CIRCULATIONAHA.109.192653. [DOI] [PubMed] [Google Scholar]
- 29.French DP, Cooper A, Weinman J. Illness perceptions predict attendance at cardiac rehabilitation following acute myocardial infarction: a systematic review with meta-analysis. J Psychosom Res. 2006;61:757–767. doi: 10.1016/j.jpsychores.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 30.Conraads VM, Deaton C, Piotrowicz E, Santaularia N, Tierney S, Piepoli MF, et al. Adherence of heart failure patients to exercise: barriers and possible solutions: a position statement of the Study Group on Exercise Training in Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2012;14:451–458. doi: 10.1093/eurjhf/hfs048. [DOI] [PubMed] [Google Scholar]