Abstract
A “health shock,” that is, a large, unanticipated adverse health event, can have long‐term financial implications for patients and their families. Colorectal cancer is the third most commonly diagnosed cancer among men and women and is an example of a specific health shock. We examined whether specific benefits (employer‐based health insurance, paid sick leave, extended sick leave, unpaid time off, disability benefits) are associated with job retention after diagnosis and treatment of colorectal cancer. In 2011–14, we surveyed patients with Stage III colorectal cancer from two representative SEER registries. The final sample was 1301 patients (68% survey response rate). For this study, we excluded 735 respondents who were not employed and 20 with unknown employment status. The final analytic sample included 546 respondents. Job retention in the year following diagnosis was assessed, and multivariable logistic regression was used to evaluate associations between job retention and access to specific employment benefits. Employer‐based health insurance (OR = 2.97; 95% CI = 1.56–6.01; P = 0.003) and paid sick leave (OR = 2.93; 95% CI = 1.23–6.98; P = 0.015) were significantly associated with job retention, after adjusting for sociodemographic, clinical, geographic, and job characteristics.
Keywords: Colorectal neoplasms, employment, insurance, health, sick leave, surveys and questionnaires
Although implementation of the Patient Protection and Affordable Care Act (ACA) expanded access to preventive medical care among working Americans who were uninsured or underinsured 1, serious illness still may cause considerable financial burden 2, 3, 4. For a substantial number of patients, bankruptcy due to serious illness or its treatment is a real risk 4, 5. The risk of bankruptcy and attendant financial burden is exacerbated by illness‐ or treatment‐related job loss 6. Employment benefits such as paid sick leave and disability benefits may help working patients retain their jobs during and after serious illness. Among workers who are eligible, the Family Medical Leave Act (FMLA) provides protection for short‐term disability in the form of unpaid leave and has been shown to influence job retention among new mothers 7.
The provision of paid medical leave, however, is not mandated under FMLA or the ACA, nor is it a part of standard health insurance coverage 2. In fact, 40% of US workers do not have access to FMLA 8 and up to 60% do not have access to paid sick leave 9. A substantial proportion of workers who experience a “health shock,” that is, a large, unanticipated adverse health event, may therefore lack the employment benefits needed to undergo treatment, recover, and return to work. Additionally, a robust literature has shown the effect of health shocks on labor outcomes 10, 11, 12, 13. These studies frequently use broad proxies for the health shock, such as changes in self‐reported health status or the presence of an inpatient stay. We addressed this issue in more granular detail by focusing on colorectal cancer, a specific health shock.
Colorectal cancer is a prevalent and serious illness frequently diagnosed among working adults without prior warning 14, 15. Treatment for advanced but curable (Stage III) colorectal cancer typically requires both major surgery and chemotherapy, initiated within 4 months of diagnosis and lasting up to 9 months. Cancer treatment can disrupt a working person's day‐to‐day life physically and economically for some or all of this time. Working‐age cancer survivors, who may be supporting young families or repaying educational debt and face a greater loss of potential earnings than older survivors, are more likely to report financial hardship 16. In previous work, we reported that as a result of diagnosis or treatment, over 50% of colorectal cancer patients reduce spending on general expenses, one‐third use savings, one‐third cut down on spending for food or clothing 3, 17, and nearly 50% who are employed at the time of diagnosis are unable to retain their jobs 6. In this study, we used data from a population‐based survey of patients with Stage III colorectal cancer to examine the association of employee benefits (employer‐based health insurance, paid sick leave, extended sick leave, unpaid time off, disability benefits) with job retention.
Methods
Study population
We identified all patients ≥18 years of age with surgically resected, pathologic Stage III colon or rectal cancer reported to the Surveillance, Epidemiology and End Results (SEER) cancer registries of metropolitan Detroit and the state of Georgia between 1 August 2011 and 31 December 2014. These sites were selected because of their demographically and racially diverse patient populations. Patients were eligible for study recruitment at 4 months following diagnosis, when all treatment should have been initiated, and returned surveys were accepted up to 12 months after diagnosis. Exclusion criteria included metastatic cancer (Stage IV) at diagnosis, change in diagnosis based on final histology, death prior to survey deployment, or residence outside SEER catchment area. We also excluded respondents who reported no employment at the time of diagnosis.
Data collection
We notified physicians of our intention to contact study subjects. After an opt‐out period by physicians, patients were invited to participate using a modified multimodal Dillman approach 18. Upon receipt of surveys, we performed extensive data checks for logic, errors, and omissions. We recontacted patients as necessary to obtain missing information and supplemented data with SEER registry‐provided clinical data and census tract‐level socioeconomic status (SES) data through a 2010 Census linkage.
The study protocol was approved by the institutional review boards of the University of Michigan, Wayne State University, Emory University, the State of Michigan, and the State of Georgia Department of Public Health.
Measures
The primary outcome was job retention at the time of survey. We asked respondents who were employed at the time of diagnosis if they were working at the time of survey completion (mean 8 months later). We validated responses with the additional survey question: “Are you currently working for pay?” (yes/no response). We also asked patients how much work they had missed as a result of cancer or its treatment.
We also explored “job lock”—whether individuals remained in their jobs due to fear that they would otherwise lose health insurance coverage for themselves or their families 19. We assessed this by asking patients whether, as a result of their colorectal cancer diagnosis or treatment, they kept their job mainly to keep their health insurance (yes/no response).
The primary exposure, availability of employment benefits, was assessed by asking respondents whether any of the following were available to them through their employer during cancer treatment: employer‐based health insurance, paid sick leave, extended sick leave, disability, unpaid leave, “other.” Respondents could select all that applied; 83 respondents left one or more of the benefit options blank. They were included in bivariate analyses but excluded from multivariable regression models. Additional covariates included self‐reported patient‐level sociodemographic characteristics: age at diagnosis, gender, race, marital status, level of educational attainment, annual household income, comorbid conditions before the cancer diagnosis, overall health status, availability and type of health insurance (none, Medicaid, Medicare, Private: employer‐based, self‐purchased, and through spouse); area‐level characteristics: geographic region, area‐level socioeconomic status (SES) index (principle component analysis of area‐level high school degree, college degree, poverty level combined into a composite standardized measure of the economic environment); and job‐related characteristics: type of occupation (white collar/blue collar derived from patient‐reported categories of manual, clerical, management/professional, military, self‐employed). The majority (>90%) of employed respondents received adjuvant chemotherapy. Thus, we did not include chemotherapy receipt as a covariate.
There were few missing values (<2%) for all variables except annual household income, for which 19% of patients did not respond or reported they did not know. Multiple imputation techniques were used to account for the missing annual household income data.
Statistical analyses
Our analytic sample consisted of all survey respondents who were working for pay at the time of cancer diagnosis. We generated descriptive statistics of time away from work due to diagnosis and treatment. We evaluated the association of job retention with patient‐level sociodemographic, area‐level, and job‐related covariates. We then examined the association of job retention with the availability of specified employment benefits. Chi‐squared tests were used to assess bivariate associations. We conducted a sensitivity analysis by constructing a cumulative variable counting the total number of job support benefits available to each respondent (range 0–6). This was tested in each model and yielded similar results to the models that used individual employment benefits. The exclusion of working patients over age 65 did not significantly change any results. Thus, they are included in the study.
To examine the relative impact of sociodemographic, area‐level, and job‐related factors (including employment benefits), on job retention, we used multivariable logistic regression to predict job retention, accounting only for patient‐level sociodemographic and area‐level covariates in the first model. We then added job‐related covariates including employment supports in a second model. Finally, as a sensitivity analysis, we fitted multivariable logistic regression to model job retention as a function of patient‐level sociodemographic and area‐level covariates as well as employment benefits, stratified by type of occupation (blue collar vs. white collar). The results of the stratified analyses were similar to those of the unstratified analysis and are therefore not described in more detail.
To address potential confounding by worker selection into “good jobs” (those more likely to offer employment benefits) and “bad jobs” (those less likely to offer employment benefits), we employed propensity score‐based analysis. We selected the availability of paid sick leave as the indicator variable in our propensity score analysis because it is policy‐relevant and the most tangible of the employment benefits investigated in our studies. Availability of paid sick leave was analyzed as a patient‐reported dichotomous variable (paid sick leave yes/no). In the first step of the analyses, propensity scores were estimated based on a logit model of the paid sick leave indicator variable, given the observed covariates age, race, education, gender, marital status, income, number of comorbid conditions, job category, SEER site, and composite census‐level SES. The propensity score for an individual, defined as the conditional probability of having paid sick leave given the individual's covariates, has been shown to serve as a balancing score and can be used to reduce bias due to any covariate imbalance 20. Once estimated, the propensity scores were grouped into quintiles. Logistic regression was used in the second‐step analysis to model job retention as a function of the availability of paid sick leave and sociodemographic, area‐level, and job‐related factors, including other employment benefits, and propensity score quintiles from the first‐step model. Additional information demonstrating the adequacy of the propensity score analysis is presented in the Statistical Appendix.
We evaluated bivariate associations between the exploratory outcome of job lock and covariates using chi‐squared tests. Wald F‐tests were used to assess associations and multivariable logistic regression for adjusted analyses. All statistical tests were two‐sided. P value <0.05 was considered statistically significant. Multicollinearity between covariates was tested using the variance inflation factor, and all pairwise interactions were tested for significance. All analyses were conducted using SAS 9.4 software (Cary, NC).
Results
Study sample and response rate
We identified 2168 patients with Stage III colorectal cancer reported to the SEER registries of Georgia and Detroit using Rapid Case Ascertainment. Among these, 259 (12%) were later determined ineligible (metastatic disease, noncolorectal primary, prior cancer diagnosis, residing outside the registry catchment area). Among 1909 eligible patients included in the final sample, 608 could not be located or did not return the survey, leaving 1301 patients (68% survey response rate). For this study, patients who were not working at the time of diagnosis (n = 735) and those missing employment information (n = 20) were excluded, leaving a final analytic cohort of 546 respondents.
Overall respondent characteristics and job impact
Among 546 employed respondents, 57% were male, 69% were white, 67% were married, 28% reported high school education or less, 38% reported annual household income less than $50,000, and 33% reported two or more comorbid conditions (Table 1). Eighteen percent of employed respondents were age 65 or older, reflective of broader trends in the US labor force: In 2010, 17.4% of US workers were over age 65 21. As a result of colorectal cancer diagnosis and treatment, 17% of respondents missed <1 month of work, 29% missed 1–3 months, 20% missed 3–6 months, and 17% missed 6–12 months of work.
Table 1.
Patient sociodemographic and area‐level characteristics and job retention among working respondents
| Patient characteristic | N = 546 | % Retained job | P‐value |
|---|---|---|---|
| Sociodemographic | |||
| Age | |||
| <50 | 164 | 54 | 0.759 |
| 50–64 | 285 | 57 | |
| ≥65 | 96 | 54 | |
| Gender | |||
| Male | 309 | 62 | 0.001 |
| Female | 233 | 48 | |
| Race | |||
| White | 371 | 62 | <0.001 |
| Black | 138 | 43 | |
| Other | 32 | 38 | |
| Marital status | |||
| Not married/partnered | 181 | 50 | 0.005 |
| Married/partnered | 363 | 60 | |
| Education | |||
| <High school | 48 | 23 | <0.001 |
| High school | 104 | 41 | |
| Some college | 194 | 52 | |
| College graduate | 192 | 74 | |
| Household incomea | |||
| <$20,000 | 48 | 13 | <0.001 |
| $20,000–$49,000 | 136 | 44 | |
| $50,000–$89,000 | 161 | 60 | |
| ≥$90,000 | 139 | 78 | |
| Comorbid conditions | |||
| 0 | 182 | 64 | 0.001 |
| 1 | 182 | 58 | |
| 2 or more | 180 | 44 | |
| Overall health | |||
| Excellent | 164 | 75 | <0.001 |
| Good | 285 | 64 | |
| Poor | 96 | 20 | |
| Area‐level | |||
| SEER site | |||
| Detroit | 162 | 53 | 0.458 |
| Georgia | 382 | 57 | |
| Area‐level SES, tertile | |||
| High | 165 | 71 | <0.001 |
| Medium | 206 | 53 | |
| Low | 171 | 44 | |
Information about household income was missing for 19% of respondents and was imputed in subsequent multivariate models.
Fifty‐five percent of working respondents retained their jobs. In unadjusted analyses, those who retained their jobs were significantly more likely to be male, white, married, and to report a higher level of educational attainment, higher annual household income, 0 or 1 comorbid conditions, and excellent health (all P < 0.01). Those residing in the upper tertile of area‐level SES were also significantly more likely to retain their jobs (P < 0.01).
Employment benefits and job retention
Among working respondents, 70% reported availability of employer‐based health insurance (Table 2). Fifty‐one percent reported availability of paid sick leave, 52% extended sick leave, 46% unpaid time off, and 57% disability benefits. Thirteen percent of respondents reported no health‐related employment benefits. These respondents were more likely to be older, black, self‐employed, and report lower annual household income (all P < 0.01; data not shown). Respondents aged 65 and older were significantly less likely to have each of the employment benefits compared with younger respondents.
Table 2.
Job‐related characteristics and job retention
| Patient characteristic | N = 546 | Retained job (%) | P‐value |
|---|---|---|---|
| Job category | |||
| Blue collar | 188 | 35 | <0.001 |
| White collar | 322 | 66 | |
| Unclassified/unknown | 12 | 58 | |
| Employer‐based health insurance | |||
| No | 163 | 34 | <0.001 |
| Yes | 381 | 65 | |
| Paid sick leave | |||
| No | 241 | 45 | <0.001 |
| Yes | 253 | 67 | |
| Extended sick leave | |||
| No | 233 | 51 | 0.038 |
| Yes | 255 | 60 | |
| Unpaid time off | |||
| No | 271 | 49 | 0.004 |
| Yes | 231 | 62 | |
| Disability benefits | |||
| No | 206 | 30 | <0.001 |
| Yes | 278 | 76 | |
In unadjusted analyses, those who retained their jobs were significantly more likely to have each of the individual employment benefits (employer‐based health insurance, paid sick leave, extended sick leave, unpaid time off, disability benefits) available. Additionally, in a count of employment benefits, we noted a linear association between the number of available benefits and odds of job retention (P < 0.01; data not shown).
Relative impact of patient‐level sociodemographic, area‐level, and job‐related characteristics on job retention
In the fully adjusted model including individual‐ and area‐level variables (age, education, income, race, gender, marital status, comorbid conditions, overall health, SEER site, and area‐level socioeconomic status) as well as job characteristics, availability of employer‐based health insurance (OR = 2.97; 95% CI = 1.56–6.01; P = 0.003) and availability of paid sick leave (OR = 2.93; 95% CI = 1.23–6.98; P = 0.015) were significantly associated with job retention. Patients with poor health were less likely than those with good health to retain their jobs (OR = 0.07; 95% CI = 0.03–0.16; P < 0.01). While income was significantly associated with job retention in the first model controlling for only sociodemographic and area‐level characteristics, it was no longer significant in the second model that additionally accounted for job‐related characteristics (Table 3). In addition, blue‐collar workers were significantly more likely than white‐collar workers to report “job lock,” that is, that they kept their jobs in order to maintain health insurance (25% vs. 16%; P = 0.02). There were no significant differences in job lock by age of respondent.
Table 3.
Multivariable logistic regression of job retention
| Model 1: Hazard ratio (HR) of job retention by sociodemographic and area‐level characteristics | Model 2: HR of job retention (Model 1 + job‐related characteristics) | |||
|---|---|---|---|---|
| HR (95% CI) | P‐value | HR (95% CI) | P‐value | |
| Age | ||||
| <50 | 1.0 (ref) | 0.611 | 1.0 (ref) | 0.265 |
| 50–64 | 1.34 (0.74–2.42) | 1.18 (0.64–2.16) | ||
| >65 | 1.34 (0.58–3.10) | 2.12 (1.85–5.28) | ||
| Education | ||||
| <High school | 1.0 (ref) | 0.122 | 1.0 (ref) | 0.386 |
| High school | 1.80 (0.55–5.87) | 1.61 (0.48–5.34) | ||
| Some college | 1.70 (0.52–5.55) | 1.10 (0.33–3.67) | ||
| College graduate | 3.20 (0.93–10.98) | 1.86 (0.52–6.60) | ||
| Income | ||||
| <$20K | 1.0 (ref) | 0.002 | 1.0 (ref) | 0.404 |
| $20–$49K | 2.85 (1.22–6.68) | 1.20 (0.48–3.00) | ||
| $50–$89K | 3.81 (1.49–9.75) | 1.37 (0.50–3.73) | ||
| ≥$90K | 7.65 (2.68–21.87) | 2.31 (0.72–7.38) | ||
| Overall health | ||||
| Excellent | 1.0 (ref) | <0.001 | 1.0 (ref) | <0.001 |
| Good | 0.68 (0.35–1.30) | 0.61 (0.28–1.31) | ||
| Poor | 0.07 (0.03–0.16) | 0.06 (0.03‐0.14) | ||
| Job category | ||||
| White collar | 1.0 (ref) | 0.247 | ||
| Blue collar | 0.56 (0.28–1.11) | |||
| Unclassified | 0.68 (0.13–3.73) | |||
| Employer‐based health insurance | ||||
| No | 1.0 (ref) | 0.003 | ||
| Yes | 2.97 (1.56–6.01) | |||
| Paid sick leave | ||||
| No | 1.0 (ref) | 0.015 | ||
| Yes | 2.93 (1.23–6.98) | |||
| Extended sick leave | ||||
| No | 1.0 (ref) | 0.335 | ||
| Yes | 1.41 (0.61–2.12) | |||
| Unpaid time off | ||||
| No | 1.0 (ref) | 0.411 | ||
| Yes | 0.79 (0.44–1.40) | |||
| Disability benefits | ||||
| No | 1.0 (ref) | 0.109 | ||
| Yes | 0.55 (0.27–1.14) | |||
95% CI: 95% confidence interval. SEER: Surveillance Epidemiology and End Results cancer registry; area‐level SES: geographic socioeconomic status based upon census income and education data aggregated at the zip‐code level.
In the preliminary adjusted model that included individual‐ and area‐level variables, only annual household income and overall health were significantly associated with job retention. In the fully adjusted model including job characteristics, income was no longer statistically significant. Both models were also adjusted for race, gender, marital status, comorbid conditions, SEER site, and area‐level socioeconomic status (SES). These covariates were not statistically significant and are therefore omitted from the table.
In the propensity score analysis, paid sick leave remained independently significantly predictive of job retention after adjusting for all other covariates as well as propensity quintile (P = 0.02). We did not find significant differences in job retention by gender nor did we find significant two‐way interactions with gender.
Discussion
Stage III colorectal cancer is a major unexpected illness that can have long‐term financial implications for patients and their families. Among employees diagnosed with Stage III colon cancer, employment benefits designed to ameliorate health shock related to job loss worked as expected. Even after controlling for patient‐level sociodemographic, area‐level, and job‐related characteristics, the availability of employer‐based health insurance and paid sick leave were significantly associated with job retention. Our specific investigation of paid sick leave was robust to multiple sensitivity analyses including adjusting for propensity score quintiles and stratifying the multivariable logistic regression model by type of occupation, supporting a causal relationship irrespective of individual, area‐level, and job characteristics.
While job retention did not vary significantly between blue‐collar and white‐collar workers, blue‐collar workers were significantly more likely to endorse “job lock” phenomenon; 25% reported that they kept their jobs in order to keep their health insurance. These findings highlight the vulnerability of some patients based on occupation, the complexity of employment impacts of health shocks, and the nuanced role health insurance plays in patients’ employment decisions and financial well‐being. While insurance coverage concerns may have been partially alleviated by the Affordable Care Act, as insurance options in the United States continue to evolve, it will become even more important to understand the role of insurance and employment in the face of a health shock and for clinicians and policy makers to recognize not only who is at risk for job loss, but also the complex reasons that patients may continue to work.
We also noted inherent socioeconomic disparities in access to employment benefits. Thirteen percent of our study sample reported a complete lack of employment benefits. These respondents were more likely to be older, black, self‐employed, and to report lower annual household income. Our results align with data from the Bureau of Labor Statistics that high‐wage earners and those in professional and managerial occupations are more than twice as likely as low‐wage earners and those with jobs in the service industry to have access to paid sick leave 22. Even among desirable jobs that offer benefits like health insurance and paid sick leave, cancer and its treatment may compound serious illness with personal financial burden 17. For those patients who are at a competitive disadvantage in the marketplace and simultaneously less likely to work for employers who offer benefits, a curable but serious illness such as cancer may be financially devastating. While those patients who are unable to retain their jobs may be eligible to collect unemployment or social security benefits, many are not eligible and those who are receive only a fraction of their previous earnings.
As noted, federal legislation to protect the jobs and health insurance of workers during illness exists as FMLA. Unfortunately, FMLA guarantees only unpaid time off and not all employees are eligible for coverage, even if their employers offer it 8. There have been several attempts to fill the gaps left by FMLA. Statewide paid sick day legislation is in place in four states as well as in the District of Columbia and 18 other municipalities across the United States 23. In September 2015, President Obama issued an Executive Order requiring federal contractors to offer paid sick days to their employees, though this does not extend to Americans working in the private sector 24 and, as an Executive Order, is reversible. Nevertheless, only an estimated one in three workers in the bottom quarter of the pay scale and one in four part‐time workers nationwide have access to paid sick leave 20.
Making policy recommendations regarding employer practices and benefits is difficult. Benefit programs that work well for large employers may be problematic for smaller organizations, especially given the complex state and federal regulations already in place. The costs of workforce turnover or other resources consumed by disruption of organizational stability due to loss of experienced workers are real but complex. In addition, societal costs and benefits associated with such policies have only been preliminarily reported. For example, workers who are able to maintain employment during health shocks rely less on public assistance and contribute more money to their local economies 8, 25.
Our study was subject to several limitations intrinsic to survey research. Analyses were limited by the sample of respondents. We note, however, that the population‐based sampling achieved broad demographic representation and the 68% response rate is higher than any previous published cohort of patients with colorectal cancer 26. The survey relied on respondent report and was thus subject to recall bias, but our reliance on patient reporting permitted individual insights that could not otherwise be obtained. We mitigated recall bias by accepting returned surveys only up until 1 year after diagnosis. Given this relatively short follow‐up period, it is possible that respondents who did not retain their jobs during cancer treatment may have later returned to work. However, previous literature indicates that job loss during cancer treatment, particularly among low‐income patients, predicts long‐term departure from the workforce 27, 28. On the other hand, previous work has found that some cancer patients who temporarily stop working during treatment but then return to work in the first year after diagnosis, as well as some patients who continue to work through treatment and the first year afterward, subsequently quit their jobs for cancer‐related reasons in years 2–5 following diagnosis 29. Therefore, it is also possible that some respondents who retained their jobs may have later departed from the workforce. Because our data were patient‐reported, we did not have access to employer‐level data such as employer size, FMLA availability, or employer‐level benefits. Although we used job retention, defined as working for pay at the time of survey completion, as our primary outcome measure, we acknowledge that there are other measures of employment impacts (decreasing work hours, changing jobs, etc.) among working patients with cancer. We note, however, that job retention reflects the ability to continue to work and earn an income and therefore represents an important element of working patients’ financial well‐being. We did not ask patients who did not retain their jobs whether the work loss was desired or undesired. However, any departure from the labor force reduces a patient's income and may therefore exacerbate the personal financial burden of cancer diagnosis and treatment. There may be unobserved selection bias as we excluded those patients who were not employed at diagnosis from our analyses. Some of these patients could have been previously employed but subsequently chose unemployment based on poor employment benefits or a lack of employment benefits. Finally, although our sample includes patients from rural to urban areas as well as Southern and Midwestern parts of the United States, our data may not be representative of the entire United States.
Conclusion
Employment benefits, specifically employer‐based health insurance and paid sick leave, were associated with a greater likelihood of job retention during serious illness. Although insurance coverage is on the rise with implementation of the Affordable Care Act, FMLA is more than 20 years old and leaves millions of working Americans potentially unsupported in times of serious illness. Based on our findings, it is plausible that provision of specific employment benefits by employers and government could facilitate job retention and reduce associated financial burden, especially among young working patients.
Conflicts of Interest
None declared.
Appendix 1.
Statistical appendix: Propensity score model
Figure A1. Distribution of propensity scores by availability of paid sick leave.
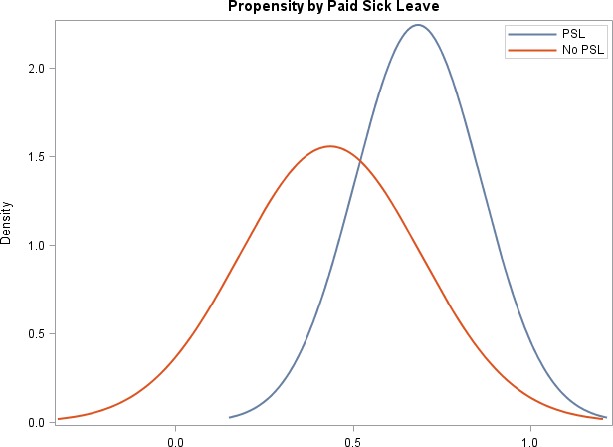
Distribution of propensity scores for patients with and without paid sick leave (PSL)
Table A1.
Propensity quintile bivariates
| Covariate | Quintile 1 (%) | Quintile 2 (%) | Quintile 3 (%) | Quintile 4 (%) | Quintile 5 (%) |
|---|---|---|---|---|---|
| Age | |||||
| <50 | 11 | 16 | 19 | 27 | 27 |
| 50–64 | 10 | 20 | 24 | 23 | 23 |
| 65+ | 65 | 27 | 8 | 0 | 0 |
| Race | |||||
| White | 19 | 21 | 19 | 23 | 19 |
| Black | 23 | 18 | 22 | 11 | 26 |
| Other | 31 | 8 | 38 | 23 | 0 |
| Education | |||||
| <High school | 56 | 31 | 7 | 7 | 0 |
| High school grad | 28 | 31 | 23 | 7 | 11 |
| Some college | 17 | 21 | 22 | 18 | 21 |
| College grad | 10 | 10 | 19 | 32 | 28 |
| Gender | |||||
| Male | 19 | 25 | 21 | 22 | 14 |
| Female | 21 | 13 | 19 | 18 | 28 |
| Marital | |||||
| Not married | 27 | 18 | 21 | 13 | 21 |
| Married | 17 | 21 | 19 | 24 | 20 |
| Income | |||||
| <$20K | 85 | 15 | 0 | 0 | 0 |
| $20–$49K | 21 | 33 | 28 | 12 | 6 |
| $50–$89K | 8 | 20 | 25 | 21 | 25 |
| >$90K | 7 | 9 | 13 | 35 | 36 |
| Geographic site | |||||
| Detroit | 28 | 25 | 22 | 20 | 5 |
| Georgia | 17 | 18 | 19 | 20 | 26 |
| SES | |||||
| Comorbid conditions | |||||
| 0 | 15 | 18 | 24 | 32 | 12 |
| 1 | 18 | 13 | 19 | 16 | 34 |
| 2+ | 27 | 29 | 17 | 13 | 14 |
| Job category | |||||
| White collar | 9 | 12 | 16 | 31 | 32 |
| Blue collar | 35 | 36 | 27 | 3 | 0 |
| Other | 100 | 0 | 0 | 0 | 0 |
| Employer‐based health insurance | |||||
| No | 39 | 26 | 19 | 8 | 8 |
| Yes | 13 | 18 | 20 | 25 | 25 |
| Paid sick leave | |||||
| No | 5 | 18 | 19 | 28 | 30 |
| Yes | 37 | 25 | 21 | 9 | 8 |
| Extended sick leave | |||||
| No | 7 | 15 | 21 | 28 | 28 |
| Yes | 31 | 25 | 19 | 11 | 13 |
| Unpaid time off | |||||
| No | 12 | 19 | 21 | 24 | 24 |
| Yes | 25 | 23 | 20 | 15 | 17 |
| Disability benefits | |||||
| No | 5 | 19 | 21 | 30 | 24 |
| Yes | 30 | 22 | 20 | 11 | 17 |
Table A2.
Sociodemographic variables and paid sick leave in the propensity‐adjusted model
| Covariate | Before adjustment | After adjustment |
|---|---|---|
| Age | <.0001 | 0.7730 |
| Race | 0.8527 | 0.8209 |
| Education | 0.0002 | 0.9790 |
| Gender | 0.3302 | 0.7861 |
| Marital status | 0.4004 | 0.6806 |
| Income | <.0001 | 0.9124 |
| Geographic site | 0.0319 | 0.9971 |
| SES | 0.0145 | 0.9010 |
| Comorbid conditions | 0.1300 | 0.8609 |
| Job category | <.0001 | 0.8929 |
Precis: Among patients who experienced a serious cancer diagnosis, access to specific health‐related employment benefits was associated with higher likelihood of job retention. Employers and governmental agencies should consider the value in expanding access to such benefits.
Notes
Bivariate distribution (row percentages) of model covariates and propensity quintiles.
Differences in the individual covariates between those with paid sick leave and those without paid sick leave after adjusting for propensity score quintiles.
References
- 1. Sommers, B. D. , Gunja M. Z., Finegold K., and Musco T.. 2015. Changes in self‐reported insurance coverage, access to care, and health under the affordable care act. JAMA 314:366–374. [DOI] [PubMed] [Google Scholar]
- 2. Langa, K. M. , Fendrick A. M., Chernew M. E., Kabeto M. U., Paisley K. L., and Hayman J. A.. 2004. Out‐of‐pocket health‐care expenditures among older Americans with cancer. Value Health 7:186–194. [DOI] [PubMed] [Google Scholar]
- 3. Regenbogen, S. E. , Veenstra C. M., Hawley S. T., Banerjee M., Ward K. C., Kato I., et al. 2014. The personal financial burden of complications after colorectal cancer surgery. Cancer 120:3074–3081. [DOI] [PubMed] [Google Scholar]
- 4. Banegas, M. P. , Guy G. P. Jr, de Moor J. S., Ekwueme D. U., Virgo K. S., Kent E. E., et al. 2016. For working‐age cancer survivors, medical debt and bankruptcy create financial hardships. Health Aff. 35:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ramsey, S. , Blough D., Kirchhoff A., Kreizenbeck K., Fedorenko C., Snell K., et al. 2013. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. 32:1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Veenstra, C. M. , Regenbogen S. E., Hawley S. T., Abrahamse P., Banerjee M., and Morris A. M.. 2015. Association of paid sick leave with job retention and financial burden among working patients with colorectal cancer. JAMA 314:2688–2690. [DOI] [PubMed] [Google Scholar]
- 7. Waldfogel, J. , Higuchi Y., and Abe M.. 1999. Family leave policies and women's retention after childbirth: evidence from the United States, Britain, and Japan. J. Popul. Econ. 12:523–545. [Google Scholar]
- 8. United States Department of Labor . Family and Medical Leave in 2012: Technical Report. Available at https://www.dol.gov/asp/evaluation/fmla/FMLA-2012-Technical-Report.pdf (accessed 3 May 2017.)
- 9. National Partnership for Women & Families . Paid sick days: Attitudes and experiences. Available at http://www.nationalpartnership.org/research-library/work-family/psd/paid-sick-days-attitudes-and-experiences-presentation.pdf (accessed 3 May 2017).
- 10. Bradley, C. J. , Neumark D., and Barkowski S.. 2013. Does employer‐provided health insurance constrain labor supply adjustments to health shocks? New evidence on women diagnosed with breast cancer. J. Health Econ. 32:833–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Garcia‐Gomez, P. , van Kippersluis H., O'Donnell O., and van Doorslaer E.. 2013. Long term and spillover effects of health shocks on employment and income. J. Hum. Resour. 48:873–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bradley, C. J. , Neumark D., Motika M. I., and National Bureau of Economic Research . 2011. The effects of health shocks on employment and health insurance the role of employer‐provided health insurance. National Bureau of Economic Research, Cambridge, MA: Available at http://www.nber.org/papers/w17223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ihbe‐Heffinger, A. , Ehlken B., Bernard R., Berger K., Peschel C., Eichler H. G., et al. 2004. The impact of delayed chemotherapy‐induced nausea and vomiting on patients, health resource utilization and costs in German cancer centers. Ann. Oncol. 15:526–536. [DOI] [PubMed] [Google Scholar]
- 14. Siegel, R. L. , Miller K. D., Fedewa S. A., Ahnen D. J., Meester R. G., Barzi A., et al. 2017. Colorectal cancer statistics, 2017. CA Cancer J. Clin. 67:177–193. [DOI] [PubMed] [Google Scholar]
- 15. Bailey, C. E. , Hu C. Y., You Y. N., Bednarski B. K., Rodriguez‐Bigas M. A., Skibber J. M., et al. 2015. Increasing disparities in the age‐related incidences of colon and rectal cancers in the United States, 1975–2010. JAMA Surg. 150:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yabroff, K. R. , Dowling E. C., Guy G. P. Jr, Banegas M. P., Davidoff A., Han X., et al. 2016. Financial hardship associated with cancer in the United States: findings from a population‐based sample of adult cancer survivors. J. Clin. Oncol. 34:259–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Veenstra, C. M. , Regenbogen S. E., Hawley S. T., Griggs J. J., Banerjee M., Kato I., et al. 2014. A composite measure of personal financial burden among patients with stage III colorectal cancer. Med. Care 52:957–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dillman, D. A. , Smyth J. D., Christian L. M., and Dillman D. A.. 2009. Internet, mail, and mixed‐mode surveys: the tailored design method, 3rd ed. Wiley & Sons, Hoboken, NJ. [Google Scholar]
- 19. Chatterji, P. , Brandon P., and Markowitz S.. 2016. Job mobility among parents of children with chronic health conditions: early effects of the 2010 Affordable Care Act. J. Health Econ. 48:26–43. [DOI] [PubMed] [Google Scholar]
- 20. D'Agostino, R. B. Jr . 1998. Propensity score methods for bias reduction in the comparison of a treatment to a non‐randomized control group. Stat. Med. 17:2265–2281. [DOI] [PubMed] [Google Scholar]
- 21. Pryor, F . 2017. Occupational choices of the elderly. Monthly Labor Review, U.S. Bureau of Labor Statistics. Available at https://doi.org/10.21916/mlr.2017.4 (accessed 2 November 2017).
- 22. United States Department of Labor Bureau of Labor Statistics . Employee benefits survey 2016. Available at https://www.bls.gov/ncs/ebs/benefits/2016/ownership/civilian/table32a.htm (accessed 3 May 2017).
- 23. National Partnership for Women & Families . Paid sick days–State, District and County Statutes. Available at http://www.nationalpartnership.org/research-library/work-family/psd/paid-sick-days-statutes.pdf (accessed 3 May 2017).
- 24. United States Department of Labor Wage and Hour Division (WHD) . Final rule: Executive Order 13706, establishing paid sick leave for federal contractors. Available at https://www.dol.gov/whd/govcontracts/eo13706/ (accessed 3 May 2017).
- 25. Houser, L. , and Vartanian T. P.. 2012. Pay matters: the positive economic impacts of paid family leave for families, businesses and the public. Rutgers Center for Women and Work, New Brunswick, NJ. [Google Scholar]
- 26. Catalano, P. J. , Ayanian J. Z., Weeks J. C., Kahn K. L., Landrum M. B., Zaslavsky A. M., et al. 2013. Representativeness of participants in the cancer care outcomes research and surveillance consortium relative to the surveillance, epidemiology, and end results program. Med. Care 51:e9–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Blinder, V. , Patil S., Eberle C., Griggs J., and Maly R. C.. 2013. Early predictors of not returning to work in low‐income breast cancer survivors: a 5‐year longitudinal study. Breast Cancer Res. Treat. 140:407–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blinder, V. S. , Patil S., Thind A., Diamant A., Hudis C. A., Basch E., et al. 2012. Return to work in low‐income Latina and non‐Latina white breast cancer survivors: a 3‐year longitudinal study. Cancer 118:1664–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Short, P. F. , Vasey J. J., and Tunceli K.. 2005. Employment pathways in a large cohort of adult cancer survivors. Cancer 103:1292–1301. [DOI] [PubMed] [Google Scholar]


