Abstract
Fatty infiltration is an important prognostic factor for cuff healing after rotator cuff repair. Treatment options for stage 2–3 Goutallier rotator cuff tears vary widely and there is lack of decent comparative studies.
Purposes
The objective of this study was 1) to give an overview of the treatment options of stage 2–3 Goutallier rotator cuff tears and their clinical outcome and 2) to give a recommendation of the optimal treatment within this specific subgroup.
Methods
We searched the databases of Medline, Embase, Cochrane library, NHS Centre for Reviews and Dissemination, PEDro from inception to December 12th, 2016. Two authors, F.H. and N.W., selected the studies after consensus. Data was extracted by one author (F.H.) and checked for completeness by a second author (N.W.). Our primary outcome was physical function, measured by shoulder-specific patient reported outcomes. Secondary outcomes were cuff integrity after rotator cuff repair, shoulder pain, general health, quality of life, activity level and adverse events.
Results
For the first research question 28 prospective as well as retrospective studies were included. For the clinical outcome of these treatments three randomized controlled trials were included.
Conclusions
Despite the high reported retear rate, rotator cuff repair has comparable results (clinical improvement) as partial repair and isolated bicepstenotomy or tenodesis. These findings suggest that the additional effect of rotator cuff repair compared to the less extensive treatment options like isolated bicepstenotomy or tenodesis should be studied, as these might form a good alternative treatment based on this systematic review.
Level of evidence
Level IV; systematic review.
Keywords: Rotator cuff tear, Fatty infiltration, Rotator cuff repair, Bicepstenotomy, Bicepstenodesis, Arthroplasty, Partial repair, Debridement
1. Background
Rotator cuff tearing is a highly prevalent disorder of the shoulder joint of which its incidence increases with age. These lesions do not always result in a symptomatic shoulder joint. Under the age of 40 years, 4% of all cuff injuries remain asymptomatic, which increases up to 54% for patients aged 60 years or older.1 Amongst elderly, tendon quality is often poor as tears are mostly degenerative by nature. Important qualitative factors to specify the amount of degeneration are the level of fatty infiltration and atrophy of the involved muscle, and retraction of the tendon. These factors are considered important for selecting appropriate candidates for rotator cuff repair.
In the literature several independent factors to define an irreparable rotator cuff tear are described such as ≥50% of fatty infiltration (Goutallier stage ≥ 3),2 retraction of the tendon to the height of the glenoid3 and acromio-humeral interval being less than 7 mm4, 5, 6
Amongst several identified negative prognostic factors for healing, fatty infiltration (FI) is frequently described as paramount predictor for healing, which implies anatomic integrity on the footprint after full recovery from surgery. The extend of FI in the rotator cuff was firstly classified by Goutallier et al2 Several clinical studies on rotator cuff repair described the functional and radiologic outcome for the subgroups of this classification separately.2, 7, 8, 9, 10, 11, 12, 13, 14 In general, for stages 0–1 (0–25% FI) the clinical outcome is described good to excellent, while stage 4 (>50% FI) is associated with poor outcomes, high retear rates and minor functional improvement.8 Consensus has been reached that cuff repair of these severe fatty infiltrated tendons should not be performed. The appropriate treatment for the remaining stage 2 and 3 fatty infiltrated cuff tears (25–50% FI) is still under discussion. Despite a high retear rate after rotator cuff repair in this patient category, patients clinically improve significantly with only minor functional differences between patients with healed repairs and patients with a retear.10, 11, 12 It is still poorly understood which element is responsible for this improvement.
Alternative treatments for restoring shoulder function after a full-thickness rotator cuff tear beside cuff repair are conservative treatment, debridement, bicepstenotomy, bicepstenodesis, subacromial decompression, tendon transfers, arthroplasty, and other new developments in the tissue engineering industry.
1.1. Objectives
The aim of this study was to perform a systematic literature review to 1) outline the treatment options for stage 2–3 Goutallier fatty degenerated rotator cuff tears and their outcome and 2) to give a recommendation of the optimal treatment within this specific subgroup. Our hypothesis is that stage 2–3 Goutallier fatty degenerated rotator cuff tears can be treated with less extensive treatment options like conservative therapy and isolated bicepstenotomy achieving comparable functional results as compared with extensive treatment options like rotator cuff repair or tendon transfers.
2. Methods
This systematic review is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.15
2.1. Eligibility criteria
A literature search for studies describing the functional outcome for treated grade 2–3 Goutallier rotator cuff tears was conducted. Included treatments were: conservative treatment, open and arthroscopic rotator cuff repair, bicepstenotomy, bicepstenodesis, acromioplasty, debridement, partial repair, latissimus dorsi transfer, other tendon transfers, arthroplasty and tissue engineering or other new developments. Prospective as well as retrospective studies were included.
2.2. Search strategy
A systematic search of Embase, PubMed, Web of Knowledge, and the Cochrane Library was performed from 1995 to June 2014. The search terms included Medical Subject Headings terms, free-text word variations, and combinations of these. Cross-references and “cited-by” articles of the included articles were screened to ensure that no relevant studies were missed. An expert in this field was consulted to check for missing relevant studies. The Netherlands Journal of Orthopaedics, which is not available via the above-mentioned bibliographic databases, was searched for relevant Dutch articles. National and international trial registries were checked for ongoing or unpublished trials. This search was performed in June 2014 and updated in January 2015 and December 2016 (APPENDIX A).
2.3. Study selection
After removing duplicates, titles and abstracts were screened according to the following criteria: (1) the publication was a clinical study, (2) the study population consisted of adult patients with a MRI or CT-scan confirmed rotator cuff tear, and (3) the publication contained information on the functional outcome; radiological information on the quality of the rotator cuff tendons and postoperative integrity was not prerequisite. Based on the titles and abstracts, manuscripts identified as potentially eligible underwent a full-text review. Papers were included in the review based on the following criteria: (1) the study included stage 2–3 Goutallier fatty infiltration rotator cuff tears, described pre- or postoperatively; (2) in case of a cuff repair an arthroscopic, mini open or open surgical technique was used; (3) studies with mixed surgical techniques were included if data on the patients were separately available; (4) the article was written in English, Dutch, French or German; and (5) the full text of the paper could be obtained. For outlining the treatment options and their outcome, no selection was made in study designs. For the second objective, to give a recommendation of the optimal treatment within this specific subgroup, only randomized studies were selected.
2.4. Data items
From the included full-text papers, the following study characteristics were systematically extracted, applying the evidence table for intervention studies: bibliographic reference, study type, number of patients, multi- or single-centre study, patient characteristics (including age and gender), tear characteristics (including retear rate and level of fatty infiltration), type of intervention, diagnostic tool(s) (pre- and postoperative), the comparison, the length of follow-up, outcome measures and effect size (scores on function and cuff integrity) and source of funding.16 A data-extraction sheet was developed a priori. One author (F.H.) extracted the data and a second author (N.W.) verified the extracted data and added data when necessary.
2.5. Assessment of risk of bias and methodological quality
Methodological quality assessment of selected papers was performed using the “methodology checklist for randomized controlled trials (RCT’s), cohort studies and prognostic studies.”16 The RCT and cohort study checklist consisted of 4 main items: selection bias, performance bias, attrition bias and detection bias. Based on the score of their respective subitems, the main items were scored as low, unclear and high risk of bias. For each main item, a low risk indicated that the study was designed and conducted in a manner that minimized the risk of bias for that item. An unclear risk was given when the information required to score an item was not reported or was not reported clearly. A priori it was decided that studies would be excluded if more than 2 out of 4 main items scored a high risk of bias (low methodological quality).
The checklist for prognostic studies consisted of 6 main items: study sampling, loss to follow-up, prognostic factors, outcome, confounders, and statistical analysis. Based on the score of their respective subitems, the main items were scored as yes, unclear or no. For each main item, a yes response indicated that the study was designed and conducted in a manner that minimized the risk of bias for that item. An unclear response was given when the information required to score an item was not reported or was not reported clearly. A priori it was decided that studies with less than 3 yes responses on the 6 main items would be excluded from this review (low methodological quality). Screening of titles, abstracts, and full text, as well as the assessment of the methodological quality of the studies, was independently performed by 2 of the authors (F.H. and N.W.). Disagreements between reviewers were resolved by consensus. For the methodology assessment, consensus had to be reached on each subitem and main item of the methodology checklist.
2.6. Assessment of risk of bias across studies
In the retrieved studies, particular attention was paid to a clear description of the patient population, the in- and exclusion criteria and incomplete outcome data, concerning different risks of bias.
3. Results
3.1. Study selection
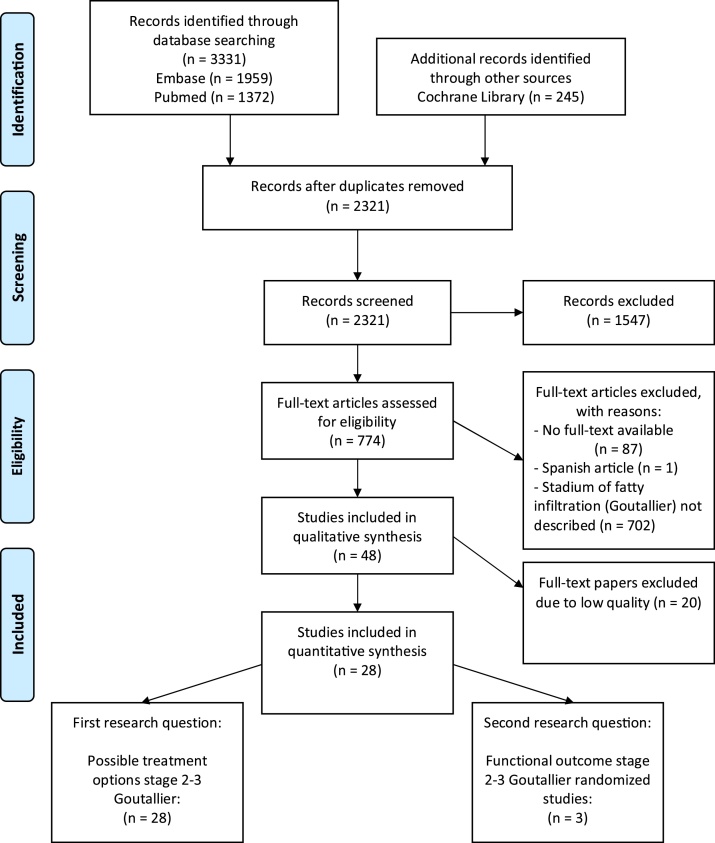
The literature search yielded a total of 3576 studies. After removing duplicates, 2321 articles remained. Titles and abstracts of the remaining 2321 studies were screened. 1547 records were discarded because they did not meet the criteria for inclusion. Full-text screening was then performed for the remaining 774 studies. 48 papers were assessed for their quality and risk of bias (Tables 1A–1C). Based on the risk of bias assessment another 20 papers were excluded. An overview of the screening process is given in Fig. 1. No unpublished relevant studies were obtained from trial registries. For the first question on possible treatment options randomized and non-randomized studies were included (n = 28) (Table 2).4, 9, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 For the first research question on functional outcome only randomized studies, describing the functional results of each stage of fatty infiltration separately (n = 3), were included (Table 3).21, 26, 27
Table 1A.
prognostic studies: Quality assessment of the included studies according to the ‘Methodology checklist for prognostic studies.’ All items were scored with a ‘yes’, ‘no’, or ‘unclear’. A ‘yes’ response indicates that the study has been designed and conducted in such a way as to minimize the risk of bias for that item. An ‘unclear’ response was given when the answer to an item is not reported or is not reported clearly.
| Study | Population | Drop-out | Prognostic factor | Outcome | Confounders | Statistical analysis | Inclusion? |
|---|---|---|---|---|---|---|---|
| Iannotti et al22 | yes | yes | yes | yes | yes | no | Yes |
| Toussaint, 201162 | yes | no | unclear | yes | unclear | no | Yes |
| Kim et al11, 23 | yes | yes | yes | yes | yes | yes | Yes |
| Cho and Rhee9 | yes | no | yes | yes | unclear | no | Yes |
| Edwards, 200246 | yes | unclear | unclear | unclear | yes | unclear | No |
| Koh, 201454 | yes | no | unclear | yes | unclear | unclear | No |
| Chung et al10, 19, 38 | yes | no | yes | yes | unclear | unclear | Yes |
| Choi et al18 | yes | no | yes | yes | unclear | unclear | Yes |
| Wiater et al36 | yes | unclear | yes | yes | unclear | unclear | Yes |
| Lapner et al24 | yes | unclear | yes | yes | yes | unclear | Yes |
| Vastamaki, 201363 | unclear | unclear | unclear | yes | unclear | no | No |
| Fuchs et al20 | yes | yes | yes | yes | no | yes | Yes |
| Goutallier, 200349 | unclear | unclear | unclear | yes | unclear | no | No |
| Mellado et al25 | yes | unclear | yes | yes | unclear | no | Yes |
| Goutallier, 200950 | yes | unclear | unclear | unclear | unclear | no | No |
| Zumstein et al37 | unclear | yes | yes | yes | unclear | yes | Yes |
| Nich et al30 | yes | unclear | yes | yes | unclear | no | Yes |
| Park et al39 | yes | unclear | yes | yes | yes | yes | Yes |
| Chung et al10, 19, 38 | yes | unclear | unclear | yes | yes | yes | Yes |
| Kim, 201655 | unclear | unclear | unclear | unclear | unclear | unclear | No |
Table 1B.
The cohort studies checklist consisted of 4 main items: selection bias, performance bias, attrition bias and detection bias. Based on the score of their respective subitems, the main items were scored as low, unclear and high risk of bias. For each main item, a low response indicated that the study was designed and conducted in a manner that minimized the risk of bias for that item. An unclear response was given when the information required to score an item was not reported or was not reported clearly. A priori, was decided that studies were excluded if more than 2 out of 4 main items would be scored as high risk of bias on the basis of low methodological quality.
| Study | Selection bias | Performance bias | Attrition bias | Detection bias | Inclusion? |
|---|---|---|---|---|---|
| Park et al32 | low | unclear | low | low | Yes |
| Franceschi, 201547 | unclear | unclear | unclear | unclear | No |
| Oh et al31 | low | unclear | low | unclear | Yes |
| Cho et al17 | unclear | unclear | low | low | Yes |
| Warner et al35 | unclear | unclear | low | low | Yes |
| Ryu, 201560 | low | unclear | low | high | Yes |
| Taniguchi, 201561 | unclear | unclear | low | unclear | No |
| Hug, 201553 | unclear | unclear | unclear | low | No |
| Namdari, 201457 | high | unclear | unclear | low | No |
| Moraiti, 201429 | unclear | unclear | low | low | Yes |
| Warner and Parsons35 | high | high | unclear | unclear | No |
| Boileau et al4 | low | unclear | low | unclear | Yes |
| Lee, 201656 | high | high | high | unclear | No |
| Gasbarro, 201648 | unclear | unclear | unclear | unclear | No |
| Shin et al40 | unclear | unclear | high | unclear | No |
| Paribelli, 201559 | high | high | low | unclear | No |
| Franceschi, 201547 | high | high | unclear | unclear | No |
Table 1C.
The randomized controlled trial checklist consisted of 4 main items: selection bias, performance bias, attrition bias and detection bias. Based on the score of their respective subitems, the main items were scored as low, unclear and high risk of bias. For each main item, a low response indicated that the study was designed and conducted in a manner that minimized the risk of bias for that item. An unclear response was given when the information required to score an item was not reported or was not reported clearly. A priori, was decided that studies were excluded if more than 2 out of 4 main items would be scored as high risk of bias on the basis of low methodological quality.
| Study | Selection bias | Performance bias | Attrition bias | Detection bias | Inclusion? |
|---|---|---|---|---|---|
| Milano et al27 | low | low | low | low | Yes |
| Van der Zwaal et al34 | low | unclear | low | unclear | Yes |
| Gumina, 201251 | unclear | unclear | low | unclear | No |
| Gumina, 201252 | high | unclear | low | unclear | No |
| Milano, 201328 | low | low | low | low | Yes |
| Berth et al44 | high | high | high | high | No |
| Grasso et al21 | low | unclear | low | low | Yes |
| Milano et al28 | low | unclear | low | low | Yes |
| Nicholas, 201658 | unclear | low | unclear | unclear | No |
| Bryant et al42 | low | low | low | low | Yes |
| Kukkonen et al41 | low | unclear | low | low | Yes |
Fig. 1.
Flow diagram of literature search.
Table 2.
Results (possible treatment options, randomized and non-randomized studies).
| Study | Study design | Treatment | Comparison | Sample size | Age at surgery | Length of follow-up (months) | Functional outcome (mean CMS and DASH score) | Retear rate | Average degree of FI | % stage 2–3 Goutallier |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 3 | ||||||||||
| Boileau et al4 | Cohort | Bicepstenotomy/ Bicepstenodesis | Tenotomy vs. Tenodesis | 72 | Tenotomy: 73.1 ± 6.2 | 35 ± 7 | CMS: | / | ISP 2.33 | 29 | 22 |
| Tenodesis: 69.8 ± 6.4 | Overall: 66.5 ± 16.3 | ||||||||||
| Bryant et al42 | RCT | Cuff repair | Repair alone vs. repair and augmentationporcine small intestine submucosa (SIS) | 62 | 56.6 ± 10.8 | 24 | CMS: | 60% | SSP: 1.5 | 61 | 3 |
| SIS: 79.3 ± 3.5 | |||||||||||
| No SIS: 87.5 ± 3.7 | |||||||||||
| Cho and Rhee9 | Prognostic | Cuff repair | Intact vs. Retear | 169 | Intact | 39 (24–83) | / | 22.5% | / | 10 | 8 |
| 53.2 (38–67) | |||||||||||
| Retear | |||||||||||
| 58.4 (45–74) | |||||||||||
| Cho et al17 | Cohort | Cuff repair | Single vs. double row | 64 | 7.5 (3–29) | CMS: | 39% | / | 7 | 63 | |
| Single: 58.1 ± 6.07 | Single: 77.4 | ||||||||||
| Double: 57.6 ± 10.39 | Double: 76.2 | ||||||||||
| Choi et al18 | Prognostic | Cuff repair | / | 147 | 62.8 (46–79) | 23.4 (12–48) | CMS: 84.3 (11–100) | 17.0% | SSP: | 46 | 27 |
| 2.22 | |||||||||||
| Chung et al10, 19, 38 | Prognostic | Cuff repair | / | 288 | 59.53 ± 8.41 | 13.5 ± 2.7 | / | 22.9% | SSP: | / | / |
| 2.35 ± 1.05 | |||||||||||
| Chung et al19 | Prognostic | Cuff repair | Intact vs. retear | 108 | 63.7 ± 6.4 | 31.7 ± 15.8 | CMS: | 39.8% | SSP: 3.13 | / | / |
| Intact: 77.1 ± 32.9 | Intact: 2.84 | ||||||||||
| Retear: 67.2 ± 27.2 (NS) | Retear: 3.55 | ||||||||||
| Fuchs et al20 | Prognostic | Cuff repair (open) | / | 32 | 59.0 (40–75) | 38 (24–53) | CMS: 78.1 | 13% | SSP: | / | / |
| Intact: 0.8 | |||||||||||
| Retear: 1.0 | |||||||||||
| Grasso et al21 | RCT | Cuff repair | Single vs. double row | 72 | Single: 58.3 ± 10.3 | 24.8 ± 1.4 | SeeTable 3 | / | / | 39 | 24 |
| Double: 55.2 ± 6.5 | |||||||||||
| Iannotti et al22 | Prognostic | Cuff repair | Intact vs. Retear | 113 | Intact: 58.6 ± 9.4 | 12 | / | 17% | Intact: 2.13± 0.65 | 9 | 0 |
| Retear: 59.1 ± 9.09 | Retear: 2.39 ± 0.76 | ||||||||||
| Kim et al23 | Prognostic | Cuff repair | Intact vs. Retear | 66 | 61.2 (50–75) | 23.5 (15–38) | CMS: | 42.4% | SSP: | / | / |
| Intact: 78.5 | Intact: 1.74 ± 0.92 | ||||||||||
| Retear: 70.6 | Retear 2.54 ± 0.84 | ||||||||||
| Kukkonen et al41 | RCT | Cuff repair/conservative/acromioplasty | 180 | 24 | CMS improvement: | 31% cuff repair group | / | ||||
| 1. Conservative | Conservative: 64 ± 5.6 | 1. 18.4 (14.2–22.6) | 1. 32 (53%) | 1. 1 (2%) | |||||||
| 2. Acromioplasty | Acromioplasty: 65 ± 5.1 | 2. 20.5 (16.4–24.6) | 2. 29 (48%) | 2. 5 (8%) | |||||||
| 3. Cuff repair | Cuff repair 65 ± 5.8 | 3. 22.6 (18.4–26.8) (p = 0.38) | 3. 30 (53%) | 3. 2 (4%) | |||||||
| Lapner et al24 | Prognostic | Anatomic total shoulder | / | 62 | 67 (34–90) | 12 | / | / | SSP 1.41 | 34 | 3 |
| Mellado et al25 | Prognostic | Partial and complete cuff repair (open) | / | 6 vs. 22 | 59.8 ± 6.8 | 44.4 (13–96) | / | 68% | SSP: 1.52 ± 0.8 | / | / |
| Milano et al26 | RCT | Cuff repair | Bio vs. metal anchors | 110 | Bio: 62.8 ± 7.9 | 24.4 ± 2.6 | SeeTable 3 | / | / | 34 | 29 |
| Metal: 60.4 ± 8.6 | |||||||||||
| Milano et al27 | RCT | Cuff repair | +/− subacromial decompression | 80 | 61 ± 7.0 | 24 | SeeTable 3 | / | / | 38 | 25 |
| 59.7 ± 9.7 | |||||||||||
| Milano et al28 | RCT | Cuff repair | +/− Microfracture | 80 | 28.1 ± 3 | CMS: | / | SSP: 1.97 | 34 | 25 | |
| Microfracture 63.1 ± 9.2 | Microfracture: 92.7 ± 16.7 | ||||||||||
| Standard repair 60.6 ± 10.1 | Standard repair: 94.5 ± 14 | ||||||||||
| DASH: Microfracture: 28.6 ± 21.3 | |||||||||||
| Standard repair: 23.3 ± 20.1 | |||||||||||
| Moraiti et al29 | Cohort | Cuff repair | Over 70 vs. under 50 years old | 80 | / | CMS: | / | SSP: | 30 | 11 | |
| >70 yrs 13.8 | >70 yrs 74.6_12.02 | >70 yrs 1.90 | |||||||||
| <50 yrs 12.9 | <50 yrs 77.18_11.02 | <50 yrs 0.81 | |||||||||
| Nich et al30 | Prognostic | Cuff repair (open) | / | 47 | 59 | 87 (60–133) | CMS: 73.7 | 12% | SSP: 0.81 | / | / |
| Oh et al31 | Cohort | Cuff repair | non-pseudoparalytic vs. pseudoparalytic | 58 | 30.5 ± 18.1 (12–72) | CMS: | Healing rate: | / | 7 | 31 | |
| Pseudo 64.6 ± 9.5 | Pseudo: 53.2 ± 18.5 | 33.3% in the pseudoparalytic | |||||||||
| Non-pseudo 65.3 ± 7.0 | Non-pseudo: 79.0 ± 56.0 | 47.4% in the non-pseudoparalytic group | |||||||||
| Park et al32 | Cohort | Cuff repair | Single vs. double row | 78 | 55.8 | 25.1 (22–30) | CMS: | / | SSP: | / | / |
| Single row: 76.68 ± 8.56 | Single row 1.70 ± 1.07 | ||||||||||
| Double row: 79.66 ± 4.52 | Double row 1.95 ± 1.33 | ||||||||||
| Park et al39 | Prognostic | Cuff repair | Intact vs. retear | 339 | 59.8 ± 7.9 | 20.8 (22–66) | CMS: Overall: 67.1 ± 12.2 (NS between groups) | 13.3% | SSP: 1.91 ± 0.82 | / | / |
| Ryu et al33 | Cohort | Cuff repair | Conventional vs. modified suture-bridge | 71 | CMS: | 15% | SSP: 0.34 | / | / | ||
| Conventional 57.0 ± 4.4 | Conventional 58 (44–77) | Conventional 73.4 ± 10.3 | |||||||||
| Modified 57.6 ± 4.6 | Modified 26 (15–35) | Modified 77.0 ± 9.8 | |||||||||
| Shin et al40 | Cohort | Cuff repair | Small vs. medium vs. large size tears | 164 | 55.2 ± 9 | 24 | CMS: No significant difference between groups | Exclusion criteria | 3 | 0 | |
| Van der Zwaal et al34 | RCT | Cuff repair | Arthroscopic (AA) vs. mini-open (MO) | 100 | 12 | CMS: | 13–17% | / | 16 | 0 | |
| AA 57.2 ± 8.0 | AA 66 (1.6) | ||||||||||
| MO 57.8 ± 7.9 | MO 62 (1.6) | ||||||||||
| DASH: | |||||||||||
| AA 65.6 (60.8–70.5) | |||||||||||
| MO 69.1 (64.3–73.9) | |||||||||||
| Warner and Parsons35 | Cohort | Latissimus dorsi transfer | Primary vs. revision | 6 vs. 16 | 25 (18–31) | CMS (age/gender adjusted): | 36% | SSP 3.09 | 27 | 36 | |
| Primary 62 (38–78) | Primary 69% (58–81) | ||||||||||
| Revision 56 (26–75) | Revision 52% (37–75) | ||||||||||
| Wiater et al36 | Prognostic | Reverse total shoulder | / | 30 | 71 ± 10 | 30 ± 7 | CMS: 67.27 ± 13.07 | / | SSP 3.1 |
7 | 20 |
| Zumstein et al37 | Prognostic | Cuff repair (open) | / | 27 | 53.7 | 9.9 years | CMS: | 57% | SSP: | / | / |
| Overall: 71 | Intact: 1.5 | ||||||||||
| Intact 81 | Retear: 1.5 | ||||||||||
| Retear: 64 | |||||||||||
Abbreviations: SSP: supraspinatus tendon; SSC: Subscapularis; ISP: infraspinatus; SIS: small intestine submucosa; yrs: years; +/− microfracturing: with or without microfracturing; +/− subacromial decompression: with or without subacromial decompression
*Tenosan: arginine L-alpha-ketoglutarate, methylsulfonylmethane, hydrolyzed type I collagen and bromelain.
Table 3.
Functional results stage 2–3 fatty infiltration.
| Sample size | Treatment | Age | Length of follow-up | Outcome parameter | Stage Goutallier fatty infiltration (n) |
||
|---|---|---|---|---|---|---|---|
| 2 | 3 | ||||||
| Milano et al26 | 101 | Bio vs. metal anchors | 61.6 ± 8.3 | 24.4 ± 2.6 | (n = 34) | (n = 29) | |
| Constanta | 104.4 ± 12.5 | 91.3 ± 25.3 | |||||
| DASH | 14.6 ± 14.1 | 28.9 ± 19.4 | |||||
| Grasso et al21 | 72 | Single vs. double row | 56.8 ± 8.7 | 24.8 ± 1.4 | (n = 28) | (n = 17) | |
| Constanta | 102.7 ± 24 | 106.4 ± 14.9 | |||||
| DASH | 14.5 ± 13.8 | 14.1 ± 13 | |||||
| Strength (lb) | 12.6 ± 6.6 | 12.8 ± 5.5 | |||||
| Milano et al27 | 71 | +/−subacromial decompression | Group 1 61 ± 7.0 Group 2 59.7 ± 9.7 | 24 | (n = 27) | (n = 18) | |
| Constanta | 103.6 ± 12.2 | 94.2 ± 21.2 | |||||
| DASH | 18.1 ± 15.5 | 23.6 ± 20.1 | |||||
age and gender adjusted Constant score.
3.2. Risk of bias assessment
Tables 1A–1C show the results of the assessed risk of bias of the individual trials.
3.2.1. Results on treatment options for stage 2–3 Goutallier cuff tears
There are several options for treating Goutallier stage 2–3 rotator cuff tears. After a critical selection of literature, articles on arthroscopic cuff repair, partial cuff repair, debridement, bicepstenotomy, bicepstenodesis, lattisimus dorsi transfer, arthroplasty and conservative treatment, were included. Literature on other therapeutical options like, ligament augmentation and other tendon transfers were not included because they did not meet the inclusion criteria or were not included due to poor study quality.
3.2.1.1. Rotator cuff repair
Twenty-three out of twenty-seven included articles described a rotator cuff repair of which 12 were prognostic studies, 5 cohort studies and 6 RCT’s. Four prognostic studies were on open rotator cuff repair.20, 25, 30, 37 There were three prognostic studies that focused on cuff integrity related to the stage of fatty infiltration.9, 22, 23 Iannotti et al22 found more retears amongst patients with stage 2 Goutallier (50%) compared to stage 0 and 1 Goutallier (16%, 11%) with comparable functional outcomes.22 The two other studies, Kim et al23 and Cho and Rhee,9 reported higher retear rates with Kim et al23 reporting 100% failure of Goutallier stage 3 and Cho and Rhee9 62% failure of Goutallier stage 3 and 47% failure rate amongst stage 2, with excellent relief of pain and functional improvement to perform the activities of daily living, despite the structural failures. Within these two studies 44%–56% of the patients underwent additional treatment of the biceps tendon (tenotomy or tenodesis).9, 23 Performing a meta-analysis was not possible due to heterogeneous data. Average fatty infiltration ranged from 0.34 to 3.24 with a mean absolute Constant score ranging from 66.1 to 93.3 and a retear rate from 12% to 86% without any linearly relation observed (see Table 2).
3.2.1.2. Partial repair
One retrospectively designed study was included comparing partial with complete rotator cuff repair, open approach. Mellado et al25 performed a partial repair in 6 out of 22 patients with massive rotator cuff tears. Results were comparable for the partial and complete repair group with a retear rate amongst the complete repair group of 68% after a mean follow-up of 44.4 months (range: 13–96).25 The University of California at Los Angeles (UCLA) score improved from an average of 12.5 ± 2.8 point for the total study population to 29.7 ± 5.3 and 31.8 ± 3.6 (p < 0.0001) point at final follow-up for respectively complete and partial rotator cuff repair.25
3.2.1.3. Isolated bicepstenotomy or tenodesis
Boileau et al4 studied the outcome of isolated bicepstenotomy (n = 39) versus tenodesis (n = 33) for the treatment of irreparable massive rotator cuff tears without the presence of true pseudoparalysis. The reparability was determined by preoperative computed tomographic arthrography and direct arthroscopic evaluation. Functional results showed no significant differences between groups. For both groups the mean Constant score improved from 46.3 ± 11.9 points preoperatively to 66.5 ± 16.3 points postoperatively (P < 0.001). From the 72 patients treated with either tenotomy or tenodesis of the biceps tendon, stage 2–3 Goutallier FI of the infraspinatus tendon was described in 51% (n = 37) (stage 2: 29% (n = 21); stage 3: 22% (n = 16)) and FI of the subscapularis tendon in 40% (n = 29) (stage 2: 32% (n = 23); stage 3: 8% (n = 6)). The extend of FI for the supraspinatus tendon was not specified. Functional results for these subgroups were not available.4
3.2.1.4. Lattisimus dorsi transfer
Scrutinizing the stages of FI of interest in the study by Warner et al,35 functional outcome decreases with the severity of FI. For the 6 patients with stage 2 FI, the mean Constant score was 69% (range 48%–75%). In contrast, the 8 patients with stage 3 FI achieved a mean Constant score of 52% (range 38%–68%). Differences in functional outcome between stage 2 and stage 3 FI were statistically significant (P < 0.05).35
3.2.1.5. Arthroplasty (reverse and anatomic total shoulder replacement)
One article, by Wiater et al,36 regarded reversed total shoulder arthroplasty. They studied the association between deltoid and rotator cuff muscle FI and clinical outcome. Quantitative fatty infiltration of the infraspinatus (30.47% ± 15.01% (range: 0–100%)) was correlated with decreased postoperative external rotation (P = 0.037). Correlation with increased level of supraspinatus fatty infiltration, which was found to have the highest degree of fatty infiltration, and functional impairment was not found.36
For anatomic total shoulder arthroplasty the condition of the supraspinatus tendon is paramount. Lapner et al24 described a negative association between a preoperatively greater supraspinatus percent of FI with preoperative shoulder strength (P = 0.001) and Constant score (P = 0.001). The postoperative infraspinatus percent of FI was negatively associated with postoperative strength (P = 0.021) and Constant score (P = 0.04). Multivariable regression analysis of possible predictive factors demonstrated that preoperative supraspinatus percent muscle area (P = 0.016) was associated with better follow-up Constant score, and preoperative supraspinatus strength was associated with postoperative strength (P = 0.002). Higher degrees of preoperative percent of FI were not associated with worse patient-reported outcomes postoperatively.24 From the total study population stage 2–3 Goutallier FI of supraspinatus tendon was represented in 35% (stage 2: 32% (n = 21); stage 3: 3% (n = 2)). Results were not specified for each stage of FI separately.
3.2.1.6. Conservative treatment
Kukkonen et al performed a methodological high quality randomized controlled trial in which they compared three type of treatments (physiotherapy-only, acromioplasty and physiotherapy, rotator cuff repair combined with acromioplasty and physiotherapy). Population characteristics were, mean age 65 years (55–81) with a full-thickness supraspinatus tear on MRI with the absence of pseudoparalysis and 51% stage 2 and 5% stage 3 Goutallier FI. There were no significant differences in baseline and in outcome (VAS pain, Constant score, range of motion) up to 2 years after surgery. They did not specify outcome for stage of FI separately.
Table 2 presents the characteristics and reported outcomes of the included studies.
3.2.2. Results on functional outcome related to fatty infiltration
3.2.2.1. Characteristics of included studies
Table 3 presents the outcomes of the included studies. Only randomized studies are presented to answer the second research question of which only three described the functional outcome for each stage of fatty infiltration separately (Milano et al, Grasso et al, Milano et al).21, 26, 27
3.2.2.2. Results of included studies
The included randomized studies all reported shoulder-specific physical function.21, 26, 27 They all used the age and gender adjusted Constant score and DASH score. Table 3 presents the functional outcome for stage 2 and 3 of fatty infiltration separately. Milano et al26 compared the clinical outcome of arthroscopic cuff repair with metal and biodegradable suture anchors. Functional outcome (DASH and Constant score) was significantly influenced by the level of FI after a mean follow-up of 24.4 ± 2.6 months. Functional outcome was significantly better for stage 2 FI of the supraspinatus tendon compared to stage 3 FI.26 Grasso et al21 compared the clinical outcome of arthroscopic rotator cuff repair with single-row and double-row techniques in which no significant difference was found between the stage of FI and clinical results.21 Milano et al27 compared the clinical outcome of arthroscopic cuff repair with and without subacromial decompression. Functional outcome and quality of life after 2 years was significantly influenced by the level of FI. The subitem Work-DASH score was significantly better for stage 2 FI of the supraspinatus tendon compared to stage 3 FI. The general DASH and Constant score were not significantly influenced by the level of FI.
4. Discussion
The aim of this study was to perform a systematic literature review to outline the treatment options for stage 2–3 Goutallier fatty degenerated rotator cuff tears and their outcome and to give a recommendation of the optimal treatment within this specific subgroup. Currently, the appropriate treatment for stage 2 and 3 fatty infiltrated cuff tears (25–50% FI) is still under discussion. To answer our first question on treatment options for Goutallier 2–3 rotator cuff tears we included 28 studies on arthroscopic cuff repair, partial cuff repair, bicepstenotomy or −tenodesis, lattisimus dorsi transfer, arthroplasty and conservative treatment.4, 9, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 For the first research question on functional outcome, describing the functional results of each stage of fatty infiltration separately, only randomized studies were included which implicated three studies on rotator cuff repair.21, 26, 27
Considering the first research question most studies consisted of mixed and heterogeneous data, which made it difficult to compare their clinical outcome. Additionally, most studies presented an average degree of fatty infiltration for their study population with a clinical outcome in terms of means, while we were also in search of the clinical outcome for each subgroup of fatty infiltration separately. There were three well designed RCT’s by Milano and Grasso et al21, 26, 27 describing these results. Milano et al26, 27 showed that functional outcome was significantly influenced by the level of fatty infiltration using a multivariate regression analysis. Grasso et al21 showed that functional outcome was not influenced by the level of fatty infiltration. Besides FI, age was the only other significant prognostic factor determining functional outcome.21, 26, 27 Unfortunately they did not report integrity of the repaired tendons at follow-up. Recurrent tearing is not uncommon amongst the degenerative rotator cuff tendons, which surprisingly not always results in deterioration of functional outcome. Interestingly, 46% underwent additional tenotomy or tenodesis of the long head of the biceps tendon, which did not result in a significant difference in functional outcome as compared with an untreated biceps tendon. Although this did not result in increased functional improvement, an isolated tenotomy or tenodesis is suggested to give comparable results from at least stage 2 FI as shown by Boileau et al4 The other included non-randomized studies did not show a linear correlation between the level of fatty infiltration and functional outcome neither with the retear rate. Additionally, the length of follow-up amongst all included studies was not associated with increased retear rate. Again, included studies were very heterogeneous which makes it difficult to draw conclusions based on these data. Recently, Jacquot et al43 compared acromioplasty and bicepstenotomy with or without arthroscopic rotator cuff repair amongst patients older than 60 years of age. They found arthroscopic rotator cuff repair functionally superior to only performing a subacromial decompression and additional bicepstenotomy with a mean follow-up of 4 years. However, they excluded stage 3 and 4 Goutallier FI and did not mention the average degree of FI for their study groups which is, based on previous literature, the most important prognostic factor. This suggested they included patients with relatively good quality of their rotator cuff tendons for which cuff repair is known to be superior as compared to subacromial decompression in combination with a bicepstenotomy.
Only one article was included describing the results of partial cuff repair. Mellado et al25 included 6 patients with massive rotator cuff tears and reported good results. The small sample size and retrospectively design makes it difficult to draw conclusions. In contrary, Berth et al,44 which was excluded due to methodological poor quality, prospectively included 42 patients and compared debridement with partial cuff repair. The study population had Goutallier stage 3 (n = 35) and 4 (n = 7) fatty infiltration. After a mean follow-up of 24 ± 2 months both groups had similar pain relief and level of satisfaction (DASH). Regardless of high rates of structural failure of the partial rotator cuff repair, the results of arthroscopic partial rotator cuff repair demonstrated only slightly better functional outcome than debridement.44 One should realize that performing a partial repair entails higher costs and longer period of patient recovery compared to only a debridement.
In case of subscapularis insufficiency latissimus dorsi transfer could be indicated. As shown in the included study by Wiater et al36 functional outcome is worse when the level of fatty infiltration increases. However, acceptable results are described even in case of increased fatty infiltration of the affected cuff.35 In case of posterosuperior cuff deficiency and low degree of fatty infiltration of the infraspinatus tendon, latissimus dorsi transfer could also be combined with reverse total shoulder arthroplasty.45
The role of conservative treatment in degenerative non-traumatic tears has not been studied widely. The included study by Kukkonen et al41 suggest that in the absence of functional disability preoperatively, physiotherapy alone could be a good alternative treatment as compared to rotator cuff repair and acromioplasty. Unfortunately they did not specify their outcome for the stages of FI separately, although more than 50% had Goutallier stage 2 FI41
Based on the results from this systematic performed review, in which we scrutinized treatment options and clinical outcome for stage 2–3 Goutallier fatty infiltrated rotator cuff tears, we could recommend for this specific subgroup conservative treatment, partial repair and isolated bicepstenotomy or −tenodesis as appropriate alternative for rotator cuff repair with comparable results. The conservative treatment and isolated bicepstonotomy or −tenodesis are less extensive and with comparable results might be cost-effective (shorter duration of surgery, faster recovery and less absenteeism). RCT’s are needed to observe the additional effect of rotator cuff repair compared to the less extensive treatment options like an isolated bicepstenotomy or tenodesis.
5. Conclusion
Our aim was to review the published literature optional treatments on stage 2–3 Goutallier fatty infiltrated rotator cuff tears describing the clinical results and to give a recommendation for optimal treatment within this subgroup. Despite the high reported retear rate, clinical improvement after rotator cuff repair is reported. Comparable results are reported after conservative treatment, partial repair and isolated bicepstenotomy or tenodesis. Amongst patients undergoing reverse total shoulder arthroplasty the level of supraspinatus fatty infiltration seems not to influence the outcome where in anatomic total shoulder arthroplasty it does. In conclusion, conservative treatment, partial repair, isolated bicepstenotomy and tenodesis seem good treatment options in patients with stage 2–3 Goutallier fatty infiltrated rotator cuff tears.
Disclaimer
None.
International review board approval
Not applicable (systematic review)
Conflict of interest statement
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Acknowledgements
None.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jor.2018.01.042.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Sher J.S., Uribe J.W., Posada A., Murphy B.J., Zlatkin M.B. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995 Jan;77(1):10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Goutallier D., Postel J.M., Bernageau J., Lavau L., Voisin M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304(July (304)):78–83. [PubMed] [Google Scholar]
- 3.Thomazeau H., Boukobza E., Morcet N., Chaperon J., Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344(November (344)):275–283. [PubMed] [Google Scholar]
- 4.Boileau P., Baque F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89(April (4)):747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 5.Maynou C., Mehdi N., Cassagnaud X., Audebert S., Mestdagh H. Clinical results of arthroscopic tenotomy of the long head of the biceps brachii in full thickness tears of the rotator cuff without repair: 40 cases. Rev Chir Orthop Reparatrice Appar Mot. 2005;91(June (4)):300–306. doi: 10.1016/s0035-1040(05)84327-2. [DOI] [PubMed] [Google Scholar]
- 6.Walch G., Edwards T.B., Boulahia A., Nove-Josserand L., Neyton L., Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14(May–June (3)):238–246. doi: 10.1016/j.jse.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Arrigoni P., Fossati C., Zottarelli L., Ragone V., Randelli P. Functional repair in massive immobile rotator cuff tears leads to satisfactory quality of living: results at 3-year follow-up. Musculoskeletal Surg. 2013;97(Suppl. 1):S73–S77. doi: 10.1007/s12306-013-0252-5. [DOI] [PubMed] [Google Scholar]
- 8.Burkhart S.S., Barth J.R., Richards D.P., Zlatkin M.B., Larsen M. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy. 2007;23(April (4)):347–354. doi: 10.1016/j.arthro.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Cho N.S., Rhee Y.G. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg. 2009;1(June (2)):96–104. doi: 10.4055/cios.2009.1.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung S.W., Kim J.Y., Kim M.H., Kim S.H., Oh J.H. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41(July (7)):1674–1683. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 11.Kim K.C., Shin H.D., Lee W.Y. Repair integrity and functional outcomes after arthroscopic suture-bridge rotator cuff repair. J Bone Joint Surg Am. 2012;18;94(April (8)):e48. doi: 10.2106/JBJS.K.00158. [DOI] [PubMed] [Google Scholar]
- 12.Meyer D.C., Wieser K., Farshad M., Gerber C. Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med. 2012;40(October (10)):2242–2247. doi: 10.1177/0363546512457587. [DOI] [PubMed] [Google Scholar]
- 13.Park J.Y., Lhee S.H., Oh K.S., Moon S.G., Hwang J.T. Clinical and ultrasonographic outcomes of arthroscopic suture bridge repair for massive rotator cuff tear. Arthroscopy. 2013;29(February (2)):280–289. doi: 10.1016/j.arthro.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Shen P.H., Lien S.B., Shen H.C., Lee C.H., Wu S.S., Lin L.C. Long-term functional outcomes after repair of rotator cuff tears correlated with atrophy of the supraspinatus muscles on magnetic resonance images. J Shoulder Elbow Surg. 2008;17(January–February(Suppl. 1)):1S–7S. doi: 10.1016/j.jse.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 15.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;21(July (339)):b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abraham C., Kelly M.P., West R., Michie S. The UK National Institute for Health and Clinical Excellence public health guidance on behaviour change: a brief introduction. Psychol Health Med. 2009;14(January (1)):1–8. doi: 10.1080/13548500802537903. [DOI] [PubMed] [Google Scholar]
- 17.Cho N.S., Yi J.W., Lee B.G., Rhee Y.G. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38(April (4)):664–671. doi: 10.1177/0363546509350081. [DOI] [PubMed] [Google Scholar]
- 18.Choi S., Kim M.K., Kim G.M., Roh Y.H., Hwang I.K., Kang H. Factors associated with clinical and structural outcomes after arthroscopic rotator cuff repair with a suture bridge technique in medium, large, and massive tears. J Shoulder Elbow Surg. 2014;23(November (11)):1675–1681. doi: 10.1016/j.jse.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 19.Chung S.W., Huong C.B., Kim S.H., Oh J.H. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy. 2013;29(February (2)):290–300. doi: 10.1016/j.arthro.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 20.Fuchs B., Gilbart M.K., Hodler J., Gerber C. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am. 2006;88(February (2)):309–316. doi: 10.2106/JBJS.E.00117. [DOI] [PubMed] [Google Scholar]
- 21.Grasso A., Milano G., Salvatore M., Falcone G., Deriu L., Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy. 2009;25(January (1)):4–12. doi: 10.1016/j.arthro.2008.09.018. [DOI] [PubMed] [Google Scholar]
- 22.Iannotti J.P., Deutsch A., Green A., Rudicel S., Christensen J., Marraffino S. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am. 2013;5;95(June (11)):965–971. doi: 10.2106/JBJS.L.00708. [DOI] [PubMed] [Google Scholar]
- 23.Kim J.R., Cho Y.S., Ryu K.J., Kim J.H. Clinical and radiographic outcomes after arthroscopic repair of massive rotator cuff tears using a suture bridge technique: assessment of repair integrity on magnetic resonance imaging. Am J Sports Med. 2012;40(April (4)):786–793. doi: 10.1177/0363546511434546. [DOI] [PubMed] [Google Scholar]
- 24.Lapner P.L., Jiang L., Zhang T., Athwal G.S. Rotator cuff fatty infiltration and atrophy are associated with functional outcomes in anatomic shoulder arthroplasty. Clin Orthop Relat Res. 2014;30(September) doi: 10.1007/s11999-014-3963-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mellado J.M., Calmet J., Olona M., Esteve C., Camins A., Perez Del Palomar L. Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. Am J Roentgenol. 2005;184(5):1456–1463. doi: 10.2214/ajr.184.5.01841456. [DOI] [PubMed] [Google Scholar]
- 26.Milano G., Grasso A., Salvatore M., Saccomanno M.F., Deriu L., Fabbriciani C. Arthroscopic rotator cuff repair with metal and biodegradable suture anchors: a prospective randomized study. Arthroscopy. 2010;26(September (Suppl. 9)):S112–S119. doi: 10.1016/j.arthro.2010.01.030. [DOI] [PubMed] [Google Scholar]
- 27.Milano G., Grasso A., Salvatore M., Zarelli D., Deriu L., Fabbriciani C. Arthroscopic rotator cuff repair with and without subacromial decompression: a prospective randomized study. Arthroscopy. 2007;23(January (1)):81–88. doi: 10.1016/j.arthro.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 28.Milano G., Saccomanno M.F., Careri S., Taccardo G., De Vitis R., Fabbriciani C. Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy. 2013;29(May (5)):802–810. doi: 10.1016/j.arthro.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 29.Moraiti C., Valle P., Maqdes A. Comparison of functional gains after arthroscopic rotator cuff repair in patients over 70 years of age versus patients under 50 years of age: a prospective multicenter study. Arthroscopy. 2015;31(Feb. (2)):184–190. doi: 10.1016/j.arthro.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 30.Nich C., Mutschler C., Vandenbussche E., Augereau B. Long-term clinical and mri results of open repair of the supraspinatus tendon. Clin Orthop Relat Res. 2009;467(10):2613–2622. doi: 10.1007/s11999-009-0917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oh J.H., Kim S.H., Shin S.H., Chung S.W., Kim J.Y., Kim S.H. Outcome of rotator cuff repair in large-to-massive tear with pseudoparalysis: a comparative study with propensity score matching. Am J Sports Med. 2011;39(July (7)):1413–1420. doi: 10.1177/0363546511399865. [DOI] [PubMed] [Google Scholar]
- 32.Park J.Y., Lhee S.H., Choi J.H., Park H.K., Yu JW Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36(July (7)):1310–1316. doi: 10.1177/0363546508315039. [DOI] [PubMed] [Google Scholar]
- 33.Ryu K.J., Kim B.H., Lee Y., Lee Y.S., Kim J.H. Modified suture-bridge technique to prevent a marginal dog-ear deformity improves structural integrity after rotator cuff repair. Am J Sports Med. 2014;24(December) doi: 10.1177/0363546514562175. [DOI] [PubMed] [Google Scholar]
- 34.Van Der Zwaal P., Pool L.D., Hacquebord S.T., Van Arkel E.R.A., Van Der List M.P.J. Arthroscopic side-to-Side repair of massive and contracted rotator cuff tears using a single uninterrupted suture: the shoestring bridge technique. Arthrosc J Arthroscopic Relat Surg. 2012;28(6):754–760. doi: 10.1016/j.arthro.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 35.Warner J.J., Parsons I.M., 4th Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2001;10(November–December (6)):514–521. doi: 10.1067/mse.2001.118629. [DOI] [PubMed] [Google Scholar]
- 36.Wiater B.P., Koueiter D.M., Maerz T., Moravek J.E., Jr, Yonan S., Marcantonio D.R. Preoperative deltoid size and fatty infiltration of the deltoid and rotator cuff correlate to outcomes after reverse total shoulder arthroplasty. Clin Orthop Relat Res. 2014;12(November) doi: 10.1007/s11999-014-4047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zumstein M.A., Jost B., Hempel J., Hodler J., Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Ser A. 2008;11;90(11):2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]
- 38.Chung S.W., Kim J.Y., Kim M.H., Kim S.H., Oh J.H. Arthroscopic repair of massive rotator cuff tears. outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41(7):1674–1683. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 39.Park J.S., Park H.J., Kim S.H., Oh J.H. Prognostic factors affecting rotator cuff healing after arthroscopic repair in small to medium-sized tears. Am J Sports Med. 2015;43(11):2386–2392. doi: 10.1177/0363546515594449. [DOI] [PubMed] [Google Scholar]
- 40.Shin S.J., Chung J., Lee J., Ko Y.-W. Recovery of muscle strength after intact arthroscopic rotator cuff repair according to preoperative rotator cuff tear size. Am J Sports Med. 2016;44(4):972–980. doi: 10.1177/0363546515625043. [DOI] [PubMed] [Google Scholar]
- 41.Kukkonen J., Joukainen A., Lehtinen J. Treatment of nontraumatic rotator cuff tears: a randomized controlled trial with two years of clinical and imaging follow-up. J Bone Joint Surg Am. 2015;4;97(21):1729–1737. doi: 10.2106/JBJS.N.01051. [DOI] [PubMed] [Google Scholar]
- 42.Bryant D., Holtby R., Willits K. A randomized clinical trial to compare the effectiveness of rotator cuff repair with or without augmentation using porcine small intestine submucosa for patients with moderate to large rotator cuff tears: a pilot study. J Shoulder Elbow Surg. 2016;25(October (10)):1623–1633. doi: 10.1016/j.jse.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 43.Jacquot A., Dezaly C., Goetzmann T., Roche O., Sirveaux F., Mole D. Is rotator cuff repair appropriate in patients older than 60 years of age? Prospective, randomised trial in 103 patients with a mean four-year follow-up. Orthop Traumatol Surg Res. 2014;100(October (Suppl. 6)):S333–S338. doi: 10.1016/j.otsr.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 44.Berth A., Neumann W., Awiszus F., Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11(March (1)):13–20. doi: 10.1007/s10195-010-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shi L.L., Cahill K.E., Ek E.T., Tompson J.D., Higgins L.D., Warner J.J. Latissimus dorsi and teres major transfer with reverse shoulder arthroplasty restores active motion and reduces pain for posterosuperior cuff dysfunction. Clin Orthop Relat Res. 2015;3(July) doi: 10.1007/s11999-015-4433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Edwards T.B., Boulahia A., Kempf J.F., Boileau P., Nemoz C., Walch G. The influence of rotator cuff disease on the results of shoulder arthroplasty for primary osteoarthritis: results of a multicenter study. J Bone Joint Surg Am. 2002;84-A(Dec. (12)):2240–2248. doi: 10.2106/00004623-200212000-00018. [DOI] [PubMed] [Google Scholar]
- 47.Franceschi F., Papalia R., Vasta S., Leonardi F., Maffulli N., Denaro V. Surgical management of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(Feb. (2)):494–501. doi: 10.1007/s00167-012-2317-7. [DOI] [PubMed] [Google Scholar]
- 48.Gasbarro G., Ye J., Newsome H. Morphologic risk factors in predicting symptomatic structural failure of arthroscopic rotator cuff repairs: tear size, location, and atrophy matter. Arthroscopy. 2016;32(Oct. (10)):1947–1952. doi: 10.1016/j.arthro.2016.01.067. [DOI] [PubMed] [Google Scholar]
- 49.Goutallier D., Postel J.M., Gleyze P., Leguilloux P., Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12(Nov–Dec (6)):550–554. doi: 10.1016/s1058-2746(03)00211-8. [DOI] [PubMed] [Google Scholar]
- 50.Goutallier D., Postel J.M., Radier C., Bernageau J., Zilber S. Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J Shoulder Elbow Surg. 2009;18(July–Aug (4)):521–528. doi: 10.1016/j.jse.2008.11.006. Epub 2009 Feb 11. [DOI] [PubMed] [Google Scholar]
- 51.Gumina S., Passaretti D., Gurzì M.D., Candela V. Arginine L-alpha-ketoglutarate, methylsulfonylmethane, hydrolyzed type I collagen and bromelain in rotator cuff tear repair: a prospective randomized study. Curr Med Res Opin. 2012;28(Nov. (11)):1767–1774. doi: 10.1185/03007995.2012.737772. [DOI] [PubMed] [Google Scholar]
- 52.Gumina S., Campagna V., Ferrazza G. Use of platelet-leukocyte membrane in arthroscopic repair of large rotator cuff tears: a prospective randomized study. J Bone Joint Surg Am. 2012;94(Aug. (15)):1345–1352. doi: 10.2106/JBJS.K.00394. [DOI] [PubMed] [Google Scholar]
- 53.Hug K., Gerhardt C., Haneveld H., Scheibel M. Arthroscopic knotless-anchor rotator cuff repair: a clinical and radiological evaluation. Knee Surg Sports Traumatol Arthrosc. 2015;23(Sep. (9)):2628–2634. doi: 10.1007/s00167-014-3026-1. [DOI] [PubMed] [Google Scholar]
- 54.Koh K.H., Lim T.K., Park Y.E., Lee S.W., Park W.H., Yoo J.C. Preoperative factors affecting footprint coverage in rotator cuff repair. Am J Sports Med. 2014;42(Apr. (4)):869–876. doi: 10.1177/0363546513518581. [DOI] [PubMed] [Google Scholar]
- 55.Kim J.K., Yoo H.J., Jeong J.H., Kim S.H. Effect of teres minor fatty infiltration on rotator cuff repair outcomes. Arthroscopy. 2016;32(Apr. (4)):552–558. doi: 10.1016/j.arthro.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 56.Lee H.J., Jeong J.Y., Kim C.K., Kim Y.S. Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: a prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg. 2016;25(July (7)):1107–1114. doi: 10.1016/j.jse.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 57.Namdari S., Donegan R.P., Dahiya N., Galatz L.M., Yamaguchi K., Keener J.D. Characteristics of small to medium-sized rotator cuff tears with and without disruption of the anterior supraspinatus tendon. J Shoulder Elbow Surg. 2014;23(Jan. (1)):20–27. doi: 10.1016/j.jse.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 58.Nicholas S.J., Lee S.J., Mullaney M.J. Functional outcomes after double-row versus single-row rotator cuff repair: a prospective randomized trial. Orthop J Sports Med. 2016;4(Oct. (10)) doi: 10.1177/2325967116667398. 2325967116667398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Paribelli G., Boschi S., Randelli P., Compagnoni R., Leonardi F., Cassarino A.M. Clinical outcome of latissimus dorsi tendon transfer and partial cuff repair in irreparable postero-superior rotator cuff tear. Musculoskelet Surg. 2015;99(Aug. (2)):127–132. doi: 10.1007/s12306-015-0353-4. [DOI] [PubMed] [Google Scholar]
- 60.Ryu K.J., Kim B.H., Lee Y., Lee Y.S., Kim J.H. Modified suture-bridge technique to prevent a marginal dog-ear deformity improves structural integrity after rotator cuff repair. Am J Sports Med. 2015;43(Mar. (3)):597–605. doi: 10.1177/0363546514562175. [DOI] [PubMed] [Google Scholar]
- 61.Taniguchi N., Suenaga N., Oizumi N. Bone marrow stimulation at the footprint of arthroscopic surface-holding repair advances cuff repair integrity. J Shoulder Elbow Surg. 2015;24(June (6)):860–866. doi: 10.1016/j.jse.2014.09.031. [DOI] [PubMed] [Google Scholar]
- 62.Toussaint B., Schnaser E., Bosley J., Lefebvre Y., Gobezie R. Early structural and functional outcomes for arthroscopic double-row transosseous-equivalent rotator cuff repair. Am J Sports Med. 2011;39(June (6)):1217–1225. doi: 10.1177/0363546510397725. [DOI] [PubMed] [Google Scholar]
- 63.Vastamäki M., Lohman M., Borgmästars N. Rotator cuff integrity correlates with clinical and functional results at a minimum 16 years after open repair. Clin Orthop Relat Res. 2013;471(Feb. (2)):554–561. doi: 10.1007/s11999-012-2494-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.